Escolar Documentos
Profissional Documentos
Cultura Documentos
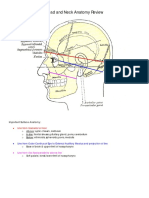
Anatomy Review
Enviado por
mmbrewDireitos autorais
Formatos disponíveis
Compartilhar este documento
Compartilhar ou incorporar documento
Você considera este documento útil?
Este conteúdo é inapropriado?
Denunciar este documentoDireitos autorais:
Formatos disponíveis
Anatomy Review
Enviado por
mmbrewDireitos autorais:
Formatos disponíveis
Contents:
Section 1:
Upper Extremity 1. Shoulder and Brachial Plexus
2. Humerus
3. Elbow 4. Forearm 5. Wrist and Hand i. Wrist
ii. Dorsal hand iii. Palmar hand
Section 11:
Abdominal wall, Pelvis and Acetabulum
Section III:
Lower Extremity 1. Hip joint 2. Thigh 3. Knee 4. Leg 5 . Foot and Ankle
Section IV:
Spine 1. Anterior Cervical Spine 2. Posterior Cervical Spine 3. Thoracolumbar Spine 4. Spinal Cord
Section I: Upper Extrem ity
The Shoulder and Brachial Plexus
Matthew A. Kippe, M.D. Osteology • Scapula o Angles
II II
Superior Inferior Medial Lateral Supraspinatus Infraspinatus Subscapularis
Borders
II
• o Fossa
II
.. .. o Spine o Coracoid Projects anteriorly and laterally from neck of scapula: at level of ' superior glenoid Important landmark for defining rotator interval and guide for shoulder arthroscopy o Acromion Bigliani and Morrison separate acromions into three types: • Type 1-flat undersurface • Typed2"j~cmt'$eclAlntletsurface
II II II
T)if>e"g~;'tHtl6k~drinder~urface
.. Liberson originally classified unfused acromial epiphyses (occurs approximately 1-2% population, 60% bilateral) • Pre-acromion ~, .. Mes-acrornion • Met-acromion
•
o
Basi-acromion
Supraglenoid tubercle o Glenoid Cavity Pear shaped Concave articular surface ·,bve[£lge 4-12 degrees of retroversion of the articular surface • Deepest portion of the glenoid articular surface lies within5mm of the lateral base of the coracoid" Avg superioinferior dimension of the glenoid is 39mm and is wider in the inferior anteroposterior dimension (avg 29mrn) than the superior anteroposterior dimension (avg 23nun) o Scapular Notch • Medial to base ofcoracoid • Spanned by transverse scapular ligament
II II II
Suprascapular nerve goes under the ligament and artery goes over the ligament (army goes over the bridge, navy under the bridge) o Origins of: .. Suprapinatus Infraspinatus Deltoid Omohyoid Long head triceps • Long head biceps Teres major Teres minor Coracobrachialis • Short head biceps .. Subscapularis Latissimus dorsi o Insertions of: Pectoralis minor • Serratus anterior Levator scapulae .. Rhomboid major and minor .. Trapezius o Blood Supply .. Derived from vessels that take fleshy origin from the scapula .. Conununicate freely with intramedullary vessels • Nutrient artery enters in the lateral scapular fossa or infrascapular fossa' .. Subscapularr-suprascapular, circumflex scapular, and acromial arteries are contributing-vessels o Fractures Well protected, covered by muscle, require significant energy to fracture. Mustr/o other injuries" • Indications to fix: • Significantly displaced acromion fracture with severe subacromial encroachment " • Glenoid fossa and fracture dislocations, glenoid neck fractures wi~hsignificant. displacement• Floating shoulderwith glenoidneck.fracture o Anomalies -Sprel'igel 's Dreformif)A .. undescended/congenital high scapula. • May have cartilaginous/fibrous union to spine = omovertebral bone which connects scapula to the C6 spinous process Shoulder girdle musculature is usually defective, the trapezius being most often affected .. Associated anomalies = fusion of ribs, cervical ribs, Klippel-Fei] syndrome, congenital scoliosis, syringomyelia' ~ Cv<r~~ rH"
II Ii Ii! Ii Ii Ii Ii Ii 11 III III fIi II
(s-I':" o f
t/"'l4-~
/{g...
"ft
J.-ce/vl~..(
7
5~u..~ ~";lc-l/o v hl\(~[r..:.e( V C-),
Scapular winging Serratus Anterior winging • Long thoracic nerve - ventral rami of 05-7" travels beneath plexus and clavicle over first rib and along lateral chest wall • Serratus ant. critical in maintaining proper scapulohumeraI rhythm during glenohumeral movement, particularly ann elevation, serves to upwardly rotate and protract-the scapula • Causes - blunt trauma, stretching during sports, repetitive industrial use of shoulder, positioning during anesthesia, neuritis, C7 radiculopathy • Scapula assumes position of superior elevation and medial .translation and the inferior pole is rotated medially, vertebral" border of scapula becomes prominent as it no longer is opposed to the thoracic cage' • Posterior periscapular pain and shoulder girdle fatigue as other periscapular muscles try to compensate" • Difficulty with ann elevation above 120deg, which will magnify degree of winging • Dx-EMG • Tx - N on-op = PT far ROM to prevent contracture, strengthening of peri scapular muscles most resolve within 6-9mo after trauma and 2years after viral or nontraumatic cause; bracing • Surgical options - scapulothoracic.fasion, dynamic muscle transfers, static stabilization procedures • Dynamic muscle transfers - Preferred is the pec. major transfer (sternocostal head) with fascia latagraft for extension, passed through inferior angle of scapula and tied back on itself
Trapezius winging
• '" • Spinal accessory nerve Shoulder·isdepressea and-the seapula-traaslated laterally wit.h the inferior angle rotatedlateially Pain and muscle spasm due to compensation with levator scapulae and rhomboids Secondary effects of winging = adhesive capsulitis, impingement, radi~ulitis from tractionon brachialplexus. Trapezius wasting, unable to "shrug.shoulder, weakness with FE andABD
• •
• Ox "'"'BMG • Tx - PT for
ROM, scapulothoracic fusion Eden ..Langeprocedure -le::yator scapulae, Rhomboids transferred laterally ,.....5crn ith small piece of medial scapular bone w
Rhomboid major and minor Rare • Innervated by dorsal scapular nerve (C5) Nerve passes through levator on its way to rhomboids .. C5 radio. or injury Winging similar to that of trapezius with scapula laterally translated and info angle rotated laterally (by pull of serratus) Tx = trapezius strengthening
II II II II
DDx: • Osteochondromas - pseudowinging Malunions of scapular fxs • Muscle abnl - congenital anomalies Scapulothoracic bursitis Secondary winging from disorders of the glenohumeral joint that produce abnl scapulothoracic dynamics'
II II II
Scapulothoracic articulation • There are two major (anatomic) bursae and four minor (adventitial) bursae • Major bursa • Infraserratus bursa - found in space between serratus" anterior muscle and the chest wan Supraserratus bursa ~ found between the subscapularis andserratusanterior muscles .~ Minor bursa Superomediaiangle of scapula - Infraserratus and SYR!£l,&~il!Ig~sibuT's·a t~e~!<:)~a.ngleQfscapula ~ Infraserratus bursa • Sp,in~9fs~>Clpula,-Trapezoid bursa = between medial spine of"s:tar;~lra,;~;~~pezius muscle' .: Scapulothoracic bursitis • Affects two areas: superomedial angle> inferior angle • Sx - pain with activity, audibJe>and palpable crepitus Tx - rest, ice, NSAIDs, PT, steroid inj, bursal excision (open vs. arthroscopic)
II II II II II
DDx
• • Osteochondroma Elastofibroma - snapping Scapula
Clavicle o First bone to ossify (membranous) and last physis to close (medial) o Osseous strut that connects the scapula to the thoracic cage through its articulation at the acromioclavicular joint and the sternoclavicular joint o Functions: • Frame for muscle attachment
Strut to guide scapulothoracic motion • Barrier to protect underlying neurovascular structures Congenital .Pseudoarthrosis • Failure of ossification of the acromial and sternal ossific centers .. Right clavicle primarily except in cases involving dextrocardia (10% bilateral) • May be due to exagg~r§:tyciarterial pulsation and pressure on thg clavicle by the subcla\Tiart artery .. PE: nontender swelling mid clavicle, neck asymmetry .. No functional disability, .. With fx will see pseudoparalysis of arm, pain with PROM and massive callus .. Ddx: cleidocranial dysostosis (s1..'1111,clavicle, scapula, pelviss " Rx: bone graft and plating 3..6 years :
II!!
