Escolar Documentos
Profissional Documentos
Cultura Documentos
A. Osteoarthritis: Understanding
Enviado por
Belle Makinano0 notas0% acharam este documento útil (0 voto)
26 visualizações4 páginashh
Título original
ARTHRITIS
Direitos autorais
© © All Rights Reserved
Formatos disponíveis
DOCX, PDF, TXT ou leia online no Scribd
Compartilhar este documento
Compartilhar ou incorporar documento
Você considera este documento útil?
Este conteúdo é inapropriado?
Denunciar este documentohh
Direitos autorais:
© All Rights Reserved
Formatos disponíveis
Baixe no formato DOCX, PDF, TXT ou leia online no Scribd
0 notas0% acharam este documento útil (0 voto)
26 visualizações4 páginasA. Osteoarthritis: Understanding
Enviado por
Belle Makinanohh
Direitos autorais:
© All Rights Reserved
Formatos disponíveis
Baixe no formato DOCX, PDF, TXT ou leia online no Scribd
Você está na página 1de 4
Understanding at the bottom of a test tube that contains a
blood sample. Normally, red blood cells
- Arthritis is the swelling and tenderness of one or
more of your joints. The main symptoms of arthritis settle relatively slowly. A faster-than-
are joint pain and stiffness, which typically worsen normal rate may indicate inflammation in
with age. The most common types of arthritis are the body.
osteoarthritis and rheumatoid arthritis. o Normal:
- Men younger than 50: 0-15 mm/h
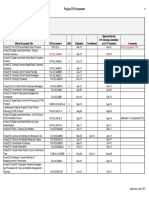
Common types of Arthritis:
- Men older than 50: 0-20 mm/h
A. Osteoarthritis - Women younger than 50: 0-20
mm/h
- Defined as a form of arthritis with progressive
- Women older than 50: 0-30 mm/h
destruction of the cartilage in both the synovial
joints and vertebrae C. Gout
- Defined as a metabolic disease marked by
Laboratory and Diagnostic Tests
increased serum uric acid levels (hyperuricemia)
X-ray Imaging – Cartilage doesn't show up on
and joint inflammation
X-ray images, but cartilage loss is revealed by
a narrowing of the space between the bones
Laboratory and Diagnostic Tests
in your joint. An X-ray can also show bone
Joint Fluid Test – Your doctor may use a
spurs around a joint.
needle to draw fluid from your affected joint.
Magnetic Resonance Imaging (MRI) – An MRI
Urate crystals may be visible when the fluid
uses radio waves and a strong magnetic field
is examined under a microscope.
to produce detailed images of bone and soft
Blood Test – Your doctor may recommend a
tissues, including cartilage. An MRI isn't
blood test to measure the levels of uric acid
commonly needed to diagnose osteoarthritis
and creatinine in your blood. Blood test
but can help provide more information in
results can be misleading, though. Some
complex cases.
people have high uric acid levels, but never
Joint Fluid Analysis – Your doctor might use
experience gout. And some people have signs
a needle to draw fluid from an affected joint.
and symptoms of gout, but don't have
The fluid is then tested for inflammation and
unusual levels of uric acid in their blood.
to determine whether your pain is caused by
X-ray Imaging – Joint X-rays can be helpful to
gout or an or an infection rather than
rule out other causes of joint inflammation.
osteoarthritis.
Ultrasound – Musculoskeletal ultrasound
can detect urate crystals in a joint or in a
B. Rheumatoid Arthritis
- Defined as a chronic, progressive, systemic, tophus. This technique is more widely used
autoimmune disease with inflammation of the in Europe than in the United States.
joints and deformity Dual Energy CT Scan – This type of imaging
Laboratory and Diagnostic Tests can detect the presence of urate crystals in a
Rheumatoid factor (RF) blood test – joint, even when it is not acutely inflamed.
