Escolar Documentos
Profissional Documentos
Cultura Documentos
Acute Respiratory Tract Infection Guideline Summary
Enviado por
Luke Rachel WurzTítulo original
Direitos autorais
Formatos disponíveis
Compartilhar este documento
Compartilhar ou incorporar documento
Você considera este documento útil?
Este conteúdo é inapropriado?
Denunciar este documentoDireitos autorais:
Formatos disponíveis
Acute Respiratory Tract Infection Guideline Summary
Enviado por
Luke Rachel WurzDireitos autorais:
Formatos disponíveis
Best Practices in the Management of Patients with Pharyngitis Reference Articles
pe
di
Clinician efforts to prescribe appropriately and to educate young patients and their parents/caregivers about antibiotics continue to play a vital role in decreasing
resistance levels. Parents/caregivers want their children to feel better soon but often do not understand that sore throat is usually caused by a virus, will not resolve with Otitis Media: Acute Respiratory
at
antibiotics, and that these medications have the potential to do more harm than good. 1. American Academy of Pediatrics, Subcommittee on Management of
Tract Infection
r
Acute Otitis Media. Diagnosis and Management of Acute Otitis Media.
Confirm a Streptococcal Cause of Pharyngitis BEFORE Prescribing Antibiotics.
ic
Pediatrics. 2004;113:1451-65.
Acute Bacterial Sinusitis:
Guideline Summary
Clinical signs and symptoms that strongly Clinical signs and symptoms that increase
suggest a non-streptococcal (usually viral) the probability of strep pharyngitis: The 1. The Sinus and Allergy Health Partnership. Antimicrobial Treatment
Selective etiology: signs and Guidelines for Acute Bacterial Rhinosinusitis. Otolaryngol Head Neck Surg.
2014
use of diagnostic • Pharyngeal or tonsillar swelling symptoms of
studies for strep • Cough • Erythema and exudate streptococcal and 2004;130:1-45.
pharyngitis on the basis • Rhinorrhea • Fever nonstreptococcal pharyngitis 2. Piccirillo JF. Acute Bacterial Siunsitis. NEJM. 2004;351:902-910.
of clinical features avoids • Oral ulcers Hoarseness • Lymphadenopathy overlap too broadly for
identifying streptococcus diagnosis to be made on 3. Wald E et al. Clinical Practice Guideline for the Diagnosis and Manage-
carriers along with acutely clinical grounds alone. ment of Acute Bacterial Sinusitis in Children Aged 1 to 18 Years. Pediatrics
Yes No Perform Yes
infected patients. Laboratory confirmation 2013;132:e232-e280.
Rapid Antigen of the diagnosis is
Detection Test necessary.
4. O’Brien K, et al. Acute Sinusitis – Principles of Judicious Use of
Antimicrobial Agents. Pediatrics. 1998;101:174-77.
Group A Strep (GAS)
Positive Negative
Strep Strep 5. Chow A, et. al. IDSA Clinical Practice Guideline for Acute Bacterial
testing usually not
Result Result Rhinosinusitis in Children and Adults.Clinical Infectious Diseases. 2012
recommended;
NO ANTIBIOTIC Apr;54(8):e72-e112. Epub 2012 Mar 20.
NEEDED Antibiotic therapy warranted Perform throat culture
Because
Negative
Pharyngitis:
of a general increase in Positive
Culture culture 1. Wessels MR. Clinical Practice. Streptococcal Pharyngitis. NEJM.
rates of resistance to antibiotics,
antimicrobial therapy should only be
2011;364:648-55.
prescribed for proven episodes of 2. Gerber GA, et al. Prevention of Rheumatic Fever and Diagnosis and Treat-
strep pharyngitis. Antibiotic therapy warranted No antibiotic needed ment of Acute Streptococcal Pharyngitis. Circulation. 2009;119:1541-1551.
Nonspecific Cough Illness/Bronchitis/Pertussis:
Opt for a narrow-spectrum antibiotic whenever possible for Symptom management 1. O’Brien K, et al. Cough Illness/Bronchitis Principles of Judicious Use of
strep pharyngitis. Avoid
Pain control is important for maintaining patient comfort, using aspirin for Antimicrobial Agents. Pediatrics. 1998;101:178-81.