'C
q~idocranial .. .. .. "
dysostosis , Deficient intramembranous ossification principally" a:tf~fting the clavicle, cranium and pelvis' Also affects the short tubular hones in the hands and feet ,AJ)'ttait Large head, small face, drooping shoulders, narrow chest,
Fractures .. Classification • Group 1: middle third (80% of all fractures) .. Group II: distal third o Subclassified into: " type 1 (interligamentous) .. type 2 (medial to CC ligaments) .. type HI (through articular surface of AC~ ioint with lizamentous disruntion) • type IV (displaced proximal segment with « CC Iigmarnents.still attached to' periosteum) • Group III: proximal third o Subclassified into: type 1 (minimally disp laceds, .. typ,e 2;.(.displaced with ligaments ruptured) .. typP,~,.,L~ITicularsurface of proximal third involved) • type 4 (epiphyseal separation in children and young adults of proximal third) • Xray: AP, 45 degreecephalic.tilt, CT scan when joint involved
"' "-' .L /
II
10
Proximal Humerus o Shaft C01U1ects ith ptoximal portion at the surgical neck, just below the w greater and lesser tuberosities o Anatomic neck above tuberosities, between articular margin of the head and the attachment of the articular capsule o Head inclined relative to the shaftl Su- 150 degrees o A vg. radius of curvature of humeral head > 24mm, avg. thickness 19rnm o The superior .articular surface of the HH lies -8-1 Omm superior to the highest point of the greater tuberosity o Lateral glenohumeral offset best defined from the lateral base of the coracoid to the lateral margin of the greater tuberosity which avgs 5457mm (can also use distance from lateral edge of acromion to lateral extent of GT whichavgs 17mm) o Center is offset approximately 6mm medially and 3 rom posteriorly from the axis of the shaft; retroversion between 20-30 degrees o Proxima1 humeral physis III Contributes to approximate1y,,&O% ofthelongitudinal growth of the upper extremity • 3 primary ossification centers • Hunaeral head • Greater tuberosity • L~s.s@f,tuberosity • "C~ai~sce between 5~7 years-to form proximal humeral physis .. Physis closes around 14-17'in ferri"tles and 16-18 males .. Periosteum stronger medially and pcstericrly .. Metaphyseal fractures displace anterior and laterally, physis is flexed, externally rotated and abducted to Tremendous remodeling potentia] o Blood Supply Ant~PQrcircun1flex artery: . • Primary,blooq: supply enters the lateral border of the intertubercular groove and terminates as the arcuate artery Posterior circumflex artery • Provides blood to small area of posterrnedial proximal humerus • Periosteal vessels from the rotator cuff
III II
Muscles • Scapulothoracic muscles o Trapezius .. Origin: medial superior nuchalline()~:pcfiput,ligamentum nuchae, all cervic:~L~nd thp1;~.9j:c:.yeI}f:lrl?tlftsp'inous processes and supraspinous ligaments ....'. .... .
II
Insertion: • Upper - distal 1/3 of clavicle '.
11
• • •
lower cervical/upper thoracic ~medial acromion and upper spine of.scapula • low thoracic - base scapula spine Action: retract scapula, elevate lateral angle Innervations: Sj:.l!~4Ji.,~SS~s.§>ory~CN also contributions from J;;I, C3,4 '" '......,·,~w,,·,'.' , ,. " ... .'
Vascular supply: superior (ascehdiag) branch of transverse cervical artery o RhomhoidS • Origin: • Minor; lower ligament of nuchae, spinous.pncoesssofC? and Tl • Maier: T2fii:.sn;mall.Siriiro'besseS" :J r • Insertion • Minor; medial scapulaat'baseof spine • M~jor; ll)~~i~!i;§;~~li?tu,J~;k~l~~:i$fl'iIl'eJ;(jnferior angle) • Action:'st:apu}aretractor, eleva'teitmedi,flJ,border • Innervation: dorsaLscapui.a.r'l1er;ve(C5), • Blood supply: dorsal scapular artery o LevatorScapulae • Origin: posterior tubercle spinouspreeessesC'l=l • Insertion: supericr.angleand .ID.~4,i~lbo~der f scapula to base of o spme • Action: elevate' superior angle of scapula • Innervation: dee.RQ[~P:QJ:!~~;.·;@(Q~if3jt,l,~Ir,~Hs"C3~4, scapular dorsal nerve C5 • Blood supply: dorsal scapular artery o SertaUlsAmterior ' • Origin: .lateral portionribs 1",9 • Insertion: meo,ia1 scapula.oostal.surface • Action: scapulaTprottaCiioU'an'd'upWard'rb1!li"Hon • Innervation: long thoracic nerve (C~6, 7) • Blood supply: iateraLtlyu:acic"artery o Latissimus Dors i • Origin: spinous processes of lower 6 thoracic vertebrae, spinous processes lumbar and sacral fascia (thoracic-lumbar fascia), aponeurosis from iliac crest, occasion slips from scapula and external oblique • Insertion: spira+s around and passes be!p\V t~re~.Il1aj()rint{) 11J.edial portion of interh.tberc~lar groqve (bu~sae and l~,t~J;l:h~~iiion~ • Action: adduction, internal rotation, and extension of ann • Innervation: tn'0raooGoTSal.nerve',C6,7 ,8) • Blood supply: thoracodorsal branch of subscapular artery
<';/j~~:'".";"~::~' i:·':::'-'
r-
'"-i.:_"~lwl.!
..~r-'~'
._,.
be~~~g"!~i~§:ii1'~Jo~
12
Deltoid
II
Origin:
., An!e:;rior; unipennate.Jateral
clavicle ....
., Miciqle,;}~w!4p~!l:flatY~@-f.fomion ..
II II:
• Post~ri~r;'u~ipeIlI:1ate~ spinQus process of scapula Insertion: all three converge to insert into deltoid tuberosity Action:
,F" •
Ap~:y"J.;i~H)t~,dMiddle:;,e1:eMatein.thescapular plane, flex sl1otl!4@l" withhelp.Jillompectof@-lis maj or and biceps tendon, however principal action is abduction .t.
•
" •
l:Jostyrior;ii}~.d-!lctlonand extens.iCll1
lIU1ervati;~'~' ~~jJl:~~:~~me.~Gj'·;;@~4,:;4;,5;cni);j.istalt9 acromion Blood supply: posteriorlmmeral.£1F.cnrnfle,>; and ,the deltoid branches of the thoracoacrornial artery Subclavius • Origin: cartilaginous portion of 1st rib .. Insertion: inferior surface of the middle 1/3 clavicle " Action: stabilize sternoclavicular joint during extensive activity • Innervation: nerve to subclavius C5 Blood supply: clavicular/pectoral branch ofthoracoacrornial artery Anomalous muscles: sternalis muscle, muscle of Albus
Ii
Rotator Cuff Muscles o,Supraspin.atus .. Origin: S14Pl<asP'~sru;s"f®.ss:a;i,and fascia Insertion: sj!:l.p'~r~;01·haIspect>efgreater.t:tW.~ro.sjty " Action: stabilizes glenohumeraljoint and as-,s.ists thedecltoid ,~J~v:a1ingthe ann " Innervation: sUFast;:~pti1ari1erve (C5,6) Blood supply: ~1,:1pr~capular,artery o ItiiFraspinatus .. Origin: iD.':fua.$'Pin:aws:~fassaand fascia Insertion: mi4fny,.,f~~t..qf greater tuberosity Action: pr4P'!:?C1;.;X!t~f;~m?1,rotator ofzhe shoulde:r.§,tabihze glenoburnetttij:(;);itl:tagainst posterior subl uxation
III II II III
in
..
