Escolar Documentos
Profissional Documentos
Cultura Documentos
MCQ S Pharmacy Chapter 1
Enviado por
Shamlin OommenTítulo original
Direitos autorais
Formatos disponíveis
Compartilhar este documento
Compartilhar ou incorporar documento
Você considera este documento útil?
Este conteúdo é inapropriado?
Denunciar este documentoDireitos autorais:
Formatos disponíveis
MCQ S Pharmacy Chapter 1
Enviado por
Shamlin OommenDireitos autorais:
Formatos disponíveis
ANTIBIOTIC PROPHYLAXIS FOR SURGERY GUIDELINE
BACKGROUND
The goal of antibiotic surgical prophylaxis is to ensure adequate serum and tissue
levels of the drug at the time of incision, and for the duration of surgery.
Antibiotic regimen should include agent(s) that are safe, active against the
most likely infecting organisms as well as being cost effective. Optimal dosing,
timing of the first dose, and redosing to maintain adequate level during the
procedure are more important than administration after the operation.
According to the 2017 CDC guideline for the prevention of surgical site
infection, administration of post-operative antibiotic doses is not
recommended in clean and clean-contaminated procedures.
PROCEDURE
1. Documentation of antimicrobial administration must include date, time of
administration, name of medication, dose, and route of administration. Do not
abbreviate name of medication and do not use unapproved abbreviations.
2. Antibiotic prophylaxis for surgery is given within one hour prior to surgical incision
except for Vancomycin, which is given within two hours prior to surgical incision.
3. All parenteral antibiotics listed in this guideline may be infused as indicated in Table 1.
Please note, it is strongly recommended that vancomycin be administered over a minimum
of 60 minutes and that all pre-operative antibiotics are completely infused before start of
procedure.
4. If a tourniquet is to be used in the procedure, the entire dose of antibiotic must be
infused prior to tourniquet inflation.
5. Intra-operative re-dosing is necessary during procedures that exceed two half-lives of
the drug to maintain adequate serum and tissue concentrations.
6. In clean and clean contaminated procedures, high-quality evidence suggests that
additional prophylactic antibiotic doses are not needed after the surgical incision is
closed in the OR even in the presence of a drain. For all other procedures, antibiotic
prophylaxis must be discontinued within 24 hours of surgical end time. Use of
antibiotics beyond the recommended post-operative duration requires proper
documentation of infection or suspected infection.
7. Vancomycin use requires documentation of the reason for use in the medical record by
the prescribing physician or his (her) designee. Reasons for use include:
a. Beta-lactam (penicillin or cephalosporin) allergy
b. Known Methicillin resistant Staphylococcus aureus (MRSA) colonization or
infection or high risk for MRSA (i.e. recent inpatient hospitalization, resides in an
extended care facility/group home, receives dialysis)
Updated July, 2017 1
Table 1. Dosing and Timing of Antibiotic Agents used for Surgical Prophylaxis
ANTIBIOTIC PEDIATRIC INFUSION TIMING OF INTRAOPERATIVE
AGENT INTRAVENOUS TIME FIRST REDOSING FOR
DOSE (MINUTES) DOSE NORMAL RENAL
(ADULT DOSE) FUNCTION
Ampicillin/ 50 mg/kg (2 30 Begin 60 Every 2 hrs
Sulbactam gm) of min or less
ampicillin before
component incision
Cefazolin 30 mg/kg 30 Begin 60 Every 4 hrs
(2 gm, 3 g for pts ≥ min or less
120 kg) before
incision
Cefoxitin 40 mg/kg 30 Begin 60 Every 2 hrs
(2 gm) min or less
before
incision
Cefepime 50 mg/kg 30 Begin 60 Every 4 hrs
(2 gm) min or less
before