• Penicillin (PCN; PO or IM) or amoxicillin + as is hydration. Assist in identifying safe home remedies children, due to the risk of 2. Centers for Disease Control and Prevention. Recommended antimicrobial
• For PCN-allergic patients, use a cephalosporin (for non-anaphy- and appropriate over-the-counter (OTC) medications (e.g., Reye’s syndrome
lactic type allergies), clindamycin, azithromycin or clarithromycin. analgesics and/or antipyretics) that may offer symptom relief. agents for the treatment and postexposure prophylaxis of pertussis: 2005
CDC guidelines. MMWR 2005;54(No. RR-14):1-16.
Educate, Advise and Assist Patients and Parents/Caregivers. Bronchiolitis/Nonspecific URI:
Viral cause: If rapid strep testing is negative, educate patients and parents/caregivers that the cause (pending possible cultures) is not strep but one of many different 1. Colgan R, et al. Appropriate Antimicrobial Prescribing: Approaches that
viruses, and antibiotics are not necessary. Even with typical symptoms, fewer than 30% of children have strep pharyngitis. Inform parents/caregivers that prior, repeated, Limit Antibiotic Resistance. AFP. 2001;64:999-1004.
or recent strep infection or exposure to someone with strep may increase the chance, but does not adequately confirm a current strep infection. 2. Dowell S, et al. Appropriate Use of Antibiotics for URIs in Children: Part II.
Value of testing/potential harm of antibiotics: Advise patients and parents/caregivers that rapid tests are highly reliable and allow providers to avoid using unneces- Cough, Pharyngitis and the Common Cold. AFP. 1998;58:1335-42.
sary antibiotics and the associated possible harm (medication side effects and increasing personal and societal antimicrobial resistance). 3. Dowell S, et al. Principles of Judicious Use of Antimicrobial Agents for
Signs of worsening: Educate patients and parents/caregivers that, occasionally, whatever the cause of a sore throat and whether antibiotics are prescribed or not, Pediatric Upper Respiratory Tract Infections. Pediatrics. 1998;101:163-65.
symptoms can worsen. If this is the case, re-evaluation is necessary. If symptoms do not begin to subside in 72 hours, schedule a re-visit for further evaluation.
4. Institute for Clinical Systems Improvement. Heath Care Guideline:
Illness prevention: Review illness prevention, including good hand and respiratory hygiene. Offer influenza vaccination to children 6 months to 18 years of age. Encour- Diagnosis and Treatment of Respiratory Illness in Children and Adults.
age parents/caregivers and household contacts of children to get vaccinated. Available at: www.icsi.org. Accessed August 2012.
Supporting Organizations Endorsing Organizations
CMA Foundation
Alameda Alliance for Health Health Plan of San Joaquin American Academy of California Association of 3840 Rosin Court, Suite 200
Anthem Blue Cross Inland Empire Health Plan Pediatrics, California District Nurse Practitioners
Blue Shield of California Kaiser Permanente Association of California California Pharmacists Association
Sacramento, CA 95834
CalOptima Kern Family Health Care Nurse Leaders California Society of Health-
Care1st Health Plan L.A. Care Health Plan California Academy of System Pharmacists
CenCal Health Molina Healthcare of California Family Physicians Urgent Care Association of America For more information visit our website:
Health Net of California California Academy of
Physician Assistants
Urgent Care College of Physicians www.aware.md
© 2013-14, California Medical Association Foundation.
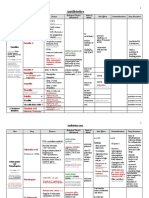
Illness Indications for Antibiotic Treatment Pathogen Antimicrobial Therapy Antibiotic Guidelines
Otitis Media When NOT to Treat with an Antibiotic: Otitis Media with Effusion. Streptococcus pneumoniae Antibiotic Duration: 7-10 days Length of oral therapy: American Academy of
• younger than 2 years or severe symptoms: 10 days Pediatrics (AAP) 2012
When to Treat with an Antibiotic: Acute Otitis Media (AOM) Nontypeable Haemophilus Severe AOM: Prescribe antibiotic therapy for AOM in • 2-5 years old with mild to moderate symptoms: 7 days
influenzae children >6 months of age with severe signs or symptoms • 6 years of age with mild to moderate symptoms: 5-7 days Centers for Disease Control and
1. Moderate to severe bulging of the tympanic membrane or new onset of otorrhea not due to acute (moderate or severe otalgia or otalgia for at least 48 hours Prevention (CDC)
otitis externa. Moraxella catarrhalis or temperature >39°C [102.2°F]). If child has not received amoxicillin in the past 30 days or the child does not have concurrent purulent
conjunctivitis: high dose amoxicillin (80-90 mg/kg/day) American Academy of
2. May diagnose acute otitis media in presence of mild bulging of the TM and recent (less than
Non-severe bilateral AOM in young children: Prescribe Family Physicians (AAFP)
48 hours) onset of ear pain (holding, tugging, rubbing of the ear in a nonverbal child) or intense
antibiotic therapy for bilateral AOM in children 6-23 months If the child has received amoxicillin in the last 30 days or has concurrent purulent conjunctivitis, or has a
erythema of the typmpanic membrane.
