Escolar Documentos
Profissional Documentos
Cultura Documentos
Nursing Care Management
Enviado por
Stephanie Rae Baccay100%(1)100% acharam este documento útil (1 voto)
125 visualizações2 páginasAdolescent development, with heightened concerns about body image, should be considered. To compensate for side effects of same drugs, teenagers will often go on fad or starvation diets. Note areas for hyperpigmentation or depigmentation, depending on phase and type of disease.
Descrição original:
Título original
NURSING CARE MANAGEMENT
Direitos autorais
© Attribution Non-Commercial (BY-NC)
Formatos disponíveis
DOC, PDF, TXT ou leia online no Scribd
Compartilhar este documento
Compartilhar ou incorporar documento
Você considera este documento útil?
Este conteúdo é inapropriado?
Denunciar este documentoAdolescent development, with heightened concerns about body image, should be considered. To compensate for side effects of same drugs, teenagers will often go on fad or starvation diets. Note areas for hyperpigmentation or depigmentation, depending on phase and type of disease.
Direitos autorais:
Attribution Non-Commercial (BY-NC)
Formatos disponíveis
Baixe no formato DOC, PDF, TXT ou leia online no Scribd
100%(1)100% acharam este documento útil (1 voto)
125 visualizações2 páginasNursing Care Management
Enviado por
Stephanie Rae BaccayAdolescent development, with heightened concerns about body image, should be considered. To compensate for side effects of same drugs, teenagers will often go on fad or starvation diets. Note areas for hyperpigmentation or depigmentation, depending on phase and type of disease.
Direitos autorais:
Attribution Non-Commercial (BY-NC)
Formatos disponíveis
Baixe no formato DOC, PDF, TXT ou leia online no Scribd
Você está na página 1de 2
NURSING CARE MANAGEMENT
1. Patient education is started at diagnosis and continued at every
opportunity, repetition is good.
2. Family members are encouraged to call with questions and concerns.
3. Patients are advised to write down their questions so they are prepared
during the appointment.
4. Adolescent development, with heightened concerns about body image
and looking different, should be considered.
5. The nurse should be open about this; skin care, cosmetics, and
unobtrusive moisturizers with sunscreen and sun block should be
discussed.
6. Weight gain is an emotional issue, and it must be approached honestly
with a workable plan for family dietary changes and realistic exercise
program.
7. Prevention of infection includes hand washing (especially at school) and
pre procedure antibiotic coverage for routine events such as dental
cleaning.
8. To compensate for the side effects of same drugs such as corticosteroid,
teenagers will often go on fad or starvation diets.
9. School attendance may decrease because of loss of self esteem,
depression, feelings of inadequacy, or poor academic performance.
10. Adolescent need to understand what the function of each drug is, how
each drug helps to manage the disease, and what effect missing does
may have on their health.
11. Perform a thorough is systemic physical assessment, inspecting skin for
erythematosus rashes and cutaneous erythematosus plaques with an
adherent scale on scalp, face, or neck.
12. Note areas for hyperpigmentation or depigmentation, depending on the
phase and type of the disease and question patient about skin changes,
specifically about sensitivity to sunlight or artificial ultraviolet light.
13. Inspect scalp for alopecia and examine mouth and throat for ulcerations;
provide appropriate oral care.
14. Observe for edema and hematuria, indicative of renal involvement.
15. Direct neurologic assessment and identifying and describing central
nervous system involvement.
16. Question family members regarding behavioral changes, neuroses or
psychoses.
17. Assess knowledge of disease process and self management.
18. Assess patients perception of and methods of coping with fatigue, body
image changes, and other problems caused by disease. Assist patient to
develop effective coping strategies.
MEDICAL MANAGEMENT/ THERAPEUTIC
1. Corticosteroid are used topically for cutaneous manifestations.
• Have been the mainstay of SLE therapy
• Generally a dosage sufficient to control symptoms is prescribed and
then the dosage is tapered to the lowest level possible to achieve an
acceptable balance between disease activity steroid side effects.
