Escolar Documentos
Profissional Documentos
Cultura Documentos
Translational Medicine Reports - Efficacy of Chemoid Ovarian Cancer
Enviado por
api-334757816Título original
Direitos autorais
Formatos disponíveis
Compartilhar este documento
Compartilhar ou incorporar documento
Você considera este documento útil?
Este conteúdo é inapropriado?
Denunciar este documentoDireitos autorais:
Formatos disponíveis
Translational Medicine Reports - Efficacy of Chemoid Ovarian Cancer
Enviado por
api-334757816Direitos autorais:
Formatos disponíveis
Translational Medicine Reports 2017; volume 1:6701
Efficacy of ChemoID® guided reported case the survival and symptom
management benefits of ChemoID® guided Correspondence: Pier Paolo Claudio,
drug selection for palliative therapy even after plateau of response to Department of Radiation Oncology,
chemotherapy in advanced cisplatin. Further studies are indicated to University of Mississippi Medical Center
increase the clinical adoption of ChemoID® Cancer Institute, Jackson, MS 39126, USA.
E-mail: pclaudio@olemiss.edu
for gynecological malignancies in the pal-
recurrent high-grade ovarian
liative setting.
adenocarcinoma: Case study
Key words: Ovarian cancer, Cancer stem
cells, Chemosensitivity assay, Chemo-predic-
Timothy G. DeEulis,1
tive assay, ChemoID®.
Candace M. Howard,2 Jagan Valluri,3
Pier Paolo Claudio4,5 Introduction Received for publication: 9 March 2017.
1 Gynecologic Oncology, Women’s Accepted for publication: 21 March 20147.
Oncologic Palliative Medicine, Epithelial ovarian cancer (EOC) is the
leading cause of death from gynecologic This work is licensed under a Creative
Huntington, WV; 2Department of Commons Attribution 4.0 License (by-nc 4.0).
malignancies with more than 23,000 cases
Radiology, University of Mississippi
annually in the United States, and 14,000
Medical Center, Jackson, MS; ©Copyright T.G. DeEulis et al., 2017
women that are expected to die from the Licensee PAGEPress, Italy
3
Department of Biological Sciences, disease.1 Although ovarian cancer accounts Translational Medicine Reports 2017; 1:6701
Marshall University, Huntington, WV; for only 3% of all cancers in women, it has doi:10.4081/tmr.6701
4
Department of BioMolecular Sciences, one of the highest death-to- incidence
National Center for Natural Products ratios, which has been primarily attributed
Research, University of Mississippi, to the unavailability of effective screening
University, MS; 5Department of ing the identification of predictive biomark-
tools, the absence of early symptoms, and
ly
Radiation Oncology, University of its typical presentation at advanced stages ers with clinical relevance, so that empirical
drug selection can be avoided. Selection of
on
Mississippi Medical Center Cancer when prognosis is poor.2,3 In particular,
patients with high- grade serous carcinoma effective chemotherapy is important not
Institute, Jackson, MS, USA
(which constitute 60-80% of EOC, and only when therapy is first initiated, but
especially for recurrent disease. In fact,
e
which represent the archetypical ovarian
cancer) most frequently present at
us administration of ineffective anticancer
Abstract therapy is associated with unnecessary tox-
advanced clinical stage and have a very
poor overall survival.4,5 icity and the development of more aggres-
Notwithstanding tremendous advances
sive cancer cell clones that is resistant to
al
in surgery, primary chemotherapy, and The common initial management for
novel treatments for recurrent disease, the newly diagnosed epithelial ovarian cancer subsequent therapies.7,8 The ability to
ci
diagnosis of advanced epithelial ovarian (EOC) includes aggressive cytoreductive choose the most effective chemotherapy
cancer (EOC) in 2016 remains ultimately surgery accompanied by the administration may help improving patients’ quality of life
er
fatal in the majority of cases. Advanced of platinum and taxane-based chemothera- by avoiding the physical, emotional, and
therapy refractory EOC patients are often py before or after surgery. Despite the inher- financial burden of ineffective therapy.9
m
treated in hospice and with chemotherapy ent resistance to chemotherapy in some Anticancer drugs for different reasons have
palliative care. The main goals of patients, about 80% of patients achieve an a high rate of failure and cell culture
m
chemotherapy for recurrent/refractory ovar- initial clinical complete response.6 chemotherapy testing has been used during
the recent past to identify which drugs are
co
ian cancer are the palliation of disease-relat- However, the majority of EOC patients will
ed symptoms, and improvement of quality eventually relapse. Some patients relapse more likely to be effective especially
and quantity of life. Unfortunately, there is within 6 months and have a short survival against those of gynecological origin.10,11
Many attempts have been made over the
on
contradicting evidence suggesting that due to platinum-resistant disease; other
chemotherapy has a role in palliation of patients have late relapses with platinum- years to develop an in-vitro anti-cancer test
symptoms with an apparent improvement in sensitive disease, and substantially longer that can provide clinically relevant treat-
N
quality of life. Anticancer drugs have a high survival. ment information. However, this approach
rate of failure and chemotherapy response Currently, clinicians do not have good has been hampered by the chemotherapy
assays have been used to identify which prognostic tools to estimate which patients testing only being performed on bulk of
drugs are more likely to be effective against are destined to have platinum-resistant or tumor cells derived from cancer biopsies.12-
21 Ovarian cancers contain a population of
those of gynecological origin. ChemoID® is sensitive disease. As a result, the current
a functional drug response assay which standard of care is to apply a general para- self- renewing cancer stem cells (CSCs)
measures the sensitivity of cancer stem cells digm to all women with ovarian cancer; that contribute to tumorigenesis, treatment
(CSCs) and bulk of tumor cells to either surgery followed by adjuvant plat- resistance and tumor recurrence.22-29
chemotherapy to determine the most effec- inum and taxane-based chemotherapy or ChemoID® is a functional test that uses
tive combination of anticancer drugs for neo-adjuvant chemotherapy with the same patient’s live tumor cells to indicate which
solid tumors. We present a clinical case that agents preceding surgery.6 Despite chemotherapy agent (or combinations) will
demonstrates the utility of ChemoID® guid- improvements in the management of ovari- kill not only the bulk tumor cells, but more
ance to commonly available drugs with an cancer patients over the last 30 years, importantly the cancer stem cells (CSCs)
identified toxicity profiles and predictable there has been only a minimal improvement that are known to cause cancer to recur.
