Escolar Documentos
Profissional Documentos
Cultura Documentos
History of Osteosynthesis
Enviado por
Pankaj Vatsa0 notas0% acharam este documento útil (0 voto)
34 visualizações9 páginasTítulo original
HISTORY OF OSTEOSYNTHESIS.docx
Direitos autorais
© © All Rights Reserved
Formatos disponíveis
DOCX, PDF, TXT ou leia online no Scribd
Compartilhar este documento
Compartilhar ou incorporar documento
Você considera este documento útil?
Este conteúdo é inapropriado?
Denunciar este documentoDireitos autorais:
© All Rights Reserved
Formatos disponíveis
Baixe no formato DOCX, PDF, TXT ou leia online no Scribd
0 notas0% acharam este documento útil (0 voto)
34 visualizações9 páginasHistory of Osteosynthesis
Enviado por
Pankaj VatsaDireitos autorais:
© All Rights Reserved
Formatos disponíveis
Baixe no formato DOCX, PDF, TXT ou leia online no Scribd
Você está na página 1de 9
HISTORY OF OSTEOSYNTHESIS
• The term osteosynthesis was coined by
Albin Lambotte a Belgian surgeon
regarded universally as the father of the
modern internal and external fixation. He
devised an external fixator and numerous
different plates and screws.
• Robert Danis as surgeon in Brussel
published two books on osteosynthesis in
1932 and 1949.
• A young swiss surgeon E. muller read his
second book and he drew around
himself a group of interested swiss
surgeons and in 1958, at an historical
weekend meeting in chur they decided
to form a study group concerning issue
of internal fixation of bone- the
Arbeitgemeinschaft fur Osteosynthesefragen, or AO.
Principles of AO :
• 1. Anatomical Reduction.
• 2. Stable internal fixation.
• 3. Preservation of Blood supply
• 4. Early active pain free mobilisation.
BIOMECHANICAL ASPECTS OF
THE AO TECHNIQUE
• Neutralization Plate or Protection Plate
• Compression Plating
• Lag screw
• Tension Band Principle
• Intra Medullary Nailing
• External Fixation.
PLATES
Introduction :
• Bone plates are like internal splints holding
together the fractured ends of a bone.
• A bone plate has two mechanical functions. It
transmits forces from one end of a bone to
the other, bypassing and thus protecting the
area of fractures. It also holds the fracture
ends together while maintaining the proper
alignment of the fragments throughout the
healing process.
Standard Plates
• Narrow DCP-4.5 mm
• Broad DCP – 4.5 mm
• 3.5 mm DCP
• LC-DCP 3.5 & 4.5mm
• Reconstruction plate 3.5 & 4.5mm
• 1/3 tubular plate 2.7, 3.5 & 4.5 mm
Special Plates
• T Plates
• T&L Buttress plates
• Lateral Tibial head buttress plates
• Condylar buttress plate
• Narrow lenthening plates
• Broad Lengthening plate
• Spoon plate
• Clover leaf plate
CLASSIFICATION
• Regardless of their length, thickness,
geometry, configuration or type of holes,
all pates may be classified in four groups
according to their function.
• Neutralization Plates.
• Compression Plates.
• Buttress Plates.
Buttress
Position
Neutral
Position
Load
Position
NEUTRALIZATION PLATE
• A neutralization plate acts as a ""bridge". It
transmits various forces from one end of the bone
to the other, bypassing the area of the fracture.
Its main function is to act as a mechanical link
between the healthy segments of bone above and
below the fracture. Such a plate does not produce
any compression at the fracture site.
• The most common clinical application of the
neutralization plate is to protect the screw fixation
of a short oblique fracture, a butterfly fragment or
a mildly comminuted fracture of a long bone, or
for the fixation of a segmental bone defect in
combination with bone grafting.
COMPRESSION PLATE
• A compression plate produces a locking force
across a fracture site to which it is applied.
The effect occurs according to Newton's Third
Law (action and reaction are equal opposite).
The plate is attached to a bone fragment. It is
then pulled across the fracture site by a
device, producing tension in the plate. As a
reaction to this tension, compression is
produced at the fracture site across which the
plate is fixed with the screws. The direction of
the compression force is parallel to the plate.