Rheumatoid factor (RF) is a protein made by This test is not used routinely in clinical
your immune system that can attack healthy practice due to the expense and is not widely
tissue in your body. Healthy people don’t available
make RF. So, the presence of RF in your blood
can indicate that you have an autoimmune Pathophysiology:
disease A. Osteoarthritis (OA)
A rheumatoid factor (RF) blood test Underlying pathophysiology:
measures the amount of the RF antibody Synovial joint cartilage deteriorates as a
present in the blood. Normally, antibodies result of damage to chondrocytes (cells
are produced by the immune system to help responsible for binding cartilage)
destroy and eliminate invading bacteria and
Cartilage softens with age, narrowing
viruses that can cause disease. But the RF
the joint space
antibody can attach to normal body tissue,
Mechanical injury also erodes articular
resulting in damage.
o Normal: 0-20 u/mL (units per cartilage
milliliter of blood) Bone underneath the cartilage is
o High: 20 u/mL or higher unprotected and scleroses
Cartilage flakes irritate the synovial
Anti-cyclic Citrullinated Peptide (anti-CCP) – lining, which becomes fibrotic, limiting
Anti-cyclic citrullinated peptide (anti-CCP) is joint movements
an antibody present in most rheumatoid
Synovial fluid may be forced into bone
arthritis patients. A positive anti-CCP test
defects, causing cysts
result can be used in conjunction with other
New bone (osteophyte, or bone spur)
blood tests, imaging tests, and/or physical
forms at joint margins as the articular
examination findings to diagnose
cartilage erodes, causing gross
rheumatoid arthritis.
alteration of the bony contours and
o Normal: 20 u/mL or less
enlargement of the joint
Erythrocyte Sedimentation Rate (ESR) – is a
Etiology:
type of blood test that measures how
a. Primary idiopathic (normal part of aging):
quickly erythrocytes (red blood cells) settle
- Metabolic factors (endocrine disorders B. Rheumatoid Arthritis (RA)
such as hyperthyroidism) and genetic
Underlying pathophysiology
factors (decreased collagen synthesis)
- Chemical factors (drugs such as steroids Exposure to a viral pathogen may
that stimulate the collagen-digesting initiate the inflammatory response;
enzymes in synovial membrane) immunoglobulin G (IgG) is formed in
- Mechanical factors (repeated stress on response to the antigen, but for some
joint) unknown reason the body begins to
b. Secondary disorder (follows an identifiable produce autoantibodies (called
predisposing event that leads to rheumatoid factors) against IgG
degenerative changes) - The rheumatoid factors
- Trauma (most common cause) combine with IgG to form
- Congenital deformity immune complexes
- Obesity - The continued presence of the
immune complexes within the
Signs and Symptoms: joint cavity results in chronic
a. Dull, aching pain in the affected joint relieved inflammation and destruction
with rest of the articular cartilage as well
b. Numbness or tingling at night, associated as surrounding joint structures
with disease progression secondary to nerve The synovial membrane (located within
damages the joint capsule and responsible for
c. Crepitus with joint movement producing synovial fluid to lubricate
d. Edema and stiffness in the affected joint joint structures) hypertrophies and
e. Decreased range of motion (ROM) and ability thickens secondary to chronic
to participate in activities of daily living inflammation
(ADLs) - Blood supply to the area is
f. Joint deformities: Heberden’s nodes occluded and cellular necrosis
(formation if hard nodules in the DIP joints, occurs
resulting in joint deformity) and Bouchard’s - These events lead to the
nodes (formation of hard nodules in the PIP formation of pannus (vascular
joints resulting in joint deformity) granulation tissue that forms in
g. Symptoms may vary in severity and may the synovial membrane of
range from mild intermittent discomfort to clients with RA)
complete disability - Pannus gradually extends from
the synovial membrane and
Complications: surface of the articular
a. Decreased joint ROM cartilage into the joint capsule
b. Irreversible joint changes and node and subchondral bone causing
formation destruction of the bone
c. Loss of independence in activities of daily Fibrous adhesions and bony ankylosis
living (ADLs) (joint immobility or fixation secondary
d. Pain (debilitating in later stages) to an underlying disease process occurs
e. Subluxation of the joint as the involved bone is destroyed; the
inflammatory process extends to the
Nursing management: support structures of the bone, tendons
a. Teach self-care skills to promote joint health and ligaments, and joint instability and
b. Assist with physical therapy, and encourage deformities occur
the patient to perform gentle isometric ROM Etiology
exercises a. Unknown etiology; however, evidence
c. If the patient needs surgery, provide supports that disease progression is related
appropriate preoperative and postoperative to autoimmune processes in middle age