cost profile available at POS, along with in overall survival. In fact, while targeted Targeting of CSCs alongside the bulk of
rapid response in correcting symptomatic therapeutic approaches for the treatment of other cancer cells is a new paradigm in can-
disease features, and minimal treatment cancer have evolved, major challenges in cer treatment. This constitutes an important
burden from toxicities. We observed in the ovarian cancer research still persist, includ- advantage of ChemoID® approach over
[page 70] [Translational Medicine Reports 2017; 1:6701]
Case Report
other cell culture testing methods. Our Each concentration was added to five repli-
recent clinical studies showed that patient cate wells on the microtiter plate. Three
derived CSCs from primary cancer cell cul- replicates wells (control 1=no treatment)
tures can be used in a drug response and three replicates wells (control 2=equal
assay.9,30-36 We have optimized the enrich- amount of solvent) were associated with
ment of CSCs from tumor biopsies and each treatment also. The cells were chal-
aspirates of effusions and have developed lenged for a 1-hour pulse with the panel of
the ChemoID® chemotherapy response anticancer drugs. Sensitivity to chemothera-
assay, which measures the sensitivity of py was assessed using a WST8 viability
CSCs and bulk of tumor cells to chemother- assay (Dojindo Molecular Technologies,
apy to determine the most effective combi- Rockville, MD, USA) on 1×10-3 cells plated
nation of anticancer drugs for solid in 5 replicas into 96-well plates. The WST8
tumors.9,30-36 assay was performed 48- hours following
chemotherapy treatment to assess cell via-
bility as previously described.9
The inhibition of bulk of tumor cells
Materials and Methods and CSCs survival was measured for each
concentration (average counts in five repli-
cates ± SE) of a given treatment. The sur-
Patient
vival of tumor cells at each concentration
Patient is a 77-year-old female present- was calculated as compared to control-2
ing with venous thromboembolism and evi- and overall percent of bulk and CSC tumor
dence of IIIC ovarian cancer, who under- cells killed were calculated for each treat-
ly
went initial cytoreductive surgery in June ment as the primary measures of potential
02, 2008. Patient relapsed to first, second,
on
therapy efficacy.
third, and fourth line standard-of-care
chemotherapy treatment before being diag-
nosed with ChemoID® drug response assay.
e
Subject was enrolled in the study only after us
a discussion of her treatment options,
including chemotherapy. ChemoID® assay
was performed after obtaining patient’s
al
consent. Marshall University Institutional
Review Board (IRB) has approved this
ci
research under the protocol #695141.
er
Drug sensitivity assay
Ascites aspirate containing a high cellu-
m
larity of malignant cells for ChemoID® in
m
vitro functional testing was collected in the
operating room from the patient. Details
co
regarding the assay procedure have been
described elsewhere.9,30-34,36 In brief, pri-
mary cultures were initiated by spinning
on
down the malignant cells present in the
ascites aspirate and by culturing the cells to
sub confluence in RPMI-1640 medium sup-
N
plemented with 5% irradiated, heat inacti-
vated, defined fetal bovine serum
(Thermofisher/Hyclone), and 50 U of peni-
Figure 2. Chest and abdomen computed
tomography with contrast enhancement
cillin and 5 µg of streptomycin/mL of medi-
showing detail of the left pleural effusion:
um (Thermofisher/Mediatech). Prolifera-
A) is a cross sectional image at the lung
tion of CSCs was obtained using a culture
base in lung windows; B) is a cross section-
methodology previously described9,31 in
al image of the upper abdomen at the level
which culture media, oxygenation, rotation-
of the liver dome with soft tissue window-
ing; C) is the same image with soft tissue
al speed of the culture vessel, temperature windowing. The images demonstrate
and CO2 were kept consistently constant
increased abdominal pressure from large
for seven days. Cells were then removed
volume abdominal ascites secondary to
and counted using trypan blue exclusion to
peritoneal carcinomatosis causing large
hiatal hernia with herniation of the bowel
determine cellular viability and cell number. Figure 1. Recurrent malignant effusion at into the retro cardiac portion of the thorax
Equal number of bulk of tumor cells and fourth relapse of epithelial ovarian cancer: with mass affect on the left atrium of the
CSCs, were counted and seeded separately
posterior/anterior (A) and left lateral (B) heart. Moderate malignant left pleural
in 96-well dishes and incubated at 37°C for
chest x-ray showing moderate malignant effusion causing passive sub-segmental
24-hours. Three concentrations of each
left pleural effusion causing passive atelec- atelectasis of the left lower lobe of the
lung. No morphologic features of cirrhosis
treatment were prepared by serial dilution.
tasis of the left lower lobe of the lung. Note
is also made of a large hiatal hernia. in the liver.
