Escolar Documentos
Profissional Documentos
Cultura Documentos
Silva 2013
Enviado por
EviDireitos autorais
Formatos disponíveis
Compartilhar este documento
Compartilhar ou incorporar documento
Você considera este documento útil?
Este conteúdo é inapropriado?
Denunciar este documentoDireitos autorais:
Formatos disponíveis
Silva 2013
Enviado por
EviDireitos autorais:
Formatos disponíveis
CHEST Original Research
CRITICAL CARE
Usefulness of Cardiothoracic Chest
Ultrasound in the Management of Acute
Respiratory Failure in Critical Care Practice
Stein Silva, MD, PhD; Caroline Biendel, MD; Jean Ruiz, MD; Michel Olivier, MD;
Benoit Bataille, MD; Thomas Geeraerts, MD, PhD; Arnaud Mari, MD;
Beatrice Riu, MD; Olivier Fourcade, MD, PhD; and Michele Genestal, MD
Background: This study investigated the clinical relevance of early general chest ultrasonography
(ie, heart and lung recordings) in patients in the ICU with acute respiratory failure (ARF).
Methods: We prospectively compared this diagnostic approach (ultrasound) to a routine evaluation
established from clinical, radiologic, and biologic data (standard). Subjects were patients consec-
utively admitted to the ICU of a university teaching hospital during a 1-year period. Inclusion
criteria were age ⱖ 18 years and the presence of severe ARF criteria to justify ICU admission. We
compared the diagnostic approaches and the final diagnosis determined by a panel of experts.
Results: Seventy-eight patients were included (age, 70 ⫾ 18 years; sex ratio, 1). Three patients
given two or more simultaneous diagnoses were subsequently excluded. The ultrasound approach
was more accurate than the standard approach (83% vs 63%, respectively; P , .02). Receiver oper-
ating characteristic curve analysis showed greater diagnostic performance of ultrasound in cases
of pneumonia (standard, 0.74 ⫾ 0.12; ultrasound, 0.87 ⫾ 0.14; P , .02), acute hemodynamic pul-
monary edema (standard, 0.79 ⫾ 0.11; ultrasound, 0.93 ⫾ 0.08; P , .007), decompensated COPD
(standard, 0.8 ⫾ 0.09; ultrasound, 0.92 ⫾ 0.15; P , .05), and pulmonary embolism (standard, 0.65 ⫾ 0.12;
ultrasound, 0.81 ⫾ 0.17; P , .04). Furthermore, we found that the use of ultrasound data could
have significantly improved the initial treatment.
Conclusions: The use of cardiothoracic ultrasound appears to be an attractive complementary
diagnostic tool and seems able to contribute to an early therapeutic decision based on reproducible
physiopathologic data. CHEST 2013; 144(3):859–865
Abbreviations: ARF 5 acute respiratory failure
A cute respiratory failure (ARF) is frequently encoun-
tered in ICUs. ARF cases do not always present
1,2
ence requirements for assessing heart and lung status
in this context, but the flaws of these familiar tools are
in conditions that are ideal for early diagnosis, which becoming increasingly acknowledged. The low accu-
sometimes compromises outcomes.3,4 Nevertheless, racy of clinical evaluations in the critical care context
immediate diagnosis and suitable treatment seem to has been highlighted frequently.7,8 Additionally, chest
improve prognosis.5,6 Traditionally, a physical exami- radiography has several technical requirements that
nation and bedside radiography are considered refer- ensure the quality of images obtained, and these cannot
be easily met in the critical care environment.9,10 Con-
Manuscript received January 22, 2013; revision accepted April 15, sequently, a need for sophisticated tests arises, which
2013.
Affiliations: From the Réanimation Polyvalente et Médecine
may delay management.11
Hyperbare (Drs Silva, Ruiz, Olivier, Mari, Riu, and Genestal) and
Pôle Anesthésie-Réanimation (Drs Silva, Ruiz, Olivier, Bataille,
Geeraerts, Mari, Riu, Fourcade, and Genestal), CHU Purpan; Pôle Correspondence to: Stein Silva, MD, PhD, Critical Care Unit,
Cardiovasculaire et Métabolique (Dr Biendel), CHU Rangueil; and CHU Purpan, 31059 Toulouse Cedex 3, France; e-mail: silvastein@
Equipe d’Accueil (Drs Silva, Geeraerts, and Fourcade), MATN, me.com; silva.s@chu-toulouse.fr
IFR 150, Université Paul Sabatier, Toulouse, France. © 2013 American College of Chest Physicians. Reproduction
Funding/Support: This research was supported by institutional of this article is prohibited without written permission from the
departmental funds from Centre Hospitalier Universitaire de American College of Chest Physicians. See online for more details.
Toulouse, Toulouse, France. DOI: 10.1378/chest.13-0167
journal.publications.chestnet.org CHEST / 144 / 3 / SEPTEMBER 2013 859
Downloaded From: http://journal.publications.chestnet.org/ by David Kinnison on 09/03/2013
Cardiac and lung ultrasonography have been inde- Cardiothoracic Ultrasound: All patients underwent a cardio-
pendently proposed as useful approaches to patients thoracic ultrasound test by investigators who did not participate in
the patient’s management (S. S., B. R.). The ultrasound test was
with acute illness, guiding management and care.12,13 performed without interrupting management at the time of ICU
For example, the accuracy of lung ultrasound has been admission (ie, within 20 ⫾ 6 min) and lasted 12 ⫾ 4 min. Investiga-
established for the diagnoses of pneumothorax,14 lung tors used standardized criteria (Table 1) and followed a strict pattern
consolidation,15 alveolar-interstitial syndrome,16 and analysis. Data were recorded for further interobserver variability
pleural effusion.17 In parallel, several studies have dem- assessment and then discussed to obtain an ultrasound diagnosis
based on consensus of the two scanners. Transthoracic echocardi-
onstrated that cardiac ultrasound can provide accu- ography and lung ultrasound assessment were performed with an
rate information with diagnostic relevance in patients HP Sonos 5500 (Hewlett-Packard Development Company, LP)
in the ICU. For example, echocardiography may accu- and 2- to 4-MHz probes. All patients were studied in the semire-
rately distinguish ARF caused by left-sided heart dys- cumbent position.