(I
Innervation: SUEEt§;S,~.yJ~,i,!:1:erve (C5,6)
Blood supply: suprascapular artery and circumflex scapular artery
o4eresMinor
• .. .. •
II
(,'
Origin: mid to upper region of the axillary border of the scapula and infraspinatus fascia",: Insertion: ipferi.oI; facet of MI::.<lteruberosity t Action: external rotator Innervation: axillary-nerve (C5,6) Blood supply: posterior circumflex artery
13
Subscapularis • Origin: su1;>,~gapularfossa . • . Insertion: upper 2/3 inserts along lesser tuberosity and lower along the humeral metaphysic, deep to coracobrachialis and short fteaGofbiceps • Action: internal rotation, prevents anterior displacement humerus • Innervation: l,1pper.(C5,6) and lower(C5,6,7) subscapular nerves; lower; has more variation (60%fi-om an independent branch-of post. cord, 23% arose near origin of axillary n., 12% from the thp~aoodorsal n.) • Blood supply: SYP$9ff1:>l:IJ¥ a.X!c:'try, anterior circumflex humeral (upper portion) • Associated bursa • ~1uperior subscapularis bursa (recess) - is an.evagination.of the glenohumerai.joint that extends superiorly and anteriorly over the 'subscapularis mU$sle; this bursa does not\,c;€triil1iuhteaH~:iwifitffie;'sl1&abromial bursa .,s'llbpq]j?Coid bussa - below:qo[,+pgig.prQ,cess, between-the subsc<lpularis.t~JJqpnandc()njoinedtf;ndon;, .does not c0I'l1,Innnh:tatewi\tni~ffj biht"buthi~ywithsubacromial
lace
ba!J:1sa:'"
o
,,tk{l):tatcrr Interval
•
i,
Structures that contribute to interval = superior border of" subscapularis, inf~Ii{l)rbo:tder:0fi;supraspinat:lits,t;;QmC;9humeral iig~meIltj sup.eri@rglenonu];ri.'eraFTi'gamenf Divided into lateral and medial aspects .I;:;aterallateraJi'to articularclinHage~bone i' trl:lflsition; composed of :4 lay.ers(fromsuperficiai'to deep) o Sup.erficiaLfibers. QfCH ligament o Fibers.-co'fsijfjs¢apuIaris and supraspinatus o Deep.fltifets)o;ffCH ligament o S:u:p.erjOt:'glenohuIlleralligamentand capsule
M.edi§:Lrt::,;,:mrQ,;.l!J:Y¥fS·."
o
o
<;;g;U~spt
~HR~ti2£:;~J&.p:gh~mf:tr~li.g:;!m~EL~~joil}t capsule Common insertion of the CH and SGH ligaments onto lesser tuberosity form a 'reflection;puUey' which is a ligamentous sling that stabilizes the LH of the biceps.beforeit.enters.the groove
14
Rotator cuff Footprint .. The tendons of the spinati muscles join15mm proximal to their insertion • Anteroposterior insertions o Mean distances for the supra, infra, teres minor and subscap were 1.63, 1.64,2.07, and 2.43cm respective} y • Medial to lateral insertion width .' • At midpcrtion of supraspinatus is .14.7rnm • tvf~~1:lsfjf;supta, infra,. teres minor and subscapularis are 12.7, ..1,3..4, 1 L.4,. and 17.9mm respectively. ..
Other Shoulder Muscles o P'ec!for<i1isMaj'Or .. Origin: • Clavicle; .media] III .. Sternocostal; anterior 2/3 manubrium and sternum, ribs 2-6 (cartil aginous porti on) .. Insertion: .. 5 ern bila1'I1i!l;W tendon to lateral lip of bicipital groove. a11teriorto.tbe coracobrachialis and.biceps, blending with .·a,.n:I§f;!',Q)tc'edge.,(lI;f:.decltoi& .'. • The fibers of the two divisions Q9DXcerge and rotate 90deg Ot:lit~ yach ollieroeforeinsertingonto the humerus .. The upper clavicular head forms the anterior tendon insertion • Sternocostal head forms the posterior tendon insertion. .. The sternocostal head spirals on itself to produce the rounded appearance of the anterior axillary fold such that the most inferior fibers of the sternocostal head insert superiorly and posteriorly to the clavicular head and the . superior fibers insert inferiorly. • The anterior laminar fibers from the clavicular head are usually intact in acute ruptures 11 Action: primarily adduction and flexion of ann, secondary internal rotator Innervation: lateral pectoral nerve (C5-7)~ clavicular and upper sternocostal portions; medial pectoral nerve (C8~Tl), lower sternocostal and abdominal portions through pectoralis minor muscle; enter the muscle on the deep medial aspect .. Blood Supply: pectoral branch of thoracoacromial artery and perforators from internal thoracic artery, lateral thoracic artery • Poland's syndrome .. Common denominator is absence of sternocostal head of pestoralis major .. in most cases pee minor is absent-as well
:i,--:.:"-.,::·_,·,_,_. -" ,-_., .-.',,, ... ...• ' .
III
15
• •
• o PectoralisMinor • Origin: costal cartilage ribs 2-5 • Insertion: inner aspect of the.base of coracoid • Action: protracts and rqta,tes the scapula inferiorly • Innervation: medial pectoral nerve (C8, Tl) • Blood supply: lateral thoracic artery, pectoral branch of thoracoacromiaI artery o Teres Major • Origin: dorsal surface of scapula at the inferior agglftnear the ~illary border • Insertion: undergoes 180 degree rotation an inserts into medial lip of the intertubercular groove, medial to l~t • Action; internal rotation • Innervation: lowersubscapular nerve (C5,6) • Blood supply: branches of subscapular and thoracodorsal arteries o Biceps • Origin: Long head from supraglenoid tuberc1eand posterior superior aspect of the glenoid labrum / Short head from coracoid, with the coracobrachialis and pectoralis minor • Insertion: bicipital tuberosity of radius and bicipital aponeurosis (lasertus fibrosis) joins deep fascia over flexors and inserts onto ulna • Action: elbow supinator and flexor, shoulder flexor and abductor • Innervation: musculocutaneous nerve (C5,6) • Blood Supply: brachial artery o Coracobrachialis • Orgin: coracoid process • Insertion: anteromedial aspect of humerus • Action: flexor and adductor of arm • Innervation: musculocutaneous nerve penetrates I.S-8cm below coracoid (C5,6) • Blood Supply: brachial artery
.-'.'J,:;c·:"_··' ',_.",..... ,".
ipsilateral brachysyndactyly thought-to be due to interruption of embryonic blood", supply causing hypoplasia of ipsilateral subclavian artery assqc" with dextToG~dia " . ..
Pedicled Latissimus dorsi flap o Primary blood supply is thoracodorsal artery (comesoffof subscapular artery, average length of artery is BAcill1 o Innervated via thoracodorsal nerve (C7) corning off of posterior cord o 'tlleneurovascular pedicle enters the undersurface of the latissimus ~ 10 to ~. 12cm from the axilla o This allows harvesting the latissimus on a long pedicle for transfers o Restoration of elbow flexion = Zancolli 'flexorplasty', humeral insertion attached to coracoid and muscular origin woven through biceps tendon
Restoration of elbow extension = 'extensorplasty', humeralinsertionto posterior acromion and muscular origin woven through distal triceps tendon
Spaces • Quadrilateral Space o Defined superiorly by teres minor, inferiorly by teres major, by long head triceps medially and laterally by medial humeral shaft o Axillary nerve and posterior circumflex humeral artery traverse this space • Triangular Interval o Defined superiorly by teres major, medially by long head of triceps and laterally by lateral head of triceps o The radial nerve and profunda brachii artery and be seen in this interval (note these structures db not traverse the interval Traingular Space o Defined superiorly by teres minor, teres major inferiorly, and long head of triceps laterally o Circumflex scapular artery transverses this space
Superficial Anatomy: skin and fascia • Cape.Distribution .. Nipple T4 • Sternal.Angle T3/4" • Xiphosternal Junction T9 • Shqwclerc:3,4 o Mainly supraclavicular nerves, dorsal rami ofthe cervical spinal nerves, and sensory branches of the axillary nerve o Significant variation in courses of these nerves as well as overlapping .z;Qves.suppJied by the cutaneous nerves " Cutaneous nerves o Ventral primary rami (intercostal nerve] Lateral. cutaneous branch (twig) .. Anterior cutaneous branch (lateral mammary branch) • Medial cutaneous branch (twig) " Lateral cutaneous branch (media] rnanunary branch) o Above holds true for most of thoracic region except T1,2 and T12 .. TI: contributes to brachial plexus and has no lateral cutaneous branch .. T2: lateral cutaneous branch forms intercostalbrachial cutaneous nerve to proximal medial ann o Breast, blood supply: • Internal thoracic artery (perforating anterior cutaneous branches) .. Lateral thoracic artery Intercostal artery
II III
17
..
