Escolar Documentos
Profissional Documentos
Cultura Documentos
Prevalence of Sleep Disturbances During Pregnancy - A Pilot Study
Enviado por
PutriPuputTítulo original
Direitos autorais
Formatos disponíveis
Compartilhar este documento
Compartilhar ou incorporar documento
Você considera este documento útil?
Este conteúdo é inapropriado?
Denunciar este documentoDireitos autorais:
Formatos disponíveis
Prevalence of Sleep Disturbances During Pregnancy - A Pilot Study
Enviado por
PutriPuputDireitos autorais:
Formatos disponíveis
BAOJ Gynaecology
Naseem Ahmed, et al. BAOJ Gynaec 2019, 2: 3
2: 019
Research Article
Prevalence of Sleep Disturbances During Pregnancy – A Pilot Study
Naseem Ahmed1*, Aneeqa Khan2, Asra Waseem2, Tooba Khan2, Hussaina Shabbir2, Abdul Waqas2
1
Department of Pathology, Dow Medical College, Dow University of Health Sciences, Karachi, Pakistan
2
Dow Medical College, Dow University of Health Sciences, Karachi, Pakistan
Abstract contributory factors. Primary care providers should pay attention
towards carrying out preventive and conservative interventions
Background
Key Words: Pregnant Women; Sleep Quality; Contributing Fac-
To determine the prevalence of sleep problems during pregnancy and tors; One Way ANOVA, PSQI Score
factors contributing to it.
Abbreviations
Methods
PSQI (Pittsburg Sleep Quality Index), BMI (body mass index)
A pilot study was conducted to determine the prevalence of sleep
disorders in pregnant women visiting gynecology and obstetrics Introduction
outpatient department, civil hospital, Karachi, Pakistan, ranging in
age from 18-37 years with sample size of 30. Willing participants were Despite being a natural phenomenon, pregnancy is associated with
included irrespective of gestational age. Relation of each contributing major hormonal, psychological and physiological changes. Therefore,
factors with PSQI score was assessed by independent sample t test. it is no wonder that about two-third of pregnant women whine about
One-way ANOVA was applied to compare PSQI scores among 3 abnormal sleep patterns as quoted by a research in Tehran city, Iran.
trimesters, correlation between sleep quality and other variables was [1]. National Sleep Foundation, a US based organization, showed by
found through Pearson’s correlation, P value≤0.05 being considered a recent analysis that more than 79% of women experience changes
significant. in sleep during pregnancy [2]. This problem conventionally worsens
linearly with every trimester [1]. The results of a research in USA
Results proved that a consequential sleep disorder in the first gestational
trimester was present in about quarter percent of women and it
30 women participated in the study among which 1(3.3%) was in her increased up to 15% in the third trimester, meanwhile sleep duration
first trimester, 5(16.7%) were in their second trimester and 24(80%) decreased progressively [3]. A study regarding inhabitants of China
were from third trimester. 16(53.3%) pregnant women being sorted
as having poor sleep quality (PSQI ≥5). Subjective sleep quality, sleep *Corresponding Author: Naseem Ahmed, Department of Pathology,
latency, sleep duration, habitual sleep efficiency, sleep disturbances, Dow Medical College, Dow University of Health Sciences, Karachi,
use of sleeping medication, daytime dysfunction as well as the global Pakistan
PSQI score was not established as being significant with the three Sub Date: April 20th, 2019, Acc Date: April 30th, 2019, Pub Date: May
trimesters (p >0.05). Furthermore, pain in lower back, frequent leg 03rd, 2019
cramps, night awakenings due to increased food cravings and a family
history of sleep disorders were discovered as significant contributing Citation: Naseem Ahmed, Aneeqa Khan, Asra Waseem, Tooba Khan,
factors (p≤0.05). et al. (2019) Prevalence of Sleep Disturbances During Pregnancy – A Pilot
Study. BAOJ Gynaec 2: 019.
Conclusion Copyright: © 2019 Naseem Ahmed, et al. This is an open access article
distributed under the terms of the Creative Commons Attribution
Disturbed sleep is a widespread problem encountered by pregnant License, which permits unrestricted use, distribution, and reproduction
women in Pakistan. Pain in lower back, leg cramps, night time cravings in any medium, provided the original author and source are credited.
for food and a family history of sleep disorder are conspicuous
BAOJ Gynaec, an open access journal Volume 2; Issue 3; 019
Citation: Naseem Ahmed, Aneeqa Khan, Asra Waseem, Tooba Khan, et al. (2019) Prevalence of Sleep Disturbances During Pregnancy – A Page 2 of 8
Pilot Study. BAOJ Gynaec 2: 019.
revealed that 35.8% of women, who conceived suffered from sleep an interim of 1 month, which was concocted by Buysse et al at
disorders [4]. Pittsburgh in USA [10]. It contains items, which are 19 in number,
generating a total of 7 components. We obtained a global score of all
Variety of sleep disorders have been defined by Diagnostic and the 7 components. The poorer the sleep quality, the more the score
Statistical Manual of Mental Disorders (4th edition) and as well as increases. A global score more than 5 was labelled as poor sleep
by International Classification Of Sleep Disorder in Oxford book of quality. This cutoff point has good psychometric properties with a
psychiatry. Among them; insomnia, snoring, restless leg syndrome are diagnostic sensitivity of 89.6% and specificity of 86.5% in ascertaining
outlined repeatedly by pregnant women in a prospective cohort study good and poor sleepers [10].
carried out in Chicago [5]. Insomnia in pregnancy can be attributed
to physical illness (backache, nausea, hormonal changes, frequent Pregnant women who were diagnosed as having poor sleep quality
urination, and growth of fetus, inadequate respiration and increase in were inquired further to reveal the contributing factors. Therefore, our
their abdomen size as expounded in a Turkish survey [6]. Additionally, questionnaire also contains other relevant questions including whether
modern data brought out a clear picture of sleep disturbances during pain in lower back, frequent leg cramps, nausea, increased vomiting,
gestation that bred untoward pregnancy sequels which included frequent fetal movements, night awakenings due to frequent urination
preterm birth and intrauterine growth retardation [2]. Also there are and food cravings during pregnancy have disturbed the participant’s
details of cognitive deficits and anxiety disorders in the offspring [7]. sleep. It also inquired about nasal stuffiness, shortness of breath when
During pregnancy, sleep changes that occurred may not be reverted lying supine, heart burn, increase in waistline during pregnancy, any
to as it was before for years [8]. An analysis conducted in Lahore has recent life stress, previous abortions, miscarriages and complications
focused on restless leg syndrome among pregnant women, where the in previous pregnancies, anemia or decreased Hemoglobin before or
prevalence was found to be 22.5% [9]. In Pakistan, few researchers during pregnancy and family history of any sleep disorder which may
have investigated sleep disturbance during gestation. contribute to sleep disturbance.