function from that resulting from noncardiac causes.12,18 The echocardiographic examination included left ventricular
systolic function (visual estimation of the left ventricular ejection
The aim of the current study was to prospectively fraction at , 30%, 30%-50%, and . 50%),23 left ventricular end-
investigate the clinical relevance of early general chest diastolic pressure estimation (pulsed Doppler echocardiography-
ultrasonography (ie, heart and lung recordings) in recorded mitral inflow and Doppler tissue imaging with the sample
patients with ARF in the ICU. We used the routine cursor placed in the lateral mitral annulus to record the following:
evaluation of clinical, radiologic, and biologic data as E-wave velocity, A-wave velocity, Ea velocity, and E/A and E/Ea
ratios),24 right ventricular function (assessment of the interven-
the standard diagnostic approach against which to test tricular septal configuration and dynamic M-mode measurement
an original integrative ultrasound procedure. The of the inferior vena cava diameter, including paradoxical septal
hypothesis was that a significant improvement would motion, right ventricular dilatation, and central venous pressure
be seen in the diagnostic accuracy of this paraclinical estimation),25 and pericardial evaluation (detection of pericardial
tool when both lung and cardiac ultrasonographic data effusion as either present or absent).12 For the lung ultrasound
examination, the anterior chest wall was delineated from the clav-
are analyzed together. Finally, we evaluated the extent icles to the diaphragm and from the sternum to the anterior axil-
to which this cardiothoracic ultrasonographic approach lary line. The lateral chest was delineated from the axillary zone to
could improve therapeutic decision-making during the the diaphragm and from the anterior to the posterior axillary line.
early management of critically ill patients with ARF. The anterior and lateral chest walls were divided into three lung
regions. Lung ultrasonograms were contemporaneously classified
in a few categories according to previously described criteria.17
Materials and Methods The pleural line was defined as a horizontal hyperechoic line vis-
ible 0.5 cm below the rib line. A normal pattern was defined as
the presence, in every lung region, of lung sliding with A lines
Patients
(A profile).26 Pleural effusion was defined as a dependent collec-
We prospectively recruited patients consecutively admitted tion limited by the diaphragm and the pleura with an inspiratory
for ARF to the ICU of a university teaching hospital between movement of the visceral pleura from depth to superficial.27 With
September 2010 and September 2011. Inclusion criteria were the use of TM mode, pneumothorax was defined by the loss of
age ⱖ 18 years and the presence of one of the following objec- pleural sliding (A9 profile).28 Alveolar consolidation was defined as
tive criteria of ARF: a respiratory rate of at least 25/min, a Pao2 the presence of poorly defined, wedge-shaped hypoechoic tissue
of ⱕ 60 mm Hg, an oxygen saturation as measured by pulse oxim- structures (C profile).29 Within the consolidation, hyperechoic punc-
etry of ⱕ 90% while breathing room air, and a Paco2 of ⱖ 45 mm Hg tiform images can be seen that correspond to air-filled bronchi (ie,
with an arterial pH ⱕ 7.35. The ethics committee of the University bronchograms).15 Pleural effusion can also be associated with the
Hospital of Toulouse, France (Comite Consultatif pour la Protec- patterns of alveolar consolidation (ie, posterolateral alveolar con-
tion des Personnes, CHU Toulouse, France; Ref 2010-A01225-48), solidation and/or pleural effusion syndrome).19 Alveolar-interstitial
approved the therapeutic and investigational procedures and waived syndrome was defined as the presence of more than two B lines in
the requirement for written informed consent. To simplify this a given lung region (B profile).30 Each of the 12 lung regions exam-
study, patients given several final diagnoses were subsequently ined per patient was classified in one or more of these profiles and
excluded.19
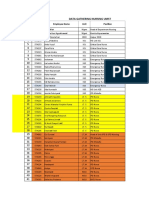
Experimental Design Table 1—Ultrasound Profiles Used in the Bedside
General Chest Ultrasound Evaluation
Routine Clinical Assessment: For every patient, standard medical
care provided by the senior ICU physician in charge (A. M., J. R.) Condition Lung Heart
included the following: medical history; physical examination find-
Pulmonary embolism A profile with DVT RV failure (acute)
ings, including signs of ARF (use of accessory respiratory muscles,
Acute hemodynamic B profile High end-diastolic
paradoxical abdominal respiration); arterial blood gas analysis while
pulmonary edema LV pressure
breathing room air; 12-lead ECG; chest radiograph; and routine
Decompensated COPD A profile RV failure (chronic)
blood tests, including plasma levels of cardiac troponin I and B-type
Pneumothorax A9 profile Nonspecific
natriuretic peptide. Experts were blinded to the ultrasound results.
Pneumonia C profile Nonspecific
As usual, after the initial presentation in the ICU, all patients were
A profile plus PLAPS
reviewed by a second senior staff member (M. O.). Thus, depend-
A/B profile
ing on the suspected diagnosis, initial treatment was decided by
these members of the medical staff in accordance with normal LV 5 left ventricular; PLAPS 5 posterolateral alveolar and/or pleural
practice and recommendations.20,21 syndrome22; RV 5 right ventricular.