care
d. Provide emotional support and reassurance Signs and Symptoms:
to help the patient cope with limited mobility a. Initially may present with vague systemic
e. Instruct on safety in home symptoms such as anorexia, weight loss,
i. Eliminate throw rugs in home fever and loss of energy
ii. Use good body mechanics when b. Early disease states will present with
performing ADLs and work/leisure inflammation, swelling, and decreased
activities movement of the joints in the hand (PIP and
iii. Use a shower chair and hand rails in MCP), feet (MTP), wrists, and elbows; as RA
bathing progresses, joints of the knees, hips, and
iv. Use cane and walker as directed to cervical spine may also be involved
decrease workload on hips and c. The American Rheumatism
knees d. Association has developed diagnostic
v. Use well-fitting, supportive shoes criteria for rheumatoid arthritis; evidence of
when ambulating four out of seven criteria must be present to
confirm the diagnosis
i. Morning stiffness lasting for at least Underlying pathophysiology
1 hour and persisting over at least 6 Uric acid becomes supersaturated in the
weeks blood and body fluids
ii. Arthritis with swelling or effusion Uric acid then crystallizes and forms a
of three or more joints persisting precipitate of urate salts that
for at least 6 weeks accumulates in connective tissue
iii. Arthritis of wrist, MCP, or PIP joints throughout the body
persisting for at least 6 weeks Crystal deposits (called tophi) trigger an
iv. Symmetric arthritis with acute inflammatory response when
simultaneous involvement of neutrophils begin to ingest them
corresponding joints on both sides Neutrophils release lysosomes that
of the body damage tissues and perpetuate the
v. Rheumatoid nodules inflammation
vi. Positive serum rheumatoid factor With gout that produces no symptoms:
vii. Characteristic radiologic changes of - Serum urate levels increase but
rheumatoid arthritis notes in hands don’t crystallize
and wrists - Progression may cause
Complications: hypertension or urate renal
a. Risk to carpal tunnel syndrome calculi
increases Etiology
b. Pain (debilitating in later stages) - Exact cause unknown
c. If rheumatoid arthritis isn't treated - Possible causes:
early or isn't well controlled, the Genetic defect in purine
inflammation in the joints could lead to metabolism causing
significant and permanent damage. hyperuricemia
Retention of uric acid
Nursing management: Combination of the above
a. Administration of medications like - Causes of secondary gout (develops
NSAIDs, systemic corticosteroids, and during the course of another disease)
disease-modifying drugs (MDARDs)
Alcoholism
b. Instruct on disease process and
Diabetes mellitus
treatment regimen
Hypertension
c. Refer to support groups including Obesity
Arthritis Foundation
Renal disease
d. Emphasize rest to decrease joint stress
Sickle cell anemia
i. Pace activities
ii. Perform activities while sitting
Signs and Symptoms:
when possible
a. Sudden onset of severe pain in one joint;
iii. Splints for hands and wrists
the great toe is most commonly affected;
iv. Relaxation techniques
however, it
v. Guided imagery
b. may occur in the instep, wrist, tarsal
e. Collaborate with physical therapy (PT)
joints, knees, elbows, and ankles
regarding therapeutic exercises
c. Joint appears red or dusky, swollen,
program, isotonic exercises, passive
edematous, and is extremely tender to
range of motion (PROM), and active
touch
range of motion (AROM) to maintain
d. Tophi: hard, movable, nodules with
muscle strength and ROM
irregular surfaces occur in synovium,
f. Collaborate with occupational therapist
helix of ear, olecranon bursa, and
(OT) regarding assistive devices for
Achilles’ tendon (most common
ADLs, tips for joint protection and work
locations); associated with chronic
simplification
untreated gout; can resolve with
g. Teach action and side effects of
treatment
medications used for pain control
h. Implement and assess effectiveness of
Complications:
pain relief measures
a. Renal calculi
i. Medications
b. Atherosclerotic disease
ii. Application of heat or cold,
c. Cardiovascular lesions
depending on what works for
d. Stroke
client
e. Coronary thrombosis
iii. Firm mattress for sleeping and
proper positioning in bed for
Nursing management:
comfort
a. Encourage bed rest, but use a foot cradle
i. Instruct on home safety
to keep bed covers off extremely
j. Instruct on hazards of immobility if
sensitive, inflamed joints
bedridden and teach prevention
b. Give pain medications as needed,
C. Gout Arthritis especially during acute attacks
c. Apply hot or cold packs to inflamed Steroids decrease inflammation and reduce the activity
joints according to what the patient of the immune system. Inflammation is a process by
finds most effective which the body's white blood cells and chemicals
d. Urge the patient to drink plenty of fluids protect the body against infection and foreign
to prevent formation of renal calculi organisms such as bacteria and viruses.