Fascia • Superficial.fascia: variable amount of fat, surrounds breast • Deep fascia: pectoral fascia surrounds pectoralis major and thickens to form floor of axillary space • Clavipectoral fascia; • Invests subclavius and pectoralis minor: • Costocoracoid membrane perforated by cephalic vein, lateralpec!m:;~>,!1e!ye"gI1q thoracoacromial artery • Blends with axillary floor as suspensory ligament of axilla, and with fascia of coracobrachialis and short head of biceps
Neuroanatomy • Brachial Plexus o All upper extremity motor except cervical plexus to levator scapulae and CNXI and cervical plexus to trapezius o Alll upper extremity sensory except supraclavicular nerves (cervical plexus) and intercostobrachial cutaneous nerve (T2-3) o Roots . • Ventral ram C5-TI, 62% from C4 Pre (22%) and post-fixed (1 %) plexus • Between anterior and middle scalene muscles• Grey rami (postganglionic) of sympathetic nervous system added' behind anterior scalene muscleo Trunks • Upper: ventralrami C5-6(Erb's point- junction of ventral rami and upper trunck • Middle: C7, • Lower:C&-Tl if
II
Divisions;
"' Anterior: pre-axial• Posterior: post-axial, posterior division ofC8and Tl , small to nonexistent Cords (named with respect to axillary artery) Posterior: from all three trunks (C5~Tl)" • Lateralsanterier'division' from uppei' and middle trunk (C5-C7) • M;~dial: ununited anterior division of inferior trunck (C8- T'l) TeiiHiba.l Branches "';,MedianNei,we: lateral' and medial cord contribute (C5- Tl)' • Motor: forearm flexors, thenars • sensory: radial hand • Musculocutaneous Nerve: lateral cord (C5-1J) • Motor; coracobrachialis, biceps, brachialis • Sensory: lateral antebrachial cutaneous nerve • Ulnar nerve: medial cord (C7 -Tl ) #' • Motor: flexor carpi ulnaris, ulnar Y2 flexor digitorum profundus, intrinsic muscles • Sensory: ulnar hand
ii' II
,c
'0
It
Radial Nerve: posterior cord (C5-8) • Motor: extensors of arm and forearm • Sensory: o Posterioranrebrachial cutaneous nerve o Posteriorbrachial cutaneous nerve o Lower lateral brachial cutaneous nerve ,A'j{t~le;{¥N erve: • posterior cord at lower border of subscapularis muscle • through quadrangular space and divides into anterior (superior) branch to deltoid, and posterior (inferior) branch which divides into branch to teres minor, superior lateral brachial cutaneous nerve and branch to post. deltoid (-80%) .. ant. and post branches separate anterior to long head of' triceps @§ o'clock position on the glenoid .. Anterior branch courses laterally toward surgical neck of humerus and lies -5cm inferior to anterolateral corner of acromion • Posterior branch - courses posteriorly along inferior glenoid rim for "--1 Omm before dividing into the superiorlateral brachial cutaneous nerve and the nerve to teres mmor .. Branch to teres minor lies directly on the joint capsule at level of glenoid rim, travels medially to enter muscle on its inferior surface • Superior-Lateral brachial cutaneous branch - pierces deep fascia at medial border of posterior aspect of deltoid .-.,,8.7cminferior to the posterolateral comer of the acromion " Branch to posterior deltoid - nerve lies -5cm directly inferior to posterolateral comer of the acromion (posterior deltoid is also supplied by branch of anterior branch of axillary nerve )"
Additional Branches .. Roots: e Muscular twigs to scalene muscles, longus cervicus C5 to phrenic nerve at lateral border anterior scalene .. Supraclavicular Branches .. Dorsal scapular nerve o From ventral rami C5 10 rhomboids and levator scapulae o Through middle scalene o Levator scapulae also innervated by C3 and C4 deep branches
19
Long Thoracic Nerve: .0 From C5,6,7 roots to serratus anterior o C5 and C6 branches join beneath the scalenus medius and join with branch of C7 caudally in the axillary region o In the supraclavicular region it has a trajectory parallel to the brachial plexus' o Enters axilla between axillary artery and anterior
scalene '
Nerve to subclavius: from upper trunk, descends anterior to subclavian artery and vein • Accessory phrenic nerve; from C5 • Suprascapular nerve o From upper trunk 9j~;6: 0% with contribution from 5 C4) to scapula~ notch under transverse scapular ligament to supraspinatus and infraspinatus o Suprascapular artery travels over the transverse scapular ligament o ~pinoglenoid ligament " , • Involved in entrapment neuropathy df suprascapular nerve • Insertions on scapular spine (-14mm) and, posferl:5raspectof the glenoid (-13.5m1n) • Has an irregular quadrangular shape • The distal branch of the suprascapular nerve and' the branches' of the suprascapular artery and.vein coursealong the base of the scapular spine below the ligament • Distance between ligament and nerve was ---4;,6:rrnn' Infraclavicular Branches • Lateral Pectoral Nerve:' o C5,6,7, lateral cord; anterior to axillary artery o Connects with medial pectoral nerve via loop o Pierces costocoracoid membrane to pectoralis major with pectoral branch of thoracoacromial artery • Medial Pectoral Nerve:" o From medial cord, e8,Tl o Through pectoralis minor o Across interpectoral space to pectoralis major • Medial Brachial Cutaneous Nerve: o From medial cord to medial distal arm • Medial Antebrachial Cutaneous Nerve o . From medial cord to medial forearm with basilica vein
20
Subscapular Nerve: o From posterior cord o Upper subscapular nerve to subscapularis o Middle subscapular nerve (thoracodorsal nerve) to latissimus dorsi o Lower subscapular nerve to teres major, some contribution to subscapularis,
Compression Syndromes - Thoracic Outlet Syndrome = Anatomy: occurs at thoracic outlet or 'under pectoralis minor .. Structures at risk = subclavian artery and VeL'1 and the brachial plexus; these 1\TV structures pass beneath the coracoid process and exit into axilla with pee minor anteriorly .. Etiology: • Congenital: cervical rib (0.5-1.0% of people) and fibrous bands-bifid clavicle ,; • Costocoracoid fascia (costocoracoid ligament); • Shoulder girdle droop • Trauma and edema: o Clavicle fractures' o Subacromial humeral dislocations o Crush injuries o Scaleneus spasm .. Scalenus and pectoralis minor hypertrophy • OA of 1sr costovertebral joint .. Syrntoms: (middle age female, right> left, poor muscle tone) .. Pain, paresthesias, numbness- most prominent sxs from neural compression, ulnar side of limb and two ulnar digits predominantly involved • Weakness o Ischemic complaints Signs .. Supraclavicular pain with palpation with radiation to little and ring fingers ,. Parathesias, worse with movement «> Hand weakness • Adson's maneuver: palpate radial pulse while patient extends neck, tilt chin up toward side, deep inspiration (elevates first rib) and downward traction on arm causes cool, pale forearm • "At attention test" - military position, shoulders back and downward compresses subclavian artery between clavicle and 1st rib
ItJ
21
.:
(0
•
II
Wright's hyperabductiontest - ann is abducted and ER, also have pt take and hold a deep breath; arterial compression by pee minor tendon Roo's test - overhead exercise test, pt flex and extends fingers with arms elevated; get fatigue and cramping within 30secs Venous distention, stasis changes
Work-up • • • Hand P Xray - chest Myelogram
• EMG • Arterio/venogram Treatment: Less common now because of increasing awareness of carpal tunnel syndrome and cervical disc disease and better response to shoulder strengthening; severe symptoms decompress by resecting offending structure; 1st rib resection by transaxillary approach, cervical rib resection by supraclavicular approach, pectoralis minor release DDx: • Shoulder hand syndrome - anterior subluxation of " glenohurneraljoint can produce symptoms of "dead arm syndrome" • Spinal cord tumors • Cervical disc disease • Cervical.spondylosis • Subclavian steel syndrome: subclavian artery block proximal to vertebral artery, shunt with exercise of arm and cerebral ischemicsymptomse Pancoast tumor • Ulnar nerve compression at elbow • Median nerve compression at wrist
Brachial Plexus Injuries • Closed: Varies from temporary paresis to midsubstance rupture to avulsion; traction injuries can cause widespread longitudinal neural and stomal disruption • Causes: o Most commonly head and shoulder being forced apart o Traction injuries to arm o With fractures, proximal humerus, scapula, rib, clavicle, transverse process of cervical vertebra
')')
,.