2. Nonsteroidal anti inflammatory drugs (NSAIDs) are used with
corticosteroid to minimize corticosteroid requirements.
• Nurses need to instruct patient to take NSAIDs with food to help
prevent G.I side effects.
• Cyclophosphamide, a potent immunosuppressive agent, used in
combination with corticosteroids, is effective in treating proliferative
lupus nephritis and neuropsychiatric lupus. A detailed
cyclophosphamide education session should be held for patient
and family at which potential benefits and risks, including infertility
and future malignancy, are clearly stated.
3. immunosuppressive agents are generally reserved for the most serious
forms of SLE.
4. In addition to medication, treatment includes general measures such as
patient and family education, rest and exercise, proper diet, sun avoidance
and social support.
• Families also want to hear about the impact of SLE on growth and
development, childbearing, schooling and vocation.
• Diet, exercise and rest are the daily elements under direct patient
control.
• There is no specific SLE diet, but a balanced diet has does not
exceed caloric expenditure is essential for maintaining appropriate
weight on corticosteroid therapy.
• Given the frequency of photosensitive rash, the dangers of
excessive ultraviolet light exposure (including exposure to
uncovered fluorescent lights) needs to be stressed.
• One rule useful to share with the adolescent who may be
surrounded by peers who regularly seek out sun exposure is the
“slip, slop, slap” rule; slip on a shirt, slop on sunscreen and slap on
a hat before going in the sun.
• Social support from family, friends, teachers, counselors, and
professional social workers and therapist can help the child and
family through difficult times and promote adaptation to an illness
that is not going to go way.
Você também pode gostar
- JR DR ArifDocumento34 páginasJR DR Arifsukma nugrohoAinda não há avaliações
- Epilepsy Prevention PlanDocumento8 páginasEpilepsy Prevention Planzainab.bspsy1735Ainda não há avaliações
- Cure Eczema Naturally - The Key to Lifelong Healthy SkinNo EverandCure Eczema Naturally - The Key to Lifelong Healthy SkinAinda não há avaliações
- ABC of Palliative Care: Special Problems of Children: Clinical ReviewDocumento12 páginasABC of Palliative Care: Special Problems of Children: Clinical ReviewvabcunhaAinda não há avaliações
- Health and WellnessDocumento2 páginasHealth and WellnessGalvan VinAinda não há avaliações
- Fall Prevention: How Can Older Adults Prevent Falls?Documento4 páginasFall Prevention: How Can Older Adults Prevent Falls?Amalina ZahariAinda não há avaliações
- Concept of Health and IllnessDocumento28 páginasConcept of Health and IllnessCeline Eliz Ang86% (7)
- NCP Knowledge Deficit (FINAL)Documento8 páginasNCP Knowledge Deficit (FINAL)Nikki Ricafrente89% (9)
- 12 PsychiatricDocumento28 páginas12 PsychiatricamalAinda não há avaliações
- Chapter 16 School HealthDocumento6 páginasChapter 16 School Healthprincessbenito13Ainda não há avaliações
- Epilepsies in Children, Young People, and Adults: Summary of Updated NICE GuidanceDocumento13 páginasEpilepsies in Children, Young People, and Adults: Summary of Updated NICE GuidanceANDREWAinda não há avaliações
- Managing Sickle Cell Pain A Comprehensive Guide for PatientsNo EverandManaging Sickle Cell Pain A Comprehensive Guide for PatientsAinda não há avaliações
- CHN211 Week 8 WORD - Integrated Management of Childhood IllnessDocumento28 páginasCHN211 Week 8 WORD - Integrated Management of Childhood IllnessYrah Elaine SanchezAinda não há avaliações
- Conceptual Models 1Documento78 páginasConceptual Models 1Elaiza RiegoAinda não há avaliações
- Models of Prevention, Primary Health Care & Health PromotionDocumento51 páginasModels of Prevention, Primary Health Care & Health PromotionReshmi100% (3)
- GeriDocumento6 páginasGeriSetia BudiAinda não há avaliações
- Introduction To Critical Care NursingDocumento33 páginasIntroduction To Critical Care NursingIbrahim RegachoAinda não há avaliações
- Radiation TherapyDocumento1 páginaRadiation TherapyJayadi D. RaAinda não há avaliações
- Health Wellness and IllnessDocumento42 páginasHealth Wellness and IllnessTwesigye DeusAinda não há avaliações
- CHN QUIZ COMPIL - MergedDocumento8 páginasCHN QUIZ COMPIL - Merged2080315Ainda não há avaliações
- The Role of Psychotherapy in Paediatric OncologyDocumento18 páginasThe Role of Psychotherapy in Paediatric OncologyZainab Ali HassanAinda não há avaliações
- Systemic Lupus ErythematosusDocumento31 páginasSystemic Lupus ErythematosusJerilee SoCute WattsAinda não há avaliações
- Drug Education and Other Related Health Problems - PPTX CTU LTS 4TH WEEKDocumento28 páginasDrug Education and Other Related Health Problems - PPTX CTU LTS 4TH WEEKJannica CagangAinda não há avaliações
- Current Issues & Trends in Older: Persons Chronic CareDocumento12 páginasCurrent Issues & Trends in Older: Persons Chronic CareKeepItSecretAinda não há avaliações
- Breaking Free: Overcoming Anorexia and Body Image DistortionNo EverandBreaking Free: Overcoming Anorexia and Body Image DistortionAinda não há avaliações
- Nursing Care Plan For Alzheimer's DiseaseDocumento4 páginasNursing Care Plan For Alzheimer's DiseaseRnspeakcom100% (1)
- Mental Retardation Treatment and ManagementDocumento12 páginasMental Retardation Treatment and ManagementMelchoniza CalagoAinda não há avaliações
- Health and IllnessDocumento6 páginasHealth and Illnessmichaella pizarroAinda não há avaliações
- Nursing Diagnoses Arranged by GordonDocumento9 páginasNursing Diagnoses Arranged by GordonJoedeson Aroco BungubungAinda não há avaliações
- Ncar (Sr. Nerlyn)Documento9 páginasNcar (Sr. Nerlyn)nerlynAinda não há avaliações
- Introduction To Pedi PTDocumento36 páginasIntroduction To Pedi PTTitanium TssAinda não há avaliações
- Pharmacological Behaviour Management (Quite Fine) (Nellore)Documento82 páginasPharmacological Behaviour Management (Quite Fine) (Nellore)ultraswamy50% (2)
- Week 3 Nstp1 Drug EducationDocumento27 páginasWeek 3 Nstp1 Drug EducationAngelica ValdezAinda não há avaliações
- CHN Chapter 5 & 7Documento77 páginasCHN Chapter 5 & 7Kyla MoretoAinda não há avaliações
- CHRONICITYDocumento5 páginasCHRONICITYvavafo7699Ainda não há avaliações
- Anxiety: Generalized Anxiety Disorder Assessment (Behavioral Health) - CEDocumento7 páginasAnxiety: Generalized Anxiety Disorder Assessment (Behavioral Health) - CEircomfarAinda não há avaliações
- CHN NotesDocumento7 páginasCHN NotesRoy SalvadorAinda não há avaliações
- Nursing and End-of-Life CareDocumento26 páginasNursing and End-of-Life CareShafiq Ur RahmanAinda não há avaliações
- Rehabilitation-WPS OfficeDocumento3 páginasRehabilitation-WPS OfficeBetiy YitbarekAinda não há avaliações
- Medication Administration and Safety GeriatricDocumento4 páginasMedication Administration and Safety Geriatricapi-651287771Ainda não há avaliações
- MAPEH HealthDocumento8 páginasMAPEH HealthLenard CabradillaAinda não há avaliações
- Case Study:: CholelithiasisDocumento19 páginasCase Study:: CholelithiasisGillarhymesAinda não há avaliações
- Pedia Module Preschooler PDFDocumento11 páginasPedia Module Preschooler PDFRegine CuntapayAinda não há avaliações
- Elective II Group 1 Chronic IllnessDocumento31 páginasElective II Group 1 Chronic IllnessAldrine Albor Anyayahan IAinda não há avaliações
- Implement and Monitor Infection Control Policies and Procedure in CaregivingDocumento91 páginasImplement and Monitor Infection Control Policies and Procedure in Caregivingjessica coronelAinda não há avaliações
- Uself - Week 8Documento9 páginasUself - Week 8Bench RodriguezAinda não há avaliações
- EceincDocumento14 páginasEceincthebonafidebossAinda não há avaliações
- Application of OremDocumento12 páginasApplication of OremAnnapurna DangetiAinda não há avaliações
- 15 BDDocumento8 páginas15 BDmayanihAinda não há avaliações
- A Nursing Case Study On Myocardial Infarction: BSN 4G Group 1 Subgroup 2Documento29 páginasA Nursing Case Study On Myocardial Infarction: BSN 4G Group 1 Subgroup 2Ryann Chel L. QuismundoAinda não há avaliações
- Chapter 66 Critical CareDocumento26 páginasChapter 66 Critical Caredcrisostomo8010Ainda não há avaliações
- Rose-Morris Final EvalDocumento13 páginasRose-Morris Final Evalapi-242018884Ainda não há avaliações
- Assessment DementiaDocumento4 páginasAssessment Dementiaintanyuanita05Ainda não há avaliações
- Childhood Obesity SMJ-62-167Documento6 páginasChildhood Obesity SMJ-62-167abAinda não há avaliações
- Caring For Children Receiving Chemotherapy, Antimicrobial Therapy and Long-Term Insulin TherapyDocumento34 páginasCaring For Children Receiving Chemotherapy, Antimicrobial Therapy and Long-Term Insulin TherapyRubinaAinda não há avaliações
- GerontologyDocumento37 páginasGerontologysushilcspoonia3030Ainda não há avaliações
- Suggested Answers To Assignments, Chapter 42, The Child With A Psychosocial DisorderDocumento6 páginasSuggested Answers To Assignments, Chapter 42, The Child With A Psychosocial DisorderHannaAinda não há avaliações
- Principles of Community Health Intervention: Strategies For Identifying CausesDocumento20 páginasPrinciples of Community Health Intervention: Strategies For Identifying CausesAmerica BelloAinda não há avaliações
- Drug Education Program - : What Will You Learn From This Module?Documento2 páginasDrug Education Program - : What Will You Learn From This Module?Kimberly ManuelAinda não há avaliações
- Sle 2010-7Documento4 páginasSle 2010-7mahi_elsemary7011Ainda não há avaliações
- Acute Glomerulonephriti S: Group 3Documento25 páginasAcute Glomerulonephriti S: Group 3AradhanaRamchandaniAinda não há avaliações
- Assessment of Immune Function: Nurs 304: Adult Nursing LECTURER: Ms. MackeyDocumento103 páginasAssessment of Immune Function: Nurs 304: Adult Nursing LECTURER: Ms. MackeyEstherThompsonAinda não há avaliações
- Perniosis (Chilblains and HomoeopathyDocumento7 páginasPerniosis (Chilblains and HomoeopathyDr. Rajneesh Kumar Sharma MD HomAinda não há avaliações
- Editorial: Drug-Induced Rheumatic Syndromes: The Need To Be AwareDocumento2 páginasEditorial: Drug-Induced Rheumatic Syndromes: The Need To Be AwaredentsavvyAinda não há avaliações
- Systemic Lupous Erythematosus (SLE) Part 2Documento68 páginasSystemic Lupous Erythematosus (SLE) Part 2Power La Victoria Floro100% (3)
- Pyoderma Gangrenosum: A Clinico-Epidemiological Study: Date of Web Publication 2-Dec-2016Documento8 páginasPyoderma Gangrenosum: A Clinico-Epidemiological Study: Date of Web Publication 2-Dec-2016Sandara ParkAinda não há avaliações
- Systemic Lupus Erythematosus PDFDocumento4 páginasSystemic Lupus Erythematosus PDFsazaki224Ainda não há avaliações
- Minireview: C-Reactive ProteinDocumento4 páginasMinireview: C-Reactive ProteinFernando Amblódegui GarcíaAinda não há avaliações
- Estrella D. S. Bañez vs. Sss and de La Salle UniversityDocumento2 páginasEstrella D. S. Bañez vs. Sss and de La Salle UniversityAnne ObnamiaAinda não há avaliações
- Overlap Syndromes v2Documento32 páginasOverlap Syndromes v2JerryEddyaPutraBoerAinda não há avaliações
- SyphilisDocumento8 páginasSyphilisGandri Ali MasumAinda não há avaliações
- Dr. Horowitz VideoDocumento21 páginasDr. Horowitz VideoByron PerryAinda não há avaliações
- Mixed Connective Tissue Disease 2016Documento17 páginasMixed Connective Tissue Disease 2016Arleth DianaAinda não há avaliações
- AutoimmunityDocumento8 páginasAutoimmunityRachit NarangAinda não há avaliações
- Euroline Ana Profile 3 (Igg) Test InstructionDocumento16 páginasEuroline Ana Profile 3 (Igg) Test Instructionkholoud mohamedAinda não há avaliações
- Antiphospholipid SyndromeDocumento8 páginasAntiphospholipid SyndromeVijeyachandhar DorairajAinda não há avaliações
- Practice Test 1Documento10 páginasPractice Test 1Riin IrasustaAinda não há avaliações
- Immunopatho MCQ 2Documento21 páginasImmunopatho MCQ 2Ebenizer DestaAinda não há avaliações
- Drug Related Pleural Disease: Charis Moschos MD., Ioannis Kalomenidis MD E-Mail: Ikalom@Documento11 páginasDrug Related Pleural Disease: Charis Moschos MD., Ioannis Kalomenidis MD E-Mail: Ikalom@roland helmizarAinda não há avaliações
- Part 2 Exam Sample Q 2015Documento194 páginasPart 2 Exam Sample Q 2015Abdul QuyyumAinda não há avaliações
- Systemic Lupus ErythematosusDocumento64 páginasSystemic Lupus Erythematosusganga2424100% (1)
- AutoimmuneSolution FINAL PDFDocumento24 páginasAutoimmuneSolution FINAL PDFMihaela Gradinaru100% (6)
- SLE MedscapeDocumento49 páginasSLE MedscapeAndino FadilAinda não há avaliações
- MCQ IN DERMATOLOGY NMT 08 - مركز إبن الاسلام ... (20ebooks.com)Documento17 páginasMCQ IN DERMATOLOGY NMT 08 - مركز إبن الاسلام ... (20ebooks.com)R Ratheesh100% (9)
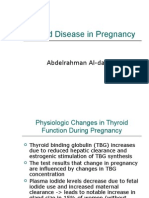
- Thyroid Disease in PregnancyDocumento36 páginasThyroid Disease in Pregnancypeni_dwiAinda não há avaliações
- Hypersensitivity Reactions BasicsDocumento101 páginasHypersensitivity Reactions Basicstummalapalli venkateswara rao100% (1)
- VN Shegal - Textbook of Clinical Dermatology, 5th EditionDocumento365 páginasVN Shegal - Textbook of Clinical Dermatology, 5th EditionAlbert Gheorghe93% (14)
- Vitamin D Benefits and RisksDocumento60 páginasVitamin D Benefits and Risksapi-393403647Ainda não há avaliações
- Problem Solving in LogyDocumento293 páginasProblem Solving in Logyveravero100% (2)