Application of Compression Plate
BONE UNDER COMPRESSION
• Superior stability – Utilization of
physiological forces.
• Improved milieu for bone healing.
• Early mobilization.
BUTTRESS PLATE
• The mechanical function of this plate, as the
name suggests, is to strengthen (buttress) a
weakened area of cortex. The plate prevents the
bone from collapsing during the healing process.
It is usually designed with a large surface area
to facilitate wider distribution of the load.
• A buttress plate applied a force to the bone
which is perpendicular (normal) to the flat
surface of the plate.
• The fixation to the bone should begin in
the middle of the plate, i.e. closest to the
fracture site on the shaft. The screws
should then be applied in an orderly
fashion, one after the other, towards both
ends of the plate.
• A representative clinical example of a
buttress plate is the T-plate used for the
fixation of fractures of the distal radius
and the tibial plateau.
DCP (Dynamic Compression Plate):
Principle :
- Its a self compression plate due to the
special geometry of screw holes which
allow the axial compression.
Dynamic compression principle: The holes of the plate are
shaped like an inclined and transverse cylinder. Like a ball, the
screw head slides down the inclined cylinder. Because the screw
head is fixed to the bone via the shaft, it can only move vertically
relative to the bone. The horizontal movement of the head, as it
impacts the angled side of the hole, results in movement of the
bone fragment relative to the plate and leads to compression of
the fracture.
• Screw hole and the spherical gliding
principle.
• Axial compression result from the an interplay
between screw hole geometry and eccentric
placement of the screw in the screw hole. The
screw hole is a combination of incline and
horizontal cylinder which permits the downward
and the horizontal movement of a sphere the
screw hand. Sideway movement of screw head
is impossible. The aim is to position the screw
head at the intersection of inclined and the
horizontal cylinder. At this point screw head has
a spherical contact in the screw hole which
result in the maximum stability without
completely blocking the horizontal movement of
the screw.
General principles of internal fixation.
The shape of the holes of the dynamic compression
plate allows inclination of the screws in a transverse
direction of +7° and in a longitudinal direction of
25°.
Advantage of DCP :
1. Inclined insertion 25° longitudinal and 7°
sideways.
2. Placement of a screw in neutral position without
the danger of distraction of fragments.
3. Insertion of a load screw for the compression.
4. Usage of two load screws in the main
fragments for axial compression.
5. Compression of several fragments individually in
comminuted fractures.
6. Application as a buttress plate in articular area.
Short Coming of DCP :
1. Flat under surface.
2. Inclination upto 25°
3. Plate hole distribution (extended middle
segment)
The structure of a limited-contact dynamic compression plate.
LC-DCP
In the dynamic compression plate (A), the area at the
plate holes is less stiff than the area between them.
During bending, the plate tends to bend only in the areas
of the hole. The limited-contact dynamic compression
plate (B) has an even stiffness without the risk of
buckling at the screw holes.
• The LC-DCP (limited contact DCP) is a further
development of the DCP is used for the same
indications as the DCP, but the improved design
offers additional advantage.
• The evenly distributed undercuts reduces the
contact area between bone and plate to a
minimum. This significantly reduces impairment
of the blood supply of the underlying cortical
bone undercuts also allow for the formation of a
small callusbridge.
• The enlarged cross section at the plate holes and
the reduced cross section between holes offer a
constant degree of stiffness along the long axis
of the plate.
• The trapezoid cross section of the plate
results in a smaller contact area between
plate and bone.
• The plate holes are uniformaly spaced,
which permits easy positioning of the
plate.
• Undercuts plate holes; undercut at each
end of the plate hole allows 40 tilting of
screws both ways along the long axis of
the plate. Lag screw fixation of short
oblique fractures is thereby possible.
Bridge Plating :
Bridge Plating for
comminuted fracture
Wave Plating :
Wave Plating for
non union.
ADDITIONAL PRINCIPLES OF
PLATE FIXATION
• The engineering principle of the tension
band is widely used in fracture fixation. It
applies to the conversion of tensile forces
to compression forces on the convex side
of an eccentrically loaded bone.
PREBENDING PLATES
• Contour to fit the bone surface snugly.
• Make a sharp bend opposite the fracture
site; midsection is elevated.
• Fix to the bone, starting on either side of
the fracture and then moving outwards.
• Plate then compresses the far cortex also.
• Apply only to two fragment fractures.
HOW MANY SCREWS ?
• Hands-on experience suggests that, in the
humerus, screws grip seven cortices on each
side of the fracture ; in the radius and the ulna,
five; in the tibia, six, and in the femur, seven.
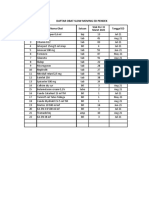
Type of
Bones No. of Cortices
Plate
Clavicle 5 to 6 Cortex 6 holes`
Femur 7 to 8 Cortex 8 holes
Tibia 7 to 8 Cortex 7 holes
Humerus 7 to 8 Cortex 8 holes
Forearm 5 to 6 Cortex 6 holes
HOW CLOSE TO THE FRACTURE SITE?
• A screw, as a result, should not be placed
closer than one centimeter from the
fracture line.
Reconstruction Plates :
• Can be bent and twisted in two
dimensions.
• Decrease stiffness than DCP.
• Should not be bent more than 15°.
• Used were the exact and complex
contouring is required. eg. Pelvis, Distal
Humerus, Clavicle.
Reconstruction plates are thicker than third tubular plates but not
quite as thick as dynamic compression plates. Designed with deep
notches between the holes, they can be contoured in 3 planes to fit
complex surfaces, as around the pelvis and acetabulum.
Reconstruction plates are provided in straight and slightly thicker and
stiffer precurved lengths. As with tubular plates, they have oval screw
holes, allowing potential for limited compression.
One Third Tubular Plates :
• Plates have the form of one third of the
circumference of a cylinder.
• Low rigidity (1mm thick).
• Oval holes – Axial compression can be
achieved.
• Uses – Lateral malleolus, distal ulna,
metatarsals.
limited stability. The thin design allows for easy shaping
and is primarily used on the lateral malleolus and distal
ulna. The oval holes allow for limited fracture
compression with eccentric screw placement.
LOCKING COMPRESSION PLATE (LCP)
Principle :
• The basic principle of LCP is its angular stability
whereas stability of conventional plate
osteosynthesis relies on the friction between
the plate and bone.
• The principle of fixation of LCP is screw locking.
• The functional LCP screw is like that of external
fixator pins, that is why they are called as
internal fixator.
• LCP provides the relative stability.
• # heals by the callus formation (Secondary
Healing).
The mechanical principle of a locked screw plate. (A) The
plate sits slightly of the bone. (B) Tightening of the screw
locks the screw head within the plate. The plate is not
drawn toward the bone and there is no compression b/w
the bone and the plate. The flux is bone/ screw/ plate/
screw/ bone.
Maintenance of primary reduction
Once the locking screws engage the plate, no further
tightening is possible. Therefore, the implant locks the bone
segments in their relative positions regardless of degree of
reduction. Precontouring the plate minimizes the gap
between the plate and the bone, but an exact fit is not
necessary for implant stability. This feature is especially
advantageous in minimally or less invasive plating
techniques because these techniques do not allow exact
contouring of the plate to the bone surface.
Bridge/Locked Plating Using
Locking Screws
• Screws lock to the plate, forming a
fixed-angle construct.
• Bone healing is achieved indirectly
by callus formation when using
locking screws exclusively.
Stability under load
By locking the screws to the
plate, the axial force is
transmitted over the length of the
plate. The risk of a secondary
loss of the intraoperative
reduction is reduced.
Blood supply to the bone
Locking the screw into the plate
does not generate additional
compression. Therefore, the
periosteum will be protected and
the blood supply to the bone
preserved.
Plate Design :
• LC DCP features :
• Tapered end for
sub
muscular insertion.
• Locking holes
Screw :
• Conical screw head
• Large core diameter.
• Self tapping.
• Star drive recess.
Principle of internal fixation
using LCP :
1. 1st reduced the # as anatomical as possible.
2. Cortical screw should be used 1st in a fracture
fragment.
3. If the locking screw have been put, use of the
cortical screw in the same fragment without
loosening and retightening of the locking
screw is not recommended.
4. If locking screw is used first avoid spinning of
plates.
5. Unicortical screws causes no loss of stability.
6. Osteoporotic bones bicortical screws
should be used.
7. In the comminuted # screw holes
close to the fracture should be used
to reduce stain.
8. In the fracture with small or no gap
the immediate screw holes should be
left unfilled to reduced the strain.
Plate length and No. of Screws :
Plate length
Plate span ratio # length
PSR 2
Comminuted #
PSR 8
Simple # No. of Screws
Plate Screw density No. of Plate holes
0.5 to 0.4
PSD
- At least 4 cortices per main fragment for
comminuted fracture
- At least 3 cortices per main fragment for simple
fracture.
Plate screw density and fracture plate quotient
Indications :
1. Osteoporotic #
2. Periprosthetic #
3. Multifragmentry #
4. Delayed change from external fixation to internal
fixation.
Advantages :
1. Angular stability
2. Axial stability
3. Plate contouring not required
4. Less damage to the blood supply of bone.
5. Decrease infection because of submuscular
technique
6. Less soft tissue damage.
Timing of Plate Removal,
Recommendations for removal of
plates in the lower limb :
• Bone / Fracture
• Time after implantation in months
• Malleolar fractures
• 8-12
• The tibial pilon
• 12-18
• The tibial shaft
• 12-18
• The tibial head
• 12-18
• The femoral condyles
• 12-24
• The femoral shaft: Single plate, Double Plate
• 24-36
• From month 18, in 2 steps ( Interval 06 months)
• Pertrochanteric and femoral neck fractures Upper
extremity
• 12-18
• Optional
• Shaft of radius / ulna
• 24-28
• Distal radius
• 8-12
• Metacarpals
Você também pode gostar
- Plate and Screw TraumaDocumento46 páginasPlate and Screw Traumaianfajar8Ainda não há avaliações
- Plates and Screws Overview: Types, Functions and ApplicationsDocumento45 páginasPlates and Screws Overview: Types, Functions and ApplicationsIan OrwaAinda não há avaliações
- Plates: Iwan B Anwar. Dr. SpotDocumento59 páginasPlates: Iwan B Anwar. Dr. SpotTiffani ApriliaAinda não há avaliações
- Surgery IIExam 1 REVIEWDocumento6 páginasSurgery IIExam 1 REVIEWEddie MillsAinda não há avaliações
- AO Plates & Their ApplicationDocumento74 páginasAO Plates & Their ApplicationAbu ZidaneAinda não há avaliações
- Screw & Plate Fixation GuideDocumento45 páginasScrew & Plate Fixation GuideRichard 151289Ainda não há avaliações
- Bone Plating - CopyDocumento54 páginasBone Plating - CopyVet IrfanAinda não há avaliações
- Screws and Plates: Fixation Mechanisms ExplainedDocumento38 páginasScrews and Plates: Fixation Mechanisms ExplainedWasim R. IssaAinda não há avaliações
- Basic Orthopedic HardwareDocumento13 páginasBasic Orthopedic HardwareJennifer C. SumadsadAinda não há avaliações
- AO Plating Basics (Brief)Documento6 páginasAO Plating Basics (Brief)Jake sanchezAinda não há avaliações
- Anatomi FemurDocumento16 páginasAnatomi FemurRio Yus RamadhaniAinda não há avaliações
- Orthopedic HardwareDocumento6 páginasOrthopedic HardwarePrince R. DemandanteAinda não há avaliações
- Plates and ScrewsDocumento96 páginasPlates and ScrewsFathy AlhallagAinda não há avaliações