860 Original Research
Downloaded From: http://journal.publications.chestnet.org/ by David Kinnison on 09/03/2013
associated with cardiac ultrasonographic data to establish a diag- Results
nosis (Table 1). Finally, a simplified DVT study was performed on
all patients with the same probe.19
Patients
Seventy-eight patients with ARF admitted to the
Final Diagnosis: The final diagnosis of ARF was determined
by two independent senior experts (T. G, O. F.) from an exami- ICU were prospectively included in the study. The
nation of the complete medical chart, including all initial clinical mean age of the patients was 70 ⫾ 18 years, and the sex
findings; emergency laboratory tests, including plasma levels of ratio was 1. At inclusion in the study, patients had a
cardiac troponin I and B-type natriuretic peptide; chest radiograph mean Pao2 of 58 ⫾ 19 mm Hg (spontaneous ventilation
data; and the results of thoracic high-resolution CT scans (per-
and Fio2 of 0.21), and mean Paco2 was 44 ⫾ 9 mm Hg.
formed in 75% of the patients). Additionally, transthoracic Dopp-
ler echocardiography was performed in 68% of the patients by a Within the first 8 h of initial treatment, 26 patients
senior cardiologist (C. B.) who was blinded to the ultrasound data (34.6%) were intubated, and 34 patients (45.3%) were
to allow an independent comparison between the different diag- treated with noninvasive mechanical ventilation. The
nostic methods. In a few cases (5% of the patients), a pulmonary mortality rate was 18%. The final diagnoses established
function test (peak expiratory flow or bedside spirometry) was con-
by the panel of experts were pneumonia (n 5 33), acute
ducted to assess the severity of a suspected airflow obstruction in
accordance with current recommendations.31 In case of disagree- hemodynamic pulmonary edema (n 5 19), decompen-
ment between the two experts, a consensus was reached with the sated COPD (n 5 12), pulmonary embolism (n 5 8),
help of a third expert (M. G.). The main diagnoses finally proposed and pneumothorax (n 5 3). It must be highlighted that
were cardiogenic pulmonary edema, including left-sided heart CT scan was used as the reference criterion to con-
failure; community-acquired pneumonia; acute exacerbation of
firm a suspected pneumothorax. In the absence of a
chronic respiratory disease; acute asthma; pulmonary embolism;
and pneumothorax. Validated criteria were used (ie, response to clinical and standard chest radiographic sign of com-
diuretic or vasodilator, results of cardiac troponin I32 and B-type pressive pneumothorax, CT scan and thoracic ultra-
natriuretic peptide tests performed at admission to the ED), and sonography were performed before pleural exsufflation
other cardiac tests were specifically analyzed for cardiogenic pul- in all three cases. All the pneumothoraces identified
monary edema.33 Response to bronchodilators, steroids, or anti-
by the gold standard procedure were also diagnosed
biotics; results from the pulmonary function test; and thoracic
high-resolution CT scans were analyzed specifically for respiratory with use of the ultrasound approach. Three patients
disorders.34 Results of echocardiography and a contrast-enhanced had several final diagnoses. To simplify the analysis,
helical CT scan were analyzed specifically for pulmonary embolism,35 these patients were subsequently excluded.
as recommended.
Initial Treatment: The initial treatment of ARF was decided Comparative Diagnostic Accuracy
by two physicians on the ICU staff (A. M., J. R., M. O.) and was
established from the standard data. It must be pointed out that With respect to the final diagnosis, the ultrasound
an inaccurate initial treatment was recorded when (1) pulmonary diagnostic approach was more accurate than the stan-
embolism was diagnosed by the experts (ie, final diagnosis) with- dard approach (83% vs 63%, respectively, P , .02)
out initial anticoagulation, (2) cardiogenic pulmonary edema was (Fig 1). Furthermore, receiver operating characteris-
diagnosed without initial administration of vasodilators or diuretics, tic analysis showed a significantly greater area under
(3) community-acquired pneumonia was diagnosed without initial
antibiotics, (4) asthma was diagnosed without initial b2-agonist the curves when the diagnosis was made with the
administration, and (5) pneumothorax/pleural effusion was diag- ultrasound rather than with the standard approach
nosed without initial thoracentesis. (Fig 2) in cases of pneumonia (standard, 0.74 ⫾ 0.12;
ultrasound, 0.87 ⫾ 0.14; P , .02), acute hemodynamic
Statistical Analysis
pulmonary edema (standard, 0.79 ⫾ 0.11; ultrasound,
Continuous data are expressed as mean ⫾ SD and categorical 0.93 ⫾ 0.08; P , .007), decompensated COPD (stan-
variables as numbers and percentages. McNemar test was used to dard, 0.8 ⫾ 0.09; ultrasound, 0.92 ⫾ 0.15; P , .05), and
compare the diagnostic approaches (standard vs ultrasound) and
the final diagnosis determined by the panel of experts. Two means
pulmonary embolism (standard, 0.65 ⫾ 0.12; ultra-
were compared with a Student test and two proportions with Fisher sound, 0.81 ⫾ 0.17; P , .04).
exact method. The diagnostic performance of each approach was
assessed by calculating the sensitivity, specificity, and diagnostic Interobserver Variability
accuracy with standard formulas.36 A receiver operating charac-
teristic curve depicting the relationship between the proportion For the 900 lung regions analyzed by two indepen-
of true-positive findings and the proportion of false-positive find- dent investigators, k values for assessing normal lung
ings was drawn.37 The level of agreement among observers for the
ultrasound finding was evaluated by means of the 900 lung regions ultrasonography pattern (Table 1), B profile, A profile,
analyzed (12 per patient) and the 300 echocardiographic data an- A profile with DVT, A9 profile, C profile, and A pro-
alyzed (four criteria per patient) with the k reliability test38; file plus posterolateral alveolar and/or pleural syndrome
k values , 0.40 indicated low agreement, values between 0.40 and were 0.81, 0.78, 0.69, 0.78, 0.72, 0.79, and 0.88 respec-
0.75 indicated medium agreement, and values . 0.75 indicated tively. For the 300 echocardiography data, k values for
high agreement between the two raters. All statistical tests were
two-sided, and P , .05 was required to reject the null hypothesis. assessing normal cardiac patterns, left ventricular sys-
Statistical analysis was performed with Statistica 7.0 (StatSoft, Inc) tolic failure, left ventricular diastolic failure, right ven-
software. tricular failure, and the presence of pericardial effusion
journal.publications.chestnet.org CHEST / 144 / 3 / SEPTEMBER 2013 861
Downloaded From: http://journal.publications.chestnet.org/ by David Kinnison on 09/03/2013
Potential Therapeutic Improvement
The accuracy of the initial treatment, established
with use of the standard approach, was compared with
the therapeutic decisions that could have been made
from the ultrasound data. The use of general ultra-
sound chest data, already available at the time of the
first therapeutic decisions, could have significantly
improved the initial treatment (Fig 3) in cases of pneu-
monia (P , .05), acute hemodynamic pulmonary edema
(P , .04), decompensated COPD (P , .009), and pul-
monary embolism (P , .05).