e. Watch for gout attacks 24 to 96 hours Side effects: Blurred vision, difficulty sleeping, high
after surgery blood pressure, increased appetite, weight gain, easy
bruising, glaucoma
f. Before and after surgery, administer
colchicine, as ordered, to help prevent
E. Hyaluronan Injections – There are several versions of
attacks
hyaluronan injections, also called
g. Make sure the patient understands the
viscosupplementation, that are used to
importance of checking serum uric acid
treat osteoarthritis of the knee. They are injected
levels
directly into the joint. Some studies have shown some
h. periodically and avoiding high-purine
benefit for reducing pain for periods of up to six
foods
months, but others have shown more limited results.
i. Teach the patient to report any adverse
effects from medications immediately Side effects: Injection site reactions (pain, swelling,
Medications: warmth, stiffness, puffiness, or fluid buildup in or around the
knee), muscle pain, trouble walking, fever, chills, nausea
A. Analgesics (Acetaminophen) – Still considered first-
line therapy although more recent trials find NSAIDs
more effective, Acetaminophen is available without a
prescription and is a commonly used pain reliever for
people with arthritis.
Side effects: Usually no side effects, rare but very
serious allergic reaction, severe dizziness, trouble
breathing
B. Nonsteroidal Anti-Inflammatory Drugs (NSAIDs)
- Aspirin (Bufferin, Bayer)
- Celecoxib (Celebrex)
- Diclofenac (Cataflam, Voltaren0
Nonsteroidal anti-inflammatory drugs or NSAIDs are
available both over-the-counter and by prescription.
Almost everyone with arthritis has taken or is taking
one of these drugs. Prescription doses can help curb
joint inflammation.
Side effects: Stomach pain and heartburn, stomach
ulcers, headache and dizziness, high blood pressure,
liver and kidney problems
C. Disease-Modifying Antirheumatic Drugs (DMARDs) –
These drugs are often able to alter the course of some
forms of inflammatory arthritis -- diseases such
as rheumatoid arthritis, psoriatic arthritis,
or ankylosing spondylitis – that can destroy the joints.
Often these drugs are the first ones used for these
diseases.
DMARDs work by interfering with or suppressing the
immune system that attacks the joints in people with
certain forms of inflammatory arthritis. Aggressive
treatment of arthritis often involves using one or more
DMARDs.
Although effective, DMARDs have a higher risk of
serious side effects. It also often takes weeks for you to
notice the benefits of taking a DMARD. Therefore, they
are often combined with a faster-working drug such as
an NSAID, another painkiller, or steroids to help relieve
some arthritis symptoms.