[Translational Medicine Reports 2017; 1:6701] [page 71]
Case Report
post cycle 1 of carboplatinum/taxol), con- biweekly topotecan 4mg/m2 from April
Results sistent with the history of a complete plat- 2014 to December 2014 and in January
inum response. Unfortunately, following 2015 the CA125 measured 395. In June
A 77-year-old female presented with
the first two years of no evidence of disease 2015, a follow-up visit discovered a fourth
venous thromboembolism (VTE) and evi-
(NED), the EOC relapsed several times in relapse with CA125 = 655, with pleural
dence of IIIC ovarian cancer, with a CA125
spite of chemotherapy management. Upon effusion and large volume ascites, both
of 340 and 3,000 cc of ascites at exploration
a follow-up visit, a relapse of the EOC was cytologically positive for adenocarcinoma,
in 2008. She had pulmonary embolism that
observed in September 2011, which was consistent with primary EOC (Figures 1 and
was treated with an inferior vena cava
treated with second-line chemotherapy con- 2). An ascites aspirate from the fourth EOC
(IVC) filter. The initial surgery of radical
sisting of 11 cycles of carboplatinum 300 relapse was sent to the clinical laboratory
cytoreduction included positive paraaortic
mg and gemcitabine 1,000 mg from for ChemoID® testing which resulted in
lymph nodes to optimal status less than 1
October 4, 2011 to September 20, 2012. A four responsive (60-100% cell kill in vitro)
cm. Pathology specimens involved both
second relapse in July 2013 was treated possible regimens (Table 1). Patient was
ovaries, omentum, urinary bladder, bilateral
with third-line pegylated doxorubicin 51mg treated with fifth-line therapy consisting of
fallopian tubes cervical stroma gall bladder
administered over 3 of 4 weeks for 9 cycles. cisplatinum 40 mg/m2 plus paclitaxel 60
serosa and paraaortic lymph nodes.
A third relapse in March of 2014 with CA mg/m2 with dose reduction due to chronic
Pathology report described the presence of
125 = 308 was treated with fourth-line kidney disease (CKD) and prior grade-2
a high-grade serous ovarian adenocarcino-
peripheral neuropathy.
ma. Within 42-days post surgery, patient
Fifth-line chemotherapy was initiated in
was treated with first-line adjuvant
July 08, 2015 after supportive care manage-
chemotherapy (carboplatinum 560 mg and
ment for pleural effusion and large volume
taxol 255 mg IV q4 weeks) beginning July
of rapidly recurrent ascites requiring Aspira
15, 2008 through July 27, 2009. Immediate
catheter (over 1,000cc/day daily drainage).
ly
post-therapeutic monitoring of CA125
Six cycles of cisplatinum and taxol fifth-
showed a satisfactory decrease (CA 125 =
on
line chemotherapy, as guided by
340 pre chemo, 99.2 = post-op, and 49.9 =
ChemoID®, were administered without dose
modification between July 2015 (Figures 3
e
and 4) and December 2015 (Figure 5) and
us resulted in a constant decline of CA125 as
follows: 06/06/2015 = 655.5; 07/25/2015 =
201.9 post cycle 1; 08/31/2015 = 68.7 post
cycle 2; 09/23/2015 = 53.4 post cycle 3;
al
10/19/2015 = 43.1 post cycle 4; 11/16/2015
ci
= 59.8 post cycle 5; 12/28/2015 = 59.7 post
cycle 6. On 12/28/2015 despite stable CA-
er
m
m
co
on
N
Figure 4. Chest and abdomen computed
tomography with contrast enhancement
showing positive therapeutic response of
the malignant pleural effusion and abdom-
inal ascites from peritoneal carcinomatosis
after one cycle of ChemoID® predicted
cisplatinum and taxol chemotherapy.
Cross sectional image at the lung bases (A)
and cross sectional image of the mid Figure 5. Abdominal computed tomogra-
Figure 3. Marked decrease of pleural effu- abdomen below the liver and the spleen phy showing further positive therapeutic
sion after one cycle of ChemoID® predict- (B). Both sections are displayed using soft response after six cycles of ChemoID® pre-
ed cisplatinum and taxol chemotherapy: tissue windows. Imaging shows marked dicted cisplatinum and taxol chemothera-
posterior/anterior (A) and left (B) lateral reduction in the left pleural post py with resolution of ascites. Cross-sec-
chest x-ray showing marked decrease of chemotherapy with minimal residual left tional image with IV and oral contrast of
prior moderate malignant left pleural effu- pleural effusion and improved aeration in the mid abdomen below the level of the
sion and improved aeration of the left the left lung base. Additionally, there is a liver and spleen. Interval complete resolu-
lower lobe of the lung. Trace residual left dramatic decrease in the abdominal ascites. tion of abdominal ascites and marked
pleural effusion. Note is also made of a Note the large hiatal hernia has re-expand- reduction of peritoneal implants and lym-
large hiatal hernia. ed following resolution of effusion. phadenopathy.