I)
Crutch palsy, post anesthetic/iatrogenic by inadvertent hyperabduction' o Obstetric brachial plexus injury Prognosis: o Root and avuIsion--------------no chance o C 5,6----~------ ------------- ------best o C5, 6, 7 ----------------~-----------intermediate o C7 ,8T I ---------------------------poor o Infraciavicular( closed)---------good o Iatrogenic----------------------good Classic syndromes o Erbspalsy: upper plexus, C5,6, +/-C7 (waiter's tip) .. Cant's abduct (deltoid-and supraspinatus) Can't ER.,,(infraspinatus and teres minor) .. Ca,n't .. upinate s • Diminished sensation over deltoid, lateral forearm, and hand with root avulsion lose serratus anterior and rhomboid o Klumpke.Jowerplexus, C8,Tl +/- Horner's " syndrome (miosis, ptosis, anhydrosis) with root o
II
a:YU1:sio rr
Radiation Therapy: DDx is ischemia vs. recurrent carcinoma/mets, difficult to explore Open Injuries: associated injuries often overshadow plexus lesions sharp trauma, high/low velocity GSW Evaluation of brachial plexus injuries Hand P Xray: Cspine, avulsion suggested with transverse process fracture, clavicle, greater stretch implied with fractures ., EMG: posterior rami affected? Myelogram - traumatic pseudomengingocele is presumptive of avulsion, done one month post injury as intradural bleeding can cause artifact " Histamine response: postganglionic lesion, no flare is good prognostic sign, lacks specificity a Exploration: controversial Indications for Surgery .. Acute-open-clean cut: • Primary repair may be possible blunt, repair, vessels first, and plexus add secondary procedure Closed: • Fractured clavicle, ORlF and secondary repair ofpJexus, expanding hematoma, explore and repair vessels, 2 repair ., Late: • No recovery 5-6 months, compression by callus or aneurysm, preogression of deficit or reversal of recovery
iii iii II II!
,0
Technique of Repair .. Neurolysis .. Neurraphy: Primary repair rarely possible • Nerve Grafting: sural, medial antebrachial, cutaneous, lateral femoral cutaneous', superficial branch radial • Neurotization: intercostals, eN IX, cervical plexus ,Obstetrical Brachial plexus injury • Incidence and prognosis: 0.1 %~O.4% of live births, upper plexus type greater than whole plexus greater than lower plexus .. Generally are postganglionic. injuries except with breech delivery where you see a preganglionic injury • Preganglionic injurys are cord avulsions, don't get motor recovery, to assess for this look for function of several nerves that arise close to the ganglions.Horners (sympathetic chain), elevated bemidiaphragm'(phrenic nerve), winged scapula (long thoracic n.), rotator cuff (suprascapular n.), rhomboids (dorsal scapular n-), latissimus dorsi (thoracodorsal n.). • If signs of recovery in first 2months get return of normal fxn • If no return by 3-6inonths worse prognosis, look for return of biceps fxn; likely need microsurgery • With lower plexus injury,'teildtoge1.,:r~ and ADD contracture - can do subscapularis release; also can do pee major release and transfer of latissimus and teres major to restore cuff; humeral derotational osteotomy .. Most recovery in first year, sensory more than motor .. High risk: large infant, breech ... With root avulsion: 70% useful sensory recovery, 33% useful
motor·
DDx:
• • • •
•
Fracture humerus; clavicle Proximal humeral epiphysis separation Acute osteomyelitis of humerus Septic arthritis shoulder In infants add: spinalcord tumor, CP, polio
o Brachial plexus neuropathy' • Idiopathic: acute painful monophasic illness • Clinical: 18'-40 year females; severe shoulder girdle pain, lasting days to weeks;xifollowed by onset of proximal weakness, most corrunonly involves serratus anterior muscle, subscapular muscle and axillary nerVe (parsonage-turner) •. • Prognosis: 90% recover in 2.. years J .. Treatment: PT, orthotic devices to prevent joint contractures
Vascular Anatomy • Axillary Region Boundries o Floor- axillary fascia o Anterior wall- pectoralis major and minor o Anterior axillary foId- pectoralis major o Posterior wall- subscapularis o Posterior axillary fold- teres maj or and latissimus dorsio Medial wall- serratus anterior o Lateral wall- humerus, intertubercular groove o Apex- convergence of clavicle, scapula, 1st rib • Axi 11ary Artery o S,ubclavian artery . - '. Ends at outer 1st rib • Brachial artery begins at lateral border of teres major Thyrocervical trunck: proximal to I st rib .. Suprscapular .. Transverse cervical artery deep( dorsal scapular artery) and superficiaJ branches to rhomboids and trapezius respectively o Divided into 3 parts by pe£tp[alis.l.11i:p.or" o Branches S-AL-SAP o Part 1:1 .. One branch behind costocoracoid membrane and behind medial cord, below axillary vein, crossed by loop between medial and lateral pectoral nerves = Superior thoracic artery to t and 2nd and 3rd intercostals muscles can arise from: .. Thoracoacrornial artery • Subclavian artery to Lateral thoracic artery o Part II: E Two branches, the cords ofthe brachial plexus are named with respectto their position near the axillary artery here, behind is subscapul aris: e Thoracoacromial artery through costocoracoid membrane into four branches deep to the clavicular head or pectoralis major muscle o Acromial branch o Deltoid branch- travels with cephalic vein o Pectoral branch- with lateral pectoral nerve o Clavicular branch • Lateral thoracic artery: o Variable, along axillary border of pectoralis to serratus may arise from thoracoacromial artery
III
25
o Part III:
• Three branches: anterior to teres major muscle, medial to coracobrachialis muscle, lateral to axillary vein, median nerve formed on it, is lateral to the medial brachial and medial antebrachial cutaneous nerves, anterior to radial and axillary nerves Subscapular artery: • Largest branch of axillary artery to subscapularis, teres major, and serratus anterior divides into: • Circumflex scapular artery at the triangular space (subscapularis, teres minor, teres major, long head triceps) • Thoracodorsal artery to angle of scapula and primary supply of latissimus dorsi with thoracodorsal nerve • Anterior humeral circumflex artery: • Small branch which travels inferior to subscapularis insertion • Posterior humeral circumflex artery: • Travels through the quadrangular space with axillary nerve and around surgical neck of humerus (teres minor, major, long head triceps, lateral head triceps)
Joints • Acromioclavicular Joint o Anatomy • Diarthrodial joint • 50% override of acromion and clavicle • Fibrocartilaginous disc which is either partial (meniscoid) or complete. Degenerates over time and virtually not functional beyond age 40 • Innervated by suprascapular nerve and lateral pectoral nerve .,. andcapsule restrain anterior to posterior motion, prevent horizontal instability • Superior AC ligament contributes approximately 56% resistance to posterior displacement of clavicle • Posterior AC ligaments contributes 25% resistance to posterior displacement of the clavicle • AC ligament ilisenion: ' • Posterior capsule 15.7mm • Ariter10rCapsule 9.5rnm .• Inferiorcapsule ,1.,2,9mm • Superior capsule 16.1 mm and greatest 20rnm • Superiorand Posterior ~igaments most important to preserve honzontal stabilitY witH distal clavicle excision
• AcromioClavicular ligaments
26
Ii
Coracoclavicular Anatomy: e Prime suspensory ligaments of upper extremity, prevents acromion from being driven down and underneath the clavicle o Trapezoid ligament: anterior and lateral to corac,~i~,;±'? trapezoid line of clavicle, lateral free edge is most anterior o Conoid Ligament: posterior arid medial coracoid to conoid tubercle of clavicle Injuries • Type 1: sprain of AC ligaments • Type 2: disruption of AC ligaments with sprain of CC ligamerits • Type 3: BothAC and CC ligaments disrupted (deltotrapezial fascia intact) • Type 4: AC andCC torn with clavicle through posterior fascia • Type 5: AC and CC torn with fascia perforated, severe displacement • Type 6: AC, +/- CC torn with inferior or subcoracoid displacement (associated with rib and chest wall injuries)
Sternoclavicular Joint o Anatomy: Diarthodial joint, incongruous • Intraarticular disc ligament; from synchondral junction of rib 1 to sternum through SC joint superior and posterior aspect medial clavicle Costoclavicular ligament (rhomboid ligament): 1.3 em wid and thick into rhomboid fossa of clavicle; anterior component resists downward rotation and medial-displacement; posterior component resists upward rotation and Iateral displacement .. Interclavicular ligament "' Capsularligament (Beam) : most important structure in preventing upward displacement of the medial clavicle "' Medial clavicle epiphysis: last to close (ossification 20 years) fuses with shaft at 25-30 years, injury through joint may actually be physeal fracture o Dislocations: .. Posterior • Anterior • Xrays include AP, serendipity view(40 degree cephalic tilt aimed at manubrium: anterior dislocation above interclavicular line, posterior below .. CT scan
III II!