Figure 1. Comparative diagnostic accuracy. Each diagnostic
approach (standard and ultrasound) was compared against the
final diagnosis determined by a panel of experts (*P , .05). Discussion
Lung and heart ultrasound generates standardized
were 0.82, 0.77, 0.82, 0.69, and 0.77, respectively. patterns, which have been independently proposed to
Finally, when the 200 echocardiographic data pro- help bedside diagnosis in patients admitted to the ICU.
vided by a senior cardiologist (C. B.) were compared Previous studies have focused on assessing the sensi-
with that obtained by intensivists, k values for assess- tivity and specificity of these profiles, comparing ultra-
ing normal cardiac patterns, left ventricular systolic sonography data to gold standard methods, such as
failure, left ventricular diastolic failure, right ventric- thoracic CT scan39 or pulmonary artery catheter.40 To
ular failure, and the presence of pericardial effusion our knowledge, this study is the first to evaluate the
were 0.88, 0.81, 0.82, 0.72, and 0.79, respectively, for diagnostic value and potential therapeutic impact of
to the first investigator (B. R.) and 0.79, 0.88, 0.79, 0.80, an approach that combines lung and heart ultrasound
and 0.81, respectively, for the second (S.S.). scans in the early management of critically ill patients
Figure 2. A-D, Receiver operating characteristic curves depicting the relationship between the proportion of true-positive findings and
the proportion of false-positive findings. The standard and ultrasound approaches are represented for each diagnosis as follows: hemody-
namic pulmonary edema (A), pneumonia (B), decompensated COPD (C), and pulmonary embolism (D).
862 Original Research
Downloaded From: http://journal.publications.chestnet.org/ by David Kinnison on 09/03/2013
for both heart and lung ultrasounds. This important
point might be related to the fact that general chest
ultrasound generates standardized and reproducible
patterns, even in the ICU environment. For example,
despite the difficult acquisition conditions, an accept-
able cardiac Doppler echocardiography examination
was possible in all cases. We believe that the data we
obtained had a significant added value and contributed
to accurately disambiguating ARF caused by left-sided
heart dysfunction from that resulting from noncar-
diac causes.40,44
Figure 3. Potential therapeutic improvement related to the use In agreement with previous studies,11,39 we observed
of the ultrasound approach. The accuracy of the initial treatment, a high concordance between chest ultrasonography
established with standard data, was compared with the therapeutic and CT scan data. We speculate that in the present
decisions that could have been made with the ultrasound approach.
The use of general ultrasound chest data could have significantly cohort, where 75% of patients underwent thoracic
improved the initial treatment in cases of pneumonia (P , .05), CT scanning, these tests could have been avoided by
acute HPE (P , .04), decompensated COPD (P , .009), and pul- thoughtful use of ultrasound in more than one-half of
monary embolism (P , .05). *P , .05. HPE 5 hemodynamic pul-
monary edema. the cases. Future studies are needed to assess the
time savings and cost-effectiveness of combined car-
with ARF. The main result was a significant improve- diothoracic ultrasonography compared with CT scan
ment in the initial diagnostic accuracy with general in this context.
chest ultrasound compared with a standard approach This study has several limitations. First, the inten-
that encompassed clinical, radiologic, and biologic data. sivists who performed the ultrasonography could not
Furthermore, greater diagnostic ability of the ultra- be blinded to obvious clues of diagnosis that might be
sound approach was identified when each main etio- readily apparent to an experienced observer while per-
logic entity was analyzed independently. forming an ultrasound examination. Second, in a few
It must be highlighted that we observed similar levels cases, the echocardiography performed by the senior
of sensitivity and specificity to those described in pre- cardiologist was probably recorded past the initial man-
vious studies that used lung ultrasonography alone.19,27,39 agement of the patient, so it had limited value in deter-
We believe that combining echocardiography with mining the diagnosis at the time of presentation. For
lung ultrasonography in this context probably does the purposes of this study, a general chest ultrasound
not improve the diagnostic value of lung ultrasound team was set up and comprised two noncardiologist
alone but could have fundamental importance in ther- intensivists (B. R., S. S.) with advanced-level training
apeutic decisions. Actually, the present data suggest and competence in lung, pleural, and cardiac ultraso-
that general chest ultrasonography provide accurate nography according to La Société de Réanimation
online assessment of lung and heart status and dynamic de Langue Française and American College of Chest
interactions, which are specifically disrupted in path- Physicians criteria.45 These investigators followed a
ologic states. For example, it has been shown that the training tailored to critical care practice (2 years) and
diagnosis of acute pulmonary edema is accurate with have . 3 years of experience in using and teaching
lung ultrasound (sensitivity near 100%),27 but with ultrasonography in their daily practice. In the pre-
heart ultrasound, we can obtain crucial information sent work, we concentrated on comparing a standard
about the etiology and underlying mechanism (acute approach and an independent general chest ultrasound
lung injury vs cardiogenic edema). Further investiga- analysis because we wanted to assess the diagnostic
tions are needed to evaluate the impact of such inte- and therapeutic impact of this novel procedure against
grative ultrasound procedures for the correct initial a gold standard approach. Finally, patients who were
treatment of ARF in this context.41-43 Furthermore, given several final diagnoses were subsequently excluded
we describe how the use of general chest ultrasonog- from this study. Future studies will need to focus on
raphy, easily performed at the patient’s bedside, could evaluating the utility of combining standard and ultra-
have improved initial treatment in cases of pneumonia, sound data to obtain better diagnostic accuracy, par-
decompensated COPD, and pulmonary embolism. ticularly when several simultaneous causes contribute
Altogether, these results confirm the present hypo- to the ARF.
thesis of a direct diagnostic and potential therapeutic
impact when general chest ultrasonography is used in Conclusions
critically ill patients with ARF.