[page 72] [Translational Medicine Reports 2017; 1:6701]
Case Report
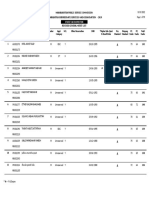
Table 1. ChemoID® assay results from ascites aspirate from a fourth recurrence of a high-grade serous carcinoma of the ovaries.
Comparative values for bulk of tumor Comparative values for cancer stem cells
Responsive 100-60% cell kill
Cyclophosphamide 600 mg/m2 +Cisplatin 100 mg/m2 72.3%±0.9 Pemetrexed 500 mg/m2 +Cisplatin 100 mg/m2 70.1%±1.0
Pemetrexed 500 mg/m2 +Cisplatin 100 mg/m2 71.3%±0.5 Cisplatin 100 mg/m2 68.7%±1.7
Cisplatin 100 mg/m2 63.3%±1.3 Cyclophosphamide 600 mg/m2 +Cisplatin 100 mg/m2 66.5%±1.2
Paclitaxel 175 mg/m2 +Cisplatin 100 mg/m2 62.5%±1.2 Fluorouracil 1000 mg/m2 +Cisplatin 100 mg/m2 60.4%±1.2
Intermediate response 60-30% cell kill
Fluorouracil 1000 mg/m2 +Cisplatin 100 mg/m2 58.9%±1.5 Paclitaxel 175 mg/m2 +Cisplatin 100 mg/m2 58.5%±1.4
Doxorubicin 75 mg/m2 54.2%±2.5 Pemetrexed 500 mg/m2 +Doxorubicin 75 mg/m2 54.2%±1.5
Pemetrexed 500 mg/m2 + Doxorubicin 75mg/m2 51.9%±0.7 Doxorubicin 75 mg/m2 51.5%±1.9
2
- - Carboplatin 350 mg/m 42.5%±1.0
Not responsive 30-0% cell kill
Carboplatin 350 mg/m2 24.5%±4.0 Pemetrexed 500 mg/m2 14.0%±4.6
Fluorouracil 1000 mg/m2 12.8%±3.7 Methotrexate 500 mg/m2 28.8%±3.6
Etoposide 50 mg/m2 11.5%±1.4 Fluorouracil 1000 mg/m2 <10%
Cyclophosphamide 600 mg/m2 <10% Etoposide 50 mg/m2 <10%
ly
Paclitaxel 175 mg/m2 <10% Cyclophosphamide 600 mg/m2 <10%
Docetaxel 75 mg/m2 <10% Paclitaxel 175 mg/m2 <10%
on
Pemetrexed 500 mg/m2 <10% Docetaxel 75 mg/m2 <10%
Methotrexate 500 mg/m2 <10% -
e
us
al
Table 2 ChemoID® assay results from pleural effusion of fifth recurrence from a high-grade serous carcinoma of the ovaries.
ci
Comparative values for bulk of tumor Comparative values for cancer stem cells
er
Responsive 100-60% cell kill
m
Gemcitabine 1250 mg/m2 +Cisplatin 100 mg/m2 69.3%±1.3 Gemcitabine 1250 mg/m2+Docetaxel 75 mg/m2 79.3%±2.4
Ifosfamide 5000 mg/m2 64.3%±0.4 Docetaxel 75 mg/m2+Cisplatin 80 mg/m2 69.8%±1.4
m
Intermediate response 60-30% cell kill
co
Docetaxel 75 mg/m2 +Cisplatin 80 mg/m2 59.3%±0.9 Gemcitabine 1250 mg/m2+Cisplatin 100 mg/m2 53.1%±1.0
Cisplatin 100 mg/m2 52.2%±1.9 Docetaxel 75 mg/m2 52.8%±2.2
Etoposide 100 mg/m2 + Paclitaxel 175 mg/m2 + 49.9%±1.8 Ifosfamide 5000 mg/m2 52.1%±0.6
on
Carboplatin 350 mg/m2
Gemcitabine 1250 mg/m2 +Docetaxel 75 mg/m2 48.5%±2.7 Etoposide 100 mg/m2+ Doxorubicin 50 mg/m2+Cisplatin 50 mg/m2 49.3%±0.4
N
Etoposide 100 mg/m2 + Doxorubicin 50 mg/m2 + 51.9%±0.7 Cisplatin 100 mg/m2 43.9%±1.2
Cisplatin 50 mg/m2
Oxaliplatin 85 mg/m2 45.5%±3.8 Etoposide 100 mg/m2+ Paclitaxel 175 mg/m2+Carboplatin 350 mg/m2 42.6%±1.6
Paclitaxel 175 mg/m2 +Carboplatin 350 mg/m2 41.1%±0.9 Doxorubicin 60 mg/m2 40.3%±2.8
Docetaxel 75 mg/m2 32.5%±1.0 Fluorouracil 1000 mg/m2+Oxaliplatin 85 mg/m2 39.4%±3.5
Topotecan 1.5 mg/m2 +Doxorubicin 60 mg/m2 31.9%±0.3 Topotecan 1.5 mg/m2+Doxorubicin 60 mg/m2 37.4%±0.7
Doxorubicin 60 mg/m2 31.0%±1.8 Paclitaxel 175 mg/m2 +Carboplatin 350 mg/m 35.9%±2.0
Fluorouracil 1000 mg/m2 +Oxaliplatin 85 mg/m2 30.1%±4.5 - -
Not responsive 30-0% cell kill
Carboplatin 350 mg/m2 22.2%±3.2 Oxaliplatin 85 mg/m2 28.1%±2.2
Paclitaxel 175 mg/m2 19.0%±2.7 Etoposide 100 mg/m2 27.3%±2.1
Fluorouracil 1000 mg/m2 13.7%±1.3 Fluorouracil 1000 mg/m2 19.4%±1.3
Etoposide 100 mg/m2 <10% Gemcitabine 1250 mg/m2 17.8%±3.5
Topotecan 1.5 mg/m2 <10% Topotecan 1.5 mg/m2 16.8%±3.0
Gemcitabine 1250 mg/m2 <10% Carboplatin 350 mg/m2 16.4%±3.7
- - Paclitaxel 175 mg/m2 <10%
[Translational Medicine Reports 2017; 1:6701] [page 73]
Case Report
125, no recurrent pleural effusion was apy within 3 months from their end of life.38 ures the sensitivity of CSCs and bulk of
found. Supportive management of pleural When ovarian cancer progresses, goals tumor cells to chemotherapy to determine
effusion with thoracic Aspira catheter main- change from cure to prolongation of life the most effective combination of anti-