27
Glenohumeral Joint o Anatomy • Glenohumeral joint allows tremendous ROM, stability achieved by both static and dynamic restraints .e Static restraints include the glenohumeral ligaments, bony architecture and orientation, and negative intra-articular pressure • Dynamic stability factors include the rotator cuff, deltoid, long head of biceps, , and scapular rotators '
11
Labrum • Peripheral rim of tissue surrounding the glenoid • Fibrous tissue, with a fibrocartilaginous transition zone at its attachment to the articular cartilage e Superior and anterior. portions differ: o Superior and anterosuperior portions are loosely attached to the glenoid resembling meniscus in !mee o At 12:00 posi~i9Ilsynovial recess between superiorp'aif'oftabrum and glenoid rim o Inferior portion firmly attached and appears as a rounded fibrous elevation o IGHL intimately attached to both the glenoid rim and the labrum • Vascular supply from branches of suprscapular artery, the circu,mflex branch.of.subscapular artery, and posterior circumflex humeral artery • Branches from these capsular and periosteal vessels supply the glenoid through its peripheral attachment but not from the underlying glenoid bone • !ggen~~ml, Stg)~_tQr?D.g.~!1.J~rOSUp~DQrr~giQns of the tht:l labrum-are less vascular than the posterior and inferior portions • Labral Variants: o 1) presence of a sublabral foramen, defined as the sulcus between a well-developed anterosuperior portion of the labrum and glenoid articular cartilage CI 2) the presence of a sublabral foramen and a: cord-like middle glenohumeral ligament o 3) a complete absence of'Iabral tissue at the anterosuperior aspect of the labrum in association with a cord-like middle glenohumeralligmament attached to the superior part of the labrum at the base of the biceps (Buford complex).
Biceps origin variants: o Forty to sixty percent of the biceps tendon origin is from the supraglenoid tubercle, while the remaining fibers originate from the superior glenoid labrum. o Furthermore, there is considerable variability in the attachment to the superior labrum. The most common variation is an equal contribution of anterior and posterior labral attachment. o The next most common is attachment mostly posterior, but with a small contribution to the anterior labrum. o Third, consists of an entirely posterior attachment. Finally, labral attachment is mostly anterior, but with a small contribution to the posterior labrum . Labrum Pathology o Anteroinferior labral lesions (Bankart) o ALPSA (Neviaser)
o
.,
.,
II
SLAP
Type I: fraying and degenerative appearance of the superior labrum Type 2; detachment of the superior labrum from the supraglenoid tubercle can be anterior, posterior, or combined anterior/posterior .. Type 3: bucket-handle tear that displaced into the joint while biceps root remains stable Type 4: bucket-handle tear that propagates into the biceps tendon .. Type 5: anterior-inferior Bankart lesion that propagates superiorly to the biceps tendon Type 6: unstable flap tear of the labrum with separation of the biceps anchor .. Type 7: superior biceps-labral detachment that extends anteriorly beneath MGHL ., Type 8: SLAP extension along posterior glenoid labrum as far as 6 0' clock Type 9 : lesion is pan-labral SLAP extending the entire circumference of the glenoid or Type 10: superior Iabral tear associated with posterior-inferior labral tear (reverse Bankart) Exam: Active compression test, Crank Test, Jobe's relocation test, Speed's test, Resisted supination external rotation
II II
29
III
Glenohumeral Ligaments " Collagenous thickenings of the joint capsule • Static restraints, particularly important in end range of motion • Coracohumeral Ligament (CHL) o Structure: dense fibrous, 1-2 em wide, thin structure o Origin: lateal surface of coracoid process o Insertion: greater and lesser tuberosities adjacent to bicipital groove o Anatomic relationships: extra-articular, intermingled with the edges of the supraspinatus and subscapularis tendons; reinforcement of the rotator interval" o Functions: limits inferior translation and external rotation when the ann is adducted and posterior translation when the shoulder is in a position of forward flexion, adduction, and internal rotation • Superior Glenohumeral Ligament (SGHL) o Structure: variable in size o Origin: superior glenoid tubercle just inferior to biceps,tendon, o Insertion: superior aspect of lesser tuberosity 1l'le4i~ltobiceps groove o Anatomic relationships: intra-articular, lies deep to eEL; reinforcement of the rotator interval o Functions: limits inferior translation and, external rotation when the ann is adducted.and ~" posterior translation wh-en the shoulder is' in a position of forward flexion, adduction, and intemafrotation • Middle Glenohumeral Ligament (MGRt) o Structure: great variation in size and presence; absent or poorly defined in 40% of individuals, cgrg7pke, Buford complex o Origin: superior glenoidtubercle and" aD.;t~I9stJper;iorabrum, often along with SGHL l o Insertion: anterior to the lesser tuberosity o Anatomic relationships: can be sheetlike and confluent with the SGHL or cordlike with foraminal separation between it and the anterior band if the IGHL complex o Functions: passive restraint to both anterior and posterior translation when the arm is abducted range 60.;90 degrees in external rotation and .
30
..
limits inferior translation when the ann is adducted at the side Inferior Glenohumeral Ligament (IGHL) o Structure: consists of three components; anterior, posterior, axillary pouch; decreases in thickness from anterior to posterior o Origin: anteroinferior labrum neck of glenoid adjacent to labrum o Insertion: inferior to the MGHL at the humeral
neck
o Anatomic relationships: intra-articular, blending with the posterior aspect of the subscapularis tendon Functions: as a hammock of the humeral head; in adduction, it acts as a secondary restraint, limiting large inferior translations;' in abduction, it becomes taut under the humeral bead, limiting inferior translation; in internal rotation, it moves posteriorly, and in external rotation, it moves anteriorly, forming a barriers to posterior and anterior dislocation, respectively Capsule Structure: thinnest region of the joint capsule without discrete ligamentous reinforcements Origin: posterior abnd of IGHL€ posterosuperior labrum to the insertion of the biceps Insertion: posterior humeral neck Anatomic relationships: blends with the posterior aspect of the infraspinatus and teres minor Functions: limits posterior translation when the ann is forward, flexed, adducted, and internally rotated Classification: Number of factors • voluntary versus involuntary subluxation or dislocation • traumatic versus atraumatic injury • direction of instability • degree of instability • TtJBS/AMBRJ incorporate clinical presentation with treatment,
..
