Escolar Documentos
Profissional Documentos
Cultura Documentos
Acute Coronary Syndrome
Enviado por
choobiTítulo original
Direitos autorais
Formatos disponíveis
Compartilhar este documento
Compartilhar ou incorporar documento
Você considera este documento útil?
Este conteúdo é inapropriado?
Denunciar este documentoDireitos autorais:
Formatos disponíveis
Acute Coronary Syndrome
Enviado por
choobiDireitos autorais:
Formatos disponíveis
Acute coronary syndrome
Patients with acute coronary syndrome have some degree of coronary artery occlusion. The degree of
occlusion defines whether the acute coronary syndrome is: • unstable angina • non–ST segment
elevation MI (non-STEMI) • ST segment elevation MI (STEMI).The development of acute coronary
syndrome begins with a rupture or erosion of plaque, an unstable and lipid-rich substance. The rupture
results in platelet adhesions, fibrin clot formation, and thrombin activation.
What causes it
Patients with certain risk factors appear to face a greater likelihood of developing acute coronary
syndrome.
These factors include:
• diabetes
• family history of heart disease
• hypertension
• obesity
• high-fat, high-carbohydrate diet
• sedentary lifestyle
• menopause
• hyperlipoproteinemia
• smoking
• stress.
How it happens
Acute coronary syndrome most commonly results when a thrombus progresses and occludes blood
flow. (An early thrombus doesn’t necessarily block blood flow.) The effect is an imbalance in myocardial
oxygen supply and demand.
Degree and duration
The degree and duration of blockage dictate the type of infarct:
• If the patient has unstable angina, a thrombus partially occludes a coronary vessel. The thrombus is
full of platelets. The partially occluded vessel may have distal microthrombi that cause necrosis in some
myocytes.
• If smaller vessels infarct, the patient is at higher risk for MI, which may progress to a non-STEMI.
Usually, only the innermost layer of the heart is damaged.
• STEMI results when reduced blood flow through one of the coronary arteries causes myocardial
ischemia, injury, and necrosis. The damage extends through all myocardial layers. What to look for A
patient with angina typically experiences:
• burning
• squeezing
Você também pode gostar
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeNo EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeNota: 4 de 5 estrelas4/5 (5794)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreNo EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreNota: 4 de 5 estrelas4/5 (1090)
- Never Split the Difference: Negotiating As If Your Life Depended On ItNo EverandNever Split the Difference: Negotiating As If Your Life Depended On ItNota: 4.5 de 5 estrelas4.5/5 (838)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceNo EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceNota: 4 de 5 estrelas4/5 (895)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersNo EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersNota: 4.5 de 5 estrelas4.5/5 (345)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureNo EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureNota: 4.5 de 5 estrelas4.5/5 (474)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)No EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Nota: 4.5 de 5 estrelas4.5/5 (121)
- The Emperor of All Maladies: A Biography of CancerNo EverandThe Emperor of All Maladies: A Biography of CancerNota: 4.5 de 5 estrelas4.5/5 (271)
- The Little Book of Hygge: Danish Secrets to Happy LivingNo EverandThe Little Book of Hygge: Danish Secrets to Happy LivingNota: 3.5 de 5 estrelas3.5/5 (400)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyNo EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyNota: 3.5 de 5 estrelas3.5/5 (2259)
- The Yellow House: A Memoir (2019 National Book Award Winner)No EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Nota: 4 de 5 estrelas4/5 (98)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaNo EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaNota: 4.5 de 5 estrelas4.5/5 (266)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryNo EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryNota: 3.5 de 5 estrelas3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnNo EverandTeam of Rivals: The Political Genius of Abraham LincolnNota: 4.5 de 5 estrelas4.5/5 (234)
- The Unwinding: An Inner History of the New AmericaNo EverandThe Unwinding: An Inner History of the New AmericaNota: 4 de 5 estrelas4/5 (45)
- CIP Com Dev 2018Documento4 páginasCIP Com Dev 2018choobiAinda não há avaliações
- Advanced Concepts in Critical Care NursingDocumento3 páginasAdvanced Concepts in Critical Care Nursingchoobi100% (1)
- ACCOMPLISHMENT REPORT On FAC. DEVDocumento3 páginasACCOMPLISHMENT REPORT On FAC. DEVchoobiAinda não há avaliações
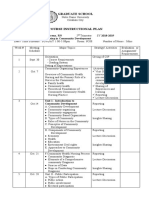
- Nres 1 Instructional PlanDocumento10 páginasNres 1 Instructional PlanchoobiAinda não há avaliações
- NEW BSN CURRICULUM - CMO 15 RevisedDocumento2 páginasNEW BSN CURRICULUM - CMO 15 RevisedchoobiAinda não há avaliações
- Universal Prec QuestionsDocumento8 páginasUniversal Prec QuestionschoobiAinda não há avaliações
- level-of-disaster-preparedness-EDITED 1Documento16 páginaslevel-of-disaster-preparedness-EDITED 1choobiAinda não há avaliações
- EVAL School Health NursingDocumento4 páginasEVAL School Health NursingchoobiAinda não há avaliações
- Assessment of Pulse SitesDocumento2 páginasAssessment of Pulse SiteschoobiAinda não há avaliações
- Nurse RoleDocumento1 páginaNurse RolechoobiAinda não há avaliações
- Quiz On School Health NursingDocumento7 páginasQuiz On School Health Nursingchoobi0% (2)
- Your Time Is LimitedDocumento1 páginaYour Time Is LimitedchoobiAinda não há avaliações
- Caselet School HealthDocumento3 páginasCaselet School HealthchoobiAinda não há avaliações
- Eval Exam CHNDocumento4 páginasEval Exam CHNchoobiAinda não há avaliações
- Community Health Nursing Exam 2Documento8 páginasCommunity Health Nursing Exam 2choobi100% (9)