tained KPS over 90 and ECOG 0 off thera- with the best possible quality for the patient. cancer drugs for solid tumors.9,30-36
py for 3 additional months (CA-125 Goals of palliative chemotherapy for cancer
01/11/2016 = 102.7; 02/11/2016 = 296.8; after fourth line are mainly directed at con-
03/08/2016 = 465.8; 04/08/2016 = 662.2 at trolling symptoms, preventing secondary
baseline). Another fluid aspirate (pleural burdens of toxicities, providing ease of Conclusions
this time) was sent to the ChemoID lab for access, limiting impact on patients’ quality
testing, which suggested resistance to cis- of time, avoid hospitalizations as far as pos- The current case demonstrates the utili-
platinum and paclitaxel, but sensitivity to sible, reducing economic burden of testing, ty of ChemoID® guidance to commonly
gemcitabine, ifosfamide and docetaxel and permitting access to testing at point of available drugs with identified toxicity pro-
(Table 2). Due to CKD the patient was service. files and predictable cost profile available at
treated with sixth-line Avastin 15mg/m2 The introduction of platinum-based POS, along with rapid response in correct-
drugs and paclitaxel has been a landmark ing symptomatic disease features, and min-
q3weeks instead, which was selected as no
development in the treatment of ovarian imal treatment burden from toxicities. We
prior exposure, although it was untested by
cancer. However, there has been little observed in the reported case the survival
the ChemoID® assay. Patient progressed on
progress in long-term survival improvement and symptom management benefits of
sixth-line chemotherapy and expired under
since the last 30 years. ChemoID® guided therapy even after
inpatient management under management
Available reported options for fourth plateau of response (9-10 months similar to
for supportive care.
line chemotherapy or beyond are limited to prior regimens after first line platinum
In our case study patient enjoyed 7 and
the data provided by the Aurelia trial of low response). Further studies are indicated to
one-half year survival after initial poor
increase the clinical adoption of ChemoID®
ly
prognosis diagnosis with aggressive cytore- dose taxol and low dose avastin, or by
for gynecological malignancies in the pal-
duction and persistent efforts at chemother- administration of PARP inhibitors in case of
liative setting.
on
apy. Patient status was KPS 90 ECOG 0 or BRCA ½ positive testing. Cells with defec-
1 throughout her disease except for 1 month tive BRCA proteins are deficient in the
in June 2015 prior to ChemoID® and in last repair of double-stranded DNA breaks by
References
e
2 months of life. ChemoID® guided homologous recombination (HR) and rely
chemotherapy selection afforded 9-10
month fifth-line chemotherapy response
us
on other pathways to repair DNA damage,
notably the PARP pathway that detects sin-
1. Jemal A, Siegel R, Ward E, et al. Cancer
statistics, 2009. CA Cancer J Clin
with KPS 90 and ECOG 0-1 status with gle DNA strand breaks and activates a num- 2009;59:225-49.
al
symptomatic control of effusions facilitated ber of effector proteins to initiate repair. 2. Jemal A, Siegel R, Ward E, et al. Cancer
by use of standard drugs. Drugs selected Administration of ineffective anticancer statistics, 2008. CA Cancer J Clin
ci
with current chemotherapy-induced nausea therapy is associated with unnecessary tox- 2008;58:71-96.
and vomiting (CINV) agents available icity and the development of more aggres-
er
3. Partridge EE, Barnes MN. Epithelial
caused less than grade-1 nausea, no vomit- sive cancer cell clones that are resistant to ovarian cancer: prevention, diagnosis,
subsequent therapies.7,8 Anticancer drugs
m
ing, and no recurrent peripheral neuropathy and treatment. CA Cancer J Clin
at dosages selected. have a high rate of failure and cell culture 1999;49:297-320.