of age without severe signs or symptoms (mild otalgia for history of recurrent AOM unresponsive to amoxicillin: high dose amoxicillin/clavulanate (80-90 mg/kg/day of
3. Signs or symptoms of middle-ear inflammation as indicated by either: less than 48 hours and temperature <39°C [102.2°F]) amoxicillin component)
a. Distinct erythema of the tympanic membrane or
b. Distinct otalgia [discomfort clearly referable to the ear(s) that interferes with or precludes normal Non-severe unilateral AOM in young children (6 months Alternatives:
activity or sleep] to 23 months of age or non-severe AOM (bilateral or For non-anaphylactic ß-Lactam allergy: cefdinir, cefpodoxime, cefuroxime, ceftriaxone (50 mg/kg IM or IV per
unilateral) in older children (24 months or older): day for 1 or 3 days)
Note: Clinicians should not diagnose AOM in children who do not have middle ear effusion.
Prescribe antibiotic therapy or offer observation and close For severe ß-Lactam allergy: clindamycin
follow-up based on joint decision-making with the parent(s)/
caregiver in children without severe signs or symptoms (mild Unable to tolerate oral antibiotic: ceftriaxone (50 mg/kg IM or IV per day for 1 or 3 days)
otalgia <48 hours and temperature <39°C [102.2°F]). When Reassess the patient if the caregiver reports that the child’s symptoms have worsened or failed to respond to
observation is used, ensure follow-up and begin antibiotic the initial antibiotic treatment within 48 to 72 hours and determine whether a change in therapy is needed.
therapy if the child worsens or fails to improve within 48-72
hours of onset of symptoms. Failure of Initial Therapy:
Reassess the patient if the caregiver reports that the child’s symptoms have worsened or failed to respond to
Analgesics and Antipyretics: Always assess pain. If pain the initial antibiotic treatment within 48 to 72 hours and determine whether a change in therapy is needed.
When NOT to Treat with an Antibiotic: Do not prescribe prophylactic antibiotics is present, add treatment to reduce pain. Oral: ibuprofen/
acetaminophen (may use acetaminophen with codeine for If initial therapy has failed: high dose amoxicillin/clavulanate (80-90 mg/kg/day of amoxicillin component), or
to reduce the frequency of episodes of Acute Otitis Media (AOM) in children with moderate-severe pain). Topical: benzocaine (> 5 years of age). ceftriaxone (50 mg/kg IM or IV per day for 3 days), or clindamycin with or without cephalosporin (cefdinir,
recurrent AOM. cefixime or cefuroxime)
Acute Bacterial When NOT to Treat with an Antibiotic: Nearly all cases of acute sinusitis resolve Mainly viral pathogens Antibiotic Duration: Antibiotic therapy should be continued 1st Line: Infectious Diseases Society
Sinusitis without antibiotics. Antibiotic use should be reserved for moderate symptoms not for 7 days after the patient becomes free of signs and • Patients without increased risk for antibiotic resistant pneumococcal infection: amoxicillin pr amoxicillin- of America (IDSA) 2012
symptoms (minimum 10 days) clavulanate 45 mg/kg/day of amoxicillin component
improving after 10 days, or that are worsening after 5-6 days, and severe symptoms. • Patients with increased risk of antibiotic resistant pneumococcal infection (in those with severe infection AAP, AAFP, CDC
Severe onset and worsening course: Antibiotic therapy [fever>39°C, threat of suppurative complications], daycare attendance, <2 years of age, recent hospi-
When to Treat with an Antibiotic: : Clinicians should make a presumptive diagnosis of acute Streptococcus pneumoniae should be prescribed for acute bacterial sinusitis in children Sinus and Allergy Health
bacterial sinusitis when a child with an acute URI presents with the following: talization, antibiotic use within the past month, immunocompromised): amoxicillin-clavulanate high dose Partnership (SAHP)
Nontypeable Haemophilus with severe onset or worsening course (signs, symptoms, (90 mg/kg/day of amoxicillin component 2nd Line:
1. Persistent illness, ie, nasal discharge (of any quality) or daytime cough or both lasting >10 days influenzae or both).
