Escolar Documentos
Profissional Documentos
Cultura Documentos
Fetal Urinary Tract Anomalies: Review of Pathophysiology, Imaging, and Management
Enviado por
Anonymous wdmpgxTítulo original
Direitos autorais
Formatos disponíveis
Compartilhar este documento
Compartilhar ou incorporar documento
Você considera este documento útil?
Este conteúdo é inapropriado?
Denunciar este documentoDireitos autorais:
Formatos disponíveis
Fetal Urinary Tract Anomalies: Review of Pathophysiology, Imaging, and Management
Enviado por
Anonymous wdmpgxDireitos autorais:
Formatos disponíveis
Pe d i a t r i c I m a g i n g • R ev i ew
Mileto et al.
Imaging of Fetal Urinary Tract Anomalies
Pediatric Imaging
Review
Downloaded from www.ajronline.org by Tufts University on 02/16/18 from IP address 130.64.11.153. Copyright ARRS. For personal use only; all rights reserved
Fetal Urinary Tract Anomalies:
FOCUS ON:
Review of Pathophysiology,
Imaging, and Management
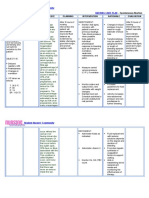
Achille Mileto1 OBJECTIVE. Common fetal anomalies of the kidneys and urinary tract encompass a
Malak Itani1 complex spectrum of abnormalities that can be detected prenatally by ultrasound. Common
Douglas S. Katz 2 fetal anomalies of the kidneys and urinary tract can affect amniotic fluid volume production
Joseph R. Siebert 3 with the development of oligohydramnios or anhydramnios, resulting in fetal pulmonary hy-
Manjiri K. Dighe1 poplasia and, potentially, abnormal development of other fetal structures.
CONCLUSION. We provide an overview of common fetal anomalies of the kidneys and
Theodore J. Dubinsky 1
urinary tract with an emphasis on sonographic patterns as well as pathologic and postnatal
Mariam Moshiri1 correlation, along with brief recommendations for postnatal management. Of note, we render
Mileto A, Itani M, Katz DS, et al. an updated classification of fetal abnormalities of the kidneys and urinary tract based on the
presence or absence of associated urinary tract dilation. In addition, we review the 2014 clas-
sification of urinary tract dilation based on the Linthicum multidisciplinary consensus panel.
he development of the fetal uri- well as pathologic and postnatal correlation,
T nary tract is a complex process
and is, therefore, associated with
an inherent substantial risk of
and we briefly discuss postnatal management.
In addition, we provide an updated classifi-
cation of fetal abnormalities of the kidneys
congenital defects. Fetal renal anomalies rep- and urinary tract based on the presence or ab-
resent approximately 20% of all fetal congeni- sence of associated urinary tract dilation. We
tal defects and are seen in 3–4% of pregnan- also review the 2014 classification of urinary
Keywords: amniotic fluid, congenital abnormalities, cies. The frequency of prenatally detected tract dilation based on the Linthicum multi-
cystic renal disease, fetal, ultrasound, urinary tract,
urinary tract dilation
common fetal anomalies of the kidneys and disciplinary consensus panel.
urinary tract is approximately 0.1–2.3% [1, 2].
doi.org/10.2214/AJR.17.18371 Urine produced by the fetal kidneys is a Organogenesis
major contributor to the volume of amniot- The urogenital system in the fetus origi-
Received April 12, 2017; accepted after revision
ic fluid in the second and third trimesters of nates from the intermediate mesoderm, which
October 27, 2017.
pregnancy. Therefore, any structural or func- develops into three early renal structures: the
Based on a presentation at the Radiological Society of tional defects in the fetal urinary tract can pronephros, the mesonephros, and the meta-
North America 2015 annual meeting, Chicago, IL. result in a substantial reduction of amniotic nephros. Of these structures, the pronephros
1
fluid volume (oligohydramnios or anhydram- is a transient excretory structure. The meso-
Department of Radiology, University of Washington
School of Medicine, Box 357115, 1959 NE Pacific St,
nios), which, in turn, can cause fetal pulmo- nephros regresses in male fetuses and gives
Seattle, WA 98195. Address correspondence to nary hypoplasia, as well as abnormal devel- rise to some parts of the genital organs in fe-
A. Mileto (amileto@uw.edu). opment of several other fetal structures [3]. male fetuses. The metanephros gives rise to
2
Fetal oligohydramnios or anhydramnios is nephron units of the fetal kidneys. The ure-
Department of Radiology, NYU Winthrop Hospital,
associated with a poor outcome, with a re- teric buds give rise to the renal collecting sys-
Mineola, NY.
ported mortality rate of 30–60% [4]. tems, the major and minor calyces, the renal
3
Department of Pathology, University of Washington, Accurate diagnosis of common fetal anom- pelves, and the renal collecting tubules. The
Seattle, WA. alies of the kidneys and urinary tract anoma- urogenital sinus gives rise to the urinary blad-
Supplemental Data
lies is essential for parental counseling, ap- der. The fetal kidneys develop in the sacral re-
Available online at www.ajronline.org. propriate pregnancy management, and proper gion and then migrate to the renal fossa.
delivery planning via a multidisciplinary The fetal kidneys begin to make urine by
AJR 2018; 210:1–12 team approach, in which the radiologist plays 10 weeks of gestation and become function-
a major role. In this article, we review imag- al by 12 weeks of gestation. By 14 weeks of
0361–803X/18/2105–1
ing of fetal genitourinary tract abnormalities gestation, they become a major contributor to
© American Roentgen Ray Society with an emphasis on sonographic patterns, as the volume of amniotic fluid, with a minor
AJR:210, May 2018 1
Mileto et al.
Downloaded from www.ajronline.org by Tufts University on 02/16/18 from IP address 130.64.11.153. Copyright ARRS. For personal use only; all rights reserved
A B
Fig. 1—Second-trimester female fetus with normal kidneys.
A, and B,Long-axis (A) and short-axis (B) ultrasound images show normal kidneys (between calipers, A) with
early corticomedullary differentiation. Note normal pelvicalyceal systems and renal pelves (arrowheads, B).
Aorta (a) and inferior vena cava (v) are seen anterior to vertebral body (b).
C, Coronal T2-weighted MR image shows normal position and appearance of fetal kidneys. RK = right kidney,
LK = left kidney.
C
contribution from the lungs, which produce absence of amniotic fluid, MRI is an excel- Abnormal Renal Number: Renal Agenesis
approximately one-third of the fluid. Neph- lent diagnostic adjunct because of its abili- Renal agenesis refers to congenital ab-
ron development in the kidney continues un- ty to provide high-quality tissue contrast and sence of the kidney, which can be bilateral or
til birth. The number of nephrons then re- wider anatomic coverage, especially in com- unilateral. Bilateral renal agenesis is a lethal
mains static, although they increase in size plex anomalies. The volume of amniotic flu- anomaly, occurring in 0.1–0.3 of 1000 live
after birth [1]. id, fetal position, and maternal conditions are births [9]. In a parent with a unilateral kid-
typically not limitations of MRI, in contrast ney, the fetus has a 1% chance of developing
Imaging and Normal Anatomy to sonography. The normal fetal renal paren- bilateral agenesis.
Ultrasound is the primary imaging mo- chyma is of intermediate signal intensity on Bilateral renal agenesis can be an isolat-
dality for the assessment of the fetal urinary T2-weighted images, whereas the renal col- ed anomaly but can also be seen in associa-
tract. The fetal kidneys can be identified by lecting systems are of higher signal intensity. tion with other fetal syndromes and genetic
approximately 10 weeks of gestation, espe- The adrenal glands are low in signal inten- anomalies, including cardiovascular (15%)
cially on transvaginal sonography. In the sity in the suprarenal fossae. The fetal uri- and musculoskeletal (40%) malformations,
transverse plane, the fetal kidneys appear as nary bladder is a high-signal-intensity round such as clubbed feet. Less commonly seen
round hyperechoic structures adjacent to the or ovoid structure in the pelvis [8]. associations include diaphragmatic hernia,
fetal spine (Fig. 1). In the longitudinal plane, tracheoesophageal fistula, hydrocephalus,
the fetal kidneys are elliptical. The kidneys Classification of Fetal myelomeningocele, and duodenal atresia.
continue to grow throughout pregnancy, with Genitourinary Anomalies The occurrence of renal agenesis with other
the renal length remaining directly propor- Common fetal anomalies of the kidneys anomalies has been described as the VAC-
tional to the gestational age. In later gesta- and urinary tract encompass a broad spec- TERL association, which refers to the asso-
tion, the renal medullary pyramids appear trum of conditions with complex pathophysi- ciation of vertebral anomalies, anal atresia,
more hypoechoic compared with the renal ology and diverse clinical outcome and man- cardiac defects, tracheoesophageal fistula or
cortexes. The ratio of fetal renal circumfer- agement implications [9]. Assessment of fetal esophageal atresia, renal and radial anoma-
ence to abdominal circumference remains at urinary tract anomalies can be approached lies, and limb defects [10, 11].
approximately 0.3 throughout the pregnancy in various ways. One method entails divid- Fetuses with bilateral renal agenesis dis-
[5, 6]. The adrenal glands are seen superior ing the anomalies by their resultant chang- play the Potter phenotypical sequence, which
to the kidneys. In the longitudinal plane, they es in renal size, whereas another approach is characterized by a receding chin, low-set
are triangular, whereas they appear as oval distributes them into categories according ears, widely spaced eyes with epicanthal
or tubular in the transverse plane. The adre- to the presence or absence of associated uri- folds, and a broad nasal bridge. These facial
nal medulla appears hyperechoic, surround- nary tract dilation. In this article, we follow features are due to the paucity of amniot-
ed by hypoechoic cortex [5, 6]. The fetal uri- the latter approach, because it is currently the ic fluid, which in normal development cush-
nary bladder is seen at approximately 10–12 most commonly used classification. ions the fetus’s face from direct trauma by the
weeks of gestation as a small fluid-filled uterine walls [12, 13]. The absence of both
structure in the pelvis. The normal urinary Nonhydronephrotic Renal Anomalies: No kidneys and renal arteries can be detected in
bladder voiding cycle is approximately every Urinary Tract Dilation the paravertebral regions at ultrasound (Fig.
55–155 minutes [7]. These structural abnormalities do not result 2). In an attempt to occupy the uninhabited
When additional information is needed, in dilation of the renal pelvis. Most of these renal fossae, the adrenal glands stretch lon-
or when ultrasound is limited because of the anomalies affect renal shape and position [5]. gitudinally, taking an elongated shape (i.e.,
2 AJR:210, May 2018
Imaging of Fetal Urinary Tract Anomalies
aging feature can be of clinical usefulness in
predicting the absence of the other kidney.
Abnormal Renal Position
Renal ectopia refers to any circumstance
in which the kidney is not positioned in the
Downloaded from www.ajronline.org by Tufts University on 02/16/18 from IP address 130.64.11.153. Copyright ARRS. For personal use only; all rights reserved
renal fossa. It is between the sixth and the
ninth weeks of gestation that the metaneph-
ros ascend to the renal fossae at the level of
the 12th thoracic vertebra [18]. Ectopia of the
kidneys, which occurs as a consequence of al-
teration at any stage of renal ascent, is usual-
ly defined as simple renal ectopia (as opposed
A B to cross-fused renal ectopia, which is covered
in the next section), because this condition is
the consequence of either a defective ascent,
most commonly resulting in a pelvic kidney
or, much less commonly, in an excessive cau-
docranial ascent into the thorax [19]. Simple
renal ectopia is seen in 1/1200 births. If not
promptly suspected, this anomaly can simu-
late unilateral renal agenesis [19].
Renal ectopia can be associated with other
genitourinary tract anomalies, including ob-
structive uropathy and reflux. Additionally,
similar to renal agenesis, other developmental
anomalies of the gynecologic, gastrointesti-
nal, cardiovascular, and musculoskeletal sys-
C D tems can also occur [14, 20, 21]. In cases of
Fig. 2—Male fetus with bilateral renal agenesis. renal ectopia, MRI can be useful to promptly
A, Oblique coronal gray-scale ultrasound image through abdomen and pelvis obtained at 23 weeks’ gestation
shows absence of both kidneys in paravertebral regions. Note adrenal glands (arrowheads).
locate the ectopic kidney and to differentiate
B, Coronal oblique color Doppler image through abdomen and pelvis obtained at 23 weeks’ gestation shows this condition from renal agenesis [21].
agenesis of both renal arteries.
C, Axial color Doppler image through fetal pelvis obtained at 29 weeks’ gestation shows lack of visualization of Abnormal Renal Size, Shape, or Position
urinary bladder due to absence of urine.
D, Postnatal ultrasound obtained at 1 day of life shows straightening of right adrenal posterior to hepatic As opposed to simple renal ectopia, fusion
parenchyma (arrowheads), compatible with lying-down adrenal gland. Neonate died at day 2 of life because of and malposition of the two kidneys can oc-
pulmonary hypoplasia. cur because of either abnormal position of
the umbilical artery or an aberrant ureteral
the lying-down appearance). In some cases, plasia is the main cause of death of newborns bud. Under such circumstances, the kidneys
the elongated adrenal glands can assume an with renal agenesis and the Potter sequence assume various abnormal shapes, including
ovoid shape, simulating the appearance of [14, 15]. Hypoplasia or absence of the uri- horseshoe kidney, crossed-fused renal ecto-
the kidneys. Severe oligohydramnios is usu- nary bladder is another expected feature in pia, and pancake kidney [22].
ally seen in the setting of bilateral renal agen- the setting of bilateral renal agenesis [1, 16]. Horseshoe kidney is the most common
esis. Oligohydramnios tends to be more evi- Unilateral renal agenesis is 4–20 times fusion abnormality, estimated at a rate of
dent after 16 weeks of gestation, because the more common than bilateral renal agenesis 1/500 births (i.e., approximately 90% of all
initial urine production by the placenta pro- and conveys a favorable prognosis [14, 15]. In renal morphologic abnormalities). Horse-
gressively declines by then, without viable the case of unilateral agenesis, the empty re- shoe configuration results from two normal-
kidneys being able to undertake this function. nal fossa with absence of the ipsilateral renal ly functioning kidneys positioned on either
Pulmonary hypoplasia with a small tho- artery can be revealed by ultrasound and col- side of the midline and are connected by a
rax is another feature commonly associated or Doppler imaging. A hypertrophied contra- parenchymal or fibrotic bridge. Most com-
with bilateral renal agenesis and the Potter lateral kidney supplied by a normal renal ar- monly, the parenchymal or fibrotic isthmus
sequence [12, 13]. Although the pathophysi- tery is usually seen (Fig. S1 can be viewed in connects the lower renal poles, with a con-
ologic mechanism causing pulmonary hypo- the AJR electronic supplement to this article, nection between the upper renal poles be-
plasia has not been entirely elucidated, to our available at www.ajronline.org). Cho and col- ing much less common [22, 23]. A horse-
knowledge, it is hypothesized that the absent leagues [17] suggested that, when the compen- shoe kidney can be challenging to diagnose
flow of amniotic fluid into the lungs along satory hypertrophy of the contralateral kidney at prenatal ultrasound because only a thin
with limited space in the fetal thorax impairs results in anteroposterior-to-transverse diam- parenchymal band is usually present (Fig.
pulmonary development. Pulmonary hypo- eter ratio greater than or equal to 0.9, this im- S2 can be viewed in the AJR electronic sup-
AJR:210, May 2018 3
Mileto et al.
plement to this article, available at www. Classification of Urinary Tract Dilation agement was also developed [27]. Overall,
ajronline.org). Urinary tract dilation can be Historically, there has been a lack of cor- the 2014 Linthicum recommendations pro-
seen in one or both renal moieties. relation between prenatal and postnatal ul- vide added value because they are based on
Cross-fused renal ectopia is the second trasound findings of urinary tract dilatation, a thorough analysis of the existing evidence-
most common fusion anomaly, with a fre- with inconsistency in description, classifica- based literature, as well as the opinion of au-
quency of 1/7500 births [22]. This condi- tion, and grading, which ultimately affects thorities reflecting the accepted standard of
Downloaded from www.ajronline.org by Tufts University on 02/16/18 from IP address 130.64.11.153. Copyright ARRS. For personal use only; all rights reserved
tion refers to fusion of the two kidneys on clinical assessment and treatment planning. care in clinical practice.
the same side of the spine. The ureter of For this reason, a consensus meeting on uri-
the ectopic kidney crosses the midline and nary tract dilation classification system was Renal Pelvis Obstruction
joins the urinary bladder at the orthotopic convened in March 2014 in Linthicum, MD, Obstruction of the renal pelvis at the level
site. Depending on the fusion site and final that was attended by representatives from of the ureteropelvic junction is the most ac-
renal shape, different variants of crossed- eight major scientific societies [27]. The con- cepted explanation for fetal urinary tract di-
fused renal ectopia are described in the lit- sensus panel had a twofold objective: to pro- lation [14, 16, 29]. Of note, obstruction of the
erature, including type A (inferior crossed pose a unified description of urinary tract ureteropelvic junction is estimated to repre-
fusion), type B (sigmoid kidney), type C, dilation prenatally and postnatally and to de- sent approximately 50% of all urinary tract
(lump kidney), type D, (disc kidney), type velop a standardized framework for prenatal abnormalities seen in newborns [14]. This is
E, (L-shaped kidney), and type F (superior- evaluation of isolated urinary tract dilatation usually a sporadic unilateral (90% of cases)
ly crossed-fused). Type A is the most com- based on ultrasound findings, which can be anomaly due to aberrant collagen or fibrotic
monly seen variant, where there is fusion applied in the postnatal period. bands at the level of the ureteropelvic junc-
between the upper pole of the cross-fused In an attempt to avoid confusion, the con- tion. However, kinking of the ureteral course,
ectopic kidney (located more inferiorly rela- sensus panel agreed on specific terminology the presence of ureteral valves, aberrant ves-
tive to the other kidney) and the lower pole to be used. Of note, the consistent adoption sels, and abnormal insertion of the ureter
of the other orthotopic kidney (located in a of the term “urinary tract dilation” was rec- with varying configurations of the pelviure-
more superior position) [22, 23]. ommended, whereas the use of other com- teral outlet have also been described as pos-
Pancake kidney is an extremely rare ab- monly used clinical terms (e.g., “hydrone- sible causes. In a minority of cases (10–30%),
normality of renal shape caused by complete phrosis,” “pyelectasis,” and “pelviectasis”) obstruction of the ureteropelvic junction can
fusion of the two kidneys in the pelvis, with was discouraged [27]. In addition, owing to be bilateral, often in association with other
two distinct collecting systems joining the the emerging substantial variability among nongenitourinary abnormalities (e.g., esoph-
urinary bladder on either side of the mid- grading systems traditionally used—descrip- ageal atresia, Hirschsprung disease, and im-
line [24]. Occasionally, the pancake kidney tive (e.g., mild, moderate, or severe), quantita- perforate anus) [14].
is drained by a single ureter [25, 26]. tive (e.g., grades 1–5 based on anteroposteri- Fetal ultrasound shows dilation of the re-
or renal pelvic diameter), or semiquantitative nal pelvis with or without dilation of renal
Hydronephrotic Renal Disease: (e.g., the Society for Fetal Urology system)— calyces; the degree of dilation depends on
Urinary Tract Dilation the consensus panel underscored the need the type and severity of the obstruction. In
Dilation of the urinary tract is seen in for using a single widely accepted method high-grade severe obstruction, development
1–2% of all pregnancies and is estimated to to be used for describing pre- and postnatal of perirenal urinomas and ascites can be ob-
affect approximately 40,000–80,000 new- ultrasound findings. Therefore, the panel es- served. This explains why both oligohydram-
borns in the United States every year [27]. tablished a standardized checklist of sono- nios and polyhydramnios can be seen in the
Although urinary tract dilation is only tran- graphic features to report anteroposterior re- setting of ureteropelvic junction obstruction;
sient or physiologic in 50–70% of cases, it nal pelvic diameter measured on transverse however, oligohydramnios is exceedingly
can also reflect a wide variety of underly- images at maximal diameter of the intrare- rare. If left untreated, long-standing obstruc-
ing pathologic conditions. The latter in- nal pelvis; calyceal dilation, either central tion can lead to increased echogenicity and
clude ureteropelvic junction obstruction (major) or peripheral (minor); parenchymal cystic changes associated with atrophy of the
(10–30%), vesicoureteral reflux (10–40%), thickness, to be reported with a subjective renal parenchyma at ultrasound [14, 16, 29].
ureterovesical junction obstruction or mega- assessment; parenchymal appearance, in- Overall, the prognosis of ureteropelvic junc-
ureter (5–15%), multicystic dysplastic kid- cluding the evaluation of echogenicity, the tion obstruction depends on many factors,
ney (MCDK) disease (2–5%), and posteri- presence of cortical cysts, and corticomedul- including the presence or absence of other
or urethral valves (1–5%). Less common are lary differentiation; ureter description, in- anomalies, amniotic fluid volume, the pres-
ectopic ureter and ureterocele in the setting cluding transient visualization and normal ence or absence of a urinoma, and cystic dys-
of collecting system duplication, polycystic versus abnormal dilation; and urinary blad- plasia of the ipsilateral kidney [14, 16, 29].
kidney disease, and prune-belly syndrome der description, including the assessment of
[28]. Prenatal identification of the aforemen- wall thickness, and the presence of a uretero- Ureteral Obstruction
tioned conditions is of critical importance celes or posterior urethral valves [27]. Dilation of the urinary tract can also be due
to prevent the development of complications The 2014 Linthicum consensus panel also to obstruction at the level of the ureterovesical
(e.g., urinary tract infection, renal calculi, issued a risk stratification model to be used junction. This condition, which is more com-
and renal failure) and to allow planning of for both pre- and postnatal urinary tract dila- mon among male than female patients, has a
postnatal management strategies in a timely tion [27]. On the basis of the aforementioned familial pattern of inheritance and is usually
manner [28]. risk stratification models, a scheme for man- due to occurrence of megaureter or stenosis of
4 AJR:210, May 2018
Imaging of Fetal Urinary Tract Anomalies
the ureterovesical junction as a result of dys- tients with primary megaureter can be man- results, causing failure of the continence
plastic or aberrant smooth muscle with fibro- aged conservatively, because this anomaly mechanism [33–35]. Although vesicoureteral
sis. Megaureter, by definition, is a dilated ure- usually resolves spontaneously by the age of reflux can be also seen in the setting of com-
ter with or without coexistent dilation of the 7 years. If the anomaly does not resolve, in plex genitourinary abnormalities (e.g., du-
renal pelvis and calyces and refers to a con- the minority of such patients the treatment is plication of the collecting system), it is more
genital anomaly of the ureterovesical junction. surgery, with resection of the aperistaltic seg- commonly an isolated condition.
Downloaded from www.ajronline.org by Tufts University on 02/16/18 from IP address 130.64.11.153. Copyright ARRS. For personal use only; all rights reserved
Primary megaureter, also known as congen- ment and ureteral reimplantation. The retrograde flow of urine into the ure-
ital megaureter, is bilateral in 20% of cases Other causes of obstruction of the ure- ters and kidneys (the latter is termed “in-
with contralateral genitourinary abnormal- terovesical junction include an ectopic ure- trarenal reflux”) increases the risk of upper
ities in 5% of cases. Although this anomaly ter with or without a ureterocele. An ectopic urinary tract infection caused by ascending
can be identified during the fetal period, de- ureter is the result of the aberrant migration bacteria and can result in renal parenchymal
finitive diagnosis of primary megaureter can of the ureteral bud, usually with caudal ec- scarring and dysfunction. Early diagnosis of
be made only postnatally [30]. Primary mega- topia of the ureteral insertion, which can be vesicoureteral reflux is important to prevent
ureter can be classified into three subcatego- into the lower portion of the urinary blad- renal damage. Vesicoureteral reflux accounts
ries: obstructive, refluxing, and nonrefluxing der, urethra, vestibule, or vagina in female for up to 40% of cases of urinary tract dila-
unobstructed. The obstructive megaureter patients, or in the seminal vesicles, vas def- tion detected prenatally at ultrasound [31]. In
is characterized by ureteral dilation proxi- erens, or ejaculatory ducts in male patients. the absence of other anomalies, prenatal doc-
mal to a short aperistaltic juxtavesical por- Often, especially if the ectopic ureter is as- umentation of urinary tract dilation should
tion of the ureter with a normal urinary blad- sociated with a duplicated ureter, imaging raise the suspicion for vesicoureteral reflux,
der. The refluxing megaureter is usually due shows a thin-walled cystic structure arising therefore warranting postnatal evaluation.
to a small or absent portion of the intravesical from the distal portion of the ureter project- Precise grading of vesicoureteral reflux is
ureter, whereas the nonrefluxing unobstructed ing into the urinary bladder lumen (i.e., ure- based on voiding cystourethrography, which
megaureter refers to lack of obstruction or re- terocele) [14, 31]. Postnatal MR urography should be promptly performed after the first
flux with dilatation of the ureter proximal to can be useful to exactly depict the course episode of urinary tract infection. According
the level of the urinary bladder [14, 31]. The and termination of the ectopic ureter within to the International Reflux Committee Study
nonrefluxing unobstructed variant is the most a ureterocele [21]. System [36], vesicoureteral reflux is classi-
common subtype (Fig. 3). fied as grade 1 when the backward urine flow
In all cases of ureteral obstruction, with or Vesicoureteral Reflux involves the ureter only; grade 2 when ure-
without megaureter, ultrasound shows a dilat- Vesicoureteral reflux consists of the back- ter and renal collecting system are involved,
ed fetal ureter proximal to the ureterovesical ward flow of urine from the urinary bladder but without dilatation; grade 3 when there is
junction. The dilated ureter is displayed as an into the ureters and kidneys due to abnormal moderate dilation of the ureter and renal col-
anechoic elongated structure with a tortuous maturation of the vesicoureteral antireflux lecting system, with no or slight blunting of
course, which can be followed throughout its mechanism [33]. Normally, a 7- to 12-mm the caliceal fornices; grade 4 when there is
entire length from the renal pelvis to the ure- portion of the distal ureter enters the urinary moderate dilation of the ureter and renal col-
terovesical junction [31]. Postnatal evaluation bladder wall obliquely at the vesicoureteral lecting system with an associated tortuous
with MRI may be warranted to better char- junction, thus serving as a continence valve, course, and complete blunting of the caliceal
acterize the type of megaureter, as well as to to prevent backward flow of urine from the fornices with maintenance of papillary im-
monitor dilation of the pelvicalyceal system urinary bladder. If the maturation of the ure- pressions; and grade 5 when there is marked
and renal parenchymal abnormalities (e.g., terovesical junction is incomplete, an abnor- dilation of the ureter and renal collecting
cortical thinning and scarring) [32]. Most pa- mally short intravesical ureteral segment system with an associated tortuous course,
A B
Fig. 3—3-month-old boy with primary megaureter.
A, Sagittal ultrasound image of right kidney (between calipers) shows parenchymal thinning (arrowheads) and pelvicalyceal dilation.
B, Sagittal ultrasound image at level of right ureterovesical junction shows tapered narrowing of distal right ureter, consistent with primary megaureter.
AJR:210, May 2018 5
Mileto et al.
Downloaded from www.ajronline.org by Tufts University on 02/16/18 from IP address 130.64.11.153. Copyright ARRS. For personal use only; all rights reserved
A B
C D
E F
Fig. 4—Two fetuses with duplicated renal collecting systems.
A–F, Sagittal ultrasound image of left kidney (between calipers, A) and transverse image of urinary bladder (B) obtained at 18 weeks’ gestation show dilation of left
pelvicalyceal system (asterisk, A) and ureterocele in urinary bladder (arrowheads, B). Ultrasound images were obtained again at 23 weeks’ gestation (C and D). Upper
pole of left kidney (between calipers, C) shows cortical atrophy and cystic changes (arrows, C), and lower pole shows pelvicalyceal dilation (asterisks, C). Urinary bladder
ureterocele is now more conspicuous at site of ureteropelvic junction (arrowheads, D), and left ureter is dilated (between calipers, D). Postnatal sagittal ultrasound image
obtained at day 2 of life (E) shows cystic dysplasia of upper pole of left kidney (arrows, E), which is related to early high-grade in utero obstruction. There is pelvicalyceal
dilation in lower pole (asterisks, E). Ultrasound image of urinary bladder (F) shows left ureterocele Sex of fetus is unknown.
(Fig. 4 continues on next page)
6 AJR:210, May 2018
Imaging of Fetal Urinary Tract Anomalies
Downloaded from www.ajronline.org by Tufts University on 02/16/18 from IP address 130.64.11.153. Copyright ARRS. For personal use only; all rights reserved
G H
Fig. 4 (continued)—Two fetuses with duplicated renal collecting systems.
G, 2-day-old infant (sex unknown, same as in A–F). Fluoroscopic retrograde cystourethrogram shows large filling defect in urinary bladder (arrowheads), corresponding
to known ureterocele.
H, 3-month-old boy who had bilateral ureteral and collecting system duplication. Photograph of pathologic specimen is shown. Patient also had cardiofaciocutaneous
syndrome from underlying MEK2 mutation.
with complete blunting of the caliceal forni- hyperkeratosis, and ichthyosis) [31, 38, 39]. (i.e., the Weigert-Meyer rule). The upper pole
ces and papillary impressions. A critical step in renal development is rep- ureter most often terminates in a ureterocele,
Although voiding cystourethrography and resented by the encounter of the metanephric whereas vesicoureteral reflux is more common-
cystoscintigraphy have been historically blastema with the ureteral bud, with the latter ly seen in the ureter draining the lower pole re-
used to diagnose and grade vesicoureteral re- originating from the mesonephric Wolffian nal moiety, although there is variability of these
flux, contrast-enhanced sonography (also re- ducts. Normally, one ureteral bud joins the findings in individual patients [31, 38].
ferred to as “voiding urosonography”) is be- metanephric blastema, giving rise to a nor- Most commonly, ultrasound findings in-
ing increasingly adopted. Owing to advances mal kidney with a single collecting system. clude urinary tract dilation involving the up-
in tissue-harmonic and second-generation Renal duplication, which can be incomplete per pole system, with a normal appearance
ultrasound contrast agents, this technique or complete, occurs when more than one ure- of the lower pole moiety (Fig. 4). In the case
renders an accurate diagnosis and permits teral bud meets the metanephros [31, 33, 39]. of long-standing upper pole urinary tract di-
long-term follow-up of patients with vesico- Incomplete duplication is the result of bi- lation, atrophy of the upper pole renal pa-
ureteral reflux without exposure to ionizing furcation of a single ureteral bud joining the renchyma can be seen. When the complete
radiation. Ascenti and co-workers [37] re- metanephric blastema with two branches, at duplication is further complicated by devel-
ported that voiding urosonography improved either the renal pelvis or the ureter. In the opment of a ureterocele involving the upper
diagnostic accuracy for vesicoureteral reflux former case, the incomplete duplication is pole system, this ureterocele (i.e., bladder-
grading compared to cystoscintigraphy. termed a “bifid pelvis,” and in the latter case, within-bladder appearance), with varying
it is termed a “bifid ureter.” In either type of degrees of ureteral dilation, can be identified
Renal Duplication incomplete duplication, there is one ureter at imaging [14, 31, 38] (Fig. 4).
Duplication of the collecting system, distally joining the urinary bladder. In rare Fetal MRI with urographic (i.e., fast heav-
also termed “renal duplication” or “ureter- instances, one ureteral ramification can ter- ily T2-weighted multiplanar) pulse sequences
al duplication,” is a common developmental minate in a blind pouch [31, 38]. can be used to confirm the diagnosis of renal
anomaly. It is estimated to occur in approxi- Complete renal duplication occurs when two duplication, to assess the renal parenchyma
mately 1% of the newborn population and is distinct ureteral buds join a single metanephros. for concurrent dysplastic changes, and to de-
identified in 10% of children with recurrent Under this circumstance, there will be two ure- termine the level of obstruction, especially
urinary tract infections. Renal duplication is ters separately traveling from the renal pelvis in cases of ureterocele [21, 32]. Prenatal de-
more common among female than male pa- to urinary bladder. The ureter arising from the tection or high suspicion of renal collecting
tients (2:1 ratio) and is bilateral in 40% of pa- lower portion of the renal pelvis usually joins system duplication mandates further postna-
tients. This anomaly can be isolated or, much the urinary bladder orthotopically at one cor- tal imaging with ultrasound and voiding cys-
less commonly, is associated with complex ner of the vesical trigone. In contrast, the ureter tourethrography [31, 38, 39]. Postnatal MR
syndromes, including the cardiofaciocutane- originating from the upper pole of the collect- urography can be a useful complement to bet-
ous syndrome (cardiac abnormalities, cra- ing system joins the urinary bladder wall inferi- ter delineate the urinary tract anatomy, par-
niofacial features accompanied by xerosis, or and medial to the orthotopic ureteral meatus ticularly the ureteral course and insertion [32].
AJR:210, May 2018 7
Mileto et al.
Cystic Renal Disease etiology [40–42]. Among inherited renal cys- Cysts can develop both in the renal cortex
Cystic renal disease comprises a heteroge- tic diseases, the ciliopathies—also known as and medulla, while the kidney itself main-
neous group of renal parenchymal disorders hereditary defects of primary nonmotile cil- tains its excretory function (Fig. S3 can be
that can be hereditary, acquired, or develop- ia—have been increasingly implicated in re- viewed in the AJR electronic supplement to
mental in origin. In some cases, obstructive nal developmental abnormalities, including this article, available at www.ajronline.org).
uropathy can be seen in the setting of cystic ARPKD and ADPKD. Renal stigmata of cil- Oligohydramnios and a nonvisualized uri-
Downloaded from www.ajronline.org by Tufts University on 02/16/18 from IP address 130.64.11.153. Copyright ARRS. For personal use only; all rights reserved
renal disease. iopathies can be associated with hepatic (i.e., nary bladder can also be seen on imaging.
The Potter classification (Potter types I– hepatorenal cystic disease spectrum), skele- Kidneys in patients with ARPKD typically
IV) has been historically used to categorize tal, and CNS disorders [40, 41]. appear diffusely enlarged and hyperintense
the different types of cystic renal disease: on T2-weighted MR images [21]. A streaky
Potter type I, infantile polycystic kidney dis- Autosomal Recessive Polycystic Kidney Disease enhancement pattern can be seen after IV
ease, is now more commonly termed “auto- (Formerly Potter Type I) gadolinium administration. Hepatic involve-
somal recessive polycystic kidney disease” ARPKD is the most common renal paren- ment is also commonly noted with multiple
(ARPKD); Potter type II, cystic dysplas- chymal abnormality seen in utero and is among hepatic cysts [41]. As a rule of thumb, the
tic kidney disease, is now more commonly the most frequently encountered cystic diseas- degree of renal and hepatic involvement has
termed “multicystic dysplastic kidney dis- es in the newborn. This condition is caused by a an inverse relationship. Portal hypertension,
ease” (MCDK); Potter type III is now termed mutation of chromosome 6p12, causing abnor- hepatic parenchymal fibrosis, and pulmo-
“autosomal dominant polycystic kidney dis- mal ciliary signaling pathway and aberrant dif- nary hypoplasia can be observed in the set-
ease” (ADPKD); and Potter type IV is now ferentiation of the renal tubules epithelial cells. ting of ARPKD, with pulmonary hypoplasia
termed “partial or intermittent urinary out- This condition is transmitted via autosomal re- leading to a higher rate of perinatal mortal-
flow obstruction” or “obstructive dysplasia.” cessive inheritance [41]. ity. ARPKD can be diagnosed with ultra-
The Potter category system has been super- ARPKD is manifest phenotypically with sound at 16–18 weeks of gestation, but usu-
seded by differentiation of the various con- many rounded cysts, ranging in size between ally manifests itself in the third trimester.
ditions on the basis of genetic or nongenetic a few millimeters up to several millimeters. Treatment of ARPKD is supportive, with di-
A B C
D E
Fig. 5—Two fetuses with Meckel-Gruber Syndrome.
A–D, Transverse ultrasound image through abdomen obtained at 17 weeks’ gestation (A) shows bilateral enlarged kidneys with multiple
cysts. Sagittal ultrasound image (B) shows massive enlargement of right kidney, which is extending from lower chest to pelvis. There is
oligohydramnios. Transverse ultrasound image through skull (C) shows occipital encephalocele (arrowhead, C). Ultrasound shows that there
are at least 6 fingers on left hand (D). Autopsy confirmed polydactyly with rudimentary fingers. Sex of fetus is unknown.
E, 20 weeks’ gestation male fetus with Meckel-Gruber syndrome. Photograph of pathologic specimen shows marked enlargement of bilateral
kidneys with innumerable cysts.
8 AJR:210, May 2018
Imaging of Fetal Urinary Tract Anomalies
alysis and renal transplant usually required polycystin-2 affects the physiologic mecha- cluded in the Young classification; however,
later in life [14, 40, 42]. nisms of differentiation and repair of renal only the Young type 1 is recognized to exist
tubules [41]. At sonography, ADPKD in the today. In this category, the rudimental mem-
Multicystic Dysplastic Kidney Disease fetus or newborn can present with either nor- brane becomes progressively stiffer, causing
(Formerly Potter Type II) mal-appearing or hyperechoic kidneys. How- urinary bladder outlet obstruction with dis-
MCDK is among the most common causes ever, detection in adults is the most common tention of the posterior urethra (i.e., the key-
Downloaded from www.ajronline.org by Tufts University on 02/16/18 from IP address 130.64.11.153. Copyright ARRS. For personal use only; all rights reserved
of end-stage renal disease and renal failure in manifestation, when enlarged kidneys are hole appearance at ultrasound) and thick-
the newborn. This condition is thought to result noted with many cysts of varying size. He- ening of the urinary bladder wall, with or
from early ureteral or pelvoinfundibular atresia patic and seminal vesicles cysts, as well as without ureteral dilation (Fig. 6). Complica-
(at 8–10 weeks), with subsequent development intracranial aneurysms, are other common tions that can be identified at imaging include
of multiple noncommunicating cysts in the kid- features of ADPKD. Prenatal ultrasound formation of urinoma and urinary ascites, uri-
neys. At imaging, the kidneys lose their reni- screening is valuable in the diagnosis of this nothorax, peritoneal calcifications, and renal
form shape and appear as paraspinal masses condition [14, 45]. MRI is increasingly being dysplasia. Detection of a posterior urethral
containing multiple noncommunicating cysts used in patients with ADPKD to monitor re- valve warrants postnatal imaging with void-
(Fig. S4 can be viewed in the AJR electronic nal cysts and renal parenchymal volume. The ing cystourethrography. Treatment of con-
supplement to this article, available at www. latter has been advocated as a potential met- firmed posterior urethral valve requires endo-
ajronline.org). On the basis of the overall size ric to quantify disease progression [41]. scopic ablation of the membrane [31, 46, 47].
of the kidneys, this condition was initially sub- Urethral atresia refers to the congenital
categorized as Potter type IIA (i.e., enlarged) or Obstructive Dysplasia (Formerly Potter Type IV) absence of the urethra, usually observed in
type IIB (i.e., atrophic or normal). MCDK can This condition is caused by early paren- the setting of urinary bladder agenesis and
also have focal or segmental distribution pat- chymal abnormality resulting from urinary prune-belly syndrome. Posterior urethral
terns, with unilateral or bilateral (only in 20% obstruction at the ureteropelvic, ureterovesi- valves and urethral atresia are the two most
of cases) renal involvement [14]. Occasion- cal, or urinary bladder outlet levels. Although common conditions causing fetal lower uri-
ally, absence or atresia of the renal artery can this condition can mimic MCDK disease, the nary tract obstruction, which may not be
be seen. The prognosis of unilateral MCDK identification of urinary obstruction is the compatible with life, depending on the se-
is excellent, with natural involution of the af- key to the diagnosis and has critical prognos- verity and associated findings, unless an al-
fected kidney and development of compensa- tic implications. The latter depends on the ternate urinary pathway is created between
tory hypertrophy of the contralateral kidney timing of detection of the obstruction (i.e., the urinary bladder and the amniotic sac. In
[43]. Nevertheless, MCDK can be fatal when it early vs late), with long-standing obstruction this setting, urinary drainage from the uri-
involves both kidneys or when it is associated causing irreversible parenchymal damage, nary bladder through vesicocentesis or cre-
with T13 or T18 chromosomal aneuploidies or possibly complicated with urinomas, oligo- ation of an intrauterine vesicoamniotic surgi-
other complex fetal syndromes, including Ap- hydramnios, and ascites, resulting in a poor cal shunt have been advocated to bypass the
ert syndrome or Meckel-Gruber syndrome [14, prognosis. Common ultrasound findings in urethral blockage and decompress the col-
40]. In Meckel-Gruber syndrome, vermian hy- obstructive dysplasia are small echogenic yet lecting systems, thereby avoiding renal im-
poplasia, occipital encephalocele, polydactyly, reniform kidneys, with cortical cysts and oli- pairment, development of oligohydramnios,
omphalocele, oligo- to anhydramnios, inter- gohydramnios. Although this condition can and pulmonary hypoplasia [48]. Percutane-
rupted aortic arch, liver ductal plate abnormal- be an isolated anomaly, an association with ous creation of a vesicoamniotic shunt is the
ities, placentomegaly, and hypoplastic urinary cardiac abnormalities or the VACTERL se- most commonly performed procedure to by-
bladder can also be seen [14, 40, 44] (Fig. 5). quence can also be seen [14, 40]. pass the urethral obstruction [40, 49]. This
At MRI, kidneys of patients with MCDK show procedure consists of ultrasound-guided
multiple noncommunicating T2-hyperintense Urinary Bladder Outlet Obstruction placement of a double-ended pigtail cathe-
cysts of different sizes [21]. Although a mild Obstruction of the urinary bladder outlet ter (i.e., either a Harrison or Rodeck-Rock-
degree of parenchymal enhancement can be can occur as a result of many anatomic ab- et catheter) with its distal and proximal tips
seen after IV gadolinium administration, no normalities, most commonly posterior ure- within the fetal urinary bladder and amniotic
opacification of the collecting system is typi- thral valves (only in male patients), urethral cavity, respectively [49, 50]. Less common-
cally observed [32]. atresia (only in female patients), cloacal atre- ly used procedures to attempt to repair lower
sia, megacystis-microcolon-intestinal hypo- urinary tract obstruction are fetal cystosco-
Autosomal Dominant Polycystic Kidney peristalsis syndrome (typically in female pa- py with ablation of posterior urethral valves
Disease (Formerly Potter Type III) tients, although not a true obstruction), and and open fetal surgery with fetal vesicosto-
ADPKD is the most common type of cys- prune-belly syndrome (typically in male pa- my [49, 50]. Owing to the inherently highly
tic renal disease and is inherited via autoso- tients, although also not a true obstruction) invasive nature and high frequency of mater-
mal dominant trait mutations of the PKD1 [14, 31, 46, 47]. nal and fetal complications, these procedures
gene on chromosome 16p or of the PKD2 Posterior urethral valve is characterized are performed at only a few specialized cen-
gene on chromosome 4q, which cause aber- by a fibrotic diaphragm embryologically de- ters, with the yield of vesicocentesis remain-
rant production of polycystin-1 or polycys- riving from Wolffian ducts, which travels ing widely controversial and debated in the
tin-2, proteins that are responsible for cal- obliquely from the verumontanum through literature, to our knowledge [49, 50].
cium channel interactions on the surface of the prostatic portion of the urethra. Three Cloacal atresia represents a condition in
renal tubules cilia. Abnormal polycystin-1 or subtypes of posterior urethral valves were in- which the urinary, genital, and gastrointes-
AJR:210, May 2018 9
Mileto et al.
Fig. 6—Two patients
with posterior urethral
valve.
A, Second trimester
male fetus. Transverse
ultrasound image of
urinary bladder shows
dilated posterior
Downloaded from www.ajronline.org by Tufts University on 02/16/18 from IP address 130.64.11.153. Copyright ARRS. For personal use only; all rights reserved
urethral valve, which is
also known as keyhole
appearance of urinary
bladder. This is typically
seen in urinary bladder
outlet obstruction.
B, 8-day-old boy.
Photograph of postnatal
pathologic specimen
of urinary tract is
shown. Infant had
severe obstruction
from posterior urethral
valve, with subsequent
dysplasia of both
kidneys.
A B
tinal systems all open into a perineal me- alies. At ultrasound, it appears as complex uterine ischemic events (e.g., difficult labor
atus with a normal abdominal wall [31]. This solid or multicystic mass that is associated or delivery, asphyxia, or septicemia) or hem-
anomaly, which is seen exclusively in fe- with polyhydramnios [53–56]. The appear- orrhagic disorders [60]. Adrenal hemorrhage
male patients, is embryologically different ance of the mesonephric blastoma at MRI is can be seen in newborns affected by the
than urinary bladder exstrophy (which can nonspecific; however, T1-hyperintense foci Beckwith-Wiedemann syndrome, a congen-
be seen in either sex), in which persistence can be identified because of intratumoral ital overgrowth syndrome characterized by
of the rudimentary cloacal membrane affects hemorrhage. Restricted diffusion can be ob- hemihypertrophy, visceromegaly, Wilms tu-
closure of the inferior abdominal wall with served within the solid component of meso- mor, macrosomia, macroglossia, nevus flam-
extrusion of the urinary bladder [31]. nephric blastomas [57]. meus, and hypoglycemia [48]. At prenatal
Megacystis-microcolon-intestinal hypope- Adrenal neuroblastoma is the most com- ultrasound, the adrenal glands appear thick-
ristalsis syndrome is a rare congenital disease mon fetal malignancy and is usually uni- ened, masslike, and echogenic, especially
that mainly affects female patients (70%). lateral. Prenatal diagnosis can be challeng- in the acute phase of hemorrhage. With ag-
Severe abdominal distention is caused by a ing; however, this tumor must be suspected ing of the hemorrhage, the adrenal glands
markedly dilated but unobstructed urinary when maternal symptoms due to increased decrease in size, and hypoechoic cystic ar-
bladder (i.e., megacystis) due to absent or ab- catecholamines are present. A prenatal adre- eas can be observed. The absence of flow at
normal urinary bladder wall motility. Colonic nal neuroblastoma appears as an echogenic Doppler evaluation is a key feature to distin-
and small-bowel peristalsis are nearly absent mass at sonography located just cephalad to guish an enlarged adrenal with a masslike
in this condition as well [51]. the kidneys, separate from the liver and the appearance due to hemorrhage from a neu-
Prune-belly syndrome (also known as Ea- spleen [58]. The Oreo-cookie appearance, roblastoma, which usually displays normal
gle-Barrett syndrome) is a condition where which is seen in normal adrenal glands or or greater Doppler flow. Owing to the typical
the absence of the rectus abdominis muscu- adrenal hyperplasia, is not identified in this behavior of hemoglobin breakdown byprod-
lature causes laxity and outward protrusion condition. At MRI, adrenal neuroblastoma ucts, MRI can be of further help to diagnose
of the anterior abdominal wall, accompanied appears as complex heterogeneous mass with adrenal hemorrhage. Intraadrenal T1-hyper-
with multisystem anomalies. Urinary tract mixed signal intensity characteristics due to intense foci can be seen in the acute phase,
involvement is usually characterized by re- the coexistence of solid components and cys- along with fluid-fluid levels on T2-weighted
nal parenchymal abnormalities with severely tic spaces. In some cases, adrenal neuroblas- imaging. After initial detection in a newborn,
dilated ureters, urinary bladder, and urethra toma can be highly aggressive, with a ten- adrenal hemorrhage typically resolves spon-
(i.e., megalocystic). Gastrointestinal, cardio- dency to rapidly metastasize to the kidneys taneously within the first month of life [53].
respiratory, and musculoskeletal involve- and to the spine and other osseous and non-
ment can also be seen [52]. osseous structures. MRI in general is pref- Conclusion
erable for detection of metastases [53]. Fetal Appropriate and normal function of the fe-
Fetal Renal and Adrenal Masses hydrops can be seen in the setting of fetal ad- tal urinary system has a major influence on fe-
Mesonephric blastoma is the most com- renal neuroblastoma [59]. tal well-being and development. Fetal urinary
mon fetal renal neoplasm. It is considered a Adrenal hemorrhage is rarely seen in ute- tract anomalies can be discovered in isolation
benign hamartoma without associated anom- ro but is usually observed in the setting of or in conjunction with other syndromes and
10 AJR:210, May 2018
Imaging of Fetal Urinary Tract Anomalies
conditions or anomalies. We have reviewed 6. Cohen HL, Cooper J, Eisenberg P, et al. Normal 21. Cassart M, Massez A, Metens T, et al. Comple-
the concepts related to normal fetal urinary length of fetal kidneys: sonographic study in 397 mentary role of MRI after sonography in assess-
tract development and have highlighted as- obstetric patients. AJR 1991; 157:545–548 ing bilateral urinary tract anomalies in the fetus.
sociated anomalies that can develop owing to 7. Doubilet PM. Ultrasound evaluation of the first tri- AJR 2004; 182:689–695
faulty or abnormal embryologic development. mester. Radiol Clin North Am 2014; 52:1191–1199 22. Türkvatan A, Olçer T, Cumhur T. Multidetector
We have presented the classification of fetal 8. Chauvin NA, Epelman M, Victoria T, Johnson CT urography of renal fusion anomalies. Diagn
Downloaded from www.ajronline.org by Tufts University on 02/16/18 from IP address 130.64.11.153. Copyright ARRS. For personal use only; all rights reserved
abnormalities of the kidneys and urinary tract AM. Complex genitourinary abnormalities on fe- Interv Radiol 2009; 15:127–134
based on the presence or absence of associat- tal MRI: imaging findings and approach to diag- 23. Bauer SB. Anomalies of the upper urinary tract.
ed urinary tract dilation. Ultrasound is the pri- nosis. AJR 2012; 199:[web]W222–W231 In: Walsh PC, Retik AB, Vaughan ED, Wein AJ,
mary imaging modality for the assessment of 9. Surabhi VR, Menias CO, George V, Matta E, eds. Campbell’s urology, 8th ed. Philadelphia, PA:
fetal anomalies of the urinary tract. Fetal MRI Kaza RK, Hasapes J. MDCT and MR urogram Saunders, 2002:1898–1906
has a complementary role in cases of equivo- spectrum of congenital anomalies of the kidney 24. Dyer RB, Chen MY, Zagoria RJ. Classic signs in uro-
cal or inconclusive ultrasound findings, to aid and urinary tract diagnoses in adulthood. AJR radiology. RadioGraphics 2004; 24(suppl 1):S247–
in definite diagnosis, thereby improving the 2015; 205:[web]W294–W304 S280
imaging-based management of the pregnancy. 10. McMullen KP, Karnes PS, Moir CR, Michels VV. 25. Goren E, Eidelman A. Pelvic cake kidney drained
In this article, we have reviewed the 2014 clas- Familial recurrence of tracheoesophageal fistula by single ureter. Urology 1987; 30:492–493
sification of urinary tract dilation based on the and associated malformations. Am J Med Genet 26. Bullo M, Tschumi S, Bucher BS, Bianchetti MG,
Linthicum multidisciplinary consensus pan- 1996; 63:525–528 Simonetti GD. Pregnancy outcome following ex-
el. To provide the readership with a practical 11. Alamo L, Meyrat BJ, Meuwly JY, Meuli RA, posure to angiotensin-converting enzyme inhibi-
synopsis, we also propose an algorithmic ap- Gudinchet F. Anorectal malformations: finding tors or angiotensin receptor antagonists: a system-
proach for the evaluation of fetal urinary tract the pathway out of the labyrinth. RadioGraphics atic review. Hypertension 2012; 60:444–450
and renal parenchymal abnormalities (Fig. S5 2013; 33:491–512 27. Nguyen HT, Benson CB, Bromley B, et al. Multidis-
can be viewed in the AJR electronic supple- 12. Copelovitch L, Kaplan BS. Developmental abnor- ciplinary consensus on the classification of prenatal
ment to this article, available at www.ajron- malities of the kidneys. In: Gleason CA, Devaskar and postnatal urinary tract dilation (UTD classifica-
line.org). This approach relies on the presence SU, eds. Avery’s diseases of the newborn, 9th ed., tion system). J Pediatr Urol 2014; 10:982–998
or absence of the kidneys on initial ultrasound chapter 83. Philadelphia, PA: Elsevier Saunders, 28. Nguyen HT, Herndon CD, Cooper C, et al. The
evaluation, as well as on the size and appear- 2012:1182–1190 Society for Fetal Urology consensus statement on
ance of the kidneys, and includes the most re- 13. Elder JS. Congenital anomalies and dysgenesis of the evaluation and management of antenatal hy-
cent recommendations for follow-up of each the kidneys. In: Kliegman RM, Stanton BF, St dronephrosis. J Pediatr Urol 2010; 6:212–231
abnormality. Familiarity of the radiologist Geme JW III, Schor NF, eds. Nelson textbook of 29. Guys JM, Borella F, Monfort G. Ureteropelvic junc-
with the anatomy and classification of urinary pediatrics, 20th ed., chapter 537. Philadelphia, tion obstructions: prenatal diagnosis and neonatal
tract and renal pathologic abnormalities, dif- PA: Elsevier, 2016:2554–2555 surgery in 47 cases. J Pediatr Surg 1988; 23:156–158
ferential diagnoses, and recommendations for 14. Dighe M, Moshiri M, Phillips G, Biyyam D, 30. Shokeir AA, Nijman RJ. Primary megaureter:
in utero management are of utmost impor- Dubinsky T. Fetal genitourinary anomalies: a picto- current trends in diagnosis and treatment. BJU Int
tance for those health care practitioners per- rial review with postnatal correlation. Ultrasound Q 2000; 86:861–868
forming and interpreting prenatal and perina- 2011; 27:7–21 31. Berrocal T, López-Pereira P, Arjonilla A, Gutiérrez
tal imaging. 15. Bronshtein M, Amit A, Achiron R, et al. The early J. Anomalies of the distal ureter, bladder, and ure-
prenatal sonographic diagnosis of renal agenesis: thra in children: embryologic, radiologic, and patho-
References techniques and possible pitfalls. Prenat Diagn logic features. RadioGraphics 2002; 22:1139–1164
1. Dias T, Sairam S, Kumarasiri S. Ultrasound diag- 1994; 14:291–297 32. Dickerson EC, Dillman JR, Smith EA, DiPietro
nosis of fetal renal abnormalities. Best Pract Res 16. Mercado-Deane MG, Beeson JE, John SD. US of MA, Lebowitz RL, Darge K. Pediatric MR urog-
Clin Obstet Gynaecol 2014; 28:403–415 renal insufficiency in neonates. RadioGraphics raphy: indications, techniques, and approach to
2. Nef S, Neuhaus TJ, Spartà G, et al. Outcome after 2002; 22:1429–1438 review. RadioGraphics 2015; 35:1208–1230
prenatal diagnosis of congenital anomalies of the 17. Cho JY, Moon MH, Lee Y, Kim KW, Kim SH. 33. Lim R. Vesicoureteral reflux and urinary tract in-
kidney and urinary tract. Eur J Pediatr 2016; Measurement of compensatory hyperplasia of the fection: evolving practices and current controversies
175:667–676 contralateral kidney: usefulness for differential in pediatric imaging. AJR 2009; 192:1197–1208
3. Mehler K, Beck BB, Kaul I, Rahimi G, Hoppe B, diagnosis of fetal unilateral empty renal fossa. 34. Ascenti G, Zimbaro G, Mazziotti S, et al. Har-
Kribs A. Respiratory and general outcome in neo- Ultrasound Obstet Gynecol 2009; 34:515–520 monic US imaging of vesicoureteric reflux in chil-
nates with renal oligohydramnios: a single-centre 18. Kuure S, Vuolteenaho R, Vainio S. Kidney mor- dren: usefulness of a second generation US con-
experience. Nephrol Dial Transplant 2011; phogenesis: cellular and molecular regulation. trast agent. Pediatr Radiol 2004; 34:481–487
26:3514–3522 Mech Dev 2000; 92:31–45 35. Zimbaro G, Ascenti G, Visalli C, et al. Contrast-
4. Spiro JE, Konrad M, Rieger-Fackeldey E, et al. 19. van den Bosch CM, van Wijk JA, Beckers GM, enhanced ultrasonography (voiding urosonogra-
Renal oligo- and anhydramnios: cause, course and van der Horst HJ, Schreuder MF, Bökenkamp A. phy) of vesicoureteral reflux: state of the art.
outcome—a single center study. Arch Gynecol Urological and nephrological findings of renal ec- Radiol Med (Torino) 2007; 112:1211–1224
Obstet 2015; 292:327–336 topia. J Urol 2010; 183:1574–1578 36. Lebowitz RL, Olbing H, Parkkulainen KV,
5. Cohen HL, Sansgiri R, Smothers C, Mari G. Top- 20. Lebowitz RL, Griscom NT. Neonatal hydrone- Smellie JM, Tamminen-Moebius TE. Internation-
ics in perinatal genitourinary system ultrasound phrosis: 146 cases. Radiol Clin North Am 1977; al system of radiographic grading of vesicoure-
evaluation. Ultrasound Q 2011; 27:229–254 15:49–59 teric reflux. Pediatr Radiol 1985; 15:105–109
AJR:210, May 2018 11
Mileto et al.
37. Ascenti G, Zimbaro G, Mazziotti S, Chimenz R, seling. Am J Hum Genet 1995; 56:1101–1107 population. Urology 2015; 85:211–215
Baldari S, Fede C. Vesicoureteral reflux: compari- 45. MacDermot KD, Saggar-Malik AK, Economides 53. Flanagan SM, Rubesova E, Jaramillo D, Barth RA.
son between urosonography and radionuclide cys- DL, Jeffery S. Prenatal diagnosis of autosomal Fetal suprarenal masses: assessing the complemen-
tography. Pediatr Nephrol 2003; 18:768–771 dominant polycystic kidney disease (PKD1) pre- tary role of magnetic resonance and ultrasound for
38. Fernbach SK, Feinstein KA, Spencer K, Lindstrom senting in utero and prognosis for very early onset diagnosis. Pediatr Radiol 2016; 46:246–254
CA. Ureteral duplication and its complications. disease. J Med Genet 1998; 35:13–16 54. Maki E, Oh K, Rogers S, Sohaey R. Imaging and
Downloaded from www.ajronline.org by Tufts University on 02/16/18 from IP address 130.64.11.153. Copyright ARRS. For personal use only; all rights reserved
RadioGraphics 1997; 17:109–127 46. Farrugia MK. Fetal bladder outlet obstruc- differential diagnosis of suprarenal masses in the
39. Kass EJ. Megaureter. In: Kelalis PP, King LR, tion: embryopathology, in utero intervention and fetus. J Ultrasound Med 2014; 33:895–904
Belman AB, eds. Clinical pediatric urology, 3rd outcome. J Pediatr Urol 2016; 12:296–303 55. Lloyd JC, Wiener JS, Gargollo PC, Inman BA,
ed. Philadelphia, PA: Saunders, 1992:781–821 47. Chevalier RL. Prognostic factors and biomarkers Ross SS, Routh JC. Contemporary epidemiologi-
40. Avni FE, Garel C, Cassart M, D’Haene N, Hall M, of congenital obstructive nephropathy. Pediatr cal trends in complex congenital genitourinary
Riccabona M. Imaging and classification of congeni- Nephrol 2016; 31:1411–1420 anomalies. J Urol 2013; 190(4 suppl):1590–1595
tal cystic renal diseases. AJR 2012; 198:1004–1013 48. Tong CC, Duffy KA, Chu DI, et al. Uro- 56. Mesrobian HG, Balcom AH, Durkee CT. Urologic
41. Chung EM, Conran RM, Schroeder JW, Rohena- logical findings in Beckwith-Wiedemann syndrome problems of the neonate. Pediatr Clin North Am
Quinquilla IR, Rooks VJ. From the radiologic pa- with chromosomal duplications of 11p15.5: evalua- 2004; 51:1051–1062
thology archives: pediatric polycystic kidney dis- tion and management. Urology 2016; 100:224–227 57. Chaudry G, Perez-atayde AR, Ngan BY, et al. Im-
ease and other ciliopathies—radiologic-pathologic 49. Morris RK, Malin GL, Quinlan-Jones E, et al. aging of congenital mesoblastic nephroma with
correlation. RadioGraphics 2014; 34:155–178 Percutaneous vesicoamniotic shunting versus pathological correlation. Pediatr Radiol 2009;
42. Avni FE, Guissard G, Hall M, Janssen F, conservative management for fetal lower urinary 39:1080–1086
DeMaertelaer V, Rypens F. Hereditary polycystic tract obstruction (PLUTO): a randomised trial. 58. Hwang SM, Yoo SY, Kim JH, Jeon TY. Congenital
kidney diseases in children: changing sonograph- Lancet 2013; 382:1496–1506 adrenal neuroblastoma with and without cystic
ic patterns through childhood. Pediatr Radiol 50. Morris RK, Khan KS, Kilby MD. Vesicoamniotic change: differentiating features with an emphasis on
2002; 32:169–174 shunting for fetal lower urinary tract obstruction: the of value of ultrasound. AJR 2016; 207:1105–1111
43. Weinstein A, Goodman TR, Iragorri S. Simple an overview. Arch Dis Child Fetal Neonatal Ed 59. Chambrier ED, Heinrichs C, Avni FE. Sonograph-
multicystic dysplastic kidney disease: end points 2007; 92:F166–F168 ic appearance of congenital adrenal hyperplasia in
for subspecialty follow-up. Pediatr Nephrol 2008; 51. Gosemann JH, Puri P. Megacystis microcolon intes- utero. J Ultrasound Med 2002; 21:97–100
23:111–116 tinal hypoperistalsis syndrome: systematic review 60. Schwärzler P, Bernard JP, Senat MV, Ville Y. Pre-
44. Guay-Woodford LM, Muecher G, Hopkins SD, et of outcome. Pediatr Surg Int 2011; 27:1041–1046 natal diagnosis of fetal adrenal masses: differen-
al. The severe perinatal form of autosomal reces- 52. Seidel NE, Arlen AM, Smith EA, Kirsch AJ. Clin- tiation between hemorrhage and solid tumor by
sive polycystic kidney disease maps to chromo- ical manifestations and management of prune- color Doppler sonography. Ultrasound Obstet
some 6p21.1-p12: implications for genetic coun- belly syndrome in a large contemporary pediatric Gynecol 1999; 13:351–355
F O R YO U R I N F O R M AT I O N
A data supplement for this article can be viewed in the online version of the article at: www.ajronline.org.
12 AJR:210, May 2018
Você também pode gostar
- USABO Competition: Answers Saved QDocumento25 páginasUSABO Competition: Answers Saved QChanguoi YOtoAinda não há avaliações
- Lesson Plan On Polycystic Ovary Syndrome (Pcos)Documento22 páginasLesson Plan On Polycystic Ovary Syndrome (Pcos)N.Subhashini100% (5)
- Michael W, COMAT ObgynDocumento12 páginasMichael W, COMAT ObgynSeanAinda não há avaliações
- Nurse's Pocket GuideDocumento11 páginasNurse's Pocket GuideRaf_Harold_427Ainda não há avaliações
- AIP Chap12 Vaginal Breech PDFDocumento14 páginasAIP Chap12 Vaginal Breech PDFviaereaAinda não há avaliações
- Medical-Surgical Nursing 75 Items TestDocumento13 páginasMedical-Surgical Nursing 75 Items Testwiffato25% (4)
- Leopold's Maneuver - Systematic Method for Fetal PresentationDocumento2 páginasLeopold's Maneuver - Systematic Method for Fetal PresentationPJ AmolarAinda não há avaliações
- MCN QUIZ With Rationale 60ptsDocumento16 páginasMCN QUIZ With Rationale 60ptsKyla CapituloAinda não há avaliações
- Fundamentals of Human Embryology: Student Manual (second edition)No EverandFundamentals of Human Embryology: Student Manual (second edition)Nota: 3 de 5 estrelas3/5 (3)
- Shoulder PresentationDocumento8 páginasShoulder PresentationvincentsharonAinda não há avaliações
- Birth Defects and Prenatal DiagnosisDocumento137 páginasBirth Defects and Prenatal DiagnosisSohera Nadeem100% (1)
- Part 1 RenalDocumento8 páginasPart 1 RenalKatherine ApostolAinda não há avaliações
- Metabolic Disorders in Pregnancy, Labour and Post PartumDocumento45 páginasMetabolic Disorders in Pregnancy, Labour and Post PartumNidhi SharmaAinda não há avaliações
- Practice Test 2 MCNDocumento8 páginasPractice Test 2 MCNIriel Nadonga50% (2)
- What The Radiologist Needs To Know About Urolithiasis: Part 1 - Pathogenesis, Types, Assessment, and Variant AnatomyDocumento8 páginasWhat The Radiologist Needs To Know About Urolithiasis: Part 1 - Pathogenesis, Types, Assessment, and Variant AnatomyQonita Aizati QomaruddinAinda não há avaliações
- Update On The Prenatal Diagnosis and Outcomes of Fetal Bilateral Renal AgenesisDocumento5 páginasUpdate On The Prenatal Diagnosis and Outcomes of Fetal Bilateral Renal AgenesisShynta AmeliaAinda não há avaliações
- Oral and Maxillofacial PathologyDocumento11 páginasOral and Maxillofacial PathologyIzadora VeigaAinda não há avaliações
- Journal of Rare Diseases MARDocumento13 páginasJournal of Rare Diseases MARDaiiny DelgadoAinda não há avaliações
- From The Archives of The AFIP: Endometriosis: Radiologic-Pathologic CorrelationDocumento24 páginasFrom The Archives of The AFIP: Endometriosis: Radiologic-Pathologic Correlation104022432 104a-Ainda não há avaliações
- (1479683X - European Journal of Endocrinology) Undescended Testes in Children - The Paediatric Urologist's Point of ViewDocumento4 páginas(1479683X - European Journal of Endocrinology) Undescended Testes in Children - The Paediatric Urologist's Point of ViewCaca mericayAinda não há avaliações
- Juvenile Granulosa Cell Tumor of The Testis PrenatDocumento4 páginasJuvenile Granulosa Cell Tumor of The Testis PrenatPuspita MahardikaAinda não há avaliações
- GastrointestinalDocumento10 páginasGastrointestinalPaola Mercedes Matos OrtegaAinda não há avaliações
- Ajr 17 19378Documento13 páginasAjr 17 19378heryanggunAinda não há avaliações
- The Paediatric Thymus: Recognising Normal and Ectopic Thymic TissueDocumento11 páginasThe Paediatric Thymus: Recognising Normal and Ectopic Thymic TissueFifi FathiraAinda não há avaliações
- Olive, D. L., & Pritts, E. A. (2001) - Treatment of Endometriosis. The New England Journal of Medicine, 345 (4), 266-275.Documento11 páginasOlive, D. L., & Pritts, E. A. (2001) - Treatment of Endometriosis. The New England Journal of Medicine, 345 (4), 266-275.Hernando Rivera-DuqueAinda não há avaliações
- Inborn Errors of Metabolism 2015Documento5 páginasInborn Errors of Metabolism 2015marcela fernandezAinda não há avaliações
- Embryology AssignmentDocumento5 páginasEmbryology Assignmentrahma kaggwaAinda não há avaliações
- Jurnal 8Documento13 páginasJurnal 8sriwahyuutamiAinda não há avaliações
- Ultrasound Findings in Paediatric Cholestasis How To Image The Patient and What To Look ForDocumento12 páginasUltrasound Findings in Paediatric Cholestasis How To Image The Patient and What To Look ForintanAinda não há avaliações
- Patof Fetal Neonatal KidneyDocumento16 páginasPatof Fetal Neonatal KidneyNia Prajnya SyailendraAinda não há avaliações
- 1 s2.0 S0140673610603558 MainDocumento11 páginas1 s2.0 S0140673610603558 MainDr. Eser AĞARAinda não há avaliações
- Meconium PeritonitisDocumento11 páginasMeconium PeritonitisGiang Dinh NguyenAinda não há avaliações
- Surgical Treatment of Anorectal MalformationsDocumento8 páginasSurgical Treatment of Anorectal MalformationsGerii Pucllas VillarAinda não há avaliações
- Benign Penile Skin Anomalies in Children: A Primer For PediatriciansDocumento8 páginasBenign Penile Skin Anomalies in Children: A Primer For Pediatriciansdrfebri86Ainda não há avaliações
- Wood 2018Documento10 páginasWood 2018dewaprasatyaAinda não há avaliações
- Jurnal MAR 2Documento10 páginasJurnal MAR 2Taufik HidayatAinda não há avaliações
- Dioxins and Endometriosis: A Plausible HypothesisDocumento7 páginasDioxins and Endometriosis: A Plausible HypothesiscountlessgalaxiesAinda não há avaliações
- Ambiguous Genitalia 3Documento4 páginasAmbiguous Genitalia 3syarifah salmaAinda não há avaliações
- Penis: 2.1 Embryology and Penile DevelopmentDocumento27 páginasPenis: 2.1 Embryology and Penile DevelopmenteeAinda não há avaliações
- Asfixia perinatal, compendiumDocumento7 páginasAsfixia perinatal, compendiumClaudia LópezAinda não há avaliações
- Aub eDocumento8 páginasAub epitriaAinda não há avaliações
- Material 3 - Acute Kidney Injury in Children - Fauziah Rudhiati, MKep., Sp. Kep - An PDFDocumento21 páginasMaterial 3 - Acute Kidney Injury in Children - Fauziah Rudhiati, MKep., Sp. Kep - An PDFINTAN MADULARAAinda não há avaliações
- Anomalias Congenias Del RiñonDocumento26 páginasAnomalias Congenias Del RiñonDr Gerardo Corral AyonAinda não há avaliações
- 6 Birth DefectsDocumento8 páginas6 Birth DefectsCearlene GalleonAinda não há avaliações
- LeucemieDocumento2 páginasLeucemieMădălina MoldovanuAinda não há avaliações
- Obstructive Nephropathy PDFDocumento14 páginasObstructive Nephropathy PDFMuhammad Firdaus J KarimiAinda não há avaliações
- Bladder Management in Children With Transverse MyelitisDocumento6 páginasBladder Management in Children With Transverse Myelitisdipan diratuAinda não há avaliações
- Ectopic Pregnancy Case Study: Nursing Care Plans and PrognosisDocumento21 páginasEctopic Pregnancy Case Study: Nursing Care Plans and PrognosisMardina A AbdulmaulaAinda não há avaliações
- Seleneum in ReproductiveDocumento19 páginasSeleneum in ReproductiveCakraEkkyAinda não há avaliações
- Reproductive SystemDocumento31 páginasReproductive SystemsabanalgenneAinda não há avaliações
- TAP 20230090 NLM New InddDocumento8 páginasTAP 20230090 NLM New InddYusuf HardiAinda não há avaliações
- Broodbank & Christian. Renal Tubular Disorders. 2018.Documento10 páginasBroodbank & Christian. Renal Tubular Disorders. 2018.Jéssica Hilário BonomoAinda não há avaliações
- 2020 Article 1400Documento10 páginas2020 Article 1400Kim RamirezAinda não há avaliações
- Urology Course Covers Congenital AnomaliesDocumento236 páginasUrology Course Covers Congenital AnomaliesAlexandra BalanAinda não há avaliações
- Klinger 1997Documento4 páginasKlinger 1997Sarly FebrianaAinda não há avaliações
- Imaging of Postpartum Complications: A Multimodality ReviewDocumento12 páginasImaging of Postpartum Complications: A Multimodality ReviewGabriela Serra del CarpioAinda não há avaliações
- Anaesthetic Management Branchial Oto Renal SyndromeDocumento5 páginasAnaesthetic Management Branchial Oto Renal SyndromeJIHAN ISMAILAinda não há avaliações
- Anophthalmis MicrophthalmiaDocumento11 páginasAnophthalmis Microphthalmiasg1964Ainda não há avaliações
- Adenomiose 2020Documento15 páginasAdenomiose 2020mariajuliabechepecheAinda não há avaliações
- Renal Ultrasound Abnormalities in Children With Syndromic Microtia Julie2018Documento4 páginasRenal Ultrasound Abnormalities in Children With Syndromic Microtia Julie2018Miguel Angel Larico QuispeAinda não há avaliações
- NMTC Keta Surgical NursingDocumento36 páginasNMTC Keta Surgical NursingselormniiqAinda não há avaliações
- Refrat Fidel Kelainan KongenitalDocumento44 páginasRefrat Fidel Kelainan KongenitalFidelia YudiAinda não há avaliações
- FOSSUM Embryology LUT TEMA 15.11.15Documento15 páginasFOSSUM Embryology LUT TEMA 15.11.15Oscar Sanchez ParisAinda não há avaliações
- Intraoperative Injuries of The Urinary TractDocumento14 páginasIntraoperative Injuries of The Urinary TractDEVINAAinda não há avaliações
- Valle 2013Documento21 páginasValle 2013Karisma NandaAinda não há avaliações
- AUR in ChildrenDocumento1 páginaAUR in ChildrenStaporn KasemsripitakAinda não há avaliações
- Congenital Anomalies of Kidney and Ureter 2161 0940 1000190Documento10 páginasCongenital Anomalies of Kidney and Ureter 2161 0940 1000190Indra JayaAinda não há avaliações
- Complex Case of Ureteropelvic Junction Obstruction 2024 International JournaDocumento3 páginasComplex Case of Ureteropelvic Junction Obstruction 2024 International JournaRonald QuezadaAinda não há avaliações
- The Isolated hepatocyte: Use in Toxicology and Xenobiotic BiotransformationsNo EverandThe Isolated hepatocyte: Use in Toxicology and Xenobiotic BiotransformationsAinda não há avaliações
- En V18n27a02 PDFDocumento11 páginasEn V18n27a02 PDFAnonymous wdmpgxAinda não há avaliações
- Refining Diagnosis and Mangaement of Chronic Venous Disease PDFDocumento8 páginasRefining Diagnosis and Mangaement of Chronic Venous Disease PDFAnonymous wdmpgxAinda não há avaliações
- Epidemiological Characteristics, Safety and Efficacy of Medical Cannabis in ElderlyDocumento7 páginasEpidemiological Characteristics, Safety and Efficacy of Medical Cannabis in ElderlyAnonymous wdmpgxAinda não há avaliações
- HBVGuidance Terrault Et Al-2018-Hepatology PDFDocumento40 páginasHBVGuidance Terrault Et Al-2018-Hepatology PDFAnonymous wdmpgxAinda não há avaliações
- High Serum Uric Acid Is Associated With Poorly Controlled Blood Pressure and Higher Arterial Stiffness in Hypertensive Subjects PDFDocumento5 páginasHigh Serum Uric Acid Is Associated With Poorly Controlled Blood Pressure and Higher Arterial Stiffness in Hypertensive Subjects PDFAnonymous wdmpgxAinda não há avaliações
- Physiological Aspects of Central Blockade (2005)Documento6 páginasPhysiological Aspects of Central Blockade (2005)Anonymous wdmpgxAinda não há avaliações
- GigiDocumento3 páginasGigiAnonymous wdmpgxAinda não há avaliações
- ScabiesDocumento12 páginasScabiesalston96Ainda não há avaliações
- Atopic Dermatitis - by KY Sayaseng - 2018 PDFDocumento11 páginasAtopic Dermatitis - by KY Sayaseng - 2018 PDFFelicia ShinamaAinda não há avaliações
- Suspected Malignant Hyperthermia in The Setting Of.7 PDFDocumento3 páginasSuspected Malignant Hyperthermia in The Setting Of.7 PDFAnonymous wdmpgxAinda não há avaliações
- Preterm Pre-Labour Rupture of The Membranes Close To Term (Ppromt) TrialDocumento6 páginasPreterm Pre-Labour Rupture of The Membranes Close To Term (Ppromt) TrialAnonymous wdmpgxAinda não há avaliações
- OsteDocumento10 páginasOsteAnonymous wdmpgxAinda não há avaliações
- Ajr. Imaging Pulmonary InfectionDocumento14 páginasAjr. Imaging Pulmonary InfectionAlbert RanggaAinda não há avaliações
- Symposium Article: Imaging of A Child With PolytraumaDocumento22 páginasSymposium Article: Imaging of A Child With PolytraumaAnonymous wdmpgxAinda não há avaliações
- Emergent Airway Management of An Uncooperative.6 PDFDocumento4 páginasEmergent Airway Management of An Uncooperative.6 PDFAnonymous wdmpgxAinda não há avaliações
- Non Steady State Modeling of The Ventilatory Depressant Effect of Remifentanil in Awake Patients Experiencing Moderate To Severe OSA PDFDocumento14 páginasNon Steady State Modeling of The Ventilatory Depressant Effect of Remifentanil in Awake Patients Experiencing Moderate To Severe OSA PDFAnonymous wdmpgxAinda não há avaliações
- Emergent Airway Management of An Uncooperative Child With A Large Retropharyngeal and Posterior Mediastinal AbscessDocumento4 páginasEmergent Airway Management of An Uncooperative Child With A Large Retropharyngeal and Posterior Mediastinal AbscessAnonymous wdmpgxAinda não há avaliações
- Screening Breast Ultrasound: Past, Present, and FutureDocumento7 páginasScreening Breast Ultrasound: Past, Present, and FutureAnonymous wdmpgxAinda não há avaliações
- Two For One A Case Report of Intravenous Lipid.6Documento3 páginasTwo For One A Case Report of Intravenous Lipid.6Anonymous wdmpgxAinda não há avaliações
- Non Steady State Modeling of The Ventilatory Depressant Effect of Remifentanil in Awake Patients Experiencing Moderate To Severe OSA PDFDocumento14 páginasNon Steady State Modeling of The Ventilatory Depressant Effect of Remifentanil in Awake Patients Experiencing Moderate To Severe OSA PDFAnonymous wdmpgxAinda não há avaliações
- C. Cozowicz, J. Poeran, N. Zubizarreta, J. Liu, S. M. Weinstein, L. Pichler, M. Mazumdar and S. G. MemtsoudisDocumento10 páginasC. Cozowicz, J. Poeran, N. Zubizarreta, J. Liu, S. M. Weinstein, L. Pichler, M. Mazumdar and S. G. MemtsoudisAnonymous wdmpgxAinda não há avaliações
- Suspected Malignant Hyperthermia in The Setting Of.7Documento3 páginasSuspected Malignant Hyperthermia in The Setting Of.7Anonymous wdmpgxAinda não há avaliações
- Imaging of GI and Abdominal Emergencies in Binge DrinkingDocumento10 páginasImaging of GI and Abdominal Emergencies in Binge DrinkingAnonymous wdmpgxAinda não há avaliações
- OSA Syndrome in The Pediatric Age PDFDocumento8 páginasOSA Syndrome in The Pediatric Age PDFAnonymous wdmpgxAinda não há avaliações
- Ultrasound of Fetal Cardiac AnomaliesDocumento14 páginasUltrasound of Fetal Cardiac AnomaliesAnailil MoralesAinda não há avaliações
- Ajr. Imaging Pulmonary InfectionDocumento14 páginasAjr. Imaging Pulmonary InfectionAlbert RanggaAinda não há avaliações
- July 2016 Ophthalmic PearlsDocumento4 páginasJuly 2016 Ophthalmic PearlsRaissaAinda não há avaliações
- Non Steady State Modeling of The Ventilatory Depressant Effect of Remifentanil in Awake Patients Experiencing Moderate To Severe OSADocumento14 páginasNon Steady State Modeling of The Ventilatory Depressant Effect of Remifentanil in Awake Patients Experiencing Moderate To Severe OSAAnonymous wdmpgxAinda não há avaliações
- Risk Factors For OIRD in Surgical PatientsDocumento10 páginasRisk Factors For OIRD in Surgical PatientsAnonymous wdmpgxAinda não há avaliações
- OSA Syndrome in The Pediatric AgeDocumento8 páginasOSA Syndrome in The Pediatric AgeAnonymous wdmpgxAinda não há avaliações
- Normal ObDocumento31 páginasNormal ObShai EstrellerAinda não há avaliações
- 10 pt3 Soalan Bi PDFDocumento28 páginas10 pt3 Soalan Bi PDFMelor DihatiAinda não há avaliações
- Nomograms of Fetal Cardiac Dimensions at 18-41 Weeks of GestationDocumento12 páginasNomograms of Fetal Cardiac Dimensions at 18-41 Weeks of GestationMarco Julcamoro AsencioAinda não há avaliações
- Forensic Aspects of Pregnancy and DeliveryDocumento118 páginasForensic Aspects of Pregnancy and DeliveryAl Giorgio SyAinda não há avaliações
- Mock Exam 2Documento18 páginasMock Exam 2Anna StacyAinda não há avaliações
- Form F Registration RecordDocumento2 páginasForm F Registration RecordArchit ChampanekarAinda não há avaliações
- Tilly's Care StudyDocumento105 páginasTilly's Care StudyRichmond AnaneAinda não há avaliações
- Antepartum Nursing AssessmentDocumento88 páginasAntepartum Nursing AssessmentDeema AbuasiAinda não há avaliações
- CP - MP .38 Ultrasound in PregnancyDocumento9 páginasCP - MP .38 Ultrasound in PregnancyRavi PalAinda não há avaliações
- NCM 109 Module Final EditedDocumento121 páginasNCM 109 Module Final EditedMary Ann G. CorsanesAinda não há avaliações
- Stages of Fetal DevelopmentDocumento42 páginasStages of Fetal DevelopmentKara Ashleigh0% (1)
- In The Fetal CirculationDocumento1 páginaIn The Fetal CirculationJesena SalveAinda não há avaliações
- Staff Nurse Exam Practice Test QuestionsDocumento30 páginasStaff Nurse Exam Practice Test QuestionsElma Simon PattamanaAinda não há avaliações
- DR Power PointDocumento30 páginasDR Power PointlezahazelAinda não há avaliações
- Student Nurses' Guide to Spontaneous Abortion Care PlanDocumento2 páginasStudent Nurses' Guide to Spontaneous Abortion Care PlanMina RacadioAinda não há avaliações
- (Bioethics 2) 2.02 - Chua-Chan - S AIDS - Health Care (Pat G)Documento13 páginas(Bioethics 2) 2.02 - Chua-Chan - S AIDS - Health Care (Pat G)Mikee MeladAinda não há avaliações
- Polyhydramnios & Oligiohydramnios: Prof. Yasmin RaashidDocumento11 páginasPolyhydramnios & Oligiohydramnios: Prof. Yasmin RaashidShimmering MoonAinda não há avaliações
- How Pandemics SpreadDocumento7 páginasHow Pandemics SpreadTấn NguyễnAinda não há avaliações
- Psychological Changes of PregnancyDocumento30 páginasPsychological Changes of PregnancyyuddAinda não há avaliações