Side Effects: Stomach upset, Liver problems, Infection-
fighting white blood cells may also be decreased
D. Corticosteroids
- Hydrocortisone (Cortisol)
- Triamcinolone acetonide (Kenalog)
- Triamcinolone hexacetonide
(Aristospan)
Você também pode gostar
- Self Assessment in Musculoskeletal Pathology X-raysNo EverandSelf Assessment in Musculoskeletal Pathology X-raysNota: 5 de 5 estrelas5/5 (2)
- Sex 2Documento14 páginasSex 2Abhijit BAinda não há avaliações
- Rheumatoid Arthritis (RA)Documento15 páginasRheumatoid Arthritis (RA)Mel Christian BaldozAinda não há avaliações
- A Study of Serum For Calcium and Ra Factor in Patients Undergoing Rheumatoid ArthritisDocumento14 páginasA Study of Serum For Calcium and Ra Factor in Patients Undergoing Rheumatoid ArthritisInternational Journal of Innovative Science and Research Technology100% (2)
- Acutely Swollen JointDocumento7 páginasAcutely Swollen JointHossein VakiliAinda não há avaliações
- Differential Diagnosis of Polyarticular ArthritisDocumento7 páginasDifferential Diagnosis of Polyarticular ArthritismedicabrujaAinda não há avaliações
- Ra and Osteoarthritis R IfDocumento43 páginasRa and Osteoarthritis R IfsnfhanAinda não há avaliações
- Lecture 3:osteoarthritis (2007 Powerpoint)Documento54 páginasLecture 3:osteoarthritis (2007 Powerpoint)j.doe.hex_87100% (1)
- AsdsDocumento5 páginasAsdsGerald MasagandaAinda não há avaliações
- 2033 Rheumatoid Arthritis 14-1 PDFDocumento48 páginas2033 Rheumatoid Arthritis 14-1 PDFAfif Al FatihAinda não há avaliações
- Rheumatoid Arthritis: Sex. AGE Family HistoryDocumento4 páginasRheumatoid Arthritis: Sex. AGE Family HistoryLiana Louisse JoseAinda não há avaliações
- Vertebral Osteomyelitis PanelDocumento11 páginasVertebral Osteomyelitis PanelAulia AgniAinda não há avaliações
- Osteoarthritis: By: Vien HardiyantiDocumento37 páginasOsteoarthritis: By: Vien HardiyantiPhannyta CherryAinda não há avaliações
- Auca1 DLP Medical Surgical 3 Bito Adam Sealtiel PasayDocumento2 páginasAuca1 DLP Medical Surgical 3 Bito Adam Sealtiel PasayYoungbloodAinda não há avaliações
- Artrocenseis - Libro de Reumato en InglesDocumento15 páginasArtrocenseis - Libro de Reumato en InglesPabloAinda não há avaliações
- Osteomyelitis Word FileDocumento6 páginasOsteomyelitis Word FileCxarina RamirezAinda não há avaliações
- Assignment Submitted To DR Iqra Naz 70063678 Habiba Jameel DPT 10 Semester. Topic: ArthritisDocumento10 páginasAssignment Submitted To DR Iqra Naz 70063678 Habiba Jameel DPT 10 Semester. Topic: ArthritisMuiz SaddozaiAinda não há avaliações
- NCM 104 - ArthrocentesisDocumento15 páginasNCM 104 - ArthrocentesisAxl SalimoAinda não há avaliações
- RheumatoidDocumento64 páginasRheumatoidtsukiyaAinda não há avaliações
- UnderstandingGout Brochure PDFDocumento12 páginasUnderstandingGout Brochure PDFGary HoAinda não há avaliações
- Presentation - JointsDocumento21 páginasPresentation - JointsAlejandra MorenoAinda não há avaliações
- Joint PainDocumento8 páginasJoint Painحنين حسن عبد علي حسينAinda não há avaliações
- Case Presentation 2 GERIA OsteoarthritisDocumento80 páginasCase Presentation 2 GERIA OsteoarthritisJasmine GomezAinda não há avaliações
- Diagnosing Osteoarthritis: Fill in The Gaps: by Alex and PacificaDocumento9 páginasDiagnosing Osteoarthritis: Fill in The Gaps: by Alex and PacificaPacifica IshimweAinda não há avaliações
- Clinical Review: OsteoarthritisDocumento4 páginasClinical Review: OsteoarthritismarindadaAinda não há avaliações
- 1 s2.0 S0301562919312736 MainDocumento1 página1 s2.0 S0301562919312736 MainOsama BasharatAinda não há avaliações
- Osteoarthritis of The Hip: Clinical PracticeDocumento9 páginasOsteoarthritis of The Hip: Clinical PracticeMarina Tomasenco - DaniciAinda não há avaliações
- Arthritis HWDocumento9 páginasArthritis HWraphaelAinda não há avaliações
- OsteomyeolitisDocumento10 páginasOsteomyeolitisJane VargasAinda não há avaliações
- Investigations in Rheumatology: What's New?Documento10 páginasInvestigations in Rheumatology: What's New?i can always make u smile :DAinda não há avaliações
- OstlitisDocumento2 páginasOstlitisБаяржавхлан СүхбаатарAinda não há avaliações
- Pseudogout Case PresentationDocumento16 páginasPseudogout Case PresentationSamantha SykesAinda não há avaliações
- Rheumatoid ArthritisDocumento37 páginasRheumatoid ArthritisPetit NacarioAinda não há avaliações
- 8.6. RadiologyDocumento3 páginas8.6. Radiologyjunius101Ainda não há avaliações
- Assessment of Musculo-Skeletal System: 2 Year B. SC NursingDocumento33 páginasAssessment of Musculo-Skeletal System: 2 Year B. SC NursingRubin100% (1)
- Assessment MusculoskeletalDocumento33 páginasAssessment MusculoskeletalRubinAinda não há avaliações
- Total Knee Replacement: Done By: Sajeda Moha'dDocumento27 páginasTotal Knee Replacement: Done By: Sajeda Moha'dlolo223Ainda não há avaliações
- Apyogenous Arthritis: Department of Orthopaedics The First Affiliated Hospital Dalian Medical University Tang KaiDocumento131 páginasApyogenous Arthritis: Department of Orthopaedics The First Affiliated Hospital Dalian Medical University Tang KaiFathimathAinda não há avaliações
- Arthritis Joint Pain ReliefDocumento14 páginasArthritis Joint Pain ReliefSam CookAinda não há avaliações
- ArthritisDocumento3 páginasArthritisGlady mae LimAinda não há avaliações
- Name: Rayan Jabar Anwar Group A Homework: Rheumatoid ArthritisDocumento2 páginasName: Rayan Jabar Anwar Group A Homework: Rheumatoid ArthritisRayan Jabbar0% (1)
- Osteoarthritis, Gouty Arthritis, and Rheumatoid ArthritisDocumento37 páginasOsteoarthritis, Gouty Arthritis, and Rheumatoid ArthritisDianaAinda não há avaliações
- All Topics Are Updated As New Evidence Becomes Available and Our Peer Review Process Is CompleteDocumento88 páginasAll Topics Are Updated As New Evidence Becomes Available and Our Peer Review Process Is CompleteJaime BarraganAinda não há avaliações
- Osteoarthritis 191016103144Documento49 páginasOsteoarthritis 191016103144dr.abouzaid098Ainda não há avaliações
- Osteo Art RiteDocumento27 páginasOsteo Art RiteRafael Attiê PennacchiAinda não há avaliações
- CPD MSK19-Thu-1-SchwabDocumento51 páginasCPD MSK19-Thu-1-SchwabGiaAinda não há avaliações
- ArthritisDocumento57 páginasArthritisSella Septi EkasariAinda não há avaliações
- Inflammatory Joint Diseases Handout-Admission ExamDocumento11 páginasInflammatory Joint Diseases Handout-Admission ExamNona NadimAinda não há avaliações
- CLN 75 1500Documento7 páginasCLN 75 1500Hevin GokulAinda não há avaliações
- Jurnal Rheumatoid Arthritis - 6 PDFDocumento4 páginasJurnal Rheumatoid Arthritis - 6 PDFJeanstepanisaragihAinda não há avaliações
- Arthritides 5th Year-UNZA LectureDocumento76 páginasArthritides 5th Year-UNZA LectureMohammed AadeelAinda não há avaliações
- Cambios Radiograficos de Aps BJM 2005Documento4 páginasCambios Radiograficos de Aps BJM 2005Leonardo GarciaAinda não há avaliações
- Arthritis: Ryan Carr Serafina Morada-Angulo Maurice SmithDocumento42 páginasArthritis: Ryan Carr Serafina Morada-Angulo Maurice SmithSandeep MuleyAinda não há avaliações
- Rheumatology Year 4Documento90 páginasRheumatology Year 4Abdalla SamatarAinda não há avaliações
- Rheumatology For AMK: Abhinav Singh PMSDocumento43 páginasRheumatology For AMK: Abhinav Singh PMSTerrence ChanAinda não há avaliações
