Escolar Documentos
Profissional Documentos
Cultura Documentos
Enviado por
Jefri Aditiya SaragihTítulo original
Direitos autorais
Formatos disponíveis
Compartilhar este documento
Compartilhar ou incorporar documento
Você considera este documento útil?
Este conteúdo é inapropriado?
Denunciar este documentoDireitos autorais:
Formatos disponíveis
Enviado por
Jefri Aditiya SaragihDireitos autorais:
Formatos disponíveis
Original Article
Skin Appendage Disord 2018;4:166–170 Received: September 7, 2017
Accepted: October 12, 2017
DOI: 10.1159/000484211
Published online: November 16, 2017
A Retrospective Study Comparing K101 Nail
Solution as a Monotherapy and in Combination
with Oral Terbinafine or Itraconazole for the
Treatment of Toenail Onychomycosis
Avner Shemer a Aditya K. Gupta b, c Meir Babaev d Aviv Barzilai d
Renata Farhi e C. Ralph Daniel III f, g
a Sackler Faculty of Medicine, Tel-Aviv University, Tel-Aviv, Israel; b Department of Medicine, University of Toronto,
Toronto, ON, and c Mediprobe Research Inc., London, ON, Canada; d Department of Dermatology, Sheba Medical
Center, Tel-Hashomer, Ramat Gan, Israel; e Hospital Nossa Senhora da Saude, University Fundação Tecnico
Educacional Souza Marques, Rio de Janeiro, Brazil; f Department of Dermatology, University of Mississippi School
of Medicine, Jackson, MS, and g Department of Dermatology, University of Alabama at Birmingham School of
Medicine, Birmingham, AL, USA
Keywords 0.029), while patients receiving itraconazole + K101 solution
Tinea unguium · Topical therapy · Fungal infection demonstrated improvement in percent of affected nail at 6
months (p = 0.037). At 15 months, there was no significant
difference between treatments for complete, clinical, and
Abstract mycological cure. Conclusion: Combination therapy with
Background: Onychomycosis is a difficult-to-treat fungal in- oral terbinafine or itraconazole and K101 nail solution results
fection of the nails. The efficacy of monotherapy is not ideal, in clearance of infected nail earlier than that with topical
and combination therapies provide an alternative that may K101 alone. These combinations may encourage compli-
increase treatment efficacy. Method: A retrospective analy- ance and be effective for patients with moderate onychomy-
sis of data from 91 patients was undertaken. Treatment for cosis. © 2017 S. Karger AG, Basel
toenail onychomycosis occurred between 2014 and 2016
and consisted of combination therapy with oral terbinafine
(250 mg/day for 12 weeks) or itraconazole (3 pulses, 400 mg/
day for 7 days) + K101 nail solution daily, or K101 nail solu- Introduction
tion monotherapy. Efficacy outcomes at 12 and 15 months
were analyzed. Results: At 12 months, the clinical cure rate Onychomycosis is a fungal infection of the nails that is
for combination of terbinafine + K101 solution was signifi- characterized by discoloration, nail plate thickening, and
cantly higher than that for K101 monotherapy (p = 0.008). onycholysis [1]. The efficacy of oral antifungal treatments
Patients receiving this combination also showed significant ranges from 38 to 75% for mycological cure and from 23
improvement in percent of affected nail at 3 months (p = to 46% for complete cure [2]. Topical antifungal treat-
© 2017 S. Karger AG, Basel Dr. Aditya K. Gupta
Mediprobe Research Inc.
645 Windermere Road
E-Mail karger@karger.com
London, ON N6H2M1 (Canada)
www.karger.com/sad
E-Mail agupta @ execulink.com
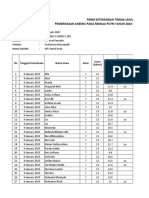
Table 1. Baseline participant characteristics
Treatment arms Total p values
K101 T + K101 I + K101
Gender males 25 22 7 54 (59.3%) 0.507
females 19 11 7 37 (40.7%)
total 44 33 14 91
Mean age ± SD, years 43.8 ± 9.3 44.7 ± 11.6 41.6 ± 7.0 43.9 ± 9.8 0.624
Disease duration <10 years 7 6 3 16 (17.6%) 0.776
10 – 19 years 19 18 6 43 (47.3%)
≥20 years 18 9 5 32 (35.2%)
total 44 33 14 91
BL severity 31 – 49% 36 27 13 76 (83.5%) 0.592
(% nail involvement) ≥50% 8 6 1 15 (16.5%)
total 44 33 14 91
BL culture dermatophyte 33 24 12 69 (75.8%) 0.731
Candida spp. 1 3 0 4 (4.4%)
NDM 4 1 1 6 (6.6%)
mixed infection 6 5 1 12 (13.2%)
total 44 33 14 91
T, terbinafine; I, itraconazole; SD, standard deviation; BL, baseline; NDM, nondermatophyte.