• If amoxicillin-clavulanate 45 mg/kg/day used initially, may increase dose to 90 mg/kg/day
without improvement; OR Persistent illness: Antibiotics should be prescribed OR offer
Moraxella catarrhalis • For non-anaphylaxtic ß-lactam allergy: cefdinir, cefuroxime, or cefpodoxime
2. Worsening course, ie, worsening or new onset of nasal discharge, daytime cough, or fever after additional outpatient observation for 3 days to children with
initial improvement; OR persistent illness (nasal discharge of any quality or cough or • For severe ß-lactam allergy: levofloxacin
3. Severe onset, ie, concurrent fever (temperature ≥39°C/102.2°F) and purulent nasal discharge for both for at least 10 days without evidence of improvement). • Combination of clindamycin (or linezolid) and cefixime
at least 3 consecutive days. For severe ß-Lactam allergy: levofloxacin
Pharyngitis When NOT to Treat with an Antibiotic: Respiratory Viral Causes Conjunctivitis, Routine respiratory viruses Group A Strep: Treatment reserved for patients with 1st Line: AAP, AAFP, CDC, IDSA, Institute
cough, rhinorrhea, diarrhea uncommon with Group A Strep. positive rapid antigen detection or throat culture. • penicillin V for Clinical Systems Improve-
• benzathine penicillin G ment (ICSI)
When to Treat with an Antibiotic: Streptococcus pyogenes (Group A Strep) Symptoms Streptococcus pyogenes Antibiotic Duration: Generally 10 days (5 days if azithro- • amoxicillin
and signs: sore throat, fever, headache, tonsillopharyngeal erythema, exudates, palatal petechiae, tender mycin used)
For non-anaphylactic ß-Lactam allergy:
enlarged anterior cervical lymph nodes. Confirm diagnosis with throat culture or rapid antigen detection. If
rapid antigen detection is negative, obtain throat culture. • cephalosporin
For severe ß-Lactam allergy:
Diagnostic studies for Group A Strep are not indicated for children <3 years of age (because acute
rheumatic fever is rare in children <3 years old and the incidence of streptococcal pharyngitis and the • clindamycin, azithromycin or clarithromycin
classic presentation of streptococcal pharyngitis are uncommon in this age group).
Nonspecific Cough When NOT to Treat with an Antibiotic: Nonspecific cough illness. > 90% of cases caused by Antibiotics are generally not indicated. • azithromycin, clarithromycin AAP, AAFP, CDC
Illness / Bronchitis / routine respiratory viruses • tetracyclines for children > 8 years of age
Treatment reserved for Bordetella pertussis,
Pertussis When to Treat with an Antibiotic: Presents with prolonged, unimproving cough (14 days). < 10% of cases caused by Bor- Chlamydophila pneumoniae, Mycoplasma pneumoniae.
Clinically differentiate from pneumonia. If pertussis is suspected, appropriate laboratory diagnosis detella pertussis, Chlamydophila
encouraged (culture, PCR). Pertussis should be reported to public health authorities. Chlamydophila pneumoniae, or Mycoplasma Length of Therapy: 7-14 days (5 days for azithromycin)
pneumoniae and Mycoplasma pneumoniae may occur in older children (unusual < 5 years of age). pneumoniae
Bronchiolitis / When NOT to Treat with an Antibiotic: Sore throat, sneezing, mild cough, fever > 200 viruses, including rhino- Antibiotics not indicated. • None AAP, AAFP, CDC, ICSI
Nonspecific URI (generally < 102° F / 38.9° C, < 3 days), rhinorrhea, nasal congestion; self-limited viruses, coronaviruses, adenovi-
ruses, respiratory syncytial virus, Ensure hydration. May advise rest, antipyretics,
(typically 5-14 days). enteroviruses (coxsackieviruses analgesics, humidifier.
and echoviruses), influenza vi-
ruses and parainfluenza viruses
This guideline summary is intended for physicians and healthcare professionals to consider in managing the care of their patients for acute respiratory tract infections. While the summary describes recommended courses of intervention, it is not
intended as a substitute for the advice of a physician or other knowledgeable healthcare professional. These guidelines represent best clinical practice at the time of publication, but practice standards may change as more knowledge is gained.
Você também pode gostar
- Transport of Critically Ill Adults 2011Documento1 páginaTransport of Critically Ill Adults 2011velocity25Ainda não há avaliações
- Abst 1Documento20 páginasAbst 1martyAinda não há avaliações
- Eucast Exposicion PDFDocumento20 páginasEucast Exposicion PDFJordan PuenteAinda não há avaliações
- ARP Antibiotics Currently in Global Clinical Development Data Table v2Documento10 páginasARP Antibiotics Currently in Global Clinical Development Data Table v2tanishtarun06Ainda não há avaliações
- (PIDST) - 391 - Pidst - 20111020114358 - Filejou 2Documento20 páginas(PIDST) - 391 - Pidst - 20111020114358 - Filejou 2Nareunart KongkaAinda não há avaliações
- Communicable Disease Summary: A Guide For SchoolsDocumento31 páginasCommunicable Disease Summary: A Guide For SchoolsMohamoud MohamedAinda não há avaliações
- WHO EMP MAR 2012.3 Eng PDFDocumento78 páginasWHO EMP MAR 2012.3 Eng PDFonovAinda não há avaliações
- Surgical Site Infection Due To Mycobacterium Peregrinum: A Case Report and Literature ReviewDocumento3 páginasSurgical Site Infection Due To Mycobacterium Peregrinum: A Case Report and Literature ReviewHanung PujanggaAinda não há avaliações
- Karlien Vanhouteghem, Annelies Aerssens, Dirk Ommeslag, Jerina Boelens, Steven Callens, Anne-Marie Van Den AbeeleDocumento1 páginaKarlien Vanhouteghem, Annelies Aerssens, Dirk Ommeslag, Jerina Boelens, Steven Callens, Anne-Marie Van Den AbeeleAfien MuktiAinda não há avaliações
- Questions 43-52 Are Based On The Following Passages.: Aureus and Streptococcus Pneumoniae) Were TreatedDocumento11 páginasQuestions 43-52 Are Based On The Following Passages.: Aureus and Streptococcus Pneumoniae) Were TreatedKellyAinda não há avaliações
- Study of Factors Associated With Acute PharyngitisDocumento2 páginasStudy of Factors Associated With Acute PharyngitisMicaAinda não há avaliações
- Farmakoterapi Penyakit Paru Obstruksi Kronik (PPOK) : Tinjauan PustakaDocumento10 páginasFarmakoterapi Penyakit Paru Obstruksi Kronik (PPOK) : Tinjauan PustakaLilisAinda não há avaliações
- MODULE B TBPresentation3Documento62 páginasMODULE B TBPresentation3Jerommy MalweleAinda não há avaliações
- Thu 348 Ilc2022Documento1 páginaThu 348 Ilc2022rtthrtfhAinda não há avaliações
- Booklet Antimicrobial Prescribing Educational Booklet Offered by BiomerieuxDocumento21 páginasBooklet Antimicrobial Prescribing Educational Booklet Offered by Biomerieuxeli ferraraAinda não há avaliações
- Acute Respiratory Infeciton (ARI)Documento19 páginasAcute Respiratory Infeciton (ARI)Haryo Prakoso Adhi PAinda não há avaliações
- Treatmen PharyngitisDocumento8 páginasTreatmen PharyngitismeysiskaAinda não há avaliações
- Acute Respiratory InfectionDocumento15 páginasAcute Respiratory InfectionmAinda não há avaliações
- Antimicrobial Drugs TableDocumento19 páginasAntimicrobial Drugs TableLaylee ClareAinda não há avaliações
- Cartaaleditor PUBMEDDocumento3 páginasCartaaleditor PUBMEDSandra DelgadoAinda não há avaliações
- SWORBHPPCPMedical Directive Book 2015Documento148 páginasSWORBHPPCPMedical Directive Book 2015richardphilp1640Ainda não há avaliações
- Managing Microbes Poster AIF 00612Documento1 páginaManaging Microbes Poster AIF 00612Devina Sari PratiwiAinda não há avaliações
- Medical Prevention of Recurrent Acute Otitis Media: An Updated OverviewDocumento10 páginasMedical Prevention of Recurrent Acute Otitis Media: An Updated OverviewholaAinda não há avaliações