It is worth noting that we observed highly satisfac- Cardiothoracic ultrasonography appears to be an
tory interobserver agreement in the experts’ findings attractive complementary diagnostic tool and one of
journal.publications.chestnet.org CHEST / 144 / 3 / SEPTEMBER 2013 863
Downloaded From: http://journal.publications.chestnet.org/ by David Kinnison on 09/03/2013
the most promising techniques for the management 3. Linko R, Okkonen M, Pettilä V, et al; FINNALI-study group.
of critically ill patients with ARF. Ultrasound is non- Acute respiratory failure in intensive care units. FINNALI:
a prospective cohort study. Intensive Care Med. 2009;35(8):
invasive, easily repeatable at the bedside, and provides 1352-1361.
an accurate online assessment of lung and heart status 4. Luhr OR, Antonsen K, Karlsson M, et al; The ARF Study Group.
and dynamic interactions, which are specifically dis- Incidence and mortality after acute respiratory failure and
rupted in pathologic states. Furthermore, this new tool acute respiratory distress syndrome in Sweden, Denmark, and
seems to contribute to an early ICU therapeutic deci- Iceland. Am J Respir Crit Care Med. 1999;159(6):1849-1861.
5. Afessa B, Morales IJ, Scanlon PD, Peters SG. Prognostic fac-
sion based on more accurate and reproducible data. tors, clinical course, and hospital outcome of patients with
Benefits to be evaluated in future studies include a chronic obstructive pulmonary disease admitted to an inten-
reduced need for CT scans and, thus, shorter delays; sive care unit for acute respiratory failure. Crit Care Med.
lower irradiation levels and cost; and above all, improved 2002;30(7):1610-1615.
prognosis for the patient. 6. Zahar JR, Azoulay E, Klement E, et al. Delayed treatment
contributes to mortality in ICU patients with severe active pul-
monary tuberculosis and acute respiratory failure. Intensive
Acknowledgments Care Med. 2001;27(3):513-520.
Author contributions: Dr Silva had full access to all of the data 7. Metlay JP, Schulz R, Li YH, et al. Influence of age on symp-
in the study and takes responsibility for the integrity of the data toms at presentation in patients with community-acquired
and the accuracy of the data analysis. pneumonia. Arch Intern Med. 1997;157(13):1453-1459.
Dr Silva: contributed to the study design; data acquisition, analysis, 8. Nielsen LS, Svanegaard J, Wiggers P, Egeblad H. The yield
and interpretation; critical revision of the manuscript for impor- of a diagnostic hospital dyspnoea clinic for the primary health
tant intellectual content; and approval of the final version of the care section. J Intern Med. 2001;250(5):422-428.
manuscript. 9. Greenbaum DM, Marschall KE. The value of routine daily
Dr Biendel: contributed to the data acquisition, critical revision of
the manuscript for important intellectual content, and approval of chest x-rays in intubated patients in the medical intensive
the final version of the manuscript. care unit. Crit Care Med. 1982;10(1):29-30.
Dr Ruiz: contributed to the study design, data acquisition, critical 10. Janower ML, Jennas-Nocera Z, Mukai J. Utility and efficacy
revision of the manuscript for important intellectual content, and of portable chest radiographs. AJR Am J Roentgenol. 1984;
approval of the final version of the manuscript. 142(2):265-267.
Dr Olivier: contributed to the data acquisition, critical revision of 11. Zanobetti M, Poggioni C, Pini R. Can chest ultrasonography
the manuscript for important intellectual content, and approval of replace standard chest radiography for evaluation of acute
the final version of the manuscript. dyspnea in the ED? Chest. 2011;139(5):1140-1147.
Dr Bataille: contributed to the study conception, data analysis, 12. Beaulieu Y. Bedside echocardiography in the assessment of
critical revision of the manuscript for important intellectual con-
tent, and approval of the final version of the manuscript. the critically ill. Crit Care Med. 2007;35(5):S235-S249.
Dr Geeraerts: contributed to the data acquisition, critical revision 13. Volpicelli G, Elbarbary M, Blaivas M, et al; International
of the manuscript for important intellectual content, and approval Liaison Committee on Lung Ultrasound (ILC-LUS) for Inter-
of the final version of the manuscript. national Consensus Conference on Lung Ultrasound (ICC-
Dr Mari: contributed to the data acquisition, critical revision of LUS). International evidence-based recommendations for
the manuscript for important intellectual content, and approval of point-of-care lung ultrasound. Intensive Care Med. 2012;
the final version of the manuscript. 38(4):577-591.
Dr Riu: contributed to the study design, data acquisition, critical 14. Lichtenstein DA, Mezière G, Lascols N, et al. Ultrasound
revision of the manuscript for important intellectual content, and diagnosis of occult pneumothorax. Crit Care Med. 2005;33(6):
approval of the final version of the manuscript.
Dr Fourcade: contributed to the data acquisition, critical revision 1231-1238.
of the manuscript for important intellectual content, and approval 15. Lichtenstein D, Mezière G, Seitz J. The dynamic air bron-
of the final version of the manuscript. chogram. A lung ultrasound sign of alveolar consolidation
Dr Genestal: contributed to the data acquisition, critical revision ruling out atelectasis. Chest. 2009;135(6):1421-1425.
of the manuscript for important intellectual content, and approval 16. Lichtenstein D, Mézière G, Biderman P, Gepner A, Barré
of the final version of the manuscript. O. The comet-tail artifact. An ultrasound sign of alveolar-
Financial/nonfinancial disclosures: The authors have reported interstitial syndrome. Am J Respir Crit Care Med. 1997;156(5):
to CHEST that no potential conflicts of interest exist with any 1640-1646.
companies/organizations whose products or services may be dis- 17. Bouhemad B, Zhang M, Lu Q, Rouby JJ. Clinical review:
cussed in this article.
Role of sponsors: The sponsor had no role in the design of the bedside lung ultrasound in critical care practice. Crit Care.
study, the collection and analysis of the data, or the preparation of 2007;11(1):205.
the manuscript. 18. Soldati G, Gargani L, Silva FR. Acute heart failure: new
Other contributions: The authors thank Marie Dao, MD; Elodie diagnostic perspectives for the emergency physician. Intern
Brunel, MD; and Andree Villaceque, MD, for their help in col- Emerg Med. 2008;3(1):37-41.
lecting data. 19. Lichtenstein D. Lung ultrasound in acute respiratory failure
an introduction to the BLUE-protocol. Minerva Anestesiol.
2009;75(5):313-317.
References 20. Organized jointly by the American Thoracic Society, the
1. Levitt JE, Bedi H, Calfee CS, Gould MK, Matthay MA. European Respiratory Society, the European Society of Inten-
Identification of early acute lung injury at initial evaluation in sive Care Medicine, and the Société de Réanimation de
an acute care setting prior to the onset of respiratory failure. Langue Française, and approved by ATS Board of Directors,
Chest. 2009;135(4):936-943. December 2000. International Consensus Conferences in
2. Vincent JL, Akça S, De Mendonça A, et al; SOFA Working Intensive Care Medicine: noninvasive positive pressure ven-
Group. The epidemiology of acute respiratory failure in criti- tilation in acute Respiratory failure. Am J Respir Crit Care
cally ill patients. Chest. 2002;121(5):1602-1609. Med. 2001;163(1):283-291.
864 Original Research
Downloaded From: http://journal.publications.chestnet.org/ by David Kinnison on 09/03/2013
21. O’Donohue WJ Jr, Baker JP, Bell GM, Muren O, Patterson JL Jr. Global Survey of Standard Treatment (ALARM-HF). Intensive
The management of acute respiratory failure in a respiratory Care Med. 2011;37(4):619-626.
intensive care unit. Chest. 1970;58(6):603-610. 34. Quon BS, Gan WQ, Sin DD. Contemporary management
22. Lichtenstein DA, Lascols N, Mezière G, Gepner A. Ultrasound of acute exacerbations of COPD: a systematic review and
diagnosis of alveolar consolidation in the critically ill. Intensive metaanalysis. Chest. 2008;133(3):756-766.
Care Med. 2004;30(2):276-281. 35. Torbicki A. Acute and long term management of pulmonary
23. Gudmundsson P, Rydberg E, Winter R, Willenheimer R. embolism. Heart. 2010;96(17):1418-1424.
Visually estimated left ventricular ejection fraction by echo- 36. Deeks JJ. Systematic reviews in health care: systematic reviews
cardiography is closely correlated with formal quantitative of evaluations of diagnostic and screening tests. BMJ. 2001;
methods. Int J Cardiol. 2005;101(2):209-212. 323(7305):157-162.
24. Boussuges A, Blanc P, Molenat F, Burnet H, Habib G, Sainty JM. 37. Bewick V, Cheek L, Ball J. Statistics review 13: receiver oper-
Evaluation of left ventricular filling pressure by transthoracic ating characteristic curves. Crit Care. 2004;8(6):508-512.
Doppler echocardiography in the intensive care unit. Crit 38. Fleiss J. The measurement of inter-rater agreement. In Statistical
Care Med. 2002;30(2):362-367. Methods for Rates and Proportions. New York, NY: Wiley;
25. Jardin F, Dubourg O, Bourdarias JP. Echocardiographic pat- 1981:212-225.
tern of acute cor pulmonale. Chest. 1997;111(1):209-217. 39. Lichtenstein D, Goldstein I, Mourgeon E, Cluzel P, Grenier P,
26. Lichtenstein DA. Ultrasound in the management of thoracic Rouby JJ. Comparative diagnostic performances of ausculta-
disease. Crit Care Med. 2007;35(5):S250-S261. tion, chest radiography, and lung ultrasonography in acute
27. Lichtenstein DA, Mezière GA. Relevance of lung ultrasound respiratory distress syndrome. Anesthesiology. 2004;100(1):
in the diagnosis of acute respiratory failure: the BLUE proto- 9-15.
col. Chest. 2008;134(1):117-125. 40. Bouhemad B, Ferrari F, Leleu K, Arbelot C, Lu Q, Rouby JJ.
28. Soldati G, Testa A, Sher S, Pignataro G, La Sala M, Silveri NG. Echocardiographic Doppler estimation of pulmonary artery
Occult traumatic pneumothorax: diagnostic accuracy of lung pressure in critically ill patients with severe hypoxemia.
ultrasonography in the emergency department. Chest. 2008; Anesthesiology. 2008;108(1):55-62.
133(1):204-211. 41. Beaulieu Y, Marik PE. Bedside ultrasonography in the ICU:
29. Soldati G, Testa A, Silva FR, Carbone L, Portale G, Silveri NG. part 2. Chest. 2005;128(3):1766-1781.
Chest ultrasonography in lung contusion. Chest. 2006;130(2): 42. Beaulieu Y, Marik PE. Bedside ultrasonography in the ICU:
533-538. part 1. Chest. 2005;128(2):881-895.
30. Soldati G, Copetti R, Sher S. Sonographic interstitial syn- 43. Lichtenstein D, Karakitsos D. Integrating lung ultrasound in
drome: the sound of lung water. J Ultrasound Med. 2009;28(2): the hemodynamic evaluation of acute circulatory failure (the
163-174. fluid administration limited by lung sonography protocol).
31. Silverman RA, Flaster E, Enright PL, Simonson SG. FEV1 J Crit Care. 2012; 27(5):533.e11-533.e19.
performance among patients with acute asthma: results from 44. Vignon P. Hemodynamic assessment of critically ill patients
a multicenter clinical trial. Chest. 2007;131(1):164-171. using echocardiography Doppler. Curr Opin Crit Care. 2005;
32. Salem R, Vallee F, Rusca M, Mebazaa A. Hemodynamic moni- 11(3):227-234.
toring by echocardiography in the ICU: the role of the new 45. Mayo PH, Beaulieu Y, Doelken P, et al. American College
echo techniques. Curr Opin Crit Care. 2008;14(5):561-568. of Chest Physicians/La Société de Réanimation de Langue
33. Follath F, Yilmaz MB, Delgado JF, et al. Clinical presenta- Française statement on competence in critical care ultraso-
tion, management and outcomes in the Acute Heart Failure nography. Chest. 2009;135(4):1050-1060.
journal.publications.chestnet.org CHEST / 144 / 3 / SEPTEMBER 2013 865
Downloaded From: http://journal.publications.chestnet.org/ by David Kinnison on 09/03/2013
Você também pode gostar
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryNo EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryNota: 3.5 de 5 estrelas3.5/5 (231)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)No EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Nota: 4.5 de 5 estrelas4.5/5 (119)
- Never Split the Difference: Negotiating As If Your Life Depended On ItNo EverandNever Split the Difference: Negotiating As If Your Life Depended On ItNota: 4.5 de 5 estrelas4.5/5 (838)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaNo EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaNota: 4.5 de 5 estrelas4.5/5 (265)
- The Little Book of Hygge: Danish Secrets to Happy LivingNo EverandThe Little Book of Hygge: Danish Secrets to Happy LivingNota: 3.5 de 5 estrelas3.5/5 (399)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyNo EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyNota: 3.5 de 5 estrelas3.5/5 (2219)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeNo EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeNota: 4 de 5 estrelas4/5 (5794)
- Team of Rivals: The Political Genius of Abraham LincolnNo EverandTeam of Rivals: The Political Genius of Abraham LincolnNota: 4.5 de 5 estrelas4.5/5 (234)
- The Emperor of All Maladies: A Biography of CancerNo EverandThe Emperor of All Maladies: A Biography of CancerNota: 4.5 de 5 estrelas4.5/5 (271)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreNo EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreNota: 4 de 5 estrelas4/5 (1090)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersNo EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersNota: 4.5 de 5 estrelas4.5/5 (344)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceNo EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceNota: 4 de 5 estrelas4/5 (894)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureNo EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureNota: 4.5 de 5 estrelas4.5/5 (474)
- The Unwinding: An Inner History of the New AmericaNo EverandThe Unwinding: An Inner History of the New AmericaNota: 4 de 5 estrelas4/5 (45)
- The Yellow House: A Memoir (2019 National Book Award Winner)No EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Nota: 4 de 5 estrelas4/5 (98)
- Emergency Department Case Management: Second EditionDocumento39 páginasEmergency Department Case Management: Second EditionsadikinAinda não há avaliações
- Urine The Spotlight. Urine Therapy Newsletter Debut - by Urine The Spotlight - Nov, 2021 - MediumDocumento28 páginasUrine The Spotlight. Urine Therapy Newsletter Debut - by Urine The Spotlight - Nov, 2021 - Mediuminfo-501699Ainda não há avaliações
- VBAC Guide: Risks, Benefits & ManagementDocumento12 páginasVBAC Guide: Risks, Benefits & Managementnyangara50% (2)
- NMC CBT SAMPLE Q&A PART 3 KEY NURSING CONCEPTSDocumento14 páginasNMC CBT SAMPLE Q&A PART 3 KEY NURSING CONCEPTSJoane FranciscoAinda não há avaliações
- NCP Risk For Impaired Skin Integrity Related To Ongoing Phototherapy Secondary To Increased Bilirubin LevelsDocumento2 páginasNCP Risk For Impaired Skin Integrity Related To Ongoing Phototherapy Secondary To Increased Bilirubin LevelsIrish Bantolo100% (1)
- Retraction Ring LeafletDocumento2 páginasRetraction Ring LeafletAna100% (1)
- Early Mobilization For Patient Use Mechanical VentilatorDocumento17 páginasEarly Mobilization For Patient Use Mechanical VentilatorEviAinda não há avaliações
- Garnacho Montero2005Documento6 páginasGarnacho Montero2005EviAinda não há avaliações
- Sarcopenia 4Documento7 páginasSarcopenia 4EviAinda não há avaliações
- Sarcopenia 1Documento2 páginasSarcopenia 1EviAinda não há avaliações
- 10 1001@jama 2016 0287Documento10 páginas10 1001@jama 2016 0287ompardor7554Ainda não há avaliações
- CCM 42 4 2013 09 20 Vanpee 12-02363 SDC1Documento12 páginasCCM 42 4 2013 09 20 Vanpee 12-02363 SDC1Roberto Godoy DiazAinda não há avaliações
- 10.1371@journal - Pone.0194967 Resiko JatuhDocumento14 páginas10.1371@journal - Pone.0194967 Resiko JatuhEviAinda não há avaliações
- Efect of EarlyDocumento12 páginasEfect of EarlyEviAinda não há avaliações
- 2014 BJM MeowsDocumento7 páginas2014 BJM MeowshendraAinda não há avaliações
- Vincent2010 SepsisDocumento5 páginasVincent2010 SepsisEviAinda não há avaliações
- Sepsis 2019Documento12 páginasSepsis 2019EviAinda não há avaliações
- Constitutive Activation of MAPK Cascade in Acute Quadriplegic MyopathyDocumento12 páginasConstitutive Activation of MAPK Cascade in Acute Quadriplegic MyopathyEviAinda não há avaliações
- Kizilarslanoglu 2016Documento7 páginasKizilarslanoglu 2016EviAinda não há avaliações
- Garnacho Montero2005Documento6 páginasGarnacho Montero2005EviAinda não há avaliações
- Accepted Manuscript: 10.1016/j.chest.2016.10.015Documento56 páginasAccepted Manuscript: 10.1016/j.chest.2016.10.015Anonymous 6bOdJC1Ainda não há avaliações
- Vanpee 2014Documento12 páginasVanpee 2014EviAinda não há avaliações
- 10 1001@jama 2016 0287Documento10 páginas10 1001@jama 2016 0287ompardor7554Ainda não há avaliações
- Constitutive Activation of MAPK Cascade in Acute Quadriplegic MyopathyDocumento12 páginasConstitutive Activation of MAPK Cascade in Acute Quadriplegic MyopathyEviAinda não há avaliações
- Aare2013 PDFDocumento9 páginasAare2013 PDFEviAinda não há avaliações
- Aare2013 PDFDocumento9 páginasAare2013 PDFEviAinda não há avaliações
- Vincent2010 SepsisDocumento5 páginasVincent2010 SepsisEviAinda não há avaliações
- Bed Rest and Myopathies: Arny A. Ferrando, Douglas Paddon-Jones and Robert R. WolfeDocumento6 páginasBed Rest and Myopathies: Arny A. Ferrando, Douglas Paddon-Jones and Robert R. WolfeEviAinda não há avaliações
- Vincent2010 SepsisDocumento5 páginasVincent2010 SepsisEviAinda não há avaliações
- Intensive Care Unit-Acquired Weakness: Risk Factors and PreventionDocumento7 páginasIntensive Care Unit-Acquired Weakness: Risk Factors and PreventionEviAinda não há avaliações
- 10 1001@jama 2016 0287Documento10 páginas10 1001@jama 2016 0287ompardor7554Ainda não há avaliações
- 10 1001@jama 2016 0287Documento10 páginas10 1001@jama 2016 0287ompardor7554Ainda não há avaliações
- 10 1001@jama 2016 0287Documento10 páginas10 1001@jama 2016 0287ompardor7554Ainda não há avaliações
- Verceles 2018Documento33 páginasVerceles 2018EviAinda não há avaliações
- Constitutive Activation of MAPK Cascade in Acute Quadriplegic MyopathyDocumento12 páginasConstitutive Activation of MAPK Cascade in Acute Quadriplegic MyopathyEviAinda não há avaliações
- Stevens 2007Documento16 páginasStevens 2007EviAinda não há avaliações
- KCS 2017 04 30 PDFDocumento192 páginasKCS 2017 04 30 PDFameetdeyAinda não há avaliações
- Shalya Paper-I PDFDocumento17 páginasShalya Paper-I PDFSusmita VinupamulaAinda não há avaliações
- Ra-031103 - Professional Teacher - Secondary (Tle) - Tacloban - 10-2022Documento135 páginasRa-031103 - Professional Teacher - Secondary (Tle) - Tacloban - 10-2022AILENAinda não há avaliações
- NachiketVp 1Documento42 páginasNachiketVp 1Nachiket Vijay PotdarAinda não há avaliações
- Clinical Laboratory LawDocumento26 páginasClinical Laboratory LawLouise AntiolaAinda não há avaliações
- Acute Purulent Diseases of Fingers and HandDocumento9 páginasAcute Purulent Diseases of Fingers and Handvem_nikhil4uAinda não há avaliações
- Ethic Letter - Arina NurfiantiDocumento1 páginaEthic Letter - Arina NurfiantiDayana SilalahiAinda não há avaliações
- Chemoregimen - Testicular CancerDocumento2 páginasChemoregimen - Testicular CancerNanda Asyura RizkyaniAinda não há avaliações
- 4 . CVS 2023Documento6 páginas4 . CVS 2023Chipego NyirendaAinda não há avaliações
- Leaflet Sched of Doctors As of May 31, 2Documento3 páginasLeaflet Sched of Doctors As of May 31, 2Philip Jay-ar DimailigAinda não há avaliações
- Book2 Wound Dressing GuideDocumento51 páginasBook2 Wound Dressing GuideBrian Niu100% (1)
- Prezentare Teo Noua 3Documento30 páginasPrezentare Teo Noua 3Zlate TeodorAinda não há avaliações
- Application of Nursing ProcessDocumento2 páginasApplication of Nursing ProcessClarence ViboraAinda não há avaliações
- Complications of Blood TransfusionsDocumento4 páginasComplications of Blood TransfusionsZain Hadi100% (1)
- Major Internship DTR JulyandaugustDocumento1 páginaMajor Internship DTR JulyandaugustGeraldineMoletaGabutin100% (1)
- Nims Tariff ListDocumento54 páginasNims Tariff ListsreekanthAinda não há avaliações
- Medical Leave CertificatesDocumento4 páginasMedical Leave CertificatesDhana LakshmiAinda não há avaliações
- Lesson 16 Nutrition HESI RN FLMIR 1904COHORT PDFDocumento16 páginasLesson 16 Nutrition HESI RN FLMIR 1904COHORT PDFLuis Hernandez100% (5)
- Herpes ZosterDocumento42 páginasHerpes ZostermehranerezvaniAinda não há avaliações
- Nurs 604 Both Journal Entries and Narrative For WeebleyDocumento11 páginasNurs 604 Both Journal Entries and Narrative For Weebleyapi-323169345Ainda não há avaliações
- Comorbidities of Hearing Loss and The Implications of Multimorbidity For Audiological Care. Hearing Research - 10.1016:j.heares.2018.06.008Documento12 páginasComorbidities of Hearing Loss and The Implications of Multimorbidity For Audiological Care. Hearing Research - 10.1016:j.heares.2018.06.008ALEIRAMGONZALEZAinda não há avaliações
- Recognizing and Reporting Red Flags For The Physical Therapist Assistant 1stDocumento52 páginasRecognizing and Reporting Red Flags For The Physical Therapist Assistant 1stsummer.yates611100% (38)
- Health Checklist Form For Visitors: Nakaranas Ka Ba NG Mga Sumusunod: Oo HindiDocumento2 páginasHealth Checklist Form For Visitors: Nakaranas Ka Ba NG Mga Sumusunod: Oo HindiCoin CharAinda não há avaliações
- Data Peserta Gartheting LT 3aumst Final 2022Documento11 páginasData Peserta Gartheting LT 3aumst Final 2022Doni IrawanAinda não há avaliações