- Implants in OrthopaedicsDocumento20 páginasImplants in OrthopaedicsDr. F. Abdul KhaderAinda não há avaliações
- External FixatorsDocumento49 páginasExternal FixatorsdvenumohanAinda não há avaliações
- Screw PlacementDocumento32 páginasScrew PlacementDraconian1Ainda não há avaliações
- AO Principles of Fracture Treatment and Different Implant ModalitiesDocumento42 páginasAO Principles of Fracture Treatment and Different Implant ModalitiesmanjunathaAinda não há avaliações
- IMPLANTSDocumento24 páginasIMPLANTSHarsh PawarAinda não há avaliações
- Internalfixators 200331111710Documento31 páginasInternalfixators 200331111710Muhammad Abbas WaliAinda não há avaliações
- ProsthesisDocumento42 páginasProsthesissmrutiptAinda não há avaliações
- Selection of Attachment. MondayDocumento49 páginasSelection of Attachment. MondayIbrahim Ahmed DahabAinda não há avaliações
- Rigid Internal FixationDocumento72 páginasRigid Internal FixationDR NASIMAinda não há avaliações
- Large Fragment Locking Compression Plate (LCP) : Technique GuideDocumento23 páginasLarge Fragment Locking Compression Plate (LCP) : Technique GuideLouis MiuAinda não há avaliações
- Intramedullar Nail 3Documento39 páginasIntramedullar Nail 3Dr NIVEDITHA CAinda não há avaliações
- DR Ashwani Panchal Jss Medical College MysoreDocumento94 páginasDR Ashwani Panchal Jss Medical College MysoreAravind RvndAinda não há avaliações
- Dept. of Orthopaedics, KMC MangaloreDocumento8 páginasDept. of Orthopaedics, KMC MangalorechinmayghaisasAinda não há avaliações
- Principle of NailingDocumento62 páginasPrinciple of Nailingsharvindan subramaniamAinda não há avaliações
- Lecture 1 TF BiomechanicsDocumento63 páginasLecture 1 TF BiomechanicsAlfred JacksonAinda não há avaliações
- Koch AO Manual Chapter 2 2005Documento45 páginasKoch AO Manual Chapter 2 2005Juan Guillermo RamirezAinda não há avaliações
- R3 Surgical Technique - IntlDocumento27 páginasR3 Surgical Technique - Intlquetecojaunburro100% (1)
- K. Adwar. Internal Fixation of #S.Documento32 páginasK. Adwar. Internal Fixation of #S.Fathy AlhallagAinda não há avaliações
- Pricippriles of Intramedullary NailingDocumento57 páginasPricippriles of Intramedullary NailingAbdallah OmerAinda não há avaliações
- Operating Room PersonnelDocumento44 páginasOperating Room Personnelamir hamzahAinda não há avaliações
- The Use of Plates in Fracture FixationDocumento23 páginasThe Use of Plates in Fracture FixationhaminatrafAinda não há avaliações
- 2.3 Use of Plates in Fracture FixationDocumento22 páginas2.3 Use of Plates in Fracture FixationAlex DiconiAinda não há avaliações
- Basic Principles and Techniques of Internal Fixation of FracturesDocumento56 páginasBasic Principles and Techniques of Internal Fixation of FracturesRudi haris munandarAinda não há avaliações
- 03-06 Internal FixationDocumento69 páginas03-06 Internal Fixation69016Ainda não há avaliações
- Bridge Plating PDFDocumento4 páginasBridge Plating PDFKae 王珊婷 Wang100% (1)
- DHS BladeDocumento15 páginasDHS BladeIndah MukarromahAinda não há avaliações
- Implant SystemsDocumento103 páginasImplant SystemsBharathi GudapatiAinda não há avaliações
- AOAF Presentation LCPDocumento45 páginasAOAF Presentation LCPRajiv YadavAinda não há avaliações
- Ilizarov Fixator: DR Pratik AgarwalDocumento86 páginasIlizarov Fixator: DR Pratik AgarwaltesfahuntekletilahunAinda não há avaliações
- Basic Orthopedic Hardware TypesDocumento17 páginasBasic Orthopedic Hardware TypesDanica SayasAinda não há avaliações
- Minor Connector FunctionsDocumento91 páginasMinor Connector FunctionsNaveen ThakurAinda não há avaliações
- Prostho Short NotesDocumento84 páginasProstho Short Notessamiksha100% (1)
- Open Reduction Internal Fixation RifDocumento16 páginasOpen Reduction Internal Fixation RifNurul Hidayah100% (2)
- Finishing Stage Maxillary Cant CorrectionDocumento132 páginasFinishing Stage Maxillary Cant Correctionsahar emadAinda não há avaliações
- Type and Biomaterial ImplantDocumento36 páginasType and Biomaterial ImplantluthfisnetAinda não há avaliações
- No 6 Dan 7 Google TerjemahanDocumento10 páginasNo 6 Dan 7 Google TerjemahanWan Adi OeyaAinda não há avaliações
- Know your tools: Flexible intramedullary nailing (FINDocumento91 páginasKnow your tools: Flexible intramedullary nailing (FINmuhammad ammar naqviAinda não há avaliações
- Internal FixationDocumento22 páginasInternal Fixationlotd6002Ainda não há avaliações
- Stress Breakers A Device A MythDocumento21 páginasStress Breakers A Device A MythShree PrabhaAinda não há avaliações
- Internal Fixation ToolsDocumento22 páginasInternal Fixation ToolsChandan Kumar ChoubeyAinda não há avaliações
- Steel Connections-Lacing-Bridge BearingDocumento11 páginasSteel Connections-Lacing-Bridge BearingRaheelAfzaalAinda não há avaliações
- 4 Precision Attachments For Partial DenturesDocumento18 páginas4 Precision Attachments For Partial DenturespriyaAinda não há avaliações
- English Screws HandoutDocumento10 páginasEnglish Screws HandouteugenetbkAinda não há avaliações
- Torquing auxiliary mechanicsDocumento39 páginasTorquing auxiliary mechanicsGudiyA KaurAinda não há avaliações
- Module 3 - Joint Types in Machine DesignDocumento28 páginasModule 3 - Joint Types in Machine DesignMahmud HassanAinda não há avaliações
- Vishwastractionppt 160921124524Documento131 páginasVishwastractionppt 160921124524pascalmugodoAinda não há avaliações
- Reduction, Relocation and Splinting in Emergency Room (RASER)No EverandReduction, Relocation and Splinting in Emergency Room (RASER)Ainda não há avaliações
- Displasia de CaderaDocumento8 páginasDisplasia de CaderaElmer NarvaezAinda não há avaliações
- Pathogenesis and Clinical Aspects of Rheumatoid Arthritis: Ivan Padjen, Cem Gabay, Daniel AletahaDocumento83 páginasPathogenesis and Clinical Aspects of Rheumatoid Arthritis: Ivan Padjen, Cem Gabay, Daniel AletahaPankaj VatsaAinda não há avaliações
- Congenital Hip DislocationDocumento1 páginaCongenital Hip DislocationVarun KumarAinda não há avaliações
- Edge Marking 2001Documento22 páginasEdge Marking 2001Pankaj VatsaAinda não há avaliações
- SSL 0x6eec8e1848: I/O Error During System Call, Software Caused Connection AbortDocumento1 páginaSSL 0x6eec8e1848: I/O Error During System Call, Software Caused Connection AbortPankaj VatsaAinda não há avaliações
- Developmental Dysplasia of The Hip: Orthopedics and RheumatologyDocumento4 páginasDevelopmental Dysplasia of The Hip: Orthopedics and RheumatologyAsnita ZulqaidaAinda não há avaliações
- Management of Proximal Humeral FracturesDocumento16 páginasManagement of Proximal Humeral FracturesAustine OsaweAinda não há avaliações
- BOS Basic Arthroscopy Course ProgrammeDocumento4 páginasBOS Basic Arthroscopy Course ProgrammePankaj VatsaAinda não há avaliações
- ISHKS 2018 BrochureDocumento11 páginasISHKS 2018 BrochurePankaj VatsaAinda não há avaliações
- Arthroscopy Course 1219 FlierDocumento1 páginaArthroscopy Course 1219 FlierPankaj VatsaAinda não há avaliações
- Booklet Language Kit GermanDocumento16 páginasBooklet Language Kit GermanNarik PaluniAinda não há avaliações
- ASSH Manual of Hand Surgery PDFDocumento653 páginasASSH Manual of Hand Surgery PDFChis Alexandra100% (1)
- Prevention of Surgical Site Infections in Orthopaedic Surgery: A Synthesis of Current RecommendationsDocumento16 páginasPrevention of Surgical Site Infections in Orthopaedic Surgery: A Synthesis of Current RecommendationsPankaj VatsaAinda não há avaliações
- Recent Advances in Wrist & Tendon Surgery: VenueDocumento1 páginaRecent Advances in Wrist & Tendon Surgery: VenuePankaj VatsaAinda não há avaliações
- 1st Circular - DR Steve Rocha Course 2019Documento6 páginas1st Circular - DR Steve Rocha Course 2019Pankaj VatsaAinda não há avaliações
- Cold Orthopaedic Cases PDFDocumento1.039 páginasCold Orthopaedic Cases PDFPankaj VatsaAinda não há avaliações
- Electronic Reservation Slip IRCTC E-Ticketing Service: (Personal User) (Agent)Documento2 páginasElectronic Reservation Slip IRCTC E-Ticketing Service: (Personal User) (Agent)A SURAinda não há avaliações
- Recent Advances in Wrist & Tendon Surgery: VenueDocumento1 páginaRecent Advances in Wrist & Tendon Surgery: VenuePankaj VatsaAinda não há avaliações
- Paper I - A&b - PDFDocumento2 páginasPaper I - A&b - PDFPankaj VatsaAinda não há avaliações
- Arthroscopy Course 1219 FlierDocumento1 páginaArthroscopy Course 1219 FlierPankaj VatsaAinda não há avaliações
- ASSH Manual of Hand Surgery PDFDocumento653 páginasASSH Manual of Hand Surgery PDFChis Alexandra100% (1)
- Orthopedics P - I June15 PDFDocumento2 páginasOrthopedics P - I June15 PDFPankaj VatsaAinda não há avaliações
- Paper Iv - A&b - PDFDocumento2 páginasPaper Iv - A&b - PDFPankaj VatsaAinda não há avaliações
- 2 International Conference & Cadaveric Workshop On Pelviacetabular Fracture and Hip ArthrosDocumento2 páginas2 International Conference & Cadaveric Workshop On Pelviacetabular Fracture and Hip ArthrosPankaj VatsaAinda não há avaliações
- Brochure For AIOC Training JanuaryDocumento4 páginasBrochure For AIOC Training JanuaryPankaj VatsaAinda não há avaliações
- Aaos Trauma DateDocumento110 páginasAaos Trauma DatePankaj VatsaAinda não há avaliações
- Final exam questions on obstetrics and gynaecologyDocumento1 páginaFinal exam questions on obstetrics and gynaecologySlashy HeugotAinda não há avaliações
- Ortho P-Iv B PDFDocumento1 páginaOrtho P-Iv B PDFPankaj VatsaAinda não há avaliações
- Orthopedics P - Iv June15 PDFDocumento2 páginasOrthopedics P - Iv June15 PDFPankaj VatsaAinda não há avaliações
- Ortho P-Iv B PDFDocumento1 páginaOrtho P-Iv B PDFPankaj VatsaAinda não há avaliações
- Fa14 Concept Map 10-26-14 2Documento2 páginasFa14 Concept Map 10-26-14 2api-270415831Ainda não há avaliações
- Medical DeviceDocumento8 páginasMedical DeviceHarshvardhan ChoudharyAinda não há avaliações
- History of Medicine in India from Ancient Times to Ayurvedic Golden AgeDocumento6 páginasHistory of Medicine in India from Ancient Times to Ayurvedic Golden AgeGhulam AbbasAinda não há avaliações
- Makalah Bahasa InggrisDocumento2 páginasMakalah Bahasa InggrisOlga RevalinaAinda não há avaliações
- A Review On Acacia Arabica - An Indian Medicinal Plant: IJPSR (2012), Vol. 3, Issue 07 (Review Article)Documento11 páginasA Review On Acacia Arabica - An Indian Medicinal Plant: IJPSR (2012), Vol. 3, Issue 07 (Review Article)amit chavanAinda não há avaliações
- Lawsuit Against Small Smiles Dental Center Aka Alabany Access Dental Center Et. Al.Documento52 páginasLawsuit Against Small Smiles Dental Center Aka Alabany Access Dental Center Et. Al.DebHgnAinda não há avaliações
- What Type of Resistance Training Program Can Help Increase Muscle MassDocumento75 páginasWhat Type of Resistance Training Program Can Help Increase Muscle Massyokimura dimaunahanAinda não há avaliações
- Complex Regional Pain Syndrome in Adults - Second Edition - 0 PDFDocumento97 páginasComplex Regional Pain Syndrome in Adults - Second Edition - 0 PDFLotteDomineAinda não há avaliações
- Sound Transduction EarDocumento7 páginasSound Transduction Earhsc5013100% (1)
- Portfolio Template for Diploma in Occupational MedicineDocumento11 páginasPortfolio Template for Diploma in Occupational MedicineChengyuan ZhangAinda não há avaliações
- Physician Assistant Certification and Recertification Exam Review - PANRE - PANCEDocumento14 páginasPhysician Assistant Certification and Recertification Exam Review - PANRE - PANCEThe Physician Assistant Life100% (3)
- Hydralazine For Severe PIHDocumento4 páginasHydralazine For Severe PIHYwagar YwagarAinda não há avaliações
- Cardiovascular Physiology Case 9Documento50 páginasCardiovascular Physiology Case 9Kim AcostaAinda não há avaliações
- Pathology - List - 89.8.20Documento25 páginasPathology - List - 89.8.20Mamula RiazAinda não há avaliações
- Daftar Obat Slow Moving Dan Ed Rawat Inap Maret 2021Documento8 páginasDaftar Obat Slow Moving Dan Ed Rawat Inap Maret 2021Vima LadipaAinda não há avaliações
- YOU IN SURGICAL - Product CatalogDocumento222 páginasYOU IN SURGICAL - Product CatalogfarazAinda não há avaliações
- Minor Surgical Procedures in Maxillofacial SurgeryDocumento65 páginasMinor Surgical Procedures in Maxillofacial SurgerydrzibranAinda não há avaliações
- RAV Admission Notice for Ayurveda CoursesDocumento4 páginasRAV Admission Notice for Ayurveda CoursesBhargav KalalAinda não há avaliações
- Clinical Examination and Management of Impairments in VariousDocumento34 páginasClinical Examination and Management of Impairments in Variousmukesh pokharelAinda não há avaliações
- Navidas-Case StudyDocumento5 páginasNavidas-Case StudyFran LanAinda não há avaliações
- Pasteurized EggsDocumento8 páginasPasteurized Eggsapi-202950260Ainda não há avaliações
- District Sales Manager in Los Angeles CA Resume Ronald FoxDocumento2 páginasDistrict Sales Manager in Los Angeles CA Resume Ronald FoxRonaldFoxAinda não há avaliações
- List of Doctors by SpecialtyDocumento6 páginasList of Doctors by Specialtykaushal shahAinda não há avaliações
- Strategic PlanDocumento84 páginasStrategic PlanAurutchat VichaiditAinda não há avaliações
- Implants Session I Revised 21 Sept 2012Documento17 páginasImplants Session I Revised 21 Sept 2012Norman AjxAinda não há avaliações
- Hospital Floor Plan Checklist ReviewDocumento5 páginasHospital Floor Plan Checklist Reviewjherica baltazarAinda não há avaliações
- Resume Jurnal-Dessy Dwi H 201720401011160Documento3 páginasResume Jurnal-Dessy Dwi H 201720401011160Pratiwi UmbohAinda não há avaliações
- Elphos Erald: Second Shot: Hillary Clinton Running Again For PresidentDocumento10 páginasElphos Erald: Second Shot: Hillary Clinton Running Again For PresidentThe Delphos HeraldAinda não há avaliações
- Introduction to Radiographic Imaging InterpretationDocumento17 páginasIntroduction to Radiographic Imaging Interpretationpradep4u21Ainda não há avaliações