incision
Clindamycin 10 mg/kg 30 Begin 60 Every 6 hrs
(900 mg) min or less
before
incision
Gentamicin 2.5 mg/kg [based 30 Begin 60 Every 8 hrs
on dosing weight] min or less
(5 mg/kg [based before
on dosing weight] incision
as a single dose)
Metronidazole 15 mg/kg 30 Begin 60 Every 6 hrs
(500 mg) min or less
before
incision
Vancomycin 15 mg/kg 60 Begin 120 Every 6 hrs
(15 mg/kg) min or less
before
incision
Updated July, 2017 2
Table 2. Recommended Intravenous Antibiotics for Surgical Procedures
PROCEDURE COMMON RECOMMENDED ANTIBIOTIC POST
PATHOGENS PROPHYLAXIS OPERATIVE
DURATION
CARDIAC S. epidermidis, Cefazolin OR
Heart surgery+, PDA (patent ductus S. aureus
Vancomycin^
arteriosis), ASD/VSD (atrial/ventricular
septal defect), Glenn Shunt, valve
replair/replacement, Aortic reconstruction,
prosthetic graft insertion No additional
antibiotic
GASTROINTESTINAL doses are
Esophageal, gastroduodenal Enteric gram- For high risk+++: Cefazolin
negative bacilli,
needed for
PEG placement/revision/ conversion to If major reaction to beta- clean, clean-
gram positive
other feeding tubes OR high-risk conditions lactams++: Clindamycin plus
cocci contaminated
Gentamicin procedures,
even in
Biliary, including lap cholecystectomy Enteric gram- For high risk*: Cefazolin presence of a
negative bacilli,
If major reaction to beta- drain
gram positive
cocci, clostridia lactam++: Clindamycin plus
Gentamicin
Colorectal** Enteric gram Cefoxitin OR
Appendectomy or ruptured viscus negative bacilli,
Ceftriaxone plus
anaerobes,
enterococci Metronidazole
If major reaction to beta-
lactams++: Clindamycin plus For other
Gentamicin procedures,
discontinue
HEAD and NECK SURGERY Anaerobes, Cefazolin OR within 24 hrs
Incision through oral or pharyngeal enteric gram- of surgical end
If major reaction to beta-
mucosa, lower jaw fraction, removal of negative bacilli,
S.aureus lactams++: Clindamycin plus time
esophagus pouch
Gentamicin
NEUROSURGERY## S. aureus, Cefazolin OR
Craniotomy, shunt placement/revision, S. epidermidis
Vancomycin^
insertion of pump/reservoir, spinal
procedure (laminectomy, fusion or cord
decompression)
ORTHOPEDIC S. epidermidis , Cefazolin or Cefepime and
Spinal procedures or implantation of S. aureus
Vancomycin^
hardware. Give dose before
tourniquet inflation
THORACIC S. aureus, Cefazolin OR
Lung resection, VATS S. epidermidis, Vancomycin^ or Clindamycin
streptococci,
enteric gram-
negative bacilli##
VASCULAR (see Cardiac) S. aureus, Cefazolin OR
Extremity amputation for ischemia, S. epidermidis,
Vancomycin^ OR Clindamycin
vascular access for hemodialysis enteric gram-
negative bacilli
Updated July, 2017 3
GYNECOLOGIC Enteric gram- Cefoxitin OR Ampicillin plus
negative bacilli, No additional
Metronidazole plus Gentamicin antibiotic doses
anaerobes, Gp B
strep, enterococci If major reaction to are needed for
beta-lactam++: clean, clean-
Clindamycin plus contaminated
Gentamicin procedures,
even in
presence of a
Enteric gram- For high risk only***: Cefazolin
negative bacilli,
drain
GENITOURINARY OR Cefoxitin OR Ampicillin plus
anaerobes,
Bladder augmentation, pyeloplasty Metronidazole plus
enterococci
Gentamicin For other
If major reaction to procedures,
beta- lactam++: discontinue
Clindamycin plus within 24 hrs of
surgical end
Gentamicin
time
^ for known MRSA or high risk for MRSA, or major reaction to beta- lactams
+For open-heart surgery only: use maximum cefazolin 2 gm; redose cefazolin when patient is removed from bypass; alternative to
cefazolin monotherapy is cefazolin plus vancomycin for patients at high risk for MRSA. (procedure involves insertion of prosthetic valve
or vascular graft).