m
chemotherapy testing have been used to 4. Seidman JD, Horkayne-Szakaly I,
identify which drugs are more likely to be Haiba M, et al. The histologic type and
co
effective especially against those of gyne- stage distribution of ovarian carcinomas
Discussion cological origin.10,11 However, this approach of surface epithelial origin. Int J
has been hindered by the chemotherapy Gynecol Pathol 2004;23:41-4.
on
Despite tremendous advances in sur- testing only being performed on bulk of 5. Selvaggi SM. Tumors of the ovary,
gery, primary chemotherapy, and novel tumor cells derived from cancer biopsies.12- maldeveloped gonads, fallopian tube,
treatments for recurrent disease, the diagno- It is known that cancer stem cells (CSCs) and broad ligament. Arch Pathol Lab
N
21
sis of advanced epithelial ovarian cancer in contribute to tumorigenesis, treatment Med 2000;124:477.
2016 remains ultimately fatal in the majori- resistance and tumor recurrence22-29 in ovar- 6. Giornelli GH. Management of relapsed
ty of cases. The main goals of chemothera- ian cancer. ovarian cancer: a review. Springerplus
py for recurrent/refractory ovarian cancer ChemoID® is a functional test that uses 2016;5:1197.
are the palliation of disease-related symp- patient’s live tumor cells to indicate which 7. Ahmed N, Abubaker K, Findlay J,
toms, and improvement of quality and chemotherapy or combination will kill not Quinn M. Cancerous ovarian stem cells:
quantity of life.37 Unfortunately, the impact only the bulk tumor cells, but more impor- obscure targets for therapy but relevant
of palliative chemotherapy on survival, tantly the cancer stem cells (CSCs) that are to chemoresistance. J Cell Biochem
quality of life and cost in advanced ovarian known to cause cancer to recur. This consti- 2013;114:21-34.
cancer are largely still unknown as there tutes an important advantage of ChemoID® 8. Ahmed N, Abubaker K, Findlay JK.
have been no studies comparing palliative approach over other cell culture testing Ovarian cancer stem cells: Molecular
treatment with best supportive care. There methods. Our recent clinical studies showed concepts and relevance as therapeutic
is some contradicting evidence to suggest that patient derived CSCs from primary targets. Mol Aspects Med 2014;39:110-
that chemotherapy has a role in palliation of cancer cell cultures can be used in a drug 25.
symptoms with an apparent improvement in response assay.9,30-36 We have optimized the 9. Mathis SE, Alberico A, Nande R, et al.
quality of life37 as well as recent reports of enrichment of CSCs from tumor biopsies Chemo-predictive assay for targeting
lack of survival benefit of patients who are and have developed the ChemoID® cancer stem-like cells in patients affect-
treated with empirically chosen chemother- chemotherapy response assay, which meas- ed by brain tumors. PLoS One
[page 74] [Translational Medicine Reports 2017; 1:6701]
Case Report
2014;9:e105710. Cancer 2011;21:494-9. 29. Cioffi M, D’Alterio C, Camerlingo R, et
10. Bhagwandin S, Naffouje S, Salti G. 19. Ness RB, Wisniewski SR, Eng H, al. Identification of a distinct population
Utility of chemoresponse assay in Christopherson W. Cell viability assay of CD133(+)CXCR4(+) cancer stem
patients undergoing cytoreductive sur- for drug testing in ovarian cancer: in cells in ovarian cancer. Sci Rep
gery plus hyperthermic intraperitoneal vitro kill versus clinical response. 2015;5:10357.
chemotherapy. Ann Surg Oncol Anticancer Res 2002;22:1145-9. 30. Cortese A, Pantaleo G, Amato M, et al.
2015;22:2573-7. 20. Rice SD, Cassino TR, Sakhamuri L, et A new complementary procedure for
11. Grendys EC Jr., Fiorica JV, Orr JW Jr., al. An in vitro chemoresponse assay patients affected by head and neck can-
et al. Overview of a chemoresponse defines a subset of colorectal and lung cer: Chemo- predictive assay. Int J Surg
assay in ovarian cancer. Clin Transl carcinomas responsive to cetuximab. Case Rep 2016;26:42-6.
Oncol 2014;16:761-9. Cancer Biol Ther 2011;11:196-203. 31. Kelly SE, Di Benedetto A, Greco A, et
12. Brower SL, Fensterer JE, Bush JE. The 21. Rice SD, Heinzman JM, Brower SL, et al. Rapid selection and proliferation of
ChemoFx assay: an ex vivo chemosen- al. Analysis of chemotherapeutic CD133+ cells from cancer cell lines:
sitivity and resistance assay for predict- response heterogeneity and drug clus- chemotherapeutic implications. PLoS
ing patient response to cancer tering based on mechanism of action One 2010;5:e10035.
chemotherapy. Methods Mol Biol using an in vitro assay. Anticancer Res. 32. Claudio PP, Mathis SE, Nande R, et al.
2008;414:57-78. 2010;30:2805-11. ChemoID Assay for Glioblastoma.