- Real-Time Alerting System For COVID-19 and Other Stress Events Using Wearable DataDocumento26 páginasReal-Time Alerting System For COVID-19 and Other Stress Events Using Wearable DataLuiz Folha FlaskAinda não há avaliações
- Affiche Infection MFA BRDocumento1 páginaAffiche Infection MFA BRcynthiaAinda não há avaliações
- Pharyngitis-Soothing The ThroatDocumento8 páginasPharyngitis-Soothing The ThroatridikittyAinda não há avaliações
- ArticulosDocumento5 páginasArticulosGrecia Alí AceroAinda não há avaliações
- Microbiology and Management of Peritonsillar, Retropharyngeal, and Parapharyngeal AbscessesDocumento6 páginasMicrobiology and Management of Peritonsillar, Retropharyngeal, and Parapharyngeal AbscessesVenter CiprianAinda não há avaliações
- Sars-Cov-2 Variants and Vaccines: Special ReportDocumento8 páginasSars-Cov-2 Variants and Vaccines: Special ReportRosamel FierroAinda não há avaliações
- ARDS Nuevas TerapiasDocumento3 páginasARDS Nuevas TerapiasEvelyn CóndorAinda não há avaliações
- Medical History Record FormDocumento4 páginasMedical History Record FormDaria BarannikAinda não há avaliações
- Surveilence Hais: Dr. Elsye Maria Rosa, M.KepDocumento9 páginasSurveilence Hais: Dr. Elsye Maria Rosa, M.KepEni MuchlisohAinda não há avaliações
- Biomérieux: Environmental Infection Control in HospitalsDocumento25 páginasBiomérieux: Environmental Infection Control in HospitalsYohana Fransisca WapiniAinda não há avaliações
- E-Poster Enterics For Global Health Shigella Surveillance StudyDocumento1 páginaE-Poster Enterics For Global Health Shigella Surveillance StudyNeyama AlladinAinda não há avaliações
- Optimization of Nursing Management Round 5ad3bdbbDocumento11 páginasOptimization of Nursing Management Round 5ad3bdbbsarvitaAinda não há avaliações
- The Effect of Turbinate Injection of Botulinum Toxin A On The Symptoms of Idiopathic RhinitisDocumento8 páginasThe Effect of Turbinate Injection of Botulinum Toxin A On The Symptoms of Idiopathic Rhinitismelon segerAinda não há avaliações
- Faringitis Fadhilla Annisa Efendi-1840312436Documento15 páginasFaringitis Fadhilla Annisa Efendi-1840312436fadhilla annisa efendiAinda não há avaliações
- Art 09Documento6 páginasArt 09Wiltor Kenner Rojas VillanuevaAinda não há avaliações
- Nhs Bronchiolitis Pathway Acute Setting South East Coast SCNDocumento2 páginasNhs Bronchiolitis Pathway Acute Setting South East Coast SCNdrgrizahAinda não há avaliações
- International Journal of Infectious DiseasesDocumento31 páginasInternational Journal of Infectious DiseasesAnonymous VXZymiAinda não há avaliações
- Vaccinegate:: Final Technical Report Molecular Profile Analysis of VaccineDocumento4 páginasVaccinegate:: Final Technical Report Molecular Profile Analysis of VaccineYiota KokkorisAinda não há avaliações
- Diarrhoea-Vomiting Pathway-Primary Care MAY 2015Documento2 páginasDiarrhoea-Vomiting Pathway-Primary Care MAY 2015nimraAinda não há avaliações
- Gastroenteritis PPT BonghanoyDocumento7 páginasGastroenteritis PPT BonghanoyELAINE ESTRERAAinda não há avaliações
- Cross Species Transmission of The Newly Identified Coronavirus 2019 nCoV - Ji - 2020 - Journal of MeDocumento1 páginaCross Species Transmission of The Newly Identified Coronavirus 2019 nCoV - Ji - 2020 - Journal of Metd5xb7w4dpAinda não há avaliações
- COVID-19 VACCINES THE 501Y.V2 Variant MLO HEALTH EDITDocumento3 páginasCOVID-19 VACCINES THE 501Y.V2 Variant MLO HEALTH EDITMelissa Albertyn-BrowneAinda não há avaliações
- Drug StudyDocumento16 páginasDrug StudygabbyAinda não há avaliações
- Objectives: Table 1. Selected Etiologies of Sore ThroatDocumento12 páginasObjectives: Table 1. Selected Etiologies of Sore ThroatRANIAinda não há avaliações
- Procalcitonin: BiomérieuxDocumento25 páginasProcalcitonin: Biomérieuxshafwan suyutiAinda não há avaliações
- SETTLING THE VIRUS DEBATE SourceDocumento2 páginasSETTLING THE VIRUS DEBATE SourceNina VictorAinda não há avaliações
- Acute TonsillopharyngitisDocumento9 páginasAcute TonsillopharyngitisMohammed HarisAinda não há avaliações
- Poster Caitlin BrennanDocumento1 páginaPoster Caitlin Brennansagun maharjanAinda não há avaliações
- Vacunas y Varantes Sars-Cov 2 Nejm 25-3-2021Documento3 páginasVacunas y Varantes Sars-Cov 2 Nejm 25-3-2021Cristhian Hormazabal WagnerAinda não há avaliações
- Period Dont Stop For PandemicDocumento1 páginaPeriod Dont Stop For PandemicMaria Nativity BanarioAinda não há avaliações
- White Paper Experimental Vaccines Covid-19 Feb 23Documento35 páginasWhite Paper Experimental Vaccines Covid-19 Feb 23Warren JamesAinda não há avaliações
- VaccinationDocumento6 páginasVaccinationJamil SalahAinda não há avaliações
- Microbiology Questions 2Documento6 páginasMicrobiology Questions 2JENNIFER JOHN MBBS2020Ainda não há avaliações
- Joy Benemor - T4-Sc-830-Aqa-Trilogy-Unit-43-Infection-And-Response-Foundation-Revision-Activity-Mat-Pack-English - Ver - 1Documento4 páginasJoy Benemor - T4-Sc-830-Aqa-Trilogy-Unit-43-Infection-And-Response-Foundation-Revision-Activity-Mat-Pack-English - Ver - 1v2jj5qfhjpAinda não há avaliações
- Can Trichomoniasis Cause Pharyngitis? A Case Report: Kitty Carter-Wicker, Onameyore Utuama and Folashade OmoleDocumento3 páginasCan Trichomoniasis Cause Pharyngitis? A Case Report: Kitty Carter-Wicker, Onameyore Utuama and Folashade OmoleradenbagasAinda não há avaliações
- Pemphigus VulgarisDocumento2 páginasPemphigus Vulgariszendah123Ainda não há avaliações
- To Test Your E/m Coding SkillsDocumento7 páginasTo Test Your E/m Coding SkillsLuke Rachel WurzAinda não há avaliações
- Nursing Sheet3Documento2 páginasNursing Sheet3Luke Rachel WurzAinda não há avaliações
- 01-08-2012 07 49 21PMDocumento1 página01-08-2012 07 49 21PMLuke Rachel WurzAinda não há avaliações
- Chapter 38 NS1030 Sue Study GuideDocumento19 páginasChapter 38 NS1030 Sue Study GuideLuke Rachel WurzAinda não há avaliações
- WatsuDocumento5 páginasWatsuTIME-TREVELER100% (1)
- SEO Roadmap - Bayut & DubizzleDocumento17 páginasSEO Roadmap - Bayut & Dubizzlebasel kotbAinda não há avaliações
- Afghanistan Law Bibliography 3rd EdDocumento28 páginasAfghanistan Law Bibliography 3rd EdTim MathewsAinda não há avaliações
- Case Study On TQMDocumento20 páginasCase Study On TQMshinyshani850% (1)
- Software Development Life CycleDocumento70 páginasSoftware Development Life CycleChaitanya MalikAinda não há avaliações
- MU151 Group Assignment 6Documento3 páginasMU151 Group Assignment 6Jay CadienteAinda não há avaliações
- AC2104 - Seminar 5Documento3 páginasAC2104 - Seminar 5Rachel LiuAinda não há avaliações
- Modbus Manual TD80 PDFDocumento34 páginasModbus Manual TD80 PDFAmar ChavanAinda não há avaliações
- EP105Use of English ArantxaReynosoDocumento6 páginasEP105Use of English ArantxaReynosoArantxaSteffiAinda não há avaliações
