Escolar Documentos
Profissional Documentos
Cultura Documentos
Circulatory Shock
Enviado por
Dasha VeeDireitos autorais
Formatos disponíveis
Compartilhar este documento
Compartilhar ou incorporar documento
Você considera este documento útil?
Este conteúdo é inapropriado?
Denunciar este documentoDireitos autorais:
Formatos disponíveis
Circulatory Shock
Enviado por
Dasha VeeDireitos autorais:
Formatos disponíveis
PEDIATRICS 2
II. HYPOVOLEMIA-HEMMORHAGIC SHOCK
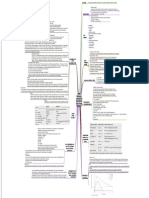
F.15 CIRCULATORY SHOCK AND PHYSIOLOGY OF ITS
TREATMENT HYPOVOLEMIA - diminished blood volume.
Dr. Balanag | May 09, 2019 HEMORRHAGE - most common cause of hypovolemic shock.
decreases the filling pressure
decreases venous return
OUTLINE: CO falls below normal, and shock may ensue
I. CIRCULATORY SHOCK
II. HYPOVOLEMIA-HEMMORHAGIC SHOCK
III. PROGRESSIVE VS. NON-PROGRESSIVE HEMORRHAGIC SHOCK
IV. IRREVERSIBLE SHOCK
V. HYPOVOLEMIC SHOCK
VI. NEUROGENIC SHOCK
VII. ANAPHYLACTIC SHOCK
VIII. SEPTIC SHOCK
IX. TREATMENT
I. CIRCULATORY SHOCK
State of acute circulatory dysfunction → failure of delivery of sufficient
oxygen and other nutrients to meet the metabolic demands of the
tissues. Since there is no more blood flow, acidosis happens. It
contributes to the vicious cycle. The more acidotic, the more it will
proliferate decrease in musculature, decrease in pumping of the
blood, decrease in the usage of nutrients. Acidosis begets further
acidosis. Eventually leading to shock. SYMPATHETIC REFLEX
Heart musculature, blood vessels, vasomotor system begins to 3 important effects:
deteriorate → once begun, is prone to become progressively worse 1. The arterioles CONSTRICT → increasing the TPR
2. The veins and venous reservoirs CONSTRICT → maintain adequate
CAUSES OF SHOCK venous return despite diminished blood volume
3. Heart activity INCREASES, to as high as 160 to 180 beats/min
1. DECREASED CARDIAC OUTPUT
In the absence of the sympathetic reflexes, only 15-20% of the BV
2 factors that can reduce cardiac output: can be removed over a period of 30 min before a person dies
CARDIAC ‒ myocardial infarction Sympathetic reflexes delays death by 2x
ABNORMALITIES ‒ toxic states of the heart ‒ geared more for maintaining arterial pressure than for
(just think of 3 ‒ severe heart valve dysfunction maintaining output
things: cardiac ‒ heart arrhythmias Second plateau at about 50 mm Hg
itself, preload & ‒ cardiogenic shock: 85% of people do not “last-ditch stand” - activation of the CNS ischemic response
after load) survive ‒ extreme stimulation of the sympathetic nervous system when the
DECREASE ‒ diminished blood volume brain begins to suffer from lack of oxygen or from excess build-
VENOUS RETURN ‒ decreased vascular tone up of carbon dioxide
‒ obstruction to blood flow
PROTECTION OF CORONARY/CEREBRAL BLOOD FLOW
2. WITHOUT DIMINISHED CARDIAC OUTPUT
AUTOREGULATION
a) excessive metabolism of the body Moderate decreases in arterial pressure from significantly
b) abnormal tissue perfusion patterns decreasing their blood flows.
Inadequate delivery of nutrients to critical tissues and critical organs ‒ blood flow through the heart and brain is maintained essentially
→ inadequate removal of cellular waste products from the tissues. at normal levels as long as the arterial pressure does not fall below
Vicious circle: Progressive circulatory shock → less adequate tissue about 70 mm Hg
perfusion → more shock → death
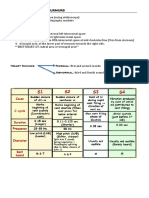
III. PROGRESSIVE VS.
STAGES OF SHOCK NONPROGRESSIVE HEMORRHAGIC SHOCK
1. NON-PROGRESSIVE STAGE (COMPENSATED STAGE): normal
circulatory compensatory mechanisms (neurohormonal) cause full
recovery without help from outside therapy
2. PROGRESSIVE STAGE: without therapy, the shock becomes steadily
worse until death.