ments may be preferred for patients with mild disease or tolytic, softening, and antimycotic effects. A randomized
those who are immunocompromised or using multiple double-blind controlled trial reported mycological cure
medications. However, the efficacy of topical antifungals rates with K101 solution that were similar to those re-
ranges from 29 to 90% for mycological cure and from 1 ported for ciclopirox and amorolfine lacquers [3]. Pa-
to 18% for complete cure [3]. tients also reported improvement of clinical symptoms,
Combining oral and topical antifungal regimens could such as thickening, discoloration, and brittleness of nails
potentially increase cure rates for onychomycosis. Where- [9].
as mild cases (<30% diseased nail) of onychomycosis may The current study is a retrospective analysis of patients
not benefit significantly more from combination treat- undergoing treatment for toenail onychomycosis. We
ment, evidence suggests that moderate to severe cases of compared combination treatment of oral terbinafine or
onychomycosis, or cases with traditionally difficult-to- itraconazole and topical K101 nail solution with K101
treat features (e.g., dermatophytoma, onycholysis), could nail solution monotherapy.
benefit from combination treatment [4–6]. Combination
therapies that have shown efficacy in treating onychomy-
cosis include oral terbinafine with topical amorolfine [5, Methods
6] or ciclopirox [6, 7], and itraconazole with amorolfine This was a retrospective analysis of data from 91 patients with
[8]. toenail onychomycosis undergoing treatment between May 2014
K101 nail solution (Emtrix®, Kerasal Nail®, NaloxTM/ and March 2016, and, as such, the analysis did not require institu-
NalocTM) is available without prescription and is market- tional approval. Patients were diagnosed with mycologically con-
ed in the EU, Asia, and North America as a treatment for firmed (positive smear and positive culture) distal lateral subun-
gual onychomycosis of the great toenail, with up to 75% baseline
onychomycosis. This nail solution is a combination of nail involvement. Mycology was performed at a government-ap-
propylene glycol (66.4%), urea (20%), and lactic acid proved mycology laboratory associated with a dermatology prac-
(10%), which likely act in combination to produce kera- tice. To determine the causative organism, nondermatophyte
Combination Therapy for Onychomycosis Skin Appendage Disord 2018;4:166–170 167
DOI: 10.1159/000484211
Table 2. Organisms cultured at baseline Results
Organism(s) Treatment arm The mean age of this sample was 43.8 ± 9.9 years, with
K101 T + K101 I + K101 59% of patients being male. The majority of patients were
aged 59 years or younger, with 38.5% under the age of 40
Dermatophytes
years and 52.7% between ages 40 and 59 years. Onycho-
Trichophyton rubrum 29 16 11
Trichophyton mentagrophytes 3 6 mycosis had been present for 10 years or longer in 83% of
Trichophyton tonsurans 1 1 the patients. Patients clinically presented with onycho-
Epidermophyton floccosum 1 1 mycosis affecting between 31 and 60% of the nail (Ta-
Nondermatophytes ble 1). Culture was obtained at baseline prior to treat-
Acremonium spp. 2 1 ment. Dermatophyte, mixed dermatophyte-nonderma-
Fusarium spp. 1 tophyte mold, nondermatophyte mold, and Candida
Penicillium spp. 1 infections comprised 75.8, 13.2, 6.6, and 4.4% of the sam-
Scopulariopsis spp. 1
ple, respectively (Tables 1, 2). There were no significant
Candida differences in baseline characteristics between the treat-
Candida albicans 2 ment groups (ps > 0.05; Table 1).
Candida krusei 1
Candida tropicalis 1
Analysis of percent of affected nail across time pro-
duced a significant time × treatment interaction (F(8,
Mixed infections 401) = 2.48, p = 0.012). All 3 treatments produced sig-
T. rubrum + Acremonium 1 1
T. mentagrophytes + C. krusei 1
nificant improvements from baseline in percent of nail
T. rubrum + Neoscytalidium affected (p < 0.001). At 3 (p = 0.001), 6 (p < 0.001), 12
dimidiatum 2 1 (p < 0.001), and 15 months (p = 0.021), the percent of af-
T. rubrum + Fusarium 2 1 fected nail for the combination of terbinafine + K101 was
T. mentagrophytes + significantly lower than that for K101 topical solution
Penicillium 1 2
alone. The combination of itraconazole + K101 also
T, terbinafine; I, itraconazole. showed significant improvement compared to K101 top-
ical solution alone at both 6 (p = 0.037) and 12 months
(p = 0.008).
Table 3 shows efficacy outcomes at 12 and 15 months.
After 12 months of topical treatment with K101, those
mold or Candida spp. were required to be cultured 3 times in the patients who also had oral terbinafine demonstrated a
absence of dermatophytes [10]. The amount of infected and
clinical cure rate that was significantly higher than that
healthy nail was measured longitudinally in mm at baseline and at
subsequent visits. with K101 treatment alone (42.4 vs. 9.1%, p = 0.003). The
All patients (n = 91) used topical K101 nail solution once daily efficacy rate of itraconazole combined with K101 was not
for 15 months. Treatment consisted of topical therapy alone (n = significantly different from either group. At 15 months,
44) or of topical therapy in parallel with either oral terbinafine, 250 there were no differences in efficacy rates between treat-
mg once daily for 12 weeks (n = 33), or 3 pulses of itraconazole,
ments for clinical, complete, and mycological cure (ps >
200 mg twice daily for 7 days (n = 14). Follow-up visits took place
at 3, 6, 12, and 15 months, with mycological samples taken at 15 0.05). χ2 tests were also conducted on dermatophyte-only
months (smear and culture). infections (Table 3) with the same patterns observed.
Efficacy outcomes evaluated in this study included clinical Omitting Candida infections from the analyses did not
cure, mycological cure, and complete cure. Clinical cure was de- alter the findings.
fined as 100% clear nail, evaluated at 12 and 15 months. Myco-
logical cure was defined as negative smear and negative culture,
and complete cure was defined as 100% clear nail with mycological
cure, both evaluated at 15 months. The proportion of affected nail Discussion
was calculated at all visits. Categorical baseline participant vari-
ables and efficacy outcomes were compared with χ2 and Fisher K101 topical nail solution monotherapy was com-
exact tests, while continuous baseline participant variables were
compared using one-way ANOVA. A mixed linear model was used
pared to K101 solution in combination with oral terbin-
to compare percent clear nail between treatments and across visits, afine or itraconazole. Combination treatments did not
and Bonferroni correction was used for comparisons. Significance produce significantly higher cure rates at 15 months.
was set to α = 0.05. However, cure rates were qualitatively higher with both
168 Skin Appendage Disord 2018;4:166–170 Shemer/Gupta/Babaev/Barzilai/Farhi/
DOI: 10.1159/000484211 Daniel III
Table 3. Efficacy outcomes stratified by organism cultured at baseline
Organism 12 months 15 months
clinical cure complete cure clinical cure mycological cure
K101 total 4/44 (9.1%) 13/44 (29.5%) 13/44 (29.5%) 24/44 (54.5%)
derm. 4/33 (12.1%) 11/33 (33.3%) 11/33 (33.3%) 16/33 (48.5%)
NDM 0/4 0/4 0/4 3/4
Candida 0/1 1/1 1/1 1/1
mixed 0/6 1/6 1/6 4/6
Terbinafine + K101 total 14/33 (42.4%)* 18/33 (54.5%) 18/33 (54.5%) 21/33 (63.6%)
derm. 10/24 (41.7%)* 14/24 (58.3%) 14/24 (58.3%) 15/24 (62.5%)
NDM 0/1 1/1 1/1 1/1
Candida 1/3 1/3 1/3 2/3
mixed 3/5 2/5 2/5 3/5
Itraconazole + K101 total 5/14 (35.7%) 9/14 (64.3%) 9/14 (64.3%) 10/14 (71.4%)
derm. 4/12 (33.3%) 8/12 (66.7%) 8/12 (66.7%) 8/12 (66.7%)
NDM 0/1 1/1 1/1 1/1
mixed 1/1 0/1 0/1 1/1
Derm., dermatophyte; NDM, nondermatophyte. * p < 0.05, terbinafine + K101 significantly different from K101 alone.
combination treatments. Additionally, evidence of suc- This sample included patients with nondermatophyte
cessful treatment was observed much earlier in time with and mixed infections. Clinical trials usually enroll derma-
the combination of oral terbinafine and K101 nail solu- tophyte-confirmed onychomycosis, yet recent epidemio-
tion compared to monotherapy; as early as 3 months into logical studies have reported a prevalence of nonderma-
treatment. Combinations can take advantage of the mul- tophyte/mixed infections ranging from 28 to 48% [13,
tiple routes by which antifungal agents reach the site of 14]. Although the present study included few patients
fungal nail infections [11]. This may be relevant for pa- with these infections (n = 18), mycological cure was ob-
tients who can tolerate oral treatment, as a reduction in served in 13 patients.
clinical signs and symptoms can encourage treatment There are limitations to this study. The retrospective
compliance. nature and small sample size of the current analysis pre-
Efficacy rates in the current sample are consistent with vent generalization of the results. Additionally, oral anti-
published results. Previously, mycological cure after K101 fungal monotherapy was not included, and it is possible
treatment for 6 months was 27.2% (dermatophyte-con- that the efficacy of the combination groups reflects oral
firmed onychomycosis with ≤50% of nail involvement), treatment alone. However, these data demonstrate that
while patient-rated reduction or patient-rated absence of combination treatment of terbinafine or itraconazole
symptoms was reported by 42.9% [12]. The current study with K101 nail solution may be effective for patients with
included patients with up to 75% of nail involvement; moderate onychomycosis. The clearance of affected nail
complete and mycological cure of dermatophyte infec- observed at 3 and 6 months with combination treatment
tions after 15 months of K101 solution alone were 33.3 may encourage patient compliance compared to mono-
and 48.5%, respectively. Combination treatment with therapy. The future in treating onychomycosis likely en-
oral terbinafine or itraconazole and K101 nail solution tails finding successful combinations of antifungal treat-
produced complete cure rates at 15 months (54.5 and ments or combinations of antifungal treatments in con-
64.3%, respectively) similar to the success rate of 59.2% cert with devices.
(negative mycology and ≤10% of original total diseased
nail still affected) reported at 18 months with oral terbin-
afine and amorolfine [5].
Combination Therapy for Onychomycosis Skin Appendage Disord 2018;4:166–170 169
DOI: 10.1159/000484211
Statement of Ethics Disclosure Statement
This was a retrospective analysis of data from 91 patients, and, The authors have nothing to disclose.
as such, the analysis did not require institutional approval.
References
1 Faergemann J, Baran R: Epidemiology, clini- 6 Jaiswal A, Sharma RP, Garg AP: An open ran- 10 Shemer A, Davidovici B, Grunwald MH, Trau
cal presentation and diagnosis of onychomy- domized comparative study to test the effica- H, Amichai B: New criteria for the laboratory
cosis. Br J Dermatol 2003;149(suppl 65):1–4. cy and safety of oral terbinafine pulse as a diagnosis of nondermatophyte moulds in on-
2 Evans EG, Sigurgeirsson B: Double blind, ran- monotherapy and in combination with topi- ychomycosis. Br J Dermatol 2009;160:37–39.
domised study of continuous terbinafine cal ciclopirox olamine 8% or topical amorol- 11 Gupta AK, Simpson FC: Routes of drug deliv-
compared with intermittent itraconazole in fine hydrochloride 5% in the treatment of on- ery into the nail apparatus: implications for
treatment of toenail onychomycosis. The ychomycosis. Indian J Dermatol Venereol the efficacy of topical nail solutions in ony-
LION Study Group. BMJ 1999; 318: 1031– Leprol 2007;73:393–396. chomycosis. J Dermatol Treat 2016;27:2–4.
1035. 7 Avner S, Nir N, Henri T: Combination of oral 12 Emtestam L, Kaaman T, Rensfeldt K: Treat-
3 Gupta AK, Daigle D, Foley KA: Topical ther- terbinafine and topical ciclopirox compared ment of distal subungual onychomycosis with
apy for toenail onychomycosis: an evidence- to oral terbinafine for the treatment of ony- a topical preparation of urea, propylene glycol
based review. Am J Clin Dermatol 2014; 15: chomycosis. J Dermatol Treat 2005; 16: 327– and lactic acid: results of a 24-week, double-
489–502. 330. blind, placebo-controlled study. Mycoses
4 Olafsson JH: Combination therapy for ony- 8 Lecha M: Amorolfine and itraconazole com- 2012;55:532–540.
chomycosis. Br J Dermatol 2003;149:15–18. bination for severe toenail onychomycosis; 13 Gupta AK, Gupta G, Jain HC, Lynde CW, Fol-
5 Baran R, Sigurgeirsson B, de Berker D, results of an open randomized trial in Spain. ey KA, Daigle D, et al: The prevalence of un-
Kaufmann R, Lecha M, Faergemann J, et al: A Br J Dermatol 2001;145(suppl 60):21–26. suspected onychomycosis and its causative
multicentre, randomized, controlled study of 9 Faergemann J, Gullstrand S, Rensfeldt K: Ear- organisms in a multicentre Canadian sample
the efficacy, safety and cost-effectiveness of a ly and visible improvements after application of 30,000 patients visiting physicians’ offices.
combination therapy with amorolfine nail of K101 in the appearance of nails discoloured J Eur Acad Dermatol Venereol 2016;30:1567–
lacquer and oral terbinafine compared with and deformed by onychomycosis. J Cosmet 1572.
oral terbinafine alone for the treatment of on- Dermatol Sci Appl 2011;1:59–63. 14 Ioannidou D, Maraki S, Krasagakis S, Tosca
ychomycosis with matrix involvement. Br J A, Tselentis Y: The epidemiology of onycho-
Dermatol 2007;157:149–157. mycoses in Crete, Greece, between 1992 and
2001. J Eur Acad Dermatol Venereol 2006;20:
170–174.
170 Skin Appendage Disord 2018;4:166–170 Shemer/Gupta/Babaev/Barzilai/Farhi/
DOI: 10.1159/000484211 Daniel III
Você também pode gostar
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeNo EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeNota: 4 de 5 estrelas4/5 (5795)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreNo EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreNota: 4 de 5 estrelas4/5 (1090)
- Never Split the Difference: Negotiating As If Your Life Depended On ItNo EverandNever Split the Difference: Negotiating As If Your Life Depended On ItNota: 4.5 de 5 estrelas4.5/5 (838)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceNo EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceNota: 4 de 5 estrelas4/5 (895)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersNo EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersNota: 4.5 de 5 estrelas4.5/5 (345)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureNo EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureNota: 4.5 de 5 estrelas4.5/5 (474)
- The Emperor of All Maladies: A Biography of CancerNo EverandThe Emperor of All Maladies: A Biography of CancerNota: 4.5 de 5 estrelas4.5/5 (271)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)No EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Nota: 4.5 de 5 estrelas4.5/5 (121)
- The Little Book of Hygge: Danish Secrets to Happy LivingNo EverandThe Little Book of Hygge: Danish Secrets to Happy LivingNota: 3.5 de 5 estrelas3.5/5 (400)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyNo EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyNota: 3.5 de 5 estrelas3.5/5 (2259)
- The Yellow House: A Memoir (2019 National Book Award Winner)No EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Nota: 4 de 5 estrelas4/5 (98)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaNo EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaNota: 4.5 de 5 estrelas4.5/5 (266)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryNo EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryNota: 3.5 de 5 estrelas3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnNo EverandTeam of Rivals: The Political Genius of Abraham LincolnNota: 4.5 de 5 estrelas4.5/5 (234)
- Feasts For The GodsDocumento79 páginasFeasts For The GodsVasile Sturzu100% (6)
- The Unwinding: An Inner History of the New AmericaNo EverandThe Unwinding: An Inner History of the New AmericaNota: 4 de 5 estrelas4/5 (45)
- Volhard Puppy Aptitude TestDocumento4 páginasVolhard Puppy Aptitude TestChristine KemperAinda não há avaliações
- Chimp Haven Federal Complaint 6-13-22Documento11 páginasChimp Haven Federal Complaint 6-13-22USA TODAY NetworkAinda não há avaliações
- Mark Passio FYMC2011Documento176 páginasMark Passio FYMC2011roseguy7100% (3)
- TNPSC Sample Paper 3 PDFDocumento40 páginasTNPSC Sample Paper 3 PDFShiva Shankar PandianAinda não há avaliações
- Roleplaying in The DisgaeaverseDocumento268 páginasRoleplaying in The DisgaeaverseChris Harvey100% (2)
- Dichotomous Key Mini-Unit Lesson PlanDocumento13 páginasDichotomous Key Mini-Unit Lesson Plancandicewest100% (4)
- Pemeriksaan Anemia SMP Darul MaarifDocumento38 páginasPemeriksaan Anemia SMP Darul MaarifPuskesmas BanyuputihAinda não há avaliações
- RPD Esthetic. ReviewDocumento6 páginasRPD Esthetic. Revieweili1Ainda não há avaliações
- Book of Arcane Magic - WE - Reborn Soul Sorcerer Bloodline PDFDocumento3 páginasBook of Arcane Magic - WE - Reborn Soul Sorcerer Bloodline PDFJohn FrangosAinda não há avaliações
- (1951) Out of Step: Events in The Two Lives of An Anti-Jewish Camel-DoctorDocumento71 páginas(1951) Out of Step: Events in The Two Lives of An Anti-Jewish Camel-DoctorHerbert Hillary Booker 2ndAinda não há avaliações
- Tajweed Rules of The Qur'anDocumento25 páginasTajweed Rules of The Qur'anridwanmdAinda não há avaliações
- 1.3 DeterminersDocumento40 páginas1.3 DeterminersTESL30621 Siti Syasya Aqilah Binti Sheikh SalimAinda não há avaliações
- Appearance VocabularyDocumento6 páginasAppearance VocabularyVICAIDIAinda não há avaliações
- Grammar Test 2Documento1 páginaGrammar Test 2Anikó AnikóAinda não há avaliações
- How To Tell Wild AnimalsDocumento20 páginasHow To Tell Wild AnimalsShreyansh SahuAinda não há avaliações
- Ountable Nouns: A Dog Is An AnimalDocumento9 páginasOuntable Nouns: A Dog Is An AnimalJoseMa AralAinda não há avaliações
- Diabetes Mellitus (DM) 2Documento1 páginaDiabetes Mellitus (DM) 2Bheru Lal100% (1)
- Patons W588 Crochet CardiganDocumento2 páginasPatons W588 Crochet CardiganAna LucioAinda não há avaliações
- EngDocumento23 páginasEngrupAinda não há avaliações
- Blok 22 - Skenario D - 2019 Neonatal Case: ST TH THDocumento6 páginasBlok 22 - Skenario D - 2019 Neonatal Case: ST TH THNur akilaAinda não há avaliações
- Bill Bryson and His Friend Stephen Katz Are Camping in The Woods of North AmericaDocumento5 páginasBill Bryson and His Friend Stephen Katz Are Camping in The Woods of North AmericaSonal BhatiaAinda não há avaliações
- NCP - BaiaeDocumento4 páginasNCP - BaiaeErmi Tañio0% (1)
- Map & Tree Map.: Figure 1: Circle Map (Sources Maps - HTML)Documento8 páginasMap & Tree Map.: Figure 1: Circle Map (Sources Maps - HTML)Hus HusainiAinda não há avaliações
- Introducing The DogDocumento22 páginasIntroducing The DogPope SmithAinda não há avaliações
- 1cambridge English Prepare 3 WorkbookDocumento90 páginas1cambridge English Prepare 3 WorkbookMariana Villalón100% (1)
- Ket CambridgeDocumento23 páginasKet Cambridgeo100Ainda não há avaliações
- 1.1 The Little School BusDocumento156 páginas1.1 The Little School BusAifa Afeeqa JamilanAinda não há avaliações
- Surrogacy DebateDocumento4 páginasSurrogacy DebateTerence ValdehuezaAinda não há avaliações
- General Awareness and Aptitude Test: Questions: 40 Marks: 160Documento58 páginasGeneral Awareness and Aptitude Test: Questions: 40 Marks: 160Nooruddin Sheik100% (2)