- Functions of Ecgc and Exim BankDocumento12 páginasFunctions of Ecgc and Exim BankbhumishahAinda não há avaliações
- Role LibrariesDocumento57 páginasRole LibrariesGiovanni AnggastaAinda não há avaliações
- Gaulish DictionaryDocumento4 páginasGaulish DictionarywoodwyseAinda não há avaliações
- Virtual Verde Release Plan Emails: Email 1Documento4 páginasVirtual Verde Release Plan Emails: Email 1Violet StarAinda não há avaliações
- Chemistry Important Questions-2015-2016Documento19 páginasChemistry Important Questions-2015-2016janu50% (4)
- A Guide To FractionsDocumento18 páginasA Guide To FractionsAnnelyanne RufinoAinda não há avaliações
- UntitledDocumento8 páginasUntitledMara GanalAinda não há avaliações
- Sample ProposalDocumento2 páginasSample ProposaltoupieAinda não há avaliações
- Read Chapter 4 Minicase: Fondren Publishing, Inc. From The Sales Force Management Textbook by Mark W. Johnston & Greg W. MarshallDocumento1 páginaRead Chapter 4 Minicase: Fondren Publishing, Inc. From The Sales Force Management Textbook by Mark W. Johnston & Greg W. MarshallKJRAinda não há avaliações
- Pengaruh Kompetensi Spiritual Guru Pendidikan Agama Kristen Terhadap Pertumbuhan Iman SiswaDocumento13 páginasPengaruh Kompetensi Spiritual Guru Pendidikan Agama Kristen Terhadap Pertumbuhan Iman SiswaK'lala GrianAinda não há avaliações
- Performance Task in Mathematics 10 First Quarter: GuidelinesDocumento2 páginasPerformance Task in Mathematics 10 First Quarter: Guidelinesbelle cutiee100% (3)
- What Does The Scripture Say - ' - Studies in The Function of Scripture in Early Judaism and Christianity, Volume 1 - The Synoptic GospelsDocumento149 páginasWhat Does The Scripture Say - ' - Studies in The Function of Scripture in Early Judaism and Christianity, Volume 1 - The Synoptic GospelsCometa Halley100% (1)
- English 7 Compare Contrast The People Could Fly Harriet TubmanDocumento3 páginasEnglish 7 Compare Contrast The People Could Fly Harriet Tubmanapi-508729334Ainda não há avaliações
- Native Americans - Clothing & Head DressesDocumento28 páginasNative Americans - Clothing & Head DressesThe 18th Century Material Culture Resource Center100% (15)
- SKI Report2008 - 50 2Documento46 páginasSKI Report2008 - 50 2nada safitriAinda não há avaliações
- Practical Interpretation and Application of Exoc Rine Panc Rea Tic Tes Ting in Small AnimalsDocumento20 páginasPractical Interpretation and Application of Exoc Rine Panc Rea Tic Tes Ting in Small Animalsl.fernandagonzalez97Ainda não há avaliações
- Gian Lorenzo BerniniDocumento12 páginasGian Lorenzo BerniniGiulia Galli LavigneAinda não há avaliações
- IPA Digital Media Owners Survey Autumn 2010Documento33 páginasIPA Digital Media Owners Survey Autumn 2010PaidContentUKAinda não há avaliações
- Complexity. Written Language Is Relatively More Complex Than Spoken Language. ..Documento3 páginasComplexity. Written Language Is Relatively More Complex Than Spoken Language. ..Toddler Channel TVAinda não há avaliações
- Bignay Chap 1 3 2Documento22 páginasBignay Chap 1 3 2Ralph AJ BalmesAinda não há avaliações
- Introduction To Professional School Counseling Advocacy Leadership and Intervention Ebook PDF VersionDocumento62 páginasIntroduction To Professional School Counseling Advocacy Leadership and Intervention Ebook PDF Versionmary.krueger918100% (50)