3. IRREVERSIBLE STAGE: all forms of known therapy are inadequate to
save the person's life, even though, for the moment, the person is still
alive
Transcribers: DATUD, ALCANTARA, TOLIONGCO Page 1 of 4
PEDIATRICS 2
NON-PROGRESSIVE SHOCK In the early stages of shock:
Negative feedback control mechanisms ‒ plays very little role in the condition of the person
‒ Baroreceptor ‒ deterioration of the heart is not severe during the first hour
‒ Central nervous system ischemic response ‒ Heart has tremendous reserve capability (300 to 400%)
‒ Reverse stress-relaxation of the circulatory system Deterioration of the heart is the most important factor in the final
‒ Formation of angiotensin by the kidneys lethal progression of the shock.
‒ Formation of vasopressin (antidiuretic hormone) by the
posterior pituitary gland GENERALIZED CELLULAR DETERIORATION
‒ Compensatory mechanisms that return the blood volume back ‒ Diminished active transport of sodium and potassium
toward normal ‒ Mitochondrial activity depression
‒ Lysosomes break open
PROGRESSIVE SHOCK ‒ Cellular metabolism depression
FURTHER DETERIORATION OF ORGANS
Liver - depression of its many metabolic and detoxification functions
Lungs - eventual development of pulmonary edema and poor ability
to oxygenate the blood
Heart - further depressing its contractility
TISSUE NECROSIS IN SEVERE SHOCK-PATCHY AREAS OF
NECROSIS DUE TO PATCHY BLOOD FLOWS IN DIFFERENT
ORGANS
‒ Not all cells are equally damaged
‒ Cells adjacent to the arterial ends of capillaries receive better
nutrition than cells adjacent to the venous ends of the same
capillaries
‒ Similar punctate lesions occur in heart muscle, kidney tubules,
lungs (shock lung syndrome)
ACIDOSIS IN SHOCK
‒ anaerobic process of glycolysis → excess lactic acid
‒ Decreased removal of carbon dioxide
CO2 reacts locally in the cells with water to form carbonic
acid → local tissue acidosis → further progression of the
shock
IRREVERSIBLE SHOCK
“POSITIVE FEEDBACK” can lead to progression of shock
Positive feedback control mechanisms
‒ Cardiac Depression
‒ Vasomotor Failure
‒ Blockage of Very Small Vessels - "Sludged Blood”
‒ Increased Capillary Permeability
‒ Release of Toxins by Ischemic Tissue
‒ Cardiac Depression Caused by Endotoxin Transfusion during the irreversible stage can sometimes cause the
‒ Generalized Cellular Deterioration cardiac output (as well as the arterial pressure) to return to normal
Beyond a certain point
PROGRESSIVE DETERIORATION OF THE HEART AT DIFFERENT ‒ tissue damage
TIMES AFTER THE ONSET OF SHOCK ‒ destructive enzymes
‒ acidosis
Many other destructive factors have caused the continuing
deterioration
Depletion of Cellular High-Energy Phosphate Reserves in
Irreversible Shock
‒ Creatine phosphate → adenosine triphosphate → adenosine
diphosphate → adenosine monophosphate → adenosine →
diffuses out of the cells into the circulating blood → Converted
into uric acid → cannot re-enter the cells to reconstitute the
adenosine phosphate system
New adenosine can be synthesized at a rate of 2% of
the normal cellular amount an hour
‒ Cellular depletion of high-energy compounds
Transcribers: DATUD, ALCANTARA, TOLIONGCO Page 2 of 4
PEDIATRICS 2
Hypovolemic Shock Caused by Plasma Loss PHYSIOLOGY OF TREATMENT IN SHOCK
‒ Intestinal obstruction
‒ Severe burns 1. REPLACEMENT THERAPY
‒ Blood viscosity increases greatly → increased RBC
a. Blood and Plasma Transfusion
concentration → exacerbates the sluggishness of blood flow
If a person is in shock caused by hemorrhage, the best possible therapy
is usually transfusion of whole blood. If the shock is caused by plasma
HYPOVOLEMIC SHOCK loss, the best therapy is administration of plasma; when dehydration is
the cause, administration of an appropriate electrolyte solution can
DEHYDRATION - loss of fluid from all fluid compartments of the body correct the shock.
1. Excessive sweating
2. Fluid loss in severe diarrhea or vomiting Whole blood is not always available, such as under battlefield conditions.
3. Excess loss of fluid by nephrotic kidneys Plasma can usually substitute adequately for whole blood because it
4. Inadequate intake of fluid and electrolytes increases the blood volume and restores normal hemodynamics. Plasma
5. Destruction of the adrenal cortices, with loss of aldosterone cannot restore a normal hematocrit, but the human body can usually
secretion and consequent failure of the kidneys to reabsorb stand a decrease in hematocrit to about half of normal before serious
sodium, chloride, and water, which occurs in the absence of the consequences result, if cardiac output is adequate. Therefore, in
adrenocortical hormone aldosterone emergency conditions, it is reasonable to use plasma in place of whole
blood for treatment of hemorrhagic or most other types of hypovolemic
NEUROGENIC SHOCK shock.
Results without any loss of blood volume Sometimes plasma is unavailable. In these instances, various plasma
Vascular capacity increases so much substitutes have been developed that perform almost exactly the same
Sudden loss of vasomotor tone hemodynamic functions as plasma. One of these is dextran solution.
Causes of Neurogenic Shock:
‒ Deep general anesthesia b. Dextran Solution as a Plasma Substitute
‒ Spinal anesthesia The principal requirement of a truly effective plasma substitute is that it
‒ Brain damage remain in the circulatory system-that is, not filter through the capillary
pores into the tissue spaces. In addition, the solution must be nontoxic
ANAPHYLACTIC SHOCK and must contain appropriate electrolytes to prevent derangement of
the body's extracellular fluid electrolytes on administration.
ANAPHYLAXIS - an allergic condition in which the cardiac output and
2. SYMPATHOMIMETIC DRUG
arterial pressure often decrease drastically
‒ Results from an antigen-antibody formation A sympathomimetic drug is a drug that mimics sympathetic
‒ Basophils in the blood and mast cells in the pericapillary stimulation. These drugs include norepinephrine, epinephrine, and a
tissues to release histamine or a histamine-like substance large number of long-acting drugs that have the same effect as
epinephrine and norepinephrine.
1. venous dilation
2. dilation of the arterioles In two types of shock, sympathomimetic drugs have proved to be
3. greatly increased capillary permeability especially beneficial. The first of these is neurogenic shock, in which the
sympathetic nervous system is severely depressed. Administering a
‒ Intravenous injection of large amounts of histamine causes sympathomimetic drug takes the place of the diminished sympathetic
"histamine shock," which has characteristics almost identical actions and can often restore full circulatory function.
to those of anaphylactic shock
The second type of shock in which sympathomimetic drugs are
valuable is anaphylactic shock, in which excess histamine plays a
SEPTIC SHOCK
prominent role. The sympathomimetic drugs have a vasoconstrictor
effect that opposes the vasodilating effect of histamine. Therefore,
Bacterial infection widely disseminated to many areas of the body, either norepinephrine or another sympathomimetic drug is often
with the infection being borne through the blood from one tissue to lifesaving.
another and causing extensive damage.
Most frequent cause of shock-related death in the modern hospital Sympathomimetic drugs have not proved to be very valuable in
‒ Peritonitis e.g. instrumental abortion, ruptured viscus hemorrhagic shock. The reason is that in this type of shock, the
‒ Skin infection e.g. Streptococcal or Staphylococcal infection sympathetic nervous system is almost always maximally activated by the
‒ Gangrenous infection circulatory reflexes already; so much norepinephrine and epinephrine
‒ Urosepsis are already circulating in the blood that sympathomimetic drugs have
Special Features of Septic Shock essentially no additional beneficial effect.
‒ High fever
‒ Marked vasodilation 3. HEAD-DOWN POSITION
‒ High cardiac output
‒ High metabolic rate
4. OXYGEN THERAPY
‒ Sludging of the blood
‒ Disseminated intravascular coagulation
5. GLUCOCORTICOIDS (ADRENAL CORTEX HORMONES THAT
CONTROL GLUCOSE METABOLISM)
experiments have shown empirically that glucocorticoids
frequently increase the strength of the heart in the late stages of
shock
stabilize lysosomes in tissue cells
Aid in the metabolism of glucose by the severely damaged cells.
Transcribers: DATUD, ALCANTARA, TOLIONGCO Page 3 of 4
PEDIATRICS 2
CIRCULATORY ARREST
>5 - 8 min of total circulatory arrest → some degree of permanent
brain damage in more than half of patients
10 - 15 min almost always permanently destroys significant amounts
of mental power
Acute cerebral hypoxia that occurs during circulatory arrest
If blood clots are prevented from occurring in the brain → prevents
most of the early deterioration of the brain during circulatory arrest
All the blood was removed from the animal's blood vessels at
the beginning of circulatory arrest → replaced at the end of
circulatory arrest so that no intravascular blood clotting could
occur
Transcribers: DATUD, ALCANTARA, TOLIONGCO Page 4 of 4
Você também pode gostar
- A Simple Guide to Hypovolemia, Diagnosis, Treatment and Related ConditionsNo EverandA Simple Guide to Hypovolemia, Diagnosis, Treatment and Related ConditionsAinda não há avaliações
- Anterior Pituitary Gland: Fawwaz Ammari Laith & HaniDocumento22 páginasAnterior Pituitary Gland: Fawwaz Ammari Laith & HaniRashed ShatnawiAinda não há avaliações
- A Simple Guide to Circulatory Shock, Diagnosis, Treatment and Related ConditionsNo EverandA Simple Guide to Circulatory Shock, Diagnosis, Treatment and Related ConditionsAinda não há avaliações
- Cardiogenic ShockDocumento27 páginasCardiogenic ShockIgor StefanetAinda não há avaliações
- Head Injury 1Documento33 páginasHead Injury 1drvishal bhattAinda não há avaliações
- ShockDocumento7 páginasShockmara5140Ainda não há avaliações
- Care of The Hospitalized Patient With Acute Exacerbation of CopdDocumento25 páginasCare of The Hospitalized Patient With Acute Exacerbation of CopdmiallyannaAinda não há avaliações
- Inferior Wall ST Elevation (STEMI)Documento46 páginasInferior Wall ST Elevation (STEMI)Hendrik100% (1)
- Management of Patient With AnemiaDocumento58 páginasManagement of Patient With AnemiaDoaa HussainAinda não há avaliações
- FAELDONEA - B. Concept MapDocumento1 páginaFAELDONEA - B. Concept MapPatricia Jean FaeldoneaAinda não há avaliações
- AnemiasDocumento13 páginasAnemiasKaloy KamaoAinda não há avaliações
- CardiomyopathyDocumento1 páginaCardiomyopathyTrisha VergaraAinda não há avaliações
- Comprehensive Nursing Assessment For Care Plan: AllergiesDocumento14 páginasComprehensive Nursing Assessment For Care Plan: AllergiesBrittany ShrewsburyAinda não há avaliações
- Coronary Artery DiseaseDocumento2 páginasCoronary Artery DiseaseDarell M. BookAinda não há avaliações
- Patent Ductus Arteriosus 6. Aortic Stenosis: Signs and Symptoms: Signs and SymptomsDocumento3 páginasPatent Ductus Arteriosus 6. Aortic Stenosis: Signs and Symptoms: Signs and SymptomsKIANA LOUISE ROMANOAinda não há avaliações
- Taufan Arif, S.Kep., NS., M.KepDocumento85 páginasTaufan Arif, S.Kep., NS., M.KepputriAinda não há avaliações
- Spinal Cord Injury Spinal Cord InjuriesDocumento6 páginasSpinal Cord Injury Spinal Cord InjuriesJamaica Leslie NovenoAinda não há avaliações
- CVPDocumento25 páginasCVPNikhil YadavAinda não há avaliações
- Shock With Hemodynamic ChangesDocumento2 páginasShock With Hemodynamic ChangesBNA_RN100% (1)
- Emergency Management of Patients With Drug OverdoseDocumento6 páginasEmergency Management of Patients With Drug Overdosetheglobalnursing0% (1)