++Major reactions include anaphylaxis, hives, shortness of breath, wheezing, edema. For minor reactions (nausea, vomiting, diarrhea,
mild rash, itching), cephalosporins may still be used.
+++High risk gastroduodenal: morbid obesity, esophageal obstruction, decreased gastric acidity or decreased gastrointestinal motility
*High risk biliary: acute cholecystitis, non-functioning gall bladder, obstructive jaundice or common duct stones
**Colorectal procedures: Oral prophylaxis prior to surgery - After appropriate diet and catharsis, 1 gram of neomycin plus 1 gram of
erythromycin at 1 pm, 2 pm, and 11 pm or 2 grams of neomycin plus 2 grams of metronidazole at 7 pm and 11pm the day before an 8 am
day operation
***High risk genitourinary: urine culture positive or unavailable, preoperative catheter, transrectal prosthetic biopsy, placement of
prosthetic material
##Vascular procedures: Clostridia can also be present in lower extremity amputation for ischemia.
REFERENCES
1. Bratzler DW, Dellinger EP, Olsen KM, Perl TM, Auwaerter PG, Bolon MK, Fish DN, Napolitano LM, Sawyer RG, Slain D,
Steinberg JP, Weinstein RA; American Society of Health-System Pharmacists; Infectious Disease Society of
America; Surgical Infection Society; Society for Healthcare Epidemiology of America.Clinical practice guidelines for
antimicrobial prophylaxis in surgery. Am J Health Syst Pharm. 2013 Feb 1;70(3):195-283.
2. Bratzler DW et al. Antibiotic prophylaxis for surgery: An advisory statement from the National Surgical Infection
Prevention Project. Clin Infect Dis 2004; 38:1706
3. Bratzler DW and Hunt DR. The surgical infection prevention and surgical care improvement projects: National
initiatives to improve outcomes for patients having surgery. Clin Infect Dis 2006; 43:322
4. Engelman R, Shahian D, Shemin R, et al. The Society of Thoracic Surgeons Practice Guideline Series: Antibiotic
prophylaxis in cardiac surgery, Party II: antibiotic Choice. Ann Thorc Surg 2007;83:1569-76
5. Talbot TR, Kaiser AB. Postoperative infections and antibiotic prophylaxis, in Mandell GL, Bennett JE, Dolin R,
Principles and Practice of Infectious Diseases Elsevier Inc. 2005, pages 3533-3547
6. Dellinger PE. Prophylactic Antibiotics: Administration and Timing before Operation Are More Important than
administration after Operation. Clin Infect Dis 2007;44:928-30
7. Berrios-Torres SI, Umscheid CA, Bratzler DW, et al. Centers for Disease Control and Prevention Guideline for
the Prevention of Surgical Site Infection, 2017. JAMA Surg. Published online May 03, 2017.
doi:10.1001/jamasurg.2017.090
Updated July, 2017 4
Você também pode gostar
- New Prometric Questions Sample (DHA)Documento7 páginasNew Prometric Questions Sample (DHA)Dr-Usman Khan84% (56)
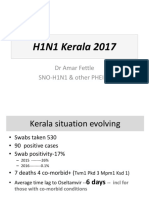
- H1N1 Kerala 2017: DR Amar Fettle SNO-H1N1 & Other PHEICSDocumento21 páginasH1N1 Kerala 2017: DR Amar Fettle SNO-H1N1 & Other PHEICSShamlin OommenAinda não há avaliações
- IELTS Writing Task 2 Workshop PDFDocumento2 páginasIELTS Writing Task 2 Workshop PDFmohammed jebreelAinda não há avaliações
- IELTS Task 1 Writing Band DescriptorsDocumento2 páginasIELTS Task 1 Writing Band Descriptorspelosa12345Ainda não há avaliações
- H1N1 Kerala 2017: DR Amar Fettle SNO-H1N1 & Other PHEICSDocumento21 páginasH1N1 Kerala 2017: DR Amar Fettle SNO-H1N1 & Other PHEICSShamlin OommenAinda não há avaliações
- 1 MCQ Pharmaceutical TechnologyDocumento23 páginas1 MCQ Pharmaceutical TechnologySSB79% (14)
- Pharmacist - Blueprint and Reference (Dec2016) PDFDocumento1 páginaPharmacist - Blueprint and Reference (Dec2016) PDFShamlin OommenAinda não há avaliações
- Pharmacist - Blueprint and Reference (Dec2016)Documento1 páginaPharmacist - Blueprint and Reference (Dec2016)Shamlin OommenAinda não há avaliações
- Fist Ulog RamDocumento5 páginasFist Ulog Ramansmart997373Ainda não há avaliações
- Cover LetterDocumento1 páginaCover LetterShamlin OommenAinda não há avaliações
- Cover LetterDocumento1 páginaCover LetterShamlin OommenAinda não há avaliações
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeNo EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeNota: 4 de 5 estrelas4/5 (5794)
- The Little Book of Hygge: Danish Secrets to Happy LivingNo EverandThe Little Book of Hygge: Danish Secrets to Happy LivingNota: 3.5 de 5 estrelas3.5/5 (400)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceNo EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceNota: 4 de 5 estrelas4/5 (895)
- The Yellow House: A Memoir (2019 National Book Award Winner)No EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Nota: 4 de 5 estrelas4/5 (98)
- The Emperor of All Maladies: A Biography of CancerNo EverandThe Emperor of All Maladies: A Biography of CancerNota: 4.5 de 5 estrelas4.5/5 (271)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryNo EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryNota: 3.5 de 5 estrelas3.5/5 (231)
- Never Split the Difference: Negotiating As If Your Life Depended On ItNo EverandNever Split the Difference: Negotiating As If Your Life Depended On ItNota: 4.5 de 5 estrelas4.5/5 (838)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureNo EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureNota: 4.5 de 5 estrelas4.5/5 (474)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaNo EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaNota: 4.5 de 5 estrelas4.5/5 (266)
- The Unwinding: An Inner History of the New AmericaNo EverandThe Unwinding: An Inner History of the New AmericaNota: 4 de 5 estrelas4/5 (45)
- Team of Rivals: The Political Genius of Abraham LincolnNo EverandTeam of Rivals: The Political Genius of Abraham LincolnNota: 4.5 de 5 estrelas4.5/5 (234)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyNo EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyNota: 3.5 de 5 estrelas3.5/5 (2259)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreNo EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreNota: 4 de 5 estrelas4/5 (1090)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersNo EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersNota: 4.5 de 5 estrelas4.5/5 (344)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)No EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Nota: 4.5 de 5 estrelas4.5/5 (121)
- Drug Study 8Documento3 páginasDrug Study 8Vicky RoqueAinda não há avaliações