Posterior o o
o o
Instability
o
III
31
0,
III
Exam Anterior and Posterior Drawer, Load and shift, Apprehension test, Jobe's relocation test, Sulcus test
o Acute anterior dislocation • -High recurrence rate <20 years old Bony injuries include Hill Sachs lesion, glenoid and greater tuberosity fractures Nerve injury as high as 30%(axillary) • Soft tissue injuries include capsuloligamentous structures and possibly rotator cuff muscles o Recurrent traumatic dislocations: • Essential lesion: anteriorinferior labrum and , capsular detachement, Hill Sachs, glenoid rim
II III
eroSIOn
• • • Operative Repair Arthroscopic qpen 6 Capsular shift'
-0
Putti -Platt
o Magnuson stack o Bone-Block: Eden-Hybbinette iliac graft to anterior glenoid rim ',,0 Bristow-Laterjet o Posterior Dislocation • 1.5% of all dislocations Direct blow, electric shock, seizure Signs: fixed adduction and IR, blocked ER, flatter anteriorly, rounded posteriorly, coracoid more obvious I:Ha~ose on axillary view, CT scan o Inferior Dislocation (Luxatio erecta) More common than superior • HYJl~abduction o Superior Dislocation • Rarest • Extreme force to adducted ann • Fracture common • Bewareiof Nv injuries o , Snapping Shoulder DDx: Biceps tendon subluxation Anterior subluxation • Labral tear Osteochondral fragment
III III III III III II II
32
Approaches to the Shoulder o Anterior = Deltopectoral Incision - straight incision from above and just lateral to the coracoid process extending distally following line of deltopectoral groove toward deltoid insertion IN? between the deltoid (axillary n.) and pec. major (medial and lateral pectoral nerves) Identify cephalic vein, and move medial or lateral, receives more branches from the deltoid .. Incise clavipectoral fascia lateral to muscular portion of coracobrachialis muscle and bluntly release adhesions under conjoined tendon and deltoid " Proximal 2cm of pec. major tendon insertion is released (protect LH biceps tendon running deep to pee major insertion) .. Leading edge of CA ligament can be excised to improve exposure to subacromial space Next release the subscapularis tendon from its insertion. The anterior humeral circumflex artery and it two accompanying veins run along the inferior border of the tendinous portion of the subscapularis and require ligation The axillary nerve runs under the muscular portion of the subscap on its way to the quadrilateral space, with increased ER of the humerus the nerve is drawn medially away from the dissection " Release needs to go past 6 o'clock position to allow adequate release for anterior dislocation o 1\nterolateral .. Incision - transverse, from anterolateral of acromion to just lateral to coracoid process Incise deep fascia in line with skin incision .. Deltoid is split in line with its fibers starting AC joint .. Deltoid is detached by sharp dissection from AC joint laterally to expose 1em of acromion leaving a cuff of tissue that will need to be reattached to the acromion through drill holes The CA ligament is exposed after retracting the edges of the deltoid o Lateral .. For mini-open rotator cuff repair Longitudinal incision made from tip of acromion Scm down lateral ann .. Deltoid is split in line with its fibers, no more than 5cm to avoid injury to axillary nerve .. Win come down on subacromial bursa which is excised giving exposure to supraspinatus tendon
III II II OJ II lOr OJ III
33
Posterior Linear incision along scapular spine to posterior corner of the acromion Detach origin of deltoid on scapular spine, plane between deltoid and infraspinatus easier to locate at lateral end of incision • Define INP between infraspinatus and teres minor by blunt dissection Retract infraspinatus superior and teres minor inferior to reach posterior glenoid and neck of scapula
II II II
Rotator Cuff Disease o General: ., There is evidence that the hypovascular zone in the distal end of the tendon is actually hypervascular in patients with impingement • Apoptosis as a possible etiologic factor, cyclic strain at high level of intensity and duration triggers protein kinases which influence regulation of apoptosis • Even in the presence of a symptomatic ReT pain relief and inc' ROM can be achieved in up to 50%" • Symptomatic tears that involve more than 50% of the width should be repaired, more than 6mm of footprint exposure suggests a 50% full-thickness loss • Margin convergence: done via longitudinal side to side closure of the leaves of the tear to decrease the strain on the lateral margins of the tear internal impingement in throwing athletes, • Injuries found usually include superior glenoid labral tears and articular-siciedPTRCT" • Caused by primary impingement of the undersurface of the posterior supraspinatus against.the superiorglenoid as the ann is brought iuto horizontal abduction and ER irr throwtng' • Two proposed mechanisms: Acquired ant microinstability caused by stretching of the ant capsule allowing the' glenohumeral articulation to move into a hyperangulation position of inc ER and-horizontal ABD; Acquired glenohumeral IR .deficit (GIRD) created by progressive contracture of the post glenohumeral.capsule and dec static and dynamic flexibilityofthe post shoulder muscles; this creates a superior .shift in the glenohumeral contact point so that when you ABD and ER around the new contact point shear forces at the biceps anchor and posterosuperior labrum increase through an excessive peel-back action of the biceps on the labrum producing a post glenoid labral lesion, also are inc shear and torsional forces on the rotator cuff
II
II
II
External imDlngement in throwing athletes • Different than that seen in older pts, which is thought to be due to alteration in subacromial space (primary impingement) Secondary external impingement (intra- or extra-articular) • Intra-articular causes such as anterior instability, superior labral tears or biceps injury, all decrease the concavity/compression effect of the hume~s on the glenoid and allow superior humeral translation with impingement; Non-articular causes involve muscle weakness and/or inflexibility (such as alteration in the scapular.stabilizers)
Shoulder exam: • ROM - ABD= 180deg(2: 1 glenohumeral to scapulothoracic), ADD=:::45deg,Flex=90deg, Ext=kideg; IR=55deg, ER=45deg Special tests: • l}~.i:ft,~fLtest - for tear of subscapularis; unable to lift the dorsum of hand off back, subseap maximally active in midlumbar position (also see excessive passive ER with subscap tear) • 2)13~nY Press test - pt presses the abdomen with the flat of the hand and attempts to keep the arm in maximal IR, elbow should remain in front of trunk if subscap intact " 3)ER lag sign - elbow is passively flexed to 90deg, shoulder 20deg elevation and near max ER; pi then asked to maintain position, magnitude of lag measured to nearest 5deg, tests the supra and, infraspinatus 4)Drop sign - hold ann 90deg elevation, full ER with elbow flexed 90deg, ask pt to maintain position, measure drop to nearest 5deg, assesses infraspinatus fxfi " 5)N~erImpingement sign - scapular rotation prevented with one hand then raise ann in forced forward elevation (bw flex and abd) causing GT to impinge against acromion 6)Hawkins impingement sign - forwardflex.humerus to 90deg and with elbow flexed 90deg, forcibly IR the shoulder 1& 7)Jobe empty can test - shoulder AB:g.90deg, flexed 30deg and IR (thumb pointed down); tests thesupraspinattls • 8)Hornblowers sign - inability to ER the elevated ann demonstrates infraspinatus weakness • 9)Sulcus test - done with arm at 0 and 45deg .WD, pull distally on ext and obs for sulcus or dimple bw humeral head and acromion; Grade 1 = <Lcrn, 2 = 1-2cm and 3 = >3cm of inferior subluxation; subluxation atOdeg more indicative of laxity of the rotator interval • 10) Shoulder Lachman test - grading ant instability; with pt supine and examining right shoulder grasp proximal humerus with left hand and right lightly holds the elbow and apply ant stress; Grade 1 = translation greater than contralateral arm; 2 = HH slips up to
II III
35
,.