- (MED1) 3.04 Approach To Hypertension (Dr. Bago-Azares)Documento11 páginas(MED1) 3.04 Approach To Hypertension (Dr. Bago-Azares)NoreenAinda não há avaliações
- Pulmonary Diseases - Dental ManagementDocumento45 páginasPulmonary Diseases - Dental Managementfilyouth4life100% (3)
- SBARQ FormDocumento1 páginaSBARQ FormTracy100% (5)
- Neuro Notes #3Documento11 páginasNeuro Notes #3Monica JubaneAinda não há avaliações
- PneumoniaDocumento53 páginasPneumoniaAtif100% (1)
- Types of Shock TableDocumento6 páginasTypes of Shock TableTP RMadAinda não há avaliações
- NUR100 Sherpath Skin Overview + Skin IntegrityDocumento15 páginasNUR100 Sherpath Skin Overview + Skin Integritycaloy2345caloy100% (1)
- Cardiac PathophysiologyDocumento83 páginasCardiac PathophysiologyJauhar Anindita SariAinda não há avaliações
- Acute Stroke Nursing GuidelineFINAL 1 2Documento5 páginasAcute Stroke Nursing GuidelineFINAL 1 2radanikmaAinda não há avaliações
- A Clinical Approach To SyncopeDocumento8 páginasA Clinical Approach To Syncopepuskesmas tarik100% (1)
- Congestive Heart FailureDocumento24 páginasCongestive Heart FailureKoka KolaAinda não há avaliações
- HivDocumento36 páginasHivfenendriyaniAinda não há avaliações
- Chapter 42 - Sepsis, Septic Shock, and Multiple Organ FailureDocumento15 páginasChapter 42 - Sepsis, Septic Shock, and Multiple Organ FailureWorrawalun FuktongAinda não há avaliações
- Early and Late Signs of Increased Intracranial PressureDocumento8 páginasEarly and Late Signs of Increased Intracranial PressureRhae Raynog100% (2)
- Adult Tachycardia With A Pulse Algorithm: Doses/DetailsDocumento1 páginaAdult Tachycardia With A Pulse Algorithm: Doses/DetailsAlexis HospitalAinda não há avaliações
- Pediatric Cardio-Respiratory AssessmentDocumento9 páginasPediatric Cardio-Respiratory AssessmentRicky SpideyAinda não há avaliações
- Rheumatic Fever and Rheumatic Heart DiseaseDocumento132 páginasRheumatic Fever and Rheumatic Heart DiseaseDamie FernandezAinda não há avaliações
- Pain 2. Pallor Poikylothermia Parasthesia Pulselessness Factor V Leiden (Activated Protein C Resistance)Documento3 páginasPain 2. Pallor Poikylothermia Parasthesia Pulselessness Factor V Leiden (Activated Protein C Resistance)Ryan TurnerAinda não há avaliações
- Lifestyle DiseasesDocumento44 páginasLifestyle Diseaseskyro draxAinda não há avaliações
- Electrolyte DisordersDocumento10 páginasElectrolyte DisordersSlavicaAinda não há avaliações
- The Integrated Management of Childhood IllnessesDocumento32 páginasThe Integrated Management of Childhood IllnessesKrishna PhulpagarAinda não há avaliações
- Shock and SIRSDocumento85 páginasShock and SIRSBryan Mae H. DegorioAinda não há avaliações
- Valvular Heart DseDocumento8 páginasValvular Heart DseJane Pineda CuraAinda não há avaliações
- Shock, Sirs & ModsDocumento37 páginasShock, Sirs & ModsambitioustamannaAinda não há avaliações
- Evaluation and Management of Suspected Sepsis and Septic Shock in AdultsDocumento62 páginasEvaluation and Management of Suspected Sepsis and Septic Shock in AdultsGiussepe Chirinos CalderonAinda não há avaliações
- PericarditisDocumento29 páginasPericarditisPavin KumarAinda não há avaliações
- SHOCK Slide WorkbookDocumento10 páginasSHOCK Slide WorkbookPATHMAPRIYA GANESANAinda não há avaliações
- Hepatobiliary Disorders: Katrina Saludar Jimenez, R. NDocumento42 páginasHepatobiliary Disorders: Katrina Saludar Jimenez, R. NKatrinaJimenezAinda não há avaliações
- MED - Finals 1.5 - Asthma PDFDocumento12 páginasMED - Finals 1.5 - Asthma PDFYestin Reece Corpus ArcegaAinda não há avaliações
- 7th Heart Sounds and MurmursDocumento6 páginas7th Heart Sounds and MurmursbabibubeboAinda não há avaliações
- Low of Blood Flow ShockDocumento2 páginasLow of Blood Flow ShockBNA_RNAinda não há avaliações
- Acute Coronary SyndromesDocumento1 páginaAcute Coronary SyndromesCamilo VidalAinda não há avaliações
- Management of Infective EndocarditisDocumento14 páginasManagement of Infective Endocarditismhafzam2020Ainda não há avaliações
- PnemoniaDocumento4 páginasPnemoniadhavalAinda não há avaliações
- Cardiac TamponadeDocumento10 páginasCardiac TamponadevineeshAinda não há avaliações
- Endocrine System Anatomy and Physiology - NurseslabsDocumento29 páginasEndocrine System Anatomy and Physiology - NurseslabsAlyssum Marie50% (2)
- Chronic Renal Failure (Handout)Documento3 páginasChronic Renal Failure (Handout)rhizzyAinda não há avaliações
- ShockDocumento21 páginasShockMin-Joo Esther ParkAinda não há avaliações
- Surviving Sepsis Campaign 2016 Guidelines Presentation FinalDocumento60 páginasSurviving Sepsis Campaign 2016 Guidelines Presentation FinalCocosul Cocosului CocosaruluiAinda não há avaliações
- Traumatic Lesions: Head Injuries: Delano, Alexandra Julianne Duran, Fatima MedrizaDocumento31 páginasTraumatic Lesions: Head Injuries: Delano, Alexandra Julianne Duran, Fatima MedrizaFatima Medriza Duran100% (1)
- F.08 PULMONARY DISEASES IN PREGNANCY (Dr.-Badua) 5-7-2019Documento5 páginasF.08 PULMONARY DISEASES IN PREGNANCY (Dr.-Badua) 5-7-2019Dasha VeeAinda não há avaliações
- Philippine Journal of Gynecologic Oncology Volume 9 Number 1 2012Documento48 páginasPhilippine Journal of Gynecologic Oncology Volume 9 Number 1 2012Dasha VeeAinda não há avaliações
- Diagnostico y Manejo de Masas AnexialesDocumento6 páginasDiagnostico y Manejo de Masas AnexialesChristopher Hernán Valenzuela ArancibiaAinda não há avaliações
- WJR 5 113Documento13 páginasWJR 5 113Valian IndrianyAinda não há avaliações
- The Characteristic Ultrasound Features of Specific Types of Ovarian Pathology (Review) PDFDocumento14 páginasThe Characteristic Ultrasound Features of Specific Types of Ovarian Pathology (Review) PDFDasha VeeAinda não há avaliações
- F.07 STD AND INFECTIONS IN PREGNANCY (DR - Jandoc) 05-03-2019 (Part 2)Documento3 páginasF.07 STD AND INFECTIONS IN PREGNANCY (DR - Jandoc) 05-03-2019 (Part 2)Dasha VeeAinda não há avaliações
- OB OSCE.06 OB GYNE ULTRASOUND (Dr. Ursua) PDFDocumento1 páginaOB OSCE.06 OB GYNE ULTRASOUND (Dr. Ursua) PDFDasha VeeAinda não há avaliações
- Practice Bulletin: Management of Adnexal MassesDocumento14 páginasPractice Bulletin: Management of Adnexal MassesDasha VeeAinda não há avaliações
- F.01 NEUROLOGIC AND PSYCHIATRIC DISEASES IN PREGNANCY (Dr. Arcellan) 04-10-2019 PDFDocumento10 páginasF.01 NEUROLOGIC AND PSYCHIATRIC DISEASES IN PREGNANCY (Dr. Arcellan) 04-10-2019 PDFDasha VeeAinda não há avaliações
- F.07 STD AND INFECTIONS IN PREGNANCY (DR - Jandoc) 05-03-2019 (Part 2)Documento3 páginasF.07 STD AND INFECTIONS IN PREGNANCY (DR - Jandoc) 05-03-2019 (Part 2)Dasha VeeAinda não há avaliações
- F.03 HEMATOLOGIC DISEASES IN PREGNANCY (DR - Taguiling) 04-25-2019 (Part 1) PDFDocumento4 páginasF.03 HEMATOLOGIC DISEASES IN PREGNANCY (DR - Taguiling) 04-25-2019 (Part 1) PDFDasha VeeAinda não há avaliações
- F.08 PULMONARY DISEASES IN PREGNANCY (Dr.-Badua) 5-7-2019Documento5 páginasF.08 PULMONARY DISEASES IN PREGNANCY (Dr.-Badua) 5-7-2019Dasha VeeAinda não há avaliações
- F.02 DERMATOLOGIC DISEASES IN PREGNANCY (Dr. Taguiling) 04-12-2019 PDFDocumento5 páginasF.02 DERMATOLOGIC DISEASES IN PREGNANCY (Dr. Taguiling) 04-12-2019 PDFDasha VeeAinda não há avaliações
- P.09 OBSTETRIC HEMORRHAGE (Dr. Ursua) 02-07-2019 (Part 1)Documento3 páginasP.09 OBSTETRIC HEMORRHAGE (Dr. Ursua) 02-07-2019 (Part 1)Dasha VeeAinda não há avaliações
- Mental HealthDocumento4 páginasMental HealthDasha VeeAinda não há avaliações
- F.06 STD and Infections in Pregnancy (Dr. Jandoc) 05-03-2019 (Part 1)Documento5 páginasF.06 STD and Infections in Pregnancy (Dr. Jandoc) 05-03-2019 (Part 1)Dasha VeeAinda não há avaliações
- Embryogenesis & Fetal DevelopementDocumento38 páginasEmbryogenesis & Fetal DevelopementDasha Vee100% (1)
- DiagnosisDocumento8 páginasDiagnosisDasha VeeAinda não há avaliações
- P.07 Thyroid and Parathyroid Glands Dr. Manalo 9-8-16Documento4 páginasP.07 Thyroid and Parathyroid Glands Dr. Manalo 9-8-16Dasha VeeAinda não há avaliações
- Obstetrics 2: Obstetric Hemorrhage (Part 2)Documento4 páginasObstetrics 2: Obstetric Hemorrhage (Part 2)Dasha VeeAinda não há avaliações
- 2011 Full Page Calendar - TomKat StudioDocumento12 páginas2011 Full Page Calendar - TomKat StudioThe TomKat StudioAinda não há avaliações
- F.09 BONE RADIOLOGY - Dr. GalangDocumento11 páginasF.09 BONE RADIOLOGY - Dr. GalangDasha VeeAinda não há avaliações
- Thyroid PDFDocumento9 páginasThyroid PDFDasha VeeAinda não há avaliações
- Philippine CPG On The Diagnosis and Management of Urinary Tract Infections in Adults-2015 Update - Part 2 PDFDocumento140 páginasPhilippine CPG On The Diagnosis and Management of Urinary Tract Infections in Adults-2015 Update - Part 2 PDFspringdingAinda não há avaliações
- m.10b Drugs Used in Gastrointestinal Diseases 03-26-18 (Table)Documento3 páginasm.10b Drugs Used in Gastrointestinal Diseases 03-26-18 (Table)Dasha VeeAinda não há avaliações
- Ob Osce.04 CTG ReadingDocumento6 páginasOb Osce.04 CTG ReadingDasha VeeAinda não há avaliações
- Antiviral Chemotherapy and Prophylaxis: Acyclovir, Valacyclovir, and FamciclovirDocumento8 páginasAntiviral Chemotherapy and Prophylaxis: Acyclovir, Valacyclovir, and FamciclovirDasha VeeAinda não há avaliações
- m.13 Dietary Supplements & Herbal Medications (Dr. Buñag) 04-04-18Documento4 páginasm.13 Dietary Supplements & Herbal Medications (Dr. Buñag) 04-04-18Dasha VeeAinda não há avaliações
- F.08 Death CertificateDocumento7 páginasF.08 Death CertificateDasha VeeAinda não há avaliações
- f.02 Intellectual Disabilities (Dr. Rebucal) 04-11-2019Documento4 páginasf.02 Intellectual Disabilities (Dr. Rebucal) 04-11-2019Dasha VeeAinda não há avaliações
- Week 3 PATIENTS RIGHTS AND RESPONSIBILITIES 19-20Documento32 páginasWeek 3 PATIENTS RIGHTS AND RESPONSIBILITIES 19-20maha abdallahAinda não há avaliações
- 1111 - USP Micro Limit Test For Non SterileDocumento2 páginas1111 - USP Micro Limit Test For Non SterileSpectre SpectreAinda não há avaliações
- Monkeypox: VirusDocumento18 páginasMonkeypox: Virusdiela dwi lestariAinda não há avaliações
- Umbilical Cord Blood BankingDocumento290 páginasUmbilical Cord Blood BankingcmAinda não há avaliações
- Concept of Health EducationDocumento14 páginasConcept of Health EducationYou PanhamorokotAinda não há avaliações
- Project PrimaryDocumento7 páginasProject PrimaryLisanwork HonseboAinda não há avaliações
- ED Produk KF - KF (Nama Apotek)Documento19 páginasED Produk KF - KF (Nama Apotek)Eko FebryandiAinda não há avaliações
- 9c5a4module 2 Self EsteemDocumento14 páginas9c5a4module 2 Self EsteemHarshita Jakhodia100% (1)
- Health Economics: Which of The Following Is Not A Reason For Increased Health Spending?Documento8 páginasHealth Economics: Which of The Following Is Not A Reason For Increased Health Spending?Arjun Aryal100% (1)
- Gluten Free Living-3Documento29 páginasGluten Free Living-3api-266549998Ainda não há avaliações
- Application Form For Accreditation SPDocumento4 páginasApplication Form For Accreditation SPMyk Twentytwenty NBeyondAinda não há avaliações
- Report Decentralised Planning Kerala 2009 OommenDocumento296 páginasReport Decentralised Planning Kerala 2009 OommenVaishnavi JayakumarAinda não há avaliações
- Water For Health 1Documento23 páginasWater For Health 1nyoman fitriAinda não há avaliações
- Miranda Miracell NewDocumento2 páginasMiranda Miracell NewPablo FaldutiAinda não há avaliações
- Sonographic Evaluation of The DiaphragmDocumento1 páginaSonographic Evaluation of The DiaphragmAngelo LongoniAinda não há avaliações
- Karyotype WorksheetDocumento4 páginasKaryotype WorksheetKellieM.8406Ainda não há avaliações
- M265 Lec 13 - Epidemiology and Public HealthDocumento10 páginasM265 Lec 13 - Epidemiology and Public HealthSawsan Z. JwaiedAinda não há avaliações
- PDFDocumento278 páginasPDFmahesh babu100% (1)
- Surgical Handicraft Manual For Surgical Residents 2015 PDFDocumento295 páginasSurgical Handicraft Manual For Surgical Residents 2015 PDFNamerahN100% (3)
- KT PDO Thread Training Stage 1 and 2 OverviewDocumento55 páginasKT PDO Thread Training Stage 1 and 2 OverviewMetin Sabuncu100% (3)
- RCI-CEL-AZA PEME FormA-Rev09-2019 FormB MedCertDocumento8 páginasRCI-CEL-AZA PEME FormA-Rev09-2019 FormB MedCertVhal AlbientoAinda não há avaliações
- ESICM/ESCMID Task Force On Practical Management of Invasive Candidiasis in Critically Ill PatientsDocumento17 páginasESICM/ESCMID Task Force On Practical Management of Invasive Candidiasis in Critically Ill PatientsrennerrsAinda não há avaliações
- Is Iso 10555 1 1995Documento21 páginasIs Iso 10555 1 1995Hemant SharmaAinda não há avaliações
- Defluoridation of Ground WaterDocumento12 páginasDefluoridation of Ground WaterNikitha PerumallaAinda não há avaliações
- The Superheroes of PharmaDocumento13 páginasThe Superheroes of PharmaMPAAinda não há avaliações
- Hardy Et Al-2018-Australian and New Zealand Journal of Public HealthDocumento5 páginasHardy Et Al-2018-Australian and New Zealand Journal of Public HealthAnggita RifkyAinda não há avaliações
- New Form 6 Leave Form TEACHERSDocumento2 páginasNew Form 6 Leave Form TEACHERSmarites mercedAinda não há avaliações
- Jurnal GadarDocumento6 páginasJurnal GadarLycia Dwi LindiyaniAinda não há avaliações
- TASSDocumento11 páginasTASSNike KeketAinda não há avaliações
- Female Foeticide in India A Bitter Truth FinalDocumento22 páginasFemale Foeticide in India A Bitter Truth Finalaman manderAinda não há avaliações