Escolar Documentos
Profissional Documentos
Cultura Documentos
Anaphylaxis, Hypersensitivity and Adverse Drug Reactions
Enviado por
Dasha Vee0 notas0% acharam este documento útil (0 voto)
15 visualizações2 páginasana
Direitos autorais
© © All Rights Reserved
Formatos disponíveis
PDF, TXT ou leia online no Scribd
Compartilhar este documento
Compartilhar ou incorporar documento
Você considera este documento útil?
Este conteúdo é inapropriado?
Denunciar este documentoana
Direitos autorais:
© All Rights Reserved
Formatos disponíveis
Baixe no formato PDF, TXT ou leia online no Scribd
0 notas0% acharam este documento útil (0 voto)
15 visualizações2 páginasAnaphylaxis, Hypersensitivity and Adverse Drug Reactions
Enviado por
Dasha Veeana
Direitos autorais:
© All Rights Reserved
Formatos disponíveis
Baixe no formato PDF, TXT ou leia online no Scribd
Você está na página 1de 2
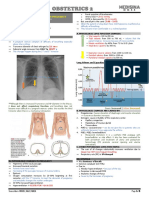
MEDICINE 2
F.24A ANAPHYLAXIS, HYPERSENSITIVITY AND ADVERSE
DRUG REACTIONS (Part 1)
Dr. Dominguez (2019 lecture) | May 7, 2019
I. OUTLINE
I. OUTLINE
II. CASE
III. ANAPHYLAXIS
a. Clinical Criteria
b. Risk Factors
c. Diagnosis
d. Treatment
i. First line treatment
ii. Second line treatment
iii. Long term management
e. Prevention
f. Adverse Drug Reactions
Outcome: Diagnose and develop management plan
*All are secreted by mast cell (Central to the development of
anaphylaxis)
II. CASE
• 25 year old female RISK FACTORS
• Sudden dyspnea and wheezing after • Atopy → recurrent pruritus and lesions on elbows, neck,
intake of Ibuprofen popliteal area, and other areas with skin folds, allergy to latex,
• BP: 70/40 dermatographism
• Severe respiratory distress • Older age
• Beta blockers→can cause bronchoconstriction
• Preexisting asthma→asthma attacks that has been intermittent
• Always ask these in history
CLASSIFICATION OF ALLERGENS (BY WORLD RANK)
• By skin contact:
o Poison plant - No
poison ivy in the
Philipppines
o Animal scratches
• Swelling of mucosal surfaces- Angioedema o Pollen, mold and
• Hives are demarcated and elevated mildew: common
• Diagnosis: Anaphylactic shock because of the blood pressure here specially if
season is
III. ANAPHYLAXIS changing from
CLINICAL CRITERIA cold to summer.
1. Acute onset of skin &/or mucosal lesions + respiratory symptoms or o Latex gloves
reduced BP/end-organ dysfunction • Injection:
• Acute: Occurs within minutes to few hours after exposure to o Bee sting
suspected allergen • Ingestion:
• Skin and mucosal: Urticarial, wheals, hives, angioedema o Medications: any medication could cause anaphylaxis
• Respiratory symptoms: wheezing, stridor (indicative of ▪ MC: Ibuprofen, penicillin, Radiocontrast media
upper respiratory tract obstruction/ laryngeal area) even ▪ A negative skin test is not 100% reliable
hypoxemia, or possible respiratory distress, increased RR, o Nuts and shellfish
poor air entry • Inhalation:
• End organ-damage: Sometimes with neurologic symptoms o Pollen, dusts
(loss of consciousness), syncope with/without o Mold and mildew
incontinence o Animal dander: are there pets inside the house?
2. ≥2 after exposure to likely allergen: skin, respiratory symptoms,
MECHANISM TRIGGERS
hypotension, GI symptoms
• Can present with uterine contractions in pregnant women Immunologic Food, venoms, drugs, NRL, aero allergens,
• GI: abdominal pain, vomiting and diarrhea. This is because (IgE dependent) seminal fluid
the intestines are also swollen
3. Hypotension after exposure to known allergen
Non-immunologic RCM, narcotics, NSAIDs, ASA, dextrans,
• The allergen has already been established on the patient.
(Direct mast cell exercise, cold, heat, sunlight, ethanol,
Confirmed and documented allergy
activation) sulfiting agents
• Hypotension as a result of widespread vasodilation due to
histamine
• Histamine→ widespread vasodilation→ increased vascular NRL – natural rubber latex
permeability → increased bronchial constriction RCM – radiocontrast media
• Has undergone skin test before Food: most common trigger for anaphylaxis in children and young
• Anaphylactic shock- if patient is already hypotensive; adults
will change the management entirely Drugs and bee stings: most common in elderly and adults
Transcribers: DE VERA E, BONIFACIO, GERVERO Page 1 of 2
MEDICINE 2
DIAGNOSIS o Methylprednisolone: the best to give
• History and PE (mainly clinical) o Hydrocortisone
• Prausnitz-Kustner reaction o May take several hours to be effective
(old, not done in practice
anymore) LONG TERM MANAGEMENT
o Employs injecting sera • Epinephrine autoinjectors/kit
containing IgE; after few o Contains 1 ampule
hours, inject antigen and epinephrine, 1 syringe and
see if there are anti-histamine tablets
development of wheals • Anaphylaxis alert tags
urticaria, etc. • Confirm anaphylaxis triggers
o Like passive immunity test. o Allergen-specific serum IgE
o Problem: danger of transmitting blood-borne levels to particular allergen
infection so this is just a historical test. o Skin tests
▪ Refer to allergologist
▪ Not done on admission of the anaphylactic episode
• Immunoassays → Introduce a known panel of antigens and • Avoidance
measure IgE levels o Avoid known triggers - If patient developed anaphylaxis due
• Intracutaneous skin testing → Done to confirm to what to drugs, avoid drugs for 5 years; if allergic to high protein
allergen the patient has been reactive to. Done after 3-4 foods, avoid for 5 years also (like nuts or foods from trees) ;
weeks after the anaphylactic reaction to make sure that it’s other types of food, avoid for at least 6 months
not due to the previous response; bread and butter of allergologist. o Allergy to excipients - take in drugs that are white in color;
• Serum Tryptase level →Tryptase is elevated in anaphylaxis avoid highly colored medications. Patient did not develop
but has very short half life; golden period is 4 hours from onset of allergy to the drugs but to the excipients
anaphylaxis. Not very effective in allergic reactions to food; • Medication desensitization
tryptase will not rise. o Patient needs the drug BUT is allergic to it, (-) alternative
medication
TREATMENT o Done within 24hours
1st LINE TREATMENT o Start with minimum dose → full dosed is reached → patient
• Epinephrine becomes desensitized → then drug is given by allergologist
o Mechanism of action: Vasoconstriction (to reduce hives and o May have anaphylactic shock anytime
swelling) and bronchodilation.
PREVENTION
o Dose: 0.3 to 0.5 ml at 1:1,000 dilution.
• For drug allergies
o Can be IM, IV or SubQ, maximum of 3 doses.
o Select structurally unrelated agent → Avoid giving 1st gen
o Can be with those with cardiac disease. Can feel numbness or
cephalosporins to penicillin-allergic patients because these
coldness of injection site.
drugs have the same nucleus; you may give 3rd gen
cephalosporins
Other Management for Shock
• Skin testing
• Fluid resuscitation
o Do scratch test first. Control is always on the left arm. Active
o If you have to fast drip with 1 L, then do it
drug is always on the right arm in skin tests.
o No actual loss of fluid but there is just relative fluid loss due
▪ Control (+) and Drug (+) →Repeat test
to excessive vasodilation → thus fill up the veins with fluid →
▪ Control (-) and Drug (+) →Positive result
goal is to increase blood pressure
▪ Control (-) and Drug (-) →Negative result
o Best: Isotonic Solution (PNSS, LRS, RS)
o If scratch test is negative, go to intradermal
o Rate is same with other kinds of shock
o If negative on both scratch and intradermal test, you are sure
o Replacement: less aggressive
that patient is really negative
o Age is not a contraindication
o Skin test for antibiotics is no longer recommended.
o Rate: 10-20 cc/kg to run for 1 hour
• Desensitization → (filling up IgEs with antigens).
• IV epinephrine vasopressors o Give first half of the computed dose as an infusion,
o Epinephrine IV 1:10,000 of 2.5 ml epinephrine or 1:100,000 watch out for reaction within 15 minutes;
dilution or other vasopressors o if no reaction, give ¼; if no reaction again, give the remaining
o Let it run for 5-10 minutes ¼ dose. If no reaction you may give the next dose in
o May use dobutamine or dopamine as an alternative full
• Oxygen inhalation/intubation ADVERSE DRUG REACTIONS
o When patient is in respiratory distress→intubate the patient Patient injury caused by a medicine taken in therapeutic doses
o Problem: Severe laryngeal swelling → difficult to intubate the
patient (done by anesthesiologist) Call the experts! Exaggerated pharmacological response
TYPE A
o Tracheostomy is done if intubation is not possible (develops bronchospasm from beta-blockers)
Nonpharmacological, often allergic response
TYPE B
SECOND LINE MANAGEMENT (all hypersensitivity reactions)
• Antihistamines Continuous or long term (time related)
Diphenhydramine is the best to give 50-100 mg IM or IV TYPE C
o (osteoporosis related to the use of steroids)
every 6 hrs; side effect: drowsiness Delayed (lag time)
o 2nd Gen (Loratadine, Cetirizine) TYPE D
(teratogenic effects of the drugs)
o 1st Generation (Diphenhydramine, Chlorphenamine) → Given Ending of use (withdrawal)
when patient is already stable TYPE E (when you suddenly withdraw clonidine then develops
• Beta-2-adrenergic agonists, aminophylline hypertension)
o To address the bronchospasm – causes bronchodilation Failure of efficacy (no response)
o Salbutamol, Albuterol, Terbutaline TYPE F
(resistance to antibiotics)
• IV glucocorticoids
Transcribers: DE VERA E, BONIFACIO, GERVERO Page 2 of 2
Você também pode gostar
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryNo EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryNota: 3.5 de 5 estrelas3.5/5 (231)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)No EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Nota: 4.5 de 5 estrelas4.5/5 (119)
- Never Split the Difference: Negotiating As If Your Life Depended On ItNo EverandNever Split the Difference: Negotiating As If Your Life Depended On ItNota: 4.5 de 5 estrelas4.5/5 (838)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaNo EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaNota: 4.5 de 5 estrelas4.5/5 (265)
- The Little Book of Hygge: Danish Secrets to Happy LivingNo EverandThe Little Book of Hygge: Danish Secrets to Happy LivingNota: 3.5 de 5 estrelas3.5/5 (399)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyNo EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyNota: 3.5 de 5 estrelas3.5/5 (2219)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeNo EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeNota: 4 de 5 estrelas4/5 (5794)
- Team of Rivals: The Political Genius of Abraham LincolnNo EverandTeam of Rivals: The Political Genius of Abraham LincolnNota: 4.5 de 5 estrelas4.5/5 (234)
- The Emperor of All Maladies: A Biography of CancerNo EverandThe Emperor of All Maladies: A Biography of CancerNota: 4.5 de 5 estrelas4.5/5 (271)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreNo EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreNota: 4 de 5 estrelas4/5 (1090)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersNo EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersNota: 4.5 de 5 estrelas4.5/5 (344)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceNo EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceNota: 4 de 5 estrelas4/5 (890)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureNo EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureNota: 4.5 de 5 estrelas4.5/5 (474)
- The Unwinding: An Inner History of the New AmericaNo EverandThe Unwinding: An Inner History of the New AmericaNota: 4 de 5 estrelas4/5 (45)
- The Yellow House: A Memoir (2019 National Book Award Winner)No EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Nota: 4 de 5 estrelas4/5 (98)
- Soil Loss EstimationDocumento77 páginasSoil Loss Estimationmys85Ainda não há avaliações
- Cakes Amp Sugarcraft - April-May 2019 EditDocumento45 páginasCakes Amp Sugarcraft - April-May 2019 Editapi-197110397100% (1)
- F.01 NEUROLOGIC AND PSYCHIATRIC DISEASES IN PREGNANCY (Dr. Arcellan) 04-10-2019 PDFDocumento10 páginasF.01 NEUROLOGIC AND PSYCHIATRIC DISEASES IN PREGNANCY (Dr. Arcellan) 04-10-2019 PDFDasha VeeAinda não há avaliações
- EVA and MVADocumento19 páginasEVA and MVATanveer Ahmad100% (1)
- F.07 STD AND INFECTIONS IN PREGNANCY (DR - Jandoc) 05-03-2019 (Part 2)Documento3 páginasF.07 STD AND INFECTIONS IN PREGNANCY (DR - Jandoc) 05-03-2019 (Part 2)Dasha VeeAinda não há avaliações
- Pulmonary Disorders in PregnancyDocumento5 páginasPulmonary Disorders in PregnancyDasha VeeAinda não há avaliações
- Philippine Journal of Gynecologic Oncology Volume 9 Number 1 2012Documento48 páginasPhilippine Journal of Gynecologic Oncology Volume 9 Number 1 2012Dasha VeeAinda não há avaliações
- OB OSCE.06 OB GYNE ULTRASOUND (Dr. Ursua) PDFDocumento1 páginaOB OSCE.06 OB GYNE ULTRASOUND (Dr. Ursua) PDFDasha VeeAinda não há avaliações
- The Characteristic Ultrasound Features of Specific Types of Ovarian Pathology (Review) PDFDocumento14 páginasThe Characteristic Ultrasound Features of Specific Types of Ovarian Pathology (Review) PDFDasha VeeAinda não há avaliações
- Practice Bulletin: Management of Adnexal MassesDocumento14 páginasPractice Bulletin: Management of Adnexal MassesDasha VeeAinda não há avaliações
- Diagnostico y Manejo de Masas AnexialesDocumento6 páginasDiagnostico y Manejo de Masas AnexialesChristopher Hernán Valenzuela ArancibiaAinda não há avaliações
- Pulmonary Disorders in PregnancyDocumento5 páginasPulmonary Disorders in PregnancyDasha VeeAinda não há avaliações
- WJR 5 113Documento13 páginasWJR 5 113Valian IndrianyAinda não há avaliações
- F.02 DERMATOLOGIC DISEASES IN PREGNANCY (Dr. Taguiling) 04-12-2019 PDFDocumento5 páginasF.02 DERMATOLOGIC DISEASES IN PREGNANCY (Dr. Taguiling) 04-12-2019 PDFDasha VeeAinda não há avaliações
- F.03 HEMATOLOGIC DISEASES IN PREGNANCY (DR - Taguiling) 04-25-2019 (Part 1) PDFDocumento4 páginasF.03 HEMATOLOGIC DISEASES IN PREGNANCY (DR - Taguiling) 04-25-2019 (Part 1) PDFDasha VeeAinda não há avaliações
- F.07 STD AND INFECTIONS IN PREGNANCY (DR - Jandoc) 05-03-2019 (Part 2)Documento3 páginasF.07 STD AND INFECTIONS IN PREGNANCY (DR - Jandoc) 05-03-2019 (Part 2)Dasha VeeAinda não há avaliações
- Embryogenesis & Fetal DevelopementDocumento38 páginasEmbryogenesis & Fetal DevelopementDasha Vee100% (1)
- P.09 OBSTETRIC HEMORRHAGE (Dr. Ursua) 02-07-2019 (Part 1)Documento3 páginasP.09 OBSTETRIC HEMORRHAGE (Dr. Ursua) 02-07-2019 (Part 1)Dasha VeeAinda não há avaliações
- Obstetrics 2: Obstetric Hemorrhage (Part 2)Documento4 páginasObstetrics 2: Obstetric Hemorrhage (Part 2)Dasha VeeAinda não há avaliações
- Antiviral Chemotherapy and Prophylaxis: Acyclovir, Valacyclovir, and FamciclovirDocumento8 páginasAntiviral Chemotherapy and Prophylaxis: Acyclovir, Valacyclovir, and FamciclovirDasha VeeAinda não há avaliações
- F.06 STD and Infections in Pregnancy (Dr. Jandoc) 05-03-2019 (Part 1)Documento5 páginasF.06 STD and Infections in Pregnancy (Dr. Jandoc) 05-03-2019 (Part 1)Dasha VeeAinda não há avaliações
- Mental HealthDocumento4 páginasMental HealthDasha VeeAinda não há avaliações
- 2011 Full Page Calendar - TomKat StudioDocumento12 páginas2011 Full Page Calendar - TomKat StudioThe TomKat StudioAinda não há avaliações
- DiagnosisDocumento8 páginasDiagnosisDasha VeeAinda não há avaliações
- m.13 Dietary Supplements & Herbal Medications (Dr. Buñag) 04-04-18Documento4 páginasm.13 Dietary Supplements & Herbal Medications (Dr. Buñag) 04-04-18Dasha VeeAinda não há avaliações
- M.10B Drugs Used in Gastrointestinal DisordersDocumento3 páginasM.10B Drugs Used in Gastrointestinal DisordersDasha VeeAinda não há avaliações
- Thyroid PDFDocumento9 páginasThyroid PDFDasha VeeAinda não há avaliações
- F.09 BONE RADIOLOGY - Dr. GalangDocumento11 páginasF.09 BONE RADIOLOGY - Dr. GalangDasha VeeAinda não há avaliações
- P.07 Thyroid and Parathyroid Glands Dr. Manalo 9-8-16Documento4 páginasP.07 Thyroid and Parathyroid Glands Dr. Manalo 9-8-16Dasha VeeAinda não há avaliações
- Philippine CPG On The Diagnosis and Management of Urinary Tract Infections in Adults-2015 Update - Part 2 PDFDocumento140 páginasPhilippine CPG On The Diagnosis and Management of Urinary Tract Infections in Adults-2015 Update - Part 2 PDFspringdingAinda não há avaliações
- MEDICAL CERTIFICATIONDocumento7 páginasMEDICAL CERTIFICATIONDasha VeeAinda não há avaliações
- f.02 Intellectual Disabilities (Dr. Rebucal) 04-11-2019Documento4 páginasf.02 Intellectual Disabilities (Dr. Rebucal) 04-11-2019Dasha VeeAinda não há avaliações
- Ob Osce.04 CTG ReadingDocumento6 páginasOb Osce.04 CTG ReadingDasha VeeAinda não há avaliações
- Catalogo Presentacion Johnial UltimoDocumento10 páginasCatalogo Presentacion Johnial UltimoEmerson BermudezAinda não há avaliações
- Aloe Vera as an Alternative Treatment for Wound HealingDocumento5 páginasAloe Vera as an Alternative Treatment for Wound HealingJeffllanoAinda não há avaliações
- Installation and Operating Instructions DPV and DPLHS PumpsDocumento36 páginasInstallation and Operating Instructions DPV and DPLHS PumpsSergeyAinda não há avaliações
- Properties of X-Rays and Gamma RaysDocumento13 páginasProperties of X-Rays and Gamma RaysjishnusajiAinda não há avaliações
- Badhabits 2022Documento53 páginasBadhabits 2022Sajad KhaldounAinda não há avaliações
- Ketamine Drug Study for AnesthesiaDocumento1 páginaKetamine Drug Study for AnesthesiaPRINCESS MARIZHAR OMARAinda não há avaliações
- Maternal and Child Health Nursing, 8 Edition.: LESSON PREVIEW/REVIEW (5 Minutes)Documento7 páginasMaternal and Child Health Nursing, 8 Edition.: LESSON PREVIEW/REVIEW (5 Minutes)raker boiAinda não há avaliações
- Courses at NeevDocumento10 páginasCourses at NeevDr Mohan SavadeAinda não há avaliações
- Time ManagementDocumento30 páginasTime ManagementVaibhav Vithoba NaikAinda não há avaliações
- Eye, E.N.T. & Dental AnaesthesiaDocumento22 páginasEye, E.N.T. & Dental AnaesthesiawellawalalasithAinda não há avaliações
- Shell Alexia 40 cylinder oil designed for IMO 2020 complianceDocumento2 páginasShell Alexia 40 cylinder oil designed for IMO 2020 complianceStefas DimitriosAinda não há avaliações
- Nutritional Profile of Ube Yam: High in Fiber, Vitamin C & AnthocyaninsDocumento3 páginasNutritional Profile of Ube Yam: High in Fiber, Vitamin C & AnthocyaninsMc SuanAinda não há avaliações
- Safety Toolbox Project ProposalDocumento33 páginasSafety Toolbox Project ProposalShaffizi Boboy100% (1)
- MANUAL Health O Meter Scale 800KLDocumento2 páginasMANUAL Health O Meter Scale 800KLElkin MaldonadoAinda não há avaliações
- UntitledDocumento77 páginasUntitledVedranL84Ainda não há avaliações
- Medical TourismDocumento18 páginasMedical TourismdhnaushAinda não há avaliações
- Hydrogen DryerDocumento2 páginasHydrogen Dryersanju_cgh5518Ainda não há avaliações
- The Baking and Frozen Dough MarketDocumento4 páginasThe Baking and Frozen Dough MarketMilling and Grain magazineAinda não há avaliações
- GS I: Factors Driving Development of Global Textile IndustriesDocumento54 páginasGS I: Factors Driving Development of Global Textile IndustriesAMIT RAJAinda não há avaliações
- LENZE E84AVxCx - 8400 StateLine-HighLine-TopLine 0.25-45kW - v9-0 - ENDocumento291 páginasLENZE E84AVxCx - 8400 StateLine-HighLine-TopLine 0.25-45kW - v9-0 - ENClaudioAinda não há avaliações
- Jose Irizarry ResumeDocumento2 páginasJose Irizarry ResumeAnastasia GloverAinda não há avaliações
- Our Vision For Copenhagen 2015: Eco-MetropoleDocumento11 páginasOur Vision For Copenhagen 2015: Eco-MetropolePascal van den Noort100% (1)
- MAstering IATFDocumento20 páginasMAstering IATFGyanesh_DBAinda não há avaliações
- Form-Ii (See Regulation 4) Postal Bill of Export - II (To Be Submitted in Duplicate)Documento1 páginaForm-Ii (See Regulation 4) Postal Bill of Export - II (To Be Submitted in Duplicate)mrthilagamAinda não há avaliações
- Frontline ArticleDocumento7 páginasFrontline Articleapi-548946265Ainda não há avaliações
- Physiology of Women Reproduction SystemDocumento52 páginasPhysiology of Women Reproduction Systemram kumarAinda não há avaliações
- Face SerumDocumento10 páginasFace SerumLiliana CojocaruAinda não há avaliações