With this pilot study we aimed at exploring the quality of sleep in one Participants were enrolled only after taking informed, verbal
of the biggest tertiary care teaching hospital in Pakistan. Our study consent. A face to face interview was conducted using a pre-coded
served three objectives, which included enumerating the commonness questionnaire. Translation of the questionnaire was done for the
of poor sleep quality during pregnancy, factors contributing to it and participants’ feasibility. In order to remove interviewer bias, the
relationship of perturbation of sleep and gestational trimester. interviewers were given training on how to ask the questions.
Material and Methods Statistical Analysis
Design and Sample Data was analyzed using SPSS version 24. Frequencies and
percentages were computed for categorical responses. Among the
This is a cross-sectional study, conducted with stratified random three trimesters, the disparity of sleep quality was revealed by using
sampling technique. The research was conducted at the outpatient one way ANOVA. Pearson coefficients were computed to outline the
department and ward of obstetrics and gynecology of Ruth KM Pfau bivariate associations. Independent sample t test was used to establish
Civil hospital Karachi, Pakistan in the duration from 15th December statistically significant relation between the probable factors and PSQI
2018 to 15th January 2019. The sample size for this pilot study was score. Overall, p value of less than or equal to 0.05 was considered
30. Recruited in this study were all the pregnant women attending statistically consequential.
gynecology and obstetrics outpatient department, who agreed to
partake in the study and were mentally sound to give informed Results
consent. Pregnant women with any obstetric complication, any prior
diagnosed psychiatric illness or sleep disorder were not included. General Characteristics
Instruments 30 pregnant women, aged between 18 and 37 (mean 24.07 years),
visiting the gynecology and obstetrics outpatient department during
Our questionnaire inquired about the participant’s demographic the study period enthusiastically participated in the survey of 30
details, gestational age and personal characteristics. We utilized participants, 1(3.3%) was in her first trimester, 5(16.7%) were in
the Pittsburgh sleep quality index (PSQI) questionnaire to assess their second trimester and 24(80%) were from third trimester. The
the participant’s sleep quality. PSQI evaluates the sleep quality over demographic details are summarized in Table 1.
BAOJ Gynaec, an open access journal Volume 2; Issue 3; 019
Citation: Naseem Ahmed, Aneeqa Khan, Asra Waseem, Tooba Khan, et al. (2019) Prevalence of Sleep Disturbances During Pregnancy – A Page 3 of 8
Pilot Study. BAOJ Gynaec 2: 019.
TABLE 1. DEMOGRAPHIC DETAILS OF PREGNANT WOMEN (N=30) Sleep Quality
VARIABLE N(%)
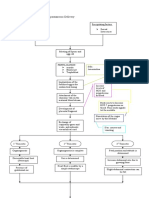
Global PSQI, individual component scores and their relations with
Pre pregnancy BMI
three trimesters quantified using one-way ANOVA are tabulated in
Underweight (BMI<19) 6 (20) Table 2. The mean score of global PSQI eventuated to be 6.43 ± 2.431,
Normal weight (19 25) 15 (50) with 16(53.3%) pregnant women being sorted as having poor sleep
Overweight (25 < BMI 6 (20) quality (PSQI > 5), illustrated in Fig 1. The only participant in her
Obesity (BMI > 30) 3 (10) first trimester scored less than 5. Besides, the women having poor
OCCUPATIONAL STATUS sleep in second and third trimester were 3(60%) and 13(54.16%)
respectively. However, no significant differences of global PSQI score
House wife 30 (100)
and it’s 7 components (subjective sleep quality, sleep latency, sleep
Part time job 0 (0.0) duration, habitual sleep efficiency, sleep disturbances, use of sleeping
Full time job 0 (0.0) medication, daytime dysfunction) were established with the three
GESTATIONAL AGE trimesters (p >0.05).
First trimester 1 (3.3)
Second trimester 55 (16.7)
Third trimester 24 (80.0)
SOCIOECONOMIC STATUS
Upper class 0 (0.0)
Middle class 23 (76.7)
Lower class 7 (23.3)
TYPE OF FAMILY
Joint 28 (93.3)
Nuclear 2 (16.7)
Fig. 1. Prevalence of sleep disturbances during pregnancy
TABLE 2. DISPARITY AMONG THREE TRIMESTERS AND THE PSQI SCORE
COMPONENTS AND GLOBAL SCORE GESTATIONAL AGE F P
Mean score First trimester Second Third
trimester trimester
(n=30) (n=1)
(n=5) (n=24)
Global score 6.43 2.431 3.00 6.40 1 6.58 5 1.047 0.365
Subjective sleep quality 1.40 0.770 0.00 1.40 1.46 1.818 0.182
Sleep latency 1.67 0.994 0.00 1.80 1.71 1.524 0.236
Sleep duration 0.43 1.00 0.20 0.46 0.938 0.404
Habitual sleep efficiency 0.10 0.00 0.00 0.13 0.386 0.684
Sleep disturbances 1.60 1.00 2.00 1.54 2.813 0.078
Use of sleeping medication 0.03 0.00 0.00 0.04 0.117 0.890
Day time dysfunction 1.20 1.00 1.00 1.25 0.180 0.836
In contrast to the second trimester, third trimester scores for all the Bivariate Associations
PSQI components were higher with the exception of sleep latency and
sleep disturbances. In contradistinction with the first trimester, the In order to point out the correlates of sleep quality in pregnant women,
scores of all the components with the exception of sleep duration were Pearson coefficients were reckoned as shown in Table 3. Though
reportedly higher in the third trimester. gestational age was positively correlated with poor sleep quality yet the
BAOJ Gynaec, an open access journal Volume 2; Issue 3; 019
Citation: Naseem Ahmed, Aneeqa Khan, Asra Waseem, Tooba Khan, et al. (2019) Prevalence of Sleep Disturbances During Pregnancy – A Page 4 of 8
Pilot Study. BAOJ Gynaec 2: 019.