13. Ochs RL, Burholt D, Kornblith P. The 22. Lin J, Ding D. The prognostic role of Chicago, IL: ASCO Annual Meeting;
ChemoFx assay: an ex vivo cell culture the cancer stem cell marker CD44 in 2015.
assay for predicting anticancer drug ovarian cancer: a meta-analysis. Cancer 33. Claudio PP, Mathis SE, Nande R, et al.
responses. Methods Mol Med Cell Int 2017;17:8. Novel chemosensitivity assay for tar-
2005;110:155-72. 23. Wiechert A, Saygin C, Thiagarajan PS, geting cancer stem-like cells in brain
14. Breidenbach M, Rein DT, Mallmann P, et al. Cisplatin induces stemness in tumors. Chicago, IL: ASCO Annual
ly
Kurbacher CM. Individualized long- ovarian cancer. Oncotarget 2016;7: Meeting; 2014.
on
term chemotherapy for recurrent ovari- 30511-22. 34. Claudio PP, Valluri J, E Mathis SE, et
an cancer after failing high-dose treat- 24. Shi YY, Jiang H. Prognostic role of the al. Chemopredictive assay for patients
ment. Anticancer Drugs 2002;13:173-6. cancer stem cell marker CD44 in ovari- with primary brain tumors. Chicago,
e
15. Ballard KS, Tedjarati SS, Robinson an cancer: a meta-analysis. Genet Mol IL: ASCO Annual Meeting; 2013.
WR, et al. Embryonal rhabdomyosarco- Res. 2016;15:3. us 35. Howard CM, Valluri J, Claudio PP.
ma: adjuvant and ex vivo assay-directed 25. Sharrow AC, Perkins B, Collector MI, Functional drug response assay for can-
chemotherapy. Int J Gynecol Cancer et al. Characterization of aldehyde cer stem cells in the era of precision
2010;20:561-3. dehydrogenase 1 high ovarian cancer medicine. Transl Med Rep 2017;1:1.
al
16. Gallion H, Christopherson WA, cells: Towards targeted stem cell thera- 36. Howard CM, Valluri V, Alberico A, et
ci
Coleman RL, et al. Progression-free py. Gynecol Oncol 2016;142:341-8. al. Analysis of chemo-predictive assay
interval in ovarian cancer and predictive 26. Deng J, Wang L, Chen H, et al. for targeting cancer stem cells in
er
value of an ex vivo chemoresponse Targeting epithelial- mesenchymal tran- glioblastoma patients. Transl Oncol
assay. Int J Gynecol Cancer 2006;16: sition and cancer stem cells for 2017;10:241-54.
m
194-201. chemoresistant ovarian cancer. 37. Patnaik A, Doyle C, Oza AM. Palliative
17. Herzog TJ, Krivak TC, Fader AN, Oncotarget 2016;7:55771-88. therapy in advanced ovarian cancer:
m
Coleman RL. Chemosensitivity testing 27. Zhou Q, Chen A, Song H, et al. balancing patient expectations, quality
with ChemoFx and overall survival in Prognostic value of cancer stem cell of life and cost. Anticancer Drugs
co
primary ovarian cancer. Am J Obstet marker CD133 in ovarian cancer: a 1998;9:869-78.
Gynecol 2010;203:68 e1-6. meta-analysis. Int J Clin Exp Med 38. Utsumi F, Kajiyama H, Niimi K, et al.
18. Huh WK, Cibull M, Gallion HH, et al. 2015;8:3080-8. Clinical significance and predicting
on
Consistency of in vitro chemoresponse 28. Ozakpinar OB, Maurer AM, Ozsavci D. indicators of post-cancer-treatment sur-
assay results and population clinical Ovarian stem cells: From basic to clini- vival in terminally ill patients with
N
response rates among women with cal applications. World J Stem Cells ovarian cancer. J Obstet Gynaecol Res
endometrial carcinoma. Int J Gynecol 2015;7:757-68. 2017;43:365-70.
[Translational Medicine Reports 2017; 1:6701] [page 75]
Você também pode gostar
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeNo EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeNota: 4 de 5 estrelas4/5 (5794)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreNo EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreNota: 4 de 5 estrelas4/5 (1090)
- Never Split the Difference: Negotiating As If Your Life Depended On ItNo EverandNever Split the Difference: Negotiating As If Your Life Depended On ItNota: 4.5 de 5 estrelas4.5/5 (838)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceNo EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceNota: 4 de 5 estrelas4/5 (895)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersNo EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersNota: 4.5 de 5 estrelas4.5/5 (344)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureNo EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureNota: 4.5 de 5 estrelas4.5/5 (474)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)No EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Nota: 4.5 de 5 estrelas4.5/5 (120)
- The Emperor of All Maladies: A Biography of CancerNo EverandThe Emperor of All Maladies: A Biography of CancerNota: 4.5 de 5 estrelas4.5/5 (271)
- The Little Book of Hygge: Danish Secrets to Happy LivingNo EverandThe Little Book of Hygge: Danish Secrets to Happy LivingNota: 3.5 de 5 estrelas3.5/5 (399)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyNo EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyNota: 3.5 de 5 estrelas3.5/5 (2259)