rim of the glenoid, 3 = HH slips over the labrum but then spontaneously relocates, 4 = dislocation 11) Cross arm test - FE to 90deg and active ADD brings the acromion into contact with the distal clavicle, pain in vicinity of AC joint indicates pathology here
o Impingement syndrome: -Neer: • Stage 1 == edema and hemorrhage within the cuff, sxs of mild activity related pain no weakness, pts usually <25yrs old; reversible • Stage 2= progression to fibrosis and thickening of subacromial bursaand chronic supraspinatus tendonitis; usually 25-40yrs old, sxs with ADLs or at night, can have dec ROM(most often dec IRdue to tightness in posterior capsule); have pain with activities that place shou1der in painful arc of 70-100 of elevation orABD " • DDX = glenohumeral instability, articular-surface PTRCT, . labrum tears, small areas ofDJD, post. glenoid-cuff impingement, lesions- of tot ator interval, AC arthritis, cspine dz; suprascapular neuropathy • Stage 3 = PTRCT or FTRCT and biceps tendon lesions o Os acromiale - acromion forms from four ossification centers that fuse by ISyrs, presentin -3% and is bilateral in 60%, ,roost are asx but some s~gest an association with impingement; tx = resect undersurface if bw meso and meta and complete resection ifbw pre and meta o Massive Rotator cuff tears: • Size of tear - small <1 em, medium 1 to <3cm, la;:ge 3 to <5cm .. massive >5cm • ~O% mcidence of FTRCT jn asymptomatic pts Qlder than 60yrs. • will see ant-superior subluxation and prominence of humeral head, infraspinatus atrophy, and prox"biceps rtlp.ture, .can get "deltoid rupture from erosion of origin by humeral head as it articulates with the acromion • xray --elevation of bum era1 head, dec. acromiohumeral distance «7mm c/w RCT, <5nun c/w massive tear), articulation with acromion, erosion and roundin 0 • MRI can see atty replacement of sllpraspjnatus in fossa • Arthroscopy with debridement and SAD - best suited for lower demand pis, avoid excessive acromioplasty (removal of 5.4mro of undersurface of ant. acromion reduces contact pressure of the a£omion on the supraspinatus tendon) and preserve CA ligament which helps prevent lossof restraint to superior humeral head subluxation
36
Burkhart et al advocate partial repair (of irreparable tears) that reestablishes the cable construct of the RC, in part this is achieved by a side to side repair • Postop position. of immobi1ization is safest with 30de§Lof elevation in the coronal or scapular plane and ER ofO-60deg (this puts least a.m.0untof strain on the repair) . Results of latissimus dorsi transfer is better with intact subscap (Gerber et al) Shoulder arthrodesis - position is 20deg FE. 30deg ABD and 40deg IR '"Hemlarthroplasty with biologic resurfacing (of glenoid and acromion) provides reproducible pain relief with modest motion gains; ifpt is able to elevate beyond 90-100de do HHR, ifnot do Reverse pros eSlS l~..!. usc e replacing prosthesis, increases the m lever arm of the delt?id). :r~ / v::-d, ~( 5(1+ ot.ee..,J..- of~;.j • Successful cuff healing IS not required to attain a high level ofpt satisfaction after attempted but failed RCR, decompression DOj cuff healing is the key to pain relief in cuff rt;"pairsurgery ,. Ant-superior escape after cuff repair debridement is related as much to or more to denervation and dehiscence of the deltoid as it is to acromioplasty or CA lig release (Burkhead) • Debridment with limited acromioplasty of irreparable cuff tears is an option in the pt whose primary complaint is pain and whose motion and strength are not perceived as disabling Inverse prostheses are successful for restoring ant. elevation, tendon transfers for restoration of rotation "' Lat transfer is indicated for _pi who has active ant elevation >90de_g_ but no active ER o Partial thickness ReT: a Ellman Grade l=frayed tendon«3mm or <1/4 of tendon thickness), 2=<50%(3-6nun, <112 thickness), 3=>50% (> 1/2 thickness), A(articular side) I?(bursal side); avg cuff thickness 212mm Kebab or SAD have not been ShOVlllo delay or prevent t ,J2rogression toa complete tear ~ Treatment with debridement and acromioplasty ofPTRCT fajled if (£./' the tear involved >50% of1he tendon (Grade 3) and thus SbmlJd he ~ repaired (Weber et at .Arthroscopy 1999) • SAD in pts with PTRCT comprising less than 50% of the tendon (grade 1 and 2) was not significantly different from that ofpts without PTRCT, the subgrQup ofpts wjth grade 2B partial tears had a statistically Significantly higher failure rate and may be better ~ served with primary repair (Cordasco et aI, AJSM 2002) C.._i9J' Bursal-side tears are seen more often at the musculotendinOllS :Pm, articular-side tears often are seen at the insertion site where vascularity and perhaps the sensations are decreased; Articular side
iii II
(fj).
>
Il
Ii
.....
---
37
• • •
• • .,
II
• •
tears are much more common than bursal side tears (2-3Xs), a:rtlcular surface of the cuff' has an ultimate falling stress only half as high as the bursal surface... fpeak incidence is in fifth and.sixth decade No evidence that debridement of a partially torn cuff stimulates a heating response (Gartsman J Shoulder Elbow Sur~ S;Jprascapular artery is the primary vascular supply to the supraspmams tendon Pathogenesis: intrinsic tendinopathy related to vascular changes; extrinsic impingement such as narrowed coracoacromial arch; tensile overload of the cuff due to repetitive micro trauma or a single violent episode; degenerative tears seen on articular surface with extensive lamination possibly due to differential shear stress affecting the layered anatomy of the cuff, ultimate stress to failure is half that of bursal surface; thus the area of hypovascularity at the articular surface close to insertion of supraspinatus tendon and the dec biomechanical properties lead to more articular sided tears Increasing evidence that PTRCTs progress !ttve a painful arc of motion bw 60-120 deg of elevation, dec ROM due to posterior capsular tightness and restncts!! MR1 T2 images see a focal defect that is limited to one surface or is intratendinous (no evidence of tendon discontinuity), fatsuppression techniques accentuate fluid signal contrast on T2 images and can inc sensitivity ofPTRCT detection MRI with gadolinium useful Intratendinous laminations are assoc. with ~50% of bursal sided and articular' surface tears PASTA lesion (partial articular supra~pinatus tendon avulsiow~ .a transtendon arthroscopic repair
Surgical technique: Three principles: • Tear pattern recognition - broadly divided into crescent shaped or U-sl}aped; Cresent shaped tears do not retract much and canDe directly repaired to the G_T;~haped tears the medial pomt of the tear doesn't represent retraction but is the shape that an L or T shap~d t~ar assumes with muscle. contraction~. ~J component by margm convergence (sIde t~lde suturing in medial to lateral direction) and the transverse componentlike a crescent shaped tear ., Secure Fixation - want minimal shear by repair according to tear pattern, need to mobilize cuff from the subacromial and intraarticular adhesions; Suture placement(simple, mattress or modified Mason-Allen) with knot security is impt, biomechanical testing has shown. that knot security is enhanced with braided suture, alternating post limbs of the sutures and post pointing;
38
iii
-------
double loading each suture anchor increases the number of fixation points and thus dec load on each indy suture; fixation placement is 4-5mm off the articular margin for sin le~row re air Restoration 0 ootprint - double row repairs result in tbe closest reapproximation of the totaTgeometry of the RC fooprint
39
References: Ball CM, Steger T, Galatz LM, Yamaguchi K. The Posterior Branch of the Axillary Nerve: An Anatomic Study. JBJS 2003; 85:1497-1501 Bertelli JA, Ghizoni MF. Long thoracic nerve: anatomy and functional assessment. J Bone Joint Surg Am. 2005; 87(5): 993-8 Bigliani LU, Bauer as, Murthi AM. Humeral Head Replacement: Techniques and SoftTissue Preparation. Instructional Course Lectures 2002; 51: 11-20 Burkart AC, Debski RE. Anatomy and Function of the Glenohumeral Ligaments in Anterior Shoulder Instability. CORR 2002; 400: 32-39 Leffert RD. Thoracic Outlet Syndrome. JAm Acad Ortho Surg. 1994; 6(2): 317-25 Gill TJ, Zarins B. Open Repairs for the treatment of anterior shoulder instability. Am J Sports Med 2003; 31: 142-153 Halder AM, Itoi E, An K. Anatomy and Biomechanics of the Shoulder Hollinshead, AH: Anatomy for Surgeons. Vol. 3, Harper Row, Philadelphia, 1982. Hoppenfeld S, deBoer P: Surgical Exposures in Orthopaedics. The Anatomic Approach. Lippincott, Philadelphia, pp 1-50, 1994. Kuhn JE, Plancher KD, Hawkins RJ; Symptomatic scapulothoracic crepitus and bursitis. ] Am Acad Ortho Surg. 1998; 5(6): 267~273 Moore KL: Clinically Oriented Anatomy. Third Edition. Williams & Wilkins, Baltimore, pp 501~553. 1985. Petilon J, Carr DR, Sekiya JK, Unger DV. Pectoralis major muscle injuries: Evaluation and Management. JAAOS 2005; 13: 59-68 Powell SE, Nord KD, Ryu R. The Diagnosis, Classification and Treatment of SLAP Lesions. Op Tech Sports Med 2004; 12: 99-110 Pierce TD, Tomaino, MM. Use of the Pedicled Latissimus Muscle flap for Upperextremity Reconstruction. JAAOS 2000; 8:324-31 Plancher KD, Peterson RK, Johnston le, Luke TