Escolar Documentos
Profissional Documentos
Cultura Documentos
A Retrospective Study On The Risk of Nonmelanoma Skin Cancer in Puva and Narrowband Uvb Treated Patients
Enviado por
Fortune JournalsTítulo original
Direitos autorais
Formatos disponíveis
Compartilhar este documento
Compartilhar ou incorporar documento
Você considera este documento útil?
Este conteúdo é inapropriado?
Denunciar este documentoDireitos autorais:
Formatos disponíveis
A Retrospective Study On The Risk of Nonmelanoma Skin Cancer in Puva and Narrowband Uvb Treated Patients
Enviado por
Fortune JournalsDireitos autorais:
Formatos disponíveis
Volume 1, Issue 3 Research Article
A Retrospective Study on the Risk of Non-Melanoma Skin
Cancer in PUVA and Narrowband UVB Treated Patients
Darukarnphut P, Rattanakaemakorn P*, Rajatanavin N
Division of Dermatology, Faculty of Medicine, Ramathibodi Hospital, Mahidol University, Thailand
*
Corresponding Author: Rattanakaemakorn P, Division of Dermatology, Faculty of Medicine, Ramathibodi
Hospital, Mahidol University, Thailand, E-mail: ploysyne@gmail.com
Received: 04 April 2017; Accepted: 24 April 2017; Published: 28 April 2017
Abstract
Background: Narrow-band ultraviolet B (NB-UVB) and Psoralen-UVA (PUVA) phototherapy are widely used as
the treatment of dermatologic diseases. The carcinogenic risk associated with NB-UVB and PUVA phototherapy
treatment is unknown.
Objective: To determine the non-melanoma skin cancer risk in a patients treated with Narrow-band ultraviolet B
(NB-UVB) and Psoralen-UVA (PUVA) phototherapy.
Methods: All Narrow-band ultraviolet B (NB-UVB) and Psoralen-UVA (PUVA) phototherapy treated patient
records who received the phototherapy in Ramathibodi Hospital from 2001 to 2015 were reviewed.
Results: A total of 726 with Narrow-band ultraviolet B (NB-UVB) and Psoralen-UVA photochemotherapy (PUVA)
phototherapy treated patients with mean age of 46.7 years. Most of patients have skin phototypes III to IV. Vitiligo
is the most common disease treated with phototherapy (43.8%). The median number of NB-UVB treatment was 126
treatments with cumulative dose 94.2 J/cm². The median number of PUVA treatment was 103 treatments with
cumulative dose 249.2 J/cm². There was no non melanoma skin cancer in our patients. The median time of follow up
was 28.4 months.
Arch Clin Biomed Res 2017; 1 (3): 116-121 116
Conclusion: This study did not shown an increase risk of skin cancer in patients who had receiving long term NB-
UVB and PUVA phototherapy. We suggest that long term NB-UVB and PUVA phototherapy are safe therapeutic
modalities for the patients with skin phototypes III to IV.
Keywords: Non Melanoma Skin Cancer Risk; NB-UVB and PUVA Phototherapy
1. Introduction
Psoralen-UVA photochemotherapy (PUVA) phototherapy and narrow-band ultraviolet B (NB-UVB) phototherapy
are the effective treatments for dermatologic diseases such as psoriasis, atopic dermatitis, vitiligo, and mycosis
fungoides [1]. Non-melanoma skin cancers (NMSC) are generally associated with cumulative exposure to ultraviolet
radiation [2]. The incidence of non-melanoma skin cancers associated with phototherapy was limited. PUVA is
associated with a definite cumulative exposure and UVA dose related increase in the risk of skin cancers [3,4]. There
was no definite associations between NB-UVB phototherapy and skin cancer were found in retrospective studies
carried out in Northern Ireland, Scotland and German, an increase risk of non-melanoma skin cancer among patients
treated with both PUVA and NB-UVB was reported.
Whereas, the European studies focused on Caucasian patients and their findings may not be applicable to non-
Caucasians [5,6,9]. PUVA and NB-UVB phototherapy are widely used in Thailand but the photocarcinogenic risk of
PUVA and NB-UVB in patients with skin phototypes III-V was unknown. Our study investigated the occurrence of
NMSC in a patients who were treated with PUVA and NB-UVB phototherapy.
2. Material and methods
2.1 Patients
The data analyzed in this retrospective study were collected from patients’ medical records. Between January 2001
and December 2015, 956 patients with psoriasis, vitiligo, atopic dermatitis, livedoid vasculitis, pityriasis lichenoides
chronica, and other dermatoses received PUVA, NB-UVB or both modalities at phototherapy clinic, Ramathibodi
hospital. 230 patients who had either the follow up period less than two months or the total treatment sessions less
than twenty were excluded. Most patients were treated two or three times per week. Treatment began with an initial
dose of 50–70% of the minimal erythema dose (MED) followed by a 10–20% incremental dose regimen. During
phototherapy, the patients received routine facial and genital protection.
We reviewed patient medical records to obtain information on demographic characteristics, skin phototype, total
number of phototherapy sessions, total cumulative dose, medical treatment combination phototherapy and other
relevant with items. Reported non-melanoma cancer cases were classified according to the International
Classification of Diseases for Oncology 3rd edition and converted according to the International Classification of
Diseases 10th edition (ICD-10).
Arch Clin Biomed Res 2017; 1 (3): 116-121 117
2.2 Statistical analysis
Expected numbers of cases in the PUVA, NB-UVB and both modalities treated group and the standardized
incidence ratios (SIRs) for NMSC were calculated from the incidence rates in the control population. Statistical
analyses were performed using SPSS version 17.0.
3. Results
3.1. Demographic Data
Demographic data for the 726 patients who underwent phototherapy more than 20 sessions or follow up period more
2 months between January 2001 and December 2015 are shown in Table 1. The mean age was 47 years old. There
was slightly female predominance (60%). Ninety nine percent of the patients were Thai. 38 patients were classified
as having skin type II, 360 skin type III, 185 skin type IV and skin type were not recorded for the remaining 143
patients. Of these 726 patients, the most common underlying diseases of the patients was vitiligo 318 (43.8%)
followed by psoriasis 269 (37.1%), mycosis fungoides 59 (8.1%), pityriasis lichenoides chronica 17 (2.3%), hand
and foot eczema 12 (1.7%), atopic dermatitis 9 (1.2%), livedoid vasculitis 9 (1.1%) and others 34 (4.7%) (Figure 1).
The most common drug use combination with phototherapy was methotrexate 161 (22%), followed by azathioprine
87 (12%), cyclosporine 76 (11%), acitretin 54 (7%), and others 33 (5%) (Figure 2). There was one patient with two
lesions of basal cell carcinoma (BCC) on face and remission after surgical treatment. The skin cancer were
developed before the initiation of phototherapy and no recurrence after long term follow up.
Parameters Values
Number of patients 726
Age, year, mean±SD 46.7±16.2
Sex, N(%)
Female 432 (59.5)
Race, N(%)
Thai 719 (99.2)
Fitzpatrick’s skin phototype, N(%)
II 38 (5.2)
III 360 (49.6)
IV 185 (25.5)
No record 143 (19.7)
Phototherapy, N(%)
PUVA 33 (4.5)
NB-UVB 624 (86)
Both PUVA and NB-UVB 69 (9.5)
Pre-existing skin cancer 2 BCCs
Table 1: Demographic parameters in patients treated with phototherapy at Ramathibodi hospital
Arch Clin Biomed Res 2017; 1 (3): 116-121 118
SD: standard deviation
Figure 1: The underlying disease of the patients treated with phototherapy
Figure 2: The combination drug use in the patients treated with phototherapy
3.2. PUVA, NB-UVB and both modalities phototherapy
There was 33 (4.5%) patients treated with PUVA, 624 (86%) treated with NB-UVB and 69 (9.5%) treated with both
modalities. The average number of phototherapy sessions in PUVA group was 103.3 and 126.3 in the NB-UVB. The
average cumulative dose of PUVA was 249.2 J/cm2 and 94.5 J/cm2 in NB-UVB group. The average number of
phototherapy sessions of PUVA and NB-UVB was 112 and 87, the average cumulative dose of PUVA and NB-
UVB was 360.3 and 146 J/cm2 and the median time of follow up was 28.4 months in PUVA and NB-UVB group
(Table 2).
Arch Clin Biomed Res 2017; 1 (3): 116-121 119
Parameters PUVA NB-UVB PUVA&NB-UVB
Number of patients, 33(4.5) 624(86) 69(9.5)
N (%)
Time of follow-up, 39.7 26.8 28.4
months, median (range) (2 - 244) (2 - 434) (2 - 264)
PUVA NB-UVB
Cumulative dose, J/cm² 249.2 94.5 360.3 146
Median (range) (40.8- 3795.2) (2.1 – 2059.7) (40.8 - 3795.2) (0.3 – 1530.8)
Number of sessions, 103.3 126.3 122 87
Median (range) (20 - 597) (20 - 877) (20 - 877) (6 – 579)
Number and types of - - - -
cancers observed
Table 2: Summary of the therapeutic parameters for PUVA, NB-UVB and both modalities
3.3. Development of skin cancer
There was no skin cancer after phototherapy in this study. There was one patient who developed two lesions of BCC
on her nose and was treated eight months before the initiation of phototherapy, she received two-year-course of NB-
UVB for her psoriasis and there was no recurrence of skin cancer after five year follow up.
4. Discussion
In our retrospective study, the medical records of 956 patients treated with phototherapy were reviewed. Among the
726 whose records were analyzed. In this study, the most common underlying diseases was vitiligo, followed by
psoriasis. The majority of participants belonged to Fitzpatrick skin phototype III and IV. The most common
combination drug use with phototherapy was methotrexate, followed by azathioprine. There was no non-melanoma
skin cancer were observed in patients receiving phototherapy. Comparing with previous studies, in Europe a study
of 3,867 Scottish patients6, an increase risk of non-melanoma skin cancer among patients treated with both PUVA
and NB-UVB was reported with 27 BCCs found compared with 14.1 expected in the matched population [6]. The
risk of NMSC following long term NB-UVB and PUVA therapy has not been reported in Asian population. There
was one report from Korea that had only one patient who developed basal cell carcinoma four months after NB-
UVB phototherapy which was not statistically difference between NB-UVB and control group [7]. The low
incidence of non-melanoma skin cancer in our study and Korean study consistent with the previous study that
Arch Clin Biomed Res 2017; 1 (3): 116-121 120
explain by the effect of ethnicity on the risk of developing skin cancer [8]. Our negative study provide the important
information for the patient who need long term phototherapy. Long term NB-UVB and PUVA therapy seem to be
the safe therapeutics modalities for the patients with skin phototypes III-IV.
5. Limitations
This study was a retrospective study, so there could be some missing data and possible ascertainment bias.
Conclusions
This study did not show a significant increase in non-melanoma skin cancer risk among patients treated with long
term PUVA and NB-UVB. The results suggest that PUVA and NB-UVB are safe modalities.
References
1. Vangipuram R, Feldman SR. Ultraviolet phototherapy for cutaneous diseases: a concise review. Oral Dis 7
(2015): 1-7.
2. Cummings SR, Tripp MK, Herrmann NB. Approaches to the prevention and control of skin cancer. Cancer
Metastasis Rev 16 (1997): 309-327.
3. Stern R, Lunder E. Risk of squamous cell carcinoma and methoxsalen (psoralen) and UV-A radiation (PUVA):
a metaanalysis. Arch Dermatol 134 (1998): 1582-1585.
4. Stern R, Lange R. Non-melanoma skin cancer occurring in patients treated with PUVA five to ten years after
first treatment. J Invest Dermatol 91 (1988): 120-124.
5. Black RJ, Gavin AT. Photocarcinogenic risk of narrowband ultraviolet B (TL-01) phototherapy: early follow-
up data. Br J Dermatol 154 (2006): 566-567.
6. Hearn R, Kerr A, Rahim K, Ferguson J, Dawe R. Incidence of skin cancers in 3867 patients treated with
narrow-band ultraviolet B phototherapy. Br J Dermatol 159 (2008): 931-935.
7. Jo SJ, Kwon HH, Choi MR, Youn JI. No evidence for increased skin cancer risk in Koreans with skin
phototypes III-V treated with narrowband UVB phototherapy. Acta Derm Venereol 91 (2011): 40-43.
8. Murase J, Lee E, Koo J. Effect of ethnicity on the risk of developing nonmelanoma skin cancer following
long-term PUVA therapy. Int J Dermatol 44 (2004): 1016-1021.
9. Weischer M, Blum A, Eberhard F, et al. No evidence for increased skin cancer risk in psoriasis patients treated
with broadband or narrowband UVB phototherapy: a first retrospective study. Acta Derm Venereol 84 (2004):
370-374.
This article is an open access article distributed under the terms and conditions of the
Creative Commons Attribution (CC-BY) license 4.0
Arch Clin Biomed Res 2017; 1 (3): 116-121 121
Você também pode gostar
- The Yellow House: A Memoir (2019 National Book Award Winner)No EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Nota: 4 de 5 estrelas4/5 (98)
- A Randomized Controlled Trial of Intravenous Paracetamol and Intravenous Tramadol For Labour AnalgesiaDocumento11 páginasA Randomized Controlled Trial of Intravenous Paracetamol and Intravenous Tramadol For Labour AnalgesiaFortune JournalsAinda não há avaliações
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeNo EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeNota: 4 de 5 estrelas4/5 (5795)
- Avsm 004Documento7 páginasAvsm 004Fortune JournalsAinda não há avaliações
- Chemical Contaminants and Pollutants in The Measurable Life of Dhaka City PDFDocumento17 páginasChemical Contaminants and Pollutants in The Measurable Life of Dhaka City PDFFortune JournalsAinda não há avaliações
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureNo EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureNota: 4.5 de 5 estrelas4.5/5 (474)
- Cerebral Infarction in Risk Factor of Adenoma and Symptomatic Aortic Stenosis Case Report and Literature Reviewp PDFDocumento8 páginasCerebral Infarction in Risk Factor of Adenoma and Symptomatic Aortic Stenosis Case Report and Literature Reviewp PDFFortune JournalsAinda não há avaliações
- Capsicum Protects Against Rotenoneinduced Toxicity in Mice Brain Via Reduced Oxidative Stress and 5lipoxygenase Activationp PDFDocumento18 páginasCapsicum Protects Against Rotenoneinduced Toxicity in Mice Brain Via Reduced Oxidative Stress and 5lipoxygenase Activationp PDFFortune JournalsAinda não há avaliações
- Cancer Therapyinduced Cardiotoxicity Where Are We Now PDFDocumento8 páginasCancer Therapyinduced Cardiotoxicity Where Are We Now PDFFortune JournalsAinda não há avaliações
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryNo EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryNota: 3.5 de 5 estrelas3.5/5 (231)
- Biomineralogy of Angiogenesis PDFDocumento7 páginasBiomineralogy of Angiogenesis PDFFortune JournalsAinda não há avaliações
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceNo EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceNota: 4 de 5 estrelas4/5 (895)
- Biochemistry and Pathophysiology of Glycation of Dna Implications in Diabetes PDFDocumento16 páginasBiochemistry and Pathophysiology of Glycation of Dna Implications in Diabetes PDFFortune JournalsAinda não há avaliações
- Never Split the Difference: Negotiating As If Your Life Depended On ItNo EverandNever Split the Difference: Negotiating As If Your Life Depended On ItNota: 4.5 de 5 estrelas4.5/5 (838)
- Brian B. Adams-Sports Dermatology (2006)Documento362 páginasBrian B. Adams-Sports Dermatology (2006)Diana IscolniiAinda não há avaliações
- The Little Book of Hygge: Danish Secrets to Happy LivingNo EverandThe Little Book of Hygge: Danish Secrets to Happy LivingNota: 3.5 de 5 estrelas3.5/5 (400)
- 2020 - JCDT - Dermato and COVID-19 - Regina Jales and Santos-FilhoDocumento5 páginas2020 - JCDT - Dermato and COVID-19 - Regina Jales and Santos-FilhoSebastião David Santos-FilhoAinda não há avaliações
- Vulva Biopsias HistopatologiaDocumento10 páginasVulva Biopsias HistopatologiamariajoseoyanederAinda não há avaliações
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersNo EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersNota: 4.5 de 5 estrelas4.5/5 (345)
- SAMPLE CASE REPORT - Efficacy of Q-Switched ND YAG Laser in The Treatment of Freckles (ABNOM)Documento9 páginasSAMPLE CASE REPORT - Efficacy of Q-Switched ND YAG Laser in The Treatment of Freckles (ABNOM)dnaielAinda não há avaliações
- Dermatitis KuliahDocumento17 páginasDermatitis KuliahFirda LudfiyahAinda não há avaliações
- The Unwinding: An Inner History of the New AmericaNo EverandThe Unwinding: An Inner History of the New AmericaNota: 4 de 5 estrelas4/5 (45)
- Fadia Sherli Asyifa - 20210310068 - Ku 2Documento1 páginaFadia Sherli Asyifa - 20210310068 - Ku 2Lisa RLAinda não há avaliações
- Team of Rivals: The Political Genius of Abraham LincolnNo EverandTeam of Rivals: The Political Genius of Abraham LincolnNota: 4.5 de 5 estrelas4.5/5 (234)
- History and Epidemiology: Key FeaturesDocumento8 páginasHistory and Epidemiology: Key FeaturesAswin KrishnaAinda não há avaliações
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyNo EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyNota: 3.5 de 5 estrelas3.5/5 (2259)
- What Is ImpetigoDocumento4 páginasWhat Is ImpetigoKate Mylhen Espenido EnerlanAinda não há avaliações
- RNJDocumento6 páginasRNJVia RamaAinda não há avaliações
- BurnDocumento37 páginasBurnGLAZEL MAE MICANAinda não há avaliações
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaNo EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaNota: 4.5 de 5 estrelas4.5/5 (266)
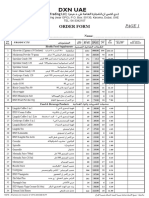
- Order Form UAE - 01-01-2023Documento2 páginasOrder Form UAE - 01-01-2023Mohammad BelalAinda não há avaliações
- The Emperor of All Maladies: A Biography of CancerNo EverandThe Emperor of All Maladies: A Biography of CancerNota: 4.5 de 5 estrelas4.5/5 (271)
- Common Skin Disorders in ChildrenDocumento79 páginasCommon Skin Disorders in ChildrenAhmed Noureldin AhmedAinda não há avaliações
- LSKDocumento4 páginasLSKAinia TaufiqaAinda não há avaliações
- Daftar Harga Distributor Per Mei 2023Documento10 páginasDaftar Harga Distributor Per Mei 2023martinAinda não há avaliações
- DermatosesDocumento12 páginasDermatosesnjoom100% (1)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreNo EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreNota: 4 de 5 estrelas4/5 (1090)
- ShopMy Where Elite Creators and Brands CollaborateDocumento1 páginaShopMy Where Elite Creators and Brands CollaborateRaquel MonacoAinda não há avaliações
- Pricelist Treatment Larissa CilacapDocumento11 páginasPricelist Treatment Larissa CilacapFitra BagasAinda não há avaliações
- Avano 2010Documento20 páginasAvano 2010omr4islamAinda não há avaliações
- Language of DermatologyDocumento45 páginasLanguage of DermatologykurutalaAinda não há avaliações
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)No EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Nota: 4.5 de 5 estrelas4.5/5 (121)
- K7 Jamur Superficial 2020Documento51 páginasK7 Jamur Superficial 2020Jimmy Fran IIAinda não há avaliações
- Rosacea Fulminans Triggered by High-Dose Vitamins B6 and B12Documento2 páginasRosacea Fulminans Triggered by High-Dose Vitamins B6 and B12PlantBasedNutritionAinda não há avaliações
- Augusts Consultations in Feline Internal Medicine, Volume 7, 1e (Susan Little DVM DABVP (Feline) )Documento1.077 páginasAugusts Consultations in Feline Internal Medicine, Volume 7, 1e (Susan Little DVM DABVP (Feline) )johnAinda não há avaliações
- Update Price List Terbaru Aug 22Documento159 páginasUpdate Price List Terbaru Aug 22Alfan FajrianAinda não há avaliações
- Dermatology Training ManualDocumento338 páginasDermatology Training ManualTewodros Demeke100% (2)
- Twenty One Pilots - CancerDocumento2 páginasTwenty One Pilots - CancerRaphael SaftaAinda não há avaliações
- Personal Care-Cleansing and Dressing, Skin Care Case History-Mrs. Mcbride New Vocabulary and Difficult WordsDocumento4 páginasPersonal Care-Cleansing and Dressing, Skin Care Case History-Mrs. Mcbride New Vocabulary and Difficult Wordsnadya wahyuAinda não há avaliações
- Urtikaria ReferatDocumento21 páginasUrtikaria ReferatRezki Tri Wahyuni SAinda não há avaliações
- Psoriasis - FINALDocumento33 páginasPsoriasis - FINALbrian mburuAinda não há avaliações
- Salin9-Form Sales Monitoring SPG'23 (Renewal)Documento1 páginaSalin9-Form Sales Monitoring SPG'23 (Renewal)rtia44429Ainda não há avaliações
- DAFTAR STOK RESELLER UpdateDocumento6 páginasDAFTAR STOK RESELLER UpdateSyahbuddinAinda não há avaliações