- Chapter7 B and T Cell Activation (1) ImmunologyDocumento21 páginasChapter7 B and T Cell Activation (1) ImmunologyIka BakarAinda não há avaliações
- Prevention of Ebola Virus InfectionDocumento55 páginasPrevention of Ebola Virus InfectionAnusha VergheseAinda não há avaliações
- Asthma2 Case StudyDocumento8 páginasAsthma2 Case StudyGlenn Asuncion PagaduanAinda não há avaliações
- ID Consult TemplateDocumento5 páginasID Consult TemplateRohitKumar100% (1)
- Module Description. Pathology of Musculosceletal SystemDocumento52 páginasModule Description. Pathology of Musculosceletal SystemAlberto MayorgaAinda não há avaliações
- Askep CKDDocumento55 páginasAskep CKDyuli ariyantiAinda não há avaliações
- PG - 2016 - 2017 SESSION List of Candidates Allotted - On 11.04.2016Documento16 páginasPG - 2016 - 2017 SESSION List of Candidates Allotted - On 11.04.2016chenda raviAinda não há avaliações
- Acu-Stim For RecoveryDocumento4 páginasAcu-Stim For Recoverycare_e_genAinda não há avaliações
- Shwayder, T., Schneider, S. L., Icecreamwala, D., & Jahnke, M. N. (2019) - Longitudinal Observation of Pediatric Dermatology Patients.Documento255 páginasShwayder, T., Schneider, S. L., Icecreamwala, D., & Jahnke, M. N. (2019) - Longitudinal Observation of Pediatric Dermatology Patients.Cristina GilcaAinda não há avaliações
- Methods of Nutrient DeliveryDocumento3 páginasMethods of Nutrient DeliveryFarmisa MannanAinda não há avaliações
- Common Poison in ChildrenDocumento31 páginasCommon Poison in ChildrenNimi BatuboAinda não há avaliações
- Precosious Puberty Case StudyDocumento27 páginasPrecosious Puberty Case Studynishavohreh100% (1)
- ISR NG Chun Ruh2Documento1 páginaISR NG Chun Ruh2Yasmine SlhAinda não há avaliações
- Step by Step Root Canal TreatmentDocumento157 páginasStep by Step Root Canal TreatmentKaaroma Tamoaieta100% (1)
- Acute Stress Disorder 1Documento22 páginasAcute Stress Disorder 1Seiska MegaAinda não há avaliações
- LAB 4 Simple Stain 2nd 2020-2021Documento17 páginasLAB 4 Simple Stain 2nd 2020-2021Deena Hajj QasemAinda não há avaliações
- Perspective: New England Journal MedicineDocumento4 páginasPerspective: New England Journal MedicineGary MaoAinda não há avaliações
- 5 Weight LossDocumento41 páginas5 Weight LossTasniiem KhmbataAinda não há avaliações
- Sarhad 8MCF BadlmaDocumento29 páginasSarhad 8MCF Badlmasoran najebAinda não há avaliações
- 11 Grammar Test: 94 Photocopiable © Oxford University PressDocumento1 página11 Grammar Test: 94 Photocopiable © Oxford University PressLauri RosseAinda não há avaliações
- Bacterial Skin and Soft Tissue Infections: Clinical Review ArticleDocumento9 páginasBacterial Skin and Soft Tissue Infections: Clinical Review ArticleRini MayaSariAinda não há avaliações
- I Nengah Kundera, Mursito Bialangi: 1. PendahuluanDocumento6 páginasI Nengah Kundera, Mursito Bialangi: 1. PendahuluanDesak Putu Widya AprilianiAinda não há avaliações
- How Can Help You?: A You A You A You A YouDocumento1 páginaHow Can Help You?: A You A You A You A Youimpresiv MAinda não há avaliações
- Activity Intolerance YAp ER NCPDocumento2 páginasActivity Intolerance YAp ER NCPmecz26100% (2)
- Care Plan TemplateDocumento8 páginasCare Plan TemplateXosweetbebeAinda não há avaliações
- Personal Notes Excpetional StuffDocumento352 páginasPersonal Notes Excpetional StuffYagyeshAinda não há avaliações
- Exosome-Based Immunotherapy: A Promising Approach For Cancer TreatmentDocumento16 páginasExosome-Based Immunotherapy: A Promising Approach For Cancer Treatment1810 15Marvin LionelAinda não há avaliações
- Role of MDCT in Coronary Artery Disease: Swachchhanda Songmen 2071Documento63 páginasRole of MDCT in Coronary Artery Disease: Swachchhanda Songmen 2071Dr KhanAinda não há avaliações
- For Demo in Teaching Strategies by Mike ReyesDocumento10 páginasFor Demo in Teaching Strategies by Mike ReyesPaulo Sandino GaliciaAinda não há avaliações