result wasn’t significant enough to warrant a direct relation between Factors Contributing To Poor Sleep Quality
the two (p >0.05). Meanwhile, maternal age and BMI were not found
to be important determinants of poor sleep quality in this pilot study. Independent samples t test was used purposefully to reveal the
possible contributing factors of poor sleep quality, the results of which
TABLE 3. Correlation coefficients between quality of sleep and other are summarized in Table 4. In this pilot study, pain in lower back,
variables
frequent leg cramps, night awakenings due to increased food cravings
Variable r P and a family history of sleep disorders were entrenched as noteworthy
Maternal age -0.086 0.653 contributing factors (p≤0.05). The number of participants answering
Pre pregnancy BMI -0.170 0.369 in approval and disapproval for individual contributing factors, asked
Gestational age 0.133 0.483 in this survey is illustrated in Fig 2.
Table 4. Factors contributing to poor sleep quality
Contributing factors Mean difference t-test significance
Pain in lower back 2.50 2.4666 0.027*
Leg cramps 3.300 4.095 0.001*
Nausea and increased vomiting 1.945 1.715 0.108
Frequent fetal movements 1.945 1.715 0.108
Night awakenings due to food cravings 3.698 5.981 0.000*
Night awakenings to frequent urination -0.744 -0.506 0.620
Nasal stuffiness -1.718 -1.219 0.243
Heart burn -0.619 -0.536 0.600
Shortness of breath on lying supine -0.919 -0.698 0.497
Recent life stress/emotional upset -1.255 -1.044 0.314
Increase in waist line -2.214 -1.345 0.200
Anemia or decreased Hemoglobin 1.255 1.044 0.314
Previous abortions or miscarriages 1.375 1.254 0.231
Family history of sleep disorders 3.357 2.236 0.042*
Complications in previous pregnancy -0.711 -0.535 0.602
Fig. 2. Possible factors contributing to poor sleep quality
BAOJ Gynaec, an open access journal Volume 2; Issue 3; 019
Citation: Naseem Ahmed, Aneeqa Khan, Asra Waseem, Tooba Khan, et al. (2019) Prevalence of Sleep Disturbances During Pregnancy – A Page 5 of 8
Pilot Study. BAOJ Gynaec 2: 019.
Discussion among the three trimesters meticulously.
Pregnant women face marked deterioration in sleep quality during Several researchers have outlined backache, urinary frequency,
pregnancy [11-20].This may even lead to undesirable outcomes. Poor spontaneous awakenings, fetal movements, increase in the abdomen
sleep quality can result in pre-term birth, gestational hypertension and size, leg discomfort and heart burn as conspicuous factors contributing
cesarean section deliveries [21,22]. It can also influence birth type, birth to poor sleep [6,12,13,15,18,44-45]. This pilot study has also addressed
weight, labor length and Apgar score inimically [23]. Pathogenesis of such relevant factors. As a result, among 16 participants, identified
adverse pregnancy outcomes is directly related to inflammation [24- as poor sleepers, 75% complained of having pain in lower back,
27]. Raised levels of inflammatory markers (IL-6, TNF alpha, and 62.5% had frequent leg cramps, 43.75% woke up at night due to food
CRP) were found to be associated with sleep disordered breathing and cravings and 12.5% had a family history of sleep disorders. The above
short sleep duration [28-31]. Sleep disorders increase inflammatory mentioned complains of participants had a statistically consequential
and oxidative stress which damages the endothelium and deranges relation with Poor Sleep Quality score (p≤0.05). Other participants
metabolism resulting in hypertension or diabetes mellitus type 2 [32- also complained of nausea and vomiting, frequent fetal movements,
35]. Besides that pregnant women also go through excruciating labour night awakenings due to frequent urination etc. which might have
pain due to lack of sufficient sleep [36, 37]. contributed to poor sleep quality. However, no statistically significant
relation was established with PSQI score.
The prevalence of sleep problems in our pilot study came out to
be 53.3%. Among which the three trimesters proportioned out to Limitations and Future Recommendations
be 0.00%, 54.16% and 60% in order. Mindell JA et al reported that
third trimester has increased incidence of poor sleep quality and The pivotal strength of this study lies in its disclosure of widespread
our results are fully assertive to their study [17]. Schweiger MS et presence of sleep deprivation throughout pregnancy and responsible
al and Suzuki Set al have mentioned in their publications that sleep etiologies that can be managed by adequate counseling during prenatal
quality declines during the first trimester and returns back to normal visits. However, they were some limitations. We didn’t find any such
in second trimester, although 19% of participants still continue to questionnaire that could have been implicated in the gestational period
experience perturbed sleep [18,19]. In contrast to their findings, this alone. Several hormonal changes occur during this period including
pilot study reveals that the global scores of PSQI and its components a surge in estrogen level which decreases REM sleep duration and
with the exception of sleep duration are interestingly higher in second exogenously administered progesterone which results in lengthening
trimester as compared to the first, yet the findings seen were from a of non REM sleep [38]. Therefore, we suggest that there is a dire need
small sample size; therefore, the interpretation is, at best, preliminary. of devising such a questionnaire. Furthermore, multiparous women
Future studies in Pakistan should bring into account problems having children less than 1 to 2 years felt confused in analyzing
including insomnia [38], narcolepsy, sleep disordered breathing their sleep adequately because some of them scheduled their sleep
[39], restless leg syndrome [40] etc. which are frequently prevalent in according to their responsibilities towards their family which may
pregnancy [5]. have fabricated the results to some extent. This issue has also been
highlighted by previous researchers, who found it difficult to interpret
Yang Y et al reported that maternal age and gestational age is the results because of factors in the milieu (for instance, a crying baby)
positively correlated with poor sleep quality [8]. Moreover, Hedman [38]. Thus, future researchers are still needed to address this issue.