- Vol4 Issue6 08Documento8 páginasVol4 Issue6 08Prasanna BabuAinda não há avaliações
- Rheumatoid Arthritis: CausesDocumento8 páginasRheumatoid Arthritis: CausesJan Ford TuqueroAinda não há avaliações
- DescargaDocumento8 páginasDescargaFrancis ValdiviaAinda não há avaliações
- Bone DisordersDocumento4 páginasBone Disorderskierz23Ainda não há avaliações
- Case Study2Documento9 páginasCase Study2Amr LotfyAinda não há avaliações
- Beginnings of GriefDocumento3 páginasBeginnings of GriefBelle MakinanoAinda não há avaliações
- Pulmonary TB DrugsDocumento6 páginasPulmonary TB DrugsBelle MakinanoAinda não há avaliações
- Belle, Health Care Ethics 1.Documento2 páginasBelle, Health Care Ethics 1.Belle MakinanoAinda não há avaliações
- Juliena DraftDocumento3 páginasJuliena DraftBelle MakinanoAinda não há avaliações
- Drug Study AmbroxolDocumento2 páginasDrug Study AmbroxolBelle MakinanoAinda não há avaliações
- Example of A BrochureDocumento3 páginasExample of A BrochureBelle MakinanoAinda não há avaliações
- Hemoglobinopathies OutlineDocumento1 páginaHemoglobinopathies OutlineBelle MakinanoAinda não há avaliações
- NCOVgroup 2Documento1 páginaNCOVgroup 2Belle MakinanoAinda não há avaliações
- Tele OlogyDocumento7 páginasTele OlogyBelle MakinanoAinda não há avaliações
- Care of Patients With Asthma: Peak Flow MonitoringDocumento2 páginasCare of Patients With Asthma: Peak Flow MonitoringBelle MakinanoAinda não há avaliações
- Pregnancy ComplicationsDocumento3 páginasPregnancy ComplicationsBelle MakinanoAinda não há avaliações
- MU2010Documento1 páginaMU2010Belle MakinanoAinda não há avaliações
- Hemoglobinopathies OutlineDocumento1 páginaHemoglobinopathies OutlineBelle MakinanoAinda não há avaliações
- HEALTHCAREDocumento1 páginaHEALTHCAREBelle MakinanoAinda não há avaliações
- Concept of Family & Family Nursing ProcessDocumento3 páginasConcept of Family & Family Nursing ProcessBelle MakinanoAinda não há avaliações
- Care of Women and Families During PostpartumDocumento3 páginasCare of Women and Families During PostpartumBelle MakinanoAinda não há avaliações
- Principles For All MedicationDocumento6 páginasPrinciples For All MedicationBelle MakinanoAinda não há avaliações
- Cardiovascular Drugs: D. Hormone DeliveryDocumento8 páginasCardiovascular Drugs: D. Hormone DeliveryBelle MakinanoAinda não há avaliações
- Ha NotesDocumento1 páginaHa NotesBelle MakinanoAinda não há avaliações
- Homeostatic Imbalances in The SkinDocumento1 páginaHomeostatic Imbalances in The SkinBelle MakinanoAinda não há avaliações
- Cardiovascular Drugs: D. Hormone DeliveryDocumento8 páginasCardiovascular Drugs: D. Hormone DeliveryBelle MakinanoAinda não há avaliações
- Sources: Karch, Pharmacology Pilliteri, Maternal Kozier: Delivery?Ismobileset FalseDocumento1 páginaSources: Karch, Pharmacology Pilliteri, Maternal Kozier: Delivery?Ismobileset FalseBelle MakinanoAinda não há avaliações
- Homeostatic Imbalances in The SkinDocumento1 páginaHomeostatic Imbalances in The SkinBelle MakinanoAinda não há avaliações
- Principles For All MedicationDocumento6 páginasPrinciples For All MedicationBelle MakinanoAinda não há avaliações
- Concept of Family & Family Nursing ProcessDocumento3 páginasConcept of Family & Family Nursing ProcessBelle MakinanoAinda não há avaliações
- Continuation Sa PregnancyDocumento3 páginasContinuation Sa PregnancyBelle MakinanoAinda não há avaliações
- Common Drugs in The Labor Room and Delivery RoomDocumento4 páginasCommon Drugs in The Labor Room and Delivery RoomBelle MakinanoAinda não há avaliações
- Control of Microbes in The EnvironmentDocumento7 páginasControl of Microbes in The EnvironmentBelle MakinanoAinda não há avaliações
- Reproductive System ReviewerDocumento2 páginasReproductive System ReviewerBelle MakinanoAinda não há avaliações
- Energy Transfer in Cell During Exercise and Oxygen Metabolism and Transport - PalakDocumento85 páginasEnergy Transfer in Cell During Exercise and Oxygen Metabolism and Transport - Palakpalooo4Ainda não há avaliações
- The Dry Bulk Management StandardDocumento18 páginasThe Dry Bulk Management Standardamu_more44100% (1)
- ELIDA Products CatalogueDocumento37 páginasELIDA Products CatalogueAbhishek AgarwalAinda não há avaliações
- 09.tracheostomy Management by Speech Language Pathologists in SwedenDocumento12 páginas09.tracheostomy Management by Speech Language Pathologists in SwedenCarlonchaCáceresAinda não há avaliações
- Do Roman Catholics KnOw About The Great Pyramids of China?Documento11 páginasDo Roman Catholics KnOw About The Great Pyramids of China?.Ainda não há avaliações
- PEDocumento12 páginasPEMae Ann Base RicafortAinda não há avaliações
- The Joy Luck Club Book 1Documento12 páginasThe Joy Luck Club Book 1loronalicelAinda não há avaliações
- Chapter 1 (PLC)Documento9 páginasChapter 1 (PLC)Kibria PrangonAinda não há avaliações
- ODA X9 2SL DatasheetDocumento8 páginasODA X9 2SL DatasheetYudy UtamaAinda não há avaliações
- DS Ltch00601daa0 R05Documento4 páginasDS Ltch00601daa0 R05rajareddy235Ainda não há avaliações
- Comparison of 3 Tests To Detect Acaricide ResistanDocumento4 páginasComparison of 3 Tests To Detect Acaricide ResistanMarvelous SungiraiAinda não há avaliações
- Bahir Dar University BIT: Faculity of Mechanical and Industrial EngineeringDocumento13 páginasBahir Dar University BIT: Faculity of Mechanical and Industrial Engineeringfraol girmaAinda não há avaliações
- Approved Project 25 StandardsDocumento5 páginasApproved Project 25 StandardsepidavriosAinda não há avaliações
- Me8072 Renewable Sources of EnergyDocumento13 páginasMe8072 Renewable Sources of EnergyNallappan Rajj AAinda não há avaliações
- S590 Machine SpecsDocumento6 páginasS590 Machine SpecsdilanAinda não há avaliações
- Statistics and Probability Module 3Documento3 páginasStatistics and Probability Module 3Eftychia LeegleeAinda não há avaliações
- 2 Contoh Narative TextDocumento9 páginas2 Contoh Narative TextRini RienzAinda não há avaliações
- PTP S3Documento8 páginasPTP S3Yongyin SHENGAinda não há avaliações
- Bolt Action Italian Painting GuideDocumento7 páginasBolt Action Italian Painting GuideTirmcdhol100% (2)
- All About PlantsDocumento14 páginasAll About Plantsapi-234860390Ainda não há avaliações
- RhythmDocumento10 páginasRhythmSalcedo NoelAinda não há avaliações
- Manual 35S EnglishDocumento41 páginasManual 35S EnglishgugiAinda não há avaliações
- Dialog Bahasa InggirsDocumento2 páginasDialog Bahasa InggirsKeRtha NeghaRaAinda não há avaliações
- Product Stock Exchange Learn BookDocumento1 páginaProduct Stock Exchange Learn BookSujit MauryaAinda não há avaliações
- Kodak Easyshare Z712 Is Zoom Digital Camera: User'S GuideDocumento75 páginasKodak Easyshare Z712 Is Zoom Digital Camera: User'S GuideIronko PepeAinda não há avaliações
- Table 1 Minimum Separation DistancesDocumento123 páginasTable 1 Minimum Separation DistancesjhonAinda não há avaliações
- Nutrient DeficiencyDocumento8 páginasNutrient Deficiencyfeiserl100% (1)
- Latihan To: Nilai: 7.4 Benar: 37 Salah: 13Documento17 páginasLatihan To: Nilai: 7.4 Benar: 37 Salah: 13glensAinda não há avaliações
- Solid Modeling Techniques: Constructive Solid Geometry (CSG)Documento22 páginasSolid Modeling Techniques: Constructive Solid Geometry (CSG)amolAinda não há avaliações