- The Yellow House: A Memoir (2019 National Book Award Winner)No EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Nota: 4 de 5 estrelas4/5 (98)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaNo EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaNota: 4.5 de 5 estrelas4.5/5 (266)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryNo EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryNota: 3.5 de 5 estrelas3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnNo EverandTeam of Rivals: The Political Genius of Abraham LincolnNota: 4.5 de 5 estrelas4.5/5 (234)
- The Unwinding: An Inner History of the New AmericaNo EverandThe Unwinding: An Inner History of the New AmericaNota: 4 de 5 estrelas4/5 (45)
- JUMPSTART TO SKINNY by Bob Harper: Rule #1Documento8 páginasJUMPSTART TO SKINNY by Bob Harper: Rule #1Random House Publishing GroupAinda não há avaliações
- RISK ASSESSMENT REPORT - George Municipality - Tender ENG0042016 Installation of Perimeter Concrete Palisade FeDocumento10 páginasRISK ASSESSMENT REPORT - George Municipality - Tender ENG0042016 Installation of Perimeter Concrete Palisade FeemmyAinda não há avaliações
- IGCSE Biology (O610) Workbook: Balanced DietDocumento5 páginasIGCSE Biology (O610) Workbook: Balanced DietPatrick Abidra100% (1)
- FEDIAF Nutritional Guidelines 2020 20200917Documento96 páginasFEDIAF Nutritional Guidelines 2020 20200917luciana ribeiroAinda não há avaliações
- EVOLUTION OF MODELS OF DISABILITY Notes OnlyDocumento1 páginaEVOLUTION OF MODELS OF DISABILITY Notes OnlyLife HacksAinda não há avaliações
- PsikosomatikDocumento65 páginasPsikosomatikHengki Permana PutraAinda não há avaliações
- Personality Disorders PDFDocumento35 páginasPersonality Disorders PDFABHINAVAinda não há avaliações
- Comm 806 NoteDocumento201 páginasComm 806 Notelyndaignatius45Ainda não há avaliações
- Mylan EpiPen StatementDocumento3 páginasMylan EpiPen StatementCBS This MorningAinda não há avaliações
- Position Paper de l'UEFA Sur L'interdiction Du Gazon Synthétique Par l'ECHA 19 Juillet 2019Documento8 páginasPosition Paper de l'UEFA Sur L'interdiction Du Gazon Synthétique Par l'ECHA 19 Juillet 2019LeMonde.frAinda não há avaliações
- Final Project DescriptionDocumento6 páginasFinal Project DescriptionCahyani DamawatiAinda não há avaliações
- Benefit Manual Group Health Insurance - CMSDocumento35 páginasBenefit Manual Group Health Insurance - CMSUmang WarudkarAinda não há avaliações
- Trail Mix Cookies IKDocumento24 páginasTrail Mix Cookies IKDwi Intan WAinda não há avaliações
- Response To States 4.2 Motion in Limine Character of VictimDocumento10 páginasResponse To States 4.2 Motion in Limine Character of VictimLaw of Self DefenseAinda não há avaliações
- Test AaDocumento55 páginasTest AaKaye PatanindagatAinda não há avaliações
- Maharashtra Public Service Commission Maharashtra Subordinate Services Main Examination - 2019Documento59 páginasMaharashtra Public Service Commission Maharashtra Subordinate Services Main Examination - 2019S KatyarmalAinda não há avaliações
- Current Clinical Strategies: Handbook of AnesthesiologyDocumento180 páginasCurrent Clinical Strategies: Handbook of AnesthesiologydramaganaAinda não há avaliações
- ERAS Protocols For Thyroid andDocumento9 páginasERAS Protocols For Thyroid andOskar MartinezAinda não há avaliações
- Notice: Agency Information Collection Activities Proposals, Submissions, and ApprovalsDocumento2 páginasNotice: Agency Information Collection Activities Proposals, Submissions, and ApprovalsJustia.comAinda não há avaliações
- Asa PSC System PDFDocumento2 páginasAsa PSC System PDFKen WonAinda não há avaliações
- SR - Hse Officer (8104)Documento5 páginasSR - Hse Officer (8104)Nijo Joseph100% (1)
- The Effectiveness of Information System in Divine Mercy Hospitalsan Pedro LagunaDocumento22 páginasThe Effectiveness of Information System in Divine Mercy Hospitalsan Pedro LagunamartAinda não há avaliações
- Acl Reconstruction Without Meniscus RepairDocumento1 páginaAcl Reconstruction Without Meniscus Repairsathvik gowdaAinda não há avaliações
- Public Health Internship Cover LetterDocumento8 páginasPublic Health Internship Cover Letterf5dct2q8100% (2)
- Nejmra 2023911Documento8 páginasNejmra 2023911Merry LeeAinda não há avaliações
- Leptospirosis PDFDocumento48 páginasLeptospirosis PDFTuan HaikalAinda não há avaliações
- Assoc Between Poor Sleep Quality - Depression Symptoms Among ElderlyDocumento8 páginasAssoc Between Poor Sleep Quality - Depression Symptoms Among ElderlyWindyanissa RecitaAinda não há avaliações
- Health Opportunities Through Physical EducationDocumento8 páginasHealth Opportunities Through Physical EducationAngel Erica TabigueAinda não há avaliações
- Sq20-030 - Fact Sheet - Informed Consent - Nsqhs-8.9aDocumento4 páginasSq20-030 - Fact Sheet - Informed Consent - Nsqhs-8.9aPedro Medeiros JrAinda não há avaliações
- Pres 2 PastpapersDocumento190 páginasPres 2 PastpapersOdetteAinda não há avaliações