C et al and Hutchinson BL et al outlined BMI as an important factor
contributing to poor sleep [41,42]. Nevertheless, in this pilot study The prevalence of sleep disorders in this pilot study numbered 53.3%.
only gestational age was positively correlated but the result wasn’t This is sufficient enough to deduce that it is a common problem during
significant enough to merit discussion. On the contrary, no substantial pregnancy in Pakistan. Therefore, we advise that medical personnel
relation was established between maternal age and BMI in this survey. should heedfully address sleep problems and deliver sufficient guidance
Study conducted by Okun ML et al discovered that third trimester during antenatal checkups. Conservative interventions are frequently
had remarkable deteriorations in sleep quality when contrasted with effective as shown in several studies. This includes improving sleep
first and second trimester [43]. The results of this pilot study are hygiene, avoiding caffeine, practicing yoga and meditation techniques,
consistent with their findings. Poorer global sleep quality, subjective sound proofing of bedroom, limiting liquid diet after evening to
sleep quality, daytime dysfunction and habitual sleep efficiency were reduce nocturnal urinary frequency, application of liniments and heat
observed in third trimester as indicated by higher scores in table 2. pads and managing low back pain with massage, local heat and pillow
However, neither the global score nor the individual components were support [46,47].Techniques to control stimulus, such as getting out
significantly correlated with the three trimesters (P>0.05). Thus future of bed in the event of prolonged awakenings and going to bed only
researches are still needed to explicate the divergence in sleep quality when sleepy, using the bed only for sleep are try worthy [48]. When
BAOJ Gynaec, an open access journal Volume 2; Issue 3; 019
Citation: Naseem Ahmed, Aneeqa Khan, Asra Waseem, Tooba Khan, et al. (2019) Prevalence of Sleep Disturbances During Pregnancy – A Page 6 of 8
Pilot Study. BAOJ Gynaec 2: 019.
these conservative measures are unable to work, the pharmacologic 5. Facco FL, Kramer J, Ho KH, Zee PC, Grobman WA (2010) Sleep
agents of choice are diphenhydramine or zolpredem, both of which Disturbances in Pregnancy. ObstetGynecol 115(1): 77-83.
are category B agents in pregnancy [49]. The authors also recommend
that future researches should take into account the individual sleep 6. KIzIlIrmak A, Timur S, Kartal B (2012) Insomnia in Pregnancy and
disorders and their relationship with the three trimesters. Factors Related to Insomnia. Sci World J 2012: 1-8.
Conclusion 7. Radhakrishnan A, Aswathy B.S, Kumar VM, Gulia KK (2014) Sleep
deprivation during late pregnancy produces hyperactivity and
In conclusion, the present study demonstrated that in the course of increased risk taking behavior in offspring. Brain Res 1596: 88-98.
pregnancy the prevalence of sleep problem turned out to be 53.3% in
8. Yang Y, Mao J, Ye Z, Zeng X, Zhao H, et al. (2018) Determinants of sleep
Pakistan. This issue should be addressed by the health care providers
quality among pregnant women in China: A cross-sectional survey.
for the wellbeing of both mother and her child. Current study appears
NursPalliat Care 2(3): 4-5.
to relate pain in lower back, leg cramps, food cravings during night
and family history of sleep disorders more strongly with poor sleep.
9. Shahzad MF, Aslam R, Fiaz R (2018) Prevalence of Restless Leg
These factors should be assimilated into a supportive template of
Syndrome in Pregnant Females. Pak.J.Med.Healthsci 12(1): 177-179.
sleep related antenatal care. In this study neither the PSQI score nor
the sleep components significantly related with the three trimesters. 10. Buysse DJ, Reynolds CF 3rd, Monk TH, Berman SR, KupferDJ (1989)
Nevertheless, third trimester had higher scores indicating decline in The Pittsburgh Sleep Quality Index: a new instrument for psychiatric
sleep quality. In addition to this, maternal age, gestational age and practice and research. Psychiatry Res 28(2): 193-213.
pre-pregnancy BMI didn’t establish any noteworthy relation with
worsening sleep quality. Hence, the empirical evidence is still scarce 11. Brunner DP, Munch M, Biedermann K, Huch R, Huch A, et al. (1994)
and further studies are needed to reach definite conclusions. Changes in sleep and sleep electroencephalogram during pregnancy.
Sleep 17(7): 576-582.
Acknowledgement
12. Driver HS, Shapiro CM (1992) A longitudinal study of sleep stages in
The authors would like to acknowledge and thank Dr Nusrat Shah, young women during pregnancy and postpartum.Sleep 15(5): 449-553.
who provided us acquaintance in this research by allowing us to
conduct the study in her department of gynecology and obstetrics 13. Hertz G,Fast A ,Feinsilver SH, et al.Sleep in normal late pregnancy.
and all the participants for giving their precious time to the study. Sleep 15(3): 246-251.
Furthermore, we would like to thank the Mr. Muhammad Arif&
Ms. Batool of Research Department of DUHS for their guidance and 14. KaracanI, HeineW, AgnewH, Albertario CL, Schulman H, et al.
support throughout the study. (1968) Characteristics of sleep patterns during late pregnancy and post
partum periods. Am J ObstetGynaecol 101(5): 579-586.
References
15. Lee KA, and DeJoseph JF (1992) Sleep disturbances, vitality and
1. Shariat M, Abedinia N, Noorbala AA, Raznahan M (2017) The fatigue among a select group of employed child bearing women. Birth
Relationship between Sleep Quality, Depression and Anxiety in 19(4): 208-213.
Pregnant Women: A Cohort study. J Sleep Sci 2(1-2): 20-27.
16. Lee KA, Zaffke ME, McEnany G (2000) Parity and sleep patterns
2. Palagini L, Gemignani A, Banti S, Manconi M, Mauri M, et al. (2014) during and after pregnancy. Obstet Gynecol 95(1): 14-18.
Chronic sleep loss during pregnancy as a determinant of stress: impact
on pregnancy outcome. Sleep Med 15: 853-859. 17. Mindell JA, and Jacobson BJ (2000) Sleep disturbances during
pregnancy. J ObstetGynecolNeonatNurs 29: 590-597.
3. Okun ML, Roberts JM, Marsland AL, Martica Hall, et al. (2009) How
disturbed sleep may be a risk factor for adverse pregnancy outcomes. 18. Schweiger MS (1972) Sleep disturbance in pregnancy. A subjective
Obstet Gynecol Surv 64(4): 273-280. sleep survey. Am J Obstet Gynecol 114(7): 879-882.
4. Zhang Y, Mai YB, Li WD, Xi WT, Wang JM , et al. (2016) Sleep quality 19. Suzuki S, Dennerstein L, Greenwood KM, Armstrong SM, Satohisa E,
and related factors among pregnant women in Xuzhou city. Chin J et al. (1994) Sleeping patterns during pregnancy in Japanese women. J
School Doctor 30: 11-13. PsychosomatObstetGynecol 15(1): 19-26.
BAOJ Gynaec, an open access journal Volume 2; Issue 3; 019
Citation: Naseem Ahmed, Aneeqa Khan, Asra Waseem, Tooba Khan, et al. (2019) Prevalence of Sleep Disturbances During Pregnancy – A Page 7 of 8
Pilot Study. BAOJ Gynaec 2: 019.
20. MindellJA, CookRA, Nikovolski (2015) Sleep patterns and sleep 32. Jelic S, Les Jemtel TH (2008) Inflammation, oxidative stress, and the
disturbances across pregnancy.Sleep Med 16(4): 483-488. vascular endothelium in obstructive sleep apnea.Trends Cardiovasc
Med 18(7): 235-260.
21. Okun ML, Schetter CD, Glynn LM (2011) Poor sleep quality is
associated with preterm birth. Sleep 34(11): 1493-1498. 33. Mullington JM, Haack M, Toth M, Serrador JM, Meier-Ewert HK
(2009) Cardiovascular, inflammatory, and metabolic consequences of
22. Sharma SK, Nehra A, Sinha S, Soneja M, Sunesh K, et al. (2016) Sleep sleep depriviation. ProgCardiovasc Dis 51(4): 294-302.
disorders in pregnancy and their association with pregnancy outcomes:
a prospective observational study. Sleep Breath 20(1): 87-93. 34. van Leeuwen WM, Letho M, Kariosola p, Lindholm H, Luukkonen
R, et al. (2009) Sleep restriction increases the risk of developing
23. Zafarghandi N, Hadavand S, Davati A, Mohesni SM, Kimiaiimoghadam cardiovascular diseases by augmenting proinflammatory responses
F, et al. (2012) The effects of sleep quality and duration in late pregnancy through IL-7 an sCd CRP. 4(2): e4589.
on labor and fetal outcome. J Matern Fetal Neonatal Med 25(5): 535-
537. 35. Zamarron C, Garcia Paz V, Riveiro A (2008) Obstructive sleep apnea
syndrome is a systemic disease: current evidence. Eur J Intern Med
24. Bartha JL, Romero-Carmona R (2003) Comino-Delgado R. 19(6): 390-398.
Inflammatory cytokines in intrauterine growth retardation. Acta
Obstet Gynecol Scand 82(12): 1099-1102. 36. Pan PH, Lee S and Harris L (2005) Chronobiology of subarachnoid
fentanyl for labor analgesia. Anesthesiology 103(3): 595-599.
25. Freeman DJ, McManus F, Brown EA, Cherry L, Norrie J, et al. (2004)
Short and long-term changes in plasma inflammatory markers 37. Beebe KR, Lee KA (2007) Sleep disturbance in late pregnancy and
associated with preeclampsia. Hypertension 44(5): 708-714. early labor. J PerinatNeonatNurs 21(2): 103-108.
26. Holcberg G, Huleihel M, Sapir O, Katz M, Tsadkin M, et al.(2001) 38. Santiago JR, Nolledo MS, KinzlerW, Santiago TV (2001) Sleep and
Increased production of tumor necrosis factor-alpha TNFalpha by sleep disorders during pregnancy. Ann Intern Med 134(5): 396-408.
IUGR human placentae. Eur J ObstetGynecolReprodBiol 94(1): 69-72.
39. Pien GW, Fife D, Pack AI, Nkwuo JE, Schwab RJ (2005) Changes in
27. Romero R, Espinoza J, Goncalves LF, Kusanovic JP, Friel LA, et al. symptoms of sleep-disordered breathing during pregnancy. Sleep
(2006) Inflammation in preterm and term labour and delivery. Seminin 28(10):1299-305.
Fetal Neonatal Med 11(5): 317-326.
40. Nikkola E, Ekblad U, Ekholm E, Mikola H, Polo O (1996) Sleep in
28. von Kanel R, Dimsdale JE, Ancoli-Israel S, Mills PJ, Patterson TL, et multiple pregnancy: breathing patterns, oxygenation, and periodic leg
al. (2006) Poor sleep is associated with higher plasma proinflammatory movements. Am J Obstet Gynecol 174(5): 1622-1625.
cytokine interleukin-6 and procoagulant marker fibrin D-dimer in
older caregivers of people with Alzheimer’s disease. J Am GeriatrSoc 41. Hedman C, Pohjasvaara T, Tolonen U, Suhonen-Malm AS, Myllyla VV
54(3): 431-437. (2002) Effects of pregnancy on mothers’ sleep. Sleep Med 3(1): 37-42.
29. McDade TW, Hawkley LC, Cacioppo JT (2006) Psychosocial and 42. Hutchinson BL, Stone PR, Mc Cowan LM, StewartAW, ThompsonJM,
behavioral predictors of inflammation in middle-aged and older adults: Mitchell EA (2012) A postal survey of maternal sleep in late pregnancy.
the Chicago health, aging, and social relations study. Psychosom Med BMC Pregnancy Childbirth 10: 144.
68(3): 376-381.
43. OkunML, RobertsJM, Marsland AL, Martica H, et al. (2009) How
30. Meier-Ewert HK, Ridker PM, Rifai N, Regan MM, Price NJ, et al. disturbed sleep may be a risk factor for adverse pregnancy outcomes.
(2004) Effect of sleep loss on C-reactive protein, an inflammatory ObstetGynecolSurv 64(4): 273-280.
marker of cardiovascular risk. J Am CollCardiol 43(4): 678-683.
44. Baratte-Beebe KR,Lee K (1999) Sources of midsleep awakenings in
31. Shamsuzzaman AS, Winnicki M, Lanfranchi P, Wolk R, Kara T, et al. childbearing women. ClinNurs Res 8(4): 386-397.
(2002) Elevated C-reactive protein in patients with obstructive sleep
45. Fast A, Hertz G (1992) Nocturnal low back pain in pregnancy
apnea. Circulation105(21): 2462-2464.
:polysomnographic correlate. Am J ReprodImunnol 28(3-4): 251-253.
BAOJ Gynaec, an open access journal Volume 2; Issue 3; 019
Citation: Naseem Ahmed, Aneeqa Khan, Asra Waseem, Tooba Khan, et al. (2019) Prevalence of Sleep Disturbances During Pregnancy – A Page 8 of 8
Pilot Study. BAOJ Gynaec 2: 019.
46. Turton P (1980) Sleep and comfort during pregnancy and after birth. 48. Buysse DJ, Reynolds CF 3rd, Kupfer DJ, Thorpy MJ, Bixler e, et al.
Nursing (Lond) 20: 863-865. (1997) Effects of diagnosis on treatment recommendations in chronic
insomnia- a report from the APA/NIMH DSM-IV field trial. Sleep
47. Jacobs G, Benson H, Friedman R (1993) Home-based central nervous 20(7): 542-552.
system of a multifactor behavioral intervention for chronic sleep-onset
insomnia. Behavior Therapy 24(1): 159-174. 49. Briggs GG, Freeman RK, Yaffe SJ (1998) Drugs in Pregnancy and
Lactation. 5th ed. Baltimore: Williams& Wilkins.
BAOJ Gynaec, an open access journal Volume 2; Issue 3; 019
Você também pode gostar
- Mental HealthDocumento7 páginasMental HealthMirjana14Ainda não há avaliações
- Ifa Didaa OgbeDocumento1.256 páginasIfa Didaa Ogbemarco91% (54)
- Handbook For ASHA FacilitatorsDocumento72 páginasHandbook For ASHA FacilitatorsachintbtAinda não há avaliações
- Hematologic DisordersDocumento30 páginasHematologic DisordersUday Kumar100% (1)
- MCN Post Test IIDocumento14 páginasMCN Post Test IIquidditch07Ainda não há avaliações
- ABNORMAL ASSESSMENT OF NEWBORNDocumento7 páginasABNORMAL ASSESSMENT OF NEWBORNPriyaAinda não há avaliações
- Physiology of Normal Spontaneous DeliveryDocumento2 páginasPhysiology of Normal Spontaneous DeliverySummer Rain100% (2)
- Reproductive Health Strategic Plan 2007-2011Documento109 páginasReproductive Health Strategic Plan 2007-2011Nana Adwoa Animah100% (2)
- Articulo Peruano PDFDocumento10 páginasArticulo Peruano PDFStephanyChavezFeriaAinda não há avaliações
- Sleep Disorders in PregnancyDocumento11 páginasSleep Disorders in PregnancyLee Foo WengAinda não há avaliações
- Insomnia and Sleep Deficiency in Pregnancy: Cristina A ReichnerDocumento4 páginasInsomnia and Sleep Deficiency in Pregnancy: Cristina A ReichnerDevhy MazrianiAinda não há avaliações
- Association Between Maternal Sleep Practices and Late Stillbirth - Findings From A Stillbirth Case-Control StudyDocumento9 páginasAssociation Between Maternal Sleep Practices and Late Stillbirth - Findings From A Stillbirth Case-Control StudyWinniaTanelyAinda não há avaliações
- Maternal Sleep PracticesDocumento11 páginasMaternal Sleep Practicesatikha apriliaAinda não há avaliações
- Art:10.1186/1471 2393 14 337 PDFDocumento10 páginasArt:10.1186/1471 2393 14 337 PDF<_>Ainda não há avaliações
- Jurnal Tidur 10Documento8 páginasJurnal Tidur 10Ratrika SariAinda não há avaliações
- Effects of Exercise On Sleep Quality in Pregnant Women A Systematic Review and Meta-Analysis of Randomized Controlled TrialsDocumento10 páginasEffects of Exercise On Sleep Quality in Pregnant Women A Systematic Review and Meta-Analysis of Randomized Controlled TrialsAdrilia AnissaAinda não há avaliações
- Sleep Medicine: Jodi A. Mindell, Rae Ann Cook, Janeta NikolovskiDocumento6 páginasSleep Medicine: Jodi A. Mindell, Rae Ann Cook, Janeta Nikolovskitony montanAinda não há avaliações
- Sleep Disorder Article 9Documento11 páginasSleep Disorder Article 9hannahAinda não há avaliações
- Arafa2020 Article AssociationOfSleepDurationAndIDocumento5 páginasArafa2020 Article AssociationOfSleepDurationAndIAnanda Amalia SavitriAinda não há avaliações
- The Use of Acupuncture With in Vitro Fertilization: Is There A Point?Documento10 páginasThe Use of Acupuncture With in Vitro Fertilization: Is There A Point?lu salviaAinda não há avaliações
- Healthcare 11 01194Documento10 páginasHealthcare 11 01194Naga MuthuAinda não há avaliações
- PIIS0015028219324847Documento18 páginasPIIS0015028219324847Maged BedeawyAinda não há avaliações
- Tugas Review Jurnal Maternitas IiDocumento10 páginasTugas Review Jurnal Maternitas IiMahasiswa PEBRIANIAinda não há avaliações
- Meconium Aspiration Syndrome and Neonatal Outcome: A Prospective StudyDocumento6 páginasMeconium Aspiration Syndrome and Neonatal Outcome: A Prospective StudyAliza Raudatin SahlyAinda não há avaliações
- Anemia MaternityDocumento5 páginasAnemia MaternityBonaventura Ahardiansyah BoAinda não há avaliações
- Minor AilmentsDocumento14 páginasMinor AilmentsGazala100% (1)
- Original Research: Screening Extremely Obese Pregnant Women For Obstructive Sleep ApneaDocumento18 páginasOriginal Research: Screening Extremely Obese Pregnant Women For Obstructive Sleep ApneaappAinda não há avaliações
- Bersalin IngDocumento6 páginasBersalin IngIngca ClaudiaAinda não há avaliações
- 610 1853 1 SMDocumento12 páginas610 1853 1 SMMaria Angelika BughaoAinda não há avaliações
- Sleep, Evening Light Exposure and Perceived Stress in Healthy Nulliparous Women in The Third Trimester of PregnancyDocumento17 páginasSleep, Evening Light Exposure and Perceived Stress in Healthy Nulliparous Women in The Third Trimester of PregnancyYenie YenAinda não há avaliações
- Prevalence of pregnancy anxiety factorsDocumento4 páginasPrevalence of pregnancy anxiety factorsMahasiswa PEBRIANIAinda não há avaliações
- Hard Arson 2008Documento7 páginasHard Arson 2008elda zulkarnainAinda não há avaliações
- 10 1080@09513590 2020 1727879Documento10 páginas10 1080@09513590 2020 1727879angelAinda não há avaliações
- JCSM 11 8 869Documento9 páginasJCSM 11 8 869Andreas NatanAinda não há avaliações
- Lemmers Et Al-2019-Cochrane Database of Systematic ReviewsDocumento4 páginasLemmers Et Al-2019-Cochrane Database of Systematic Reviewsjuanda raynaldiAinda não há avaliações
- Prevalence of pregnancy anxiety factorsDocumento2 páginasPrevalence of pregnancy anxiety factorsMahasiswa PEBRIANIAinda não há avaliações
- Oxytocin MassaseDocumento8 páginasOxytocin MassaseJery PradilaAinda não há avaliações
- 4470-Article Text-33089-2-10-20211122Documento5 páginas4470-Article Text-33089-2-10-20211122Bianca Maria PricopAinda não há avaliações
- Daniel Scott, Fatima Elsayed, Joseph Wright, Inaki Moya, Grace CookDocumento28 páginasDaniel Scott, Fatima Elsayed, Joseph Wright, Inaki Moya, Grace CookINAKI MOYAAinda não há avaliações
- Development and Validation of A Pregnancysymptoms InventoryDocumento9 páginasDevelopment and Validation of A Pregnancysymptoms InventoryElenaAinda não há avaliações
- Differences in Vaginal Progesterone Provision Among Racial and Socioeconomic GroupsDocumento10 páginasDifferences in Vaginal Progesterone Provision Among Racial and Socioeconomic GroupsHerald Scholarly Open AccessAinda não há avaliações
- 10 1016@j PMN 2020 05 001Documento8 páginas10 1016@j PMN 2020 05 001Dzaki Prakoso RamadhanAinda não há avaliações
- HHS Public AccessDocumento16 páginasHHS Public AccessMahlina Nur LailiAinda não há avaliações
- Listening to Quran Recitation Reduces Anxiety in Pregnant WomenDocumento5 páginasListening to Quran Recitation Reduces Anxiety in Pregnant Womenfachrudin arrozaqAinda não há avaliações
- Sadeq Saad Abd El Moghny, Ahmed Kaid Allow, Belqees Ahmed and Bracamonte MaryamDocumento7 páginasSadeq Saad Abd El Moghny, Ahmed Kaid Allow, Belqees Ahmed and Bracamonte Maryamgamal attamAinda não há avaliações
- ijwh-5-501Documento7 páginasijwh-5-501MarianaafiatiAinda não há avaliações
- Sleep Disorder Article 1Documento34 páginasSleep Disorder Article 1hannahAinda não há avaliações
- Assessment of Perception and Management Practices of Pre-Eclampsia Among Pregnant Women in Southwest NigeriaDocumento7 páginasAssessment of Perception and Management Practices of Pre-Eclampsia Among Pregnant Women in Southwest NigeriaInternational Journal of Innovative Science and Research TechnologyAinda não há avaliações
- D'Souza-2019-Maternal Body Mass Index and PregDocumento17 páginasD'Souza-2019-Maternal Body Mass Index and PregMARIATUL QIFTIYAHAinda não há avaliações
- Aetiology of Infertility: An Epidemiological Study: National Journal of Community Medicine Volume 8 Issue 1 Jan 2017Documento5 páginasAetiology of Infertility: An Epidemiological Study: National Journal of Community Medicine Volume 8 Issue 1 Jan 2017vinnieAinda não há avaliações
- Risk Factors For Neonatal Asphyxia Occurrence at General Hospital Dr. M. Soewandhie, SurabayaDocumento6 páginasRisk Factors For Neonatal Asphyxia Occurrence at General Hospital Dr. M. Soewandhie, SurabayaFatimah FadilahAinda não há avaliações
- 418-Article Text-2672-1-10-20230110Documento5 páginas418-Article Text-2672-1-10-20230110aastoree1Ainda não há avaliações
- Antenatal Dexamethasone For Early Preterm Birth in Low-Resource CountriesDocumento12 páginasAntenatal Dexamethasone For Early Preterm Birth in Low-Resource CountriesMemento MoriAinda não há avaliações
- The Effect of Anemia On The Incidence of Premature Rupture of Membrane (Prom) in Kertha Usada Hospital, Singaraja, BaliDocumento7 páginasThe Effect of Anemia On The Incidence of Premature Rupture of Membrane (Prom) in Kertha Usada Hospital, Singaraja, BaliFirman AmalAinda não há avaliações
- CD005943 AbstractDocumento3 páginasCD005943 AbstractNuryn UridhaAinda não há avaliações
- Complementary Therapies in Clinical Practice: Semiha Ayd In Özkan, Gülay Rath FischDocumento6 páginasComplementary Therapies in Clinical Practice: Semiha Ayd In Özkan, Gülay Rath FischAlek OkeAinda não há avaliações
- AnesthEssaysRes124769-8259973 225639Documento5 páginasAnesthEssaysRes124769-8259973 225639Dica ArifiantiAinda não há avaliações
- 2012 Article 61Documento5 páginas2012 Article 61Al MubartaAinda não há avaliações
- Lit Review NealeDocumento9 páginasLit Review Nealeapi-726948535Ainda não há avaliações
- Cervical Effacement Associated with Faster Labor Progression in Nulliparous WomenDocumento12 páginasCervical Effacement Associated with Faster Labor Progression in Nulliparous WomenM Iqbal EffendiAinda não há avaliações
- Does Acupuncture Influence the Endometrium and IVF OutcomesDocumento7 páginasDoes Acupuncture Influence the Endometrium and IVF OutcomesdirkvandeweyerAinda não há avaliações
- Nop2 8 2345Documento9 páginasNop2 8 2345api-600421611Ainda não há avaliações
- Owais 2018Documento57 páginasOwais 2018Guillermo MoranteAinda não há avaliações
- Guidelines On 8 Key Evidence Based Practices During Labour - 353Documento35 páginasGuidelines On 8 Key Evidence Based Practices During Labour - 353National Child Health Resource Centre (NCHRC)Ainda não há avaliações
- Ijogr 6 4 466 468Documento3 páginasIjogr 6 4 466 468RachnaAinda não há avaliações
- Research ArticleDocumento11 páginasResearch ArticleErgyan 'Egy'Ainda não há avaliações
- Diminished Ovarian Reserve and Assisted Reproductive Technologies: Current Research and Clinical ManagementNo EverandDiminished Ovarian Reserve and Assisted Reproductive Technologies: Current Research and Clinical ManagementOrhan BukulmezAinda não há avaliações
- Pittsburgh Sleep Quality IndexDocumento4 páginasPittsburgh Sleep Quality IndexPutriPuputAinda não há avaliações
- Vol 29 No 3&4, July-December 2015 - Article - 07Documento24 páginasVol 29 No 3&4, July-December 2015 - Article - 07PutriPuputAinda não há avaliações
- Endorphin Massage and Pregnancy Exercise Relieve Back PainDocumento7 páginasEndorphin Massage and Pregnancy Exercise Relieve Back PainPutriPuputAinda não há avaliações
- Hangat Campuran Kencur Terhadap Edema Kaki Ibu Hamil Trimester Iii Di Wilayah Kerja Puskesmas I Wangon, BanyumasDocumento13 páginasHangat Campuran Kencur Terhadap Edema Kaki Ibu Hamil Trimester Iii Di Wilayah Kerja Puskesmas I Wangon, BanyumasFauziahAinda não há avaliações
- Endorphin Massage Reduces Childbirth PainDocumento8 páginasEndorphin Massage Reduces Childbirth PainPutriPuputAinda não há avaliações
- Function of SleepDocumento20 páginasFunction of SleepnopAinda não há avaliações
- A Review HypertensionDocumento7 páginasA Review HypertensionEditor IJTSRDAinda não há avaliações
- Case-Presentation Final Nagd Ni ShetDocumento7 páginasCase-Presentation Final Nagd Ni ShetMary Beth AbelidoAinda não há avaliações
- Population Geography: Demography and Global TrendsDocumento106 páginasPopulation Geography: Demography and Global TrendsMummy MasayuAinda não há avaliações
- Hypertension in PregnancyDocumento31 páginasHypertension in PregnancyradhabobbyAinda não há avaliações
- Leasson 4Documento11 páginasLeasson 4DARLYN DAYANA GARCIA VASQUEZAinda não há avaliações
- Nlex 1Documento4 páginasNlex 1Aileen AlphaAinda não há avaliações
- Maternal MidtermDocumento253 páginasMaternal MidtermTrishaAinda não há avaliações
- Paediatric NP FormDocumento2 páginasPaediatric NP FormBOWEN TLCAinda não há avaliações
- Test Bank For Healthcare Human Resource Management 3rd EditionDocumento37 páginasTest Bank For Healthcare Human Resource Management 3rd Editionsequelundam6h17s100% (11)
- Opinion Piece Navigating Indonesia's Abortion Debate With EmpathyDocumento2 páginasOpinion Piece Navigating Indonesia's Abortion Debate With EmpathyNiko SerafinoAinda não há avaliações
- قبالةDocumento88 páginasقبالةMostafa MahmoudAinda não há avaliações
- Antidepressants in Pregnancy and Breastfeeding PDFDocumento3 páginasAntidepressants in Pregnancy and Breastfeeding PDFTatenda BrunoAinda não há avaliações
- Panik Poli RS USU 6 April 2021 EDIT ANSDocumento77 páginasPanik Poli RS USU 6 April 2021 EDIT ANSRizkilbs LbsAinda não há avaliações
- NCP - Diabetes Mellitus Prepregnancy/GestationalDocumento13 páginasNCP - Diabetes Mellitus Prepregnancy/GestationalClaudine Christophe100% (1)
- Causes of MiscarriageDocumento7 páginasCauses of MiscarriageClaire Nimor VentulanAinda não há avaliações
- Case Study FormDocumento2 páginasCase Study FormAbhiramAinda não há avaliações
- Preterm BirthDocumento198 páginasPreterm BirthHoopmen tampubolonAinda não há avaliações
- Dwnload Full Foundations of Maternal Newborn and Womens Health Nursing 5th Edition Murray Test Bank PDFDocumento15 páginasDwnload Full Foundations of Maternal Newborn and Womens Health Nursing 5th Edition Murray Test Bank PDFroxaneblyefx100% (11)
- Presby Methotrexate Protocol For Ectopic PregnancyDocumento3 páginasPresby Methotrexate Protocol For Ectopic PregnancyTrina JoyceAinda não há avaliações
- Preterm Labor: Prevention and Nursing Management,: 3rd EditionDocumento59 páginasPreterm Labor: Prevention and Nursing Management,: 3rd Editionshaynie07Ainda não há avaliações
- Marriott's Employee Engagement Through Preventive HealthDocumento12 páginasMarriott's Employee Engagement Through Preventive HealthShakalya NagAinda não há avaliações
- Pregnancy Dialogue Between Midwife and MothersDocumento7 páginasPregnancy Dialogue Between Midwife and MothersziyanAinda não há avaliações
- Myths and Facts About Marijuana UseDocumento2 páginasMyths and Facts About Marijuana UseDyanie PlummerAinda não há avaliações