Escolar Documentos
Profissional Documentos
Cultura Documentos
Ppe1 PDF
Enviado por
Anonymous CqAPN7PJ8Título original
Direitos autorais
Formatos disponíveis
Compartilhar este documento
Compartilhar ou incorporar documento
Você considera este documento útil?
Este conteúdo é inapropriado?
Denunciar este documentoDireitos autorais:
Formatos disponíveis
Ppe1 PDF
Enviado por
Anonymous CqAPN7PJ8Direitos autorais:
Formatos disponíveis
1428 Letters to the Editor / American Journal of Infection Control 44 (2016) 1427-30
Sonja Skljarevski, MDa, Amanda Barner, PharmD, BCPSb,*, In the care of patients with Ebola virus disease, a key principle
Lou Ann Bruno-Murtha, DOa,c,d was to remove all body PPE before removing the facial PPE in the
a
Internal Medicine, Cambridge Health Alliance, Cambridge, MA event of aerosolization as the gown is removed, protecting mucous
b membranes.8 Example 2 shows the jumbled removal of gown
Clinical Pharmacy, Cambridge Health Alliance, Cambridge, MA
and gloves together. This method is ripe with opportunities for
c
Division of Infectious Diseases, Cambridge Health Alliance, losing control of the gloves, which are the most contaminated
Cambridge, MA elements of the PPE worn. Good glove-in-glove technique keeping
d the cuffs of the gown clean is a much safer alternative. Clean
Harvard Medical School, Cambridge, MA
cuffs can then be slid over the hands before gown removal to
prevent the dirty side of the sleeves from coming into contact
* Address correspondence to Amanda Barner, PharmD, BCPS,
with skin.9
Cambridge Health Alliance, 1035 Cambridge St, Cambridge, MA
A clear standard for PPE use is critical to safe and cohesive prac-
02141.
tices when the infectious risk for an illness is great or the mortality
E-mail address: abarner@challiance.org (A. Barner).
rate for a newly emerging pathogen is high. Current and future health
care professionals deserve clear and concise guidance on how best
http://dx.doi.org/10.1016/j.ajic.2016.07.029
to protect themselves in light of the many infectious threats which
will likely emerge in the coming years. More research into clinical
actions that generate aerosols and what role PPE plays in preven-
tion is also needed. No health care–associated infection of a health
care worker or the patients in their care should be acceptable
when the tools are available to protect them if used and used
correctly.
Call for improvement in References
personal protective 1. Centers for Disease Control and Prevention. Guideline for isolation precautions:
preventing transmission of infectious agents in healthcare settings 2007.
equipment guidance and 2007. Available from: http://www.cdc.gov/hicpac/pubs.html. Accessed April 26,
2016.
research 2. Public Health Agency of Canada. Prevention and control of influenza during a
pandemic for all healthcare settings. Annex F. 2011. Available from:
http://www.phac-aspc.gc.ca/cpip-pclcpi/assets/pdf/ann-f-eng.pdf. Accessed April
26, 2016.
To the Editor: 3. World Health Organization. Epidemic and pandemic alert and response. 2008.
Available from: http://www.who.int/csr/resources/publications/PPE_EN_A1sl
There is urgent need for improvements to the current guid- .pdf?ua=1. Accessed April 26, 2016.
4. Jaeger JL, Patel M, Dharan N, Hancock K, Meites E, Mattson C, et al. Transmission
ance on personal protective equipment (PPE) use for health care of 2009 pandemic influenza A (H1N1) virus among healthcare personnel-Southern
workers from the Centers for Disease Control and Prevention.1 California, 2009. Infect Control Hosp Epidemiol 2011;32:1149-57.
The guidance informs health care professions’ curriculum and 5. Ofner-Agostini M, Gravel D, McDonald LC, Lem M, Sarwal S, McGeer A, et al. Cluster
of cases of severe acute respiratory syndrome among Toronto healthcare workers
professional examinations throughout the United States. Stan- after implementation of infection control precautions: a case series. Infect Control
dards from other international partners differ, particularly in the Hosp Epidemiol 2006;27:473-8.
doffing sequence.2,3 Health care workers are known to inconsis- 6. National Institute of Occupational Health and Safety (NIOSH). Preventing
occupational exposures to antineoplastic and other hazardous drugs in health
tently or inadequately use PPE, even in the face of epidemic
care settings. Publication No. 2004-165. Cincinnati (OH): National Institute for
diseases, such as severe acute respiratory syndrome and pandem- Occupational Safety and Health (NIOSH); 2004.
ic influenza A (H1N1) virus.4,5 One clear and safe standard which 7. Munoz-Price LS, Banach D, Bearman G, Gould JM, Leekha S, Morgan D, et al.
Isolation precautions for visitors. Infect Control Hosp Epidemiol 2015;36:747-58.
moves seamlessly from preventing health care–associated infec-
doi:10.1017/ice.2015.67.
tions to protecting health care workers in the care of patients 8. Beam EL, Schwedhelm S, Boulter K, Kratochvil C, Lowe J, Hewlett A, et al. Personal
with highly infectious diseases is needed. An expert consortium protective equipment processes and rationale for the Nebraska biocontainment
should be formed to focus on agreeing to a standard step-by-step unit during the 2014 activations for Ebola virus disease. Am J Infect Control
2015;44:340-2.
process, but also identifying essential safety concepts in the event 9. Beam EL, Gibbs SG, Hewlett AL, Iwen PC, Nuss SL, Smith PW. Clinical challenges
that a breach, contamination situation, or unexpected clinical in isolation care: safe practices for nurses at the bedside. Am J Nurs 2015;115:
event warrants a slight change in process. The standard should 44-9.
include the use of PPE for special circumstances, such as chemo- Conflicts of interest: None to report.
therapy administration,6 patient transportation of an isolation
patient for ancillary medical services, and visitors of isolation Elizabeth L. Beam, PhD, RN*
patients.7 A specific list of inappropriate behaviors would also be 985330 Nebraska Medical Center, University of Nebraska Medical
helpful for clinicians, such as wearing isolation gowns for Center College of Nursing, Omaha, NE
warmth or wearing surgical PPE in the cafeteria or public hospital
areas. * Address correspondence to Elizabeth L. Beam, PhD, RN, 985330
The current Centers for Disease Control and Prevention guid- Nebraska Medical Center, University of Nebraska Medical Center
ance for prevention of health care–associated infections for donning College of Nursing, Omaha, NE 68198-5330.
and doffing sequence of PPE present critical concerns for clini- E-mail address: ebeam@unmc.edu.
cians and health care workers (http://www.cdc.gov/hai/pdfs/ppe/
PPE-Sequence.pdf). The concerns relate to safe doffing processes http://dx.doi.org/10.1016/j.ajic.2016.05.040
used after patient care or other use of PPE. In example 1, the facial
PPE (goggles or face shield) is removed before the gown is removed.
Você também pode gostar
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryNo EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryNota: 3.5 de 5 estrelas3.5/5 (231)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)No EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Nota: 4.5 de 5 estrelas4.5/5 (119)
- Never Split the Difference: Negotiating As If Your Life Depended On ItNo EverandNever Split the Difference: Negotiating As If Your Life Depended On ItNota: 4.5 de 5 estrelas4.5/5 (838)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaNo EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaNota: 4.5 de 5 estrelas4.5/5 (265)
- The Little Book of Hygge: Danish Secrets to Happy LivingNo EverandThe Little Book of Hygge: Danish Secrets to Happy LivingNota: 3.5 de 5 estrelas3.5/5 (399)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyNo EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyNota: 3.5 de 5 estrelas3.5/5 (2219)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeNo EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeNota: 4 de 5 estrelas4/5 (5794)
- Team of Rivals: The Political Genius of Abraham LincolnNo EverandTeam of Rivals: The Political Genius of Abraham LincolnNota: 4.5 de 5 estrelas4.5/5 (234)
- The Emperor of All Maladies: A Biography of CancerNo EverandThe Emperor of All Maladies: A Biography of CancerNota: 4.5 de 5 estrelas4.5/5 (271)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreNo EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreNota: 4 de 5 estrelas4/5 (1090)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersNo EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersNota: 4.5 de 5 estrelas4.5/5 (344)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceNo EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceNota: 4 de 5 estrelas4/5 (890)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureNo EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureNota: 4.5 de 5 estrelas4.5/5 (474)
- The Unwinding: An Inner History of the New AmericaNo EverandThe Unwinding: An Inner History of the New AmericaNota: 4 de 5 estrelas4/5 (45)
- The Yellow House: A Memoir (2019 National Book Award Winner)No EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Nota: 4 de 5 estrelas4/5 (98)
- Bell-John Deere 315 SK Workshop Service Repair PDFDocumento733 páginasBell-John Deere 315 SK Workshop Service Repair PDFRonaldWiseman52% (27)
- HT & PWHT JsaDocumento3 páginasHT & PWHT JsaNature BeautiesAinda não há avaliações
- 2.0 - Personal Protective Equipment v3.0 EnglishDocumento14 páginas2.0 - Personal Protective Equipment v3.0 EnglishkaiserfaheemAinda não há avaliações
- Curing Compound ApplicationDocumento3 páginasCuring Compound Applicationmoytabura96Ainda não há avaliações
- HSE Requirements For Contracts 1Documento31 páginasHSE Requirements For Contracts 1bibin0474Ainda não há avaliações
- (En) Jasic Evo20 Tig Acdc LCD User Manual Tig200pacdc PFC (E2s23) Tig200pacdc (E2s13)Documento61 páginas(En) Jasic Evo20 Tig Acdc LCD User Manual Tig200pacdc PFC (E2s23) Tig200pacdc (E2s13)sotirisinAinda não há avaliações
- Mellitah Oil & Gas BV: Libyan BranchDocumento8 páginasMellitah Oil & Gas BV: Libyan BranchSamerAinda não há avaliações
- CBC Food Beverages Services NC IIDocumento63 páginasCBC Food Beverages Services NC IINolram Leuqar86% (7)
- 064 Method Statement For Construction of Air-Cooled CondensDocumento13 páginas064 Method Statement For Construction of Air-Cooled CondensMohd NasharuddinAinda não há avaliações
- 3700-AC P2 Operacion y PartesDocumento80 páginas3700-AC P2 Operacion y PartesParedes Miler100% (4)
- For Information For Review For Approval For Construction As-BuiltDocumento20 páginasFor Information For Review For Approval For Construction As-BuiltUtku Can KılıçAinda não há avaliações
- JCI Standards Only 6th Ed HospitalDocumento11 páginasJCI Standards Only 6th Ed HospitalAnonymous CqAPN7PJ8Ainda não há avaliações
- LET Research1Documento9 páginasLET Research1Jovenil BacatanAinda não há avaliações
- The Prevalence of Vitamin D Deficiency in Patients With Myocardialinfarction 2329 9517 1000307Documento1 páginaThe Prevalence of Vitamin D Deficiency in Patients With Myocardialinfarction 2329 9517 1000307Anonymous CqAPN7PJ8Ainda não há avaliações
- Early Treatment Dmt2Documento8 páginasEarly Treatment Dmt2Aulia CandraAinda não há avaliações
- CA ReviewDocumento2 páginasCA ReviewAnonymous CqAPN7PJ8Ainda não há avaliações
- CA (Cellular Alterations) : Myocardial ToxicityDocumento4 páginasCA (Cellular Alterations) : Myocardial ToxicityAnonymous CqAPN7PJ8Ainda não há avaliações
- Hospital Surface Disinfection: Need, Gaps, Challenges and Management For "Basin and Mop" MethodDocumento5 páginasHospital Surface Disinfection: Need, Gaps, Challenges and Management For "Basin and Mop" MethodAnonymous CqAPN7PJ8Ainda não há avaliações
- CA ReviewDocumento2 páginasCA ReviewAnonymous CqAPN7PJ8Ainda não há avaliações
- 3 Point GaitDocumento4 páginas3 Point GaitAnonymous CqAPN7PJ8Ainda não há avaliações
- CA (Cellular Alterations) : Myocardial ToxicityDocumento4 páginasCA (Cellular Alterations) : Myocardial ToxicityAnonymous CqAPN7PJ8Ainda não há avaliações
- ReflectionDocumento1 páginaReflectionAnonymous CqAPN7PJ8Ainda não há avaliações
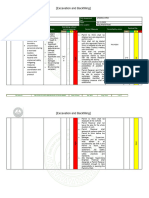
- UNIMAC - KKR - RA-031 - Excavation and BackfillingDocumento17 páginasUNIMAC - KKR - RA-031 - Excavation and Backfillingrustam khanAinda não há avaliações
- ARM BARRIER Part 1 Manual Installation& OperationDocumento54 páginasARM BARRIER Part 1 Manual Installation& OperationSVS SVSAinda não há avaliações
- AGRI-VAC Model 5614 To 7816 Operator'S Manual and Parts BookDocumento94 páginasAGRI-VAC Model 5614 To 7816 Operator'S Manual and Parts BookGiri DanuartoAinda não há avaliações
- DIESEL GENERATOR MANUALDocumento32 páginasDIESEL GENERATOR MANUALRui FerreiraAinda não há avaliações
- Semstone 145: Selection & Specification DataDocumento4 páginasSemstone 145: Selection & Specification DataSHAIK ASIMUDDINAinda não há avaliações
- OHAS UGRD ENG6201 Occupational Health and Safety MIDTERM 1Documento43 páginasOHAS UGRD ENG6201 Occupational Health and Safety MIDTERM 1Not Racist By The WayAinda não há avaliações
- DMAIC Approach To Improve On Safety Performance Using Safety Management System in Kuwait International AirportDocumento10 páginasDMAIC Approach To Improve On Safety Performance Using Safety Management System in Kuwait International AirportZelalem EjiguAinda não há avaliações
- MasterSeal 550 SDS 2027551Documento9 páginasMasterSeal 550 SDS 2027551Wahab SajjadAinda não há avaliações
- Lifesaving Rules BookletDocumento20 páginasLifesaving Rules BookletDLPS HSEAinda não há avaliações
- MTK 1043 Smaw 1Documento22 páginasMTK 1043 Smaw 1Mohd Dinie HafiqAinda não há avaliações
- Silver Solder MSDSDocumento4 páginasSilver Solder MSDSsalcabesAinda não há avaliações
- LA60341-CPC Circulation Oil R32 - R150 (v5.3)Documento7 páginasLA60341-CPC Circulation Oil R32 - R150 (v5.3)Миша ЖигалкинAinda não há avaliações
- 0059 Lca Safety Inspection ChecklistDocumento3 páginas0059 Lca Safety Inspection ChecklistIvanna Celeste Duran RojasAinda não há avaliações
- Risk Assessment Format OCLDocumento4 páginasRisk Assessment Format OCLThusithaAinda não há avaliações
- Duraguard MsdsDocumento1 páginaDuraguard MsdsSantosh Kumar GoudaAinda não há avaliações
- SBF PHILIPPINES DRILLING RESOURCES CORP. HAZARD IDENTIFICATIONDocumento11 páginasSBF PHILIPPINES DRILLING RESOURCES CORP. HAZARD IDENTIFICATIONMarson Apsay100% (1)
- Mcdo BrochureeeDocumento4 páginasMcdo BrochureeeCherry Blummhea MonteverdeAinda não há avaliações
- Rope Access IntroDocumento21 páginasRope Access IntroWan Rozaidi100% (1)
- OSHMS360 Webinar COSH OutlineDocumento4 páginasOSHMS360 Webinar COSH OutlineMichael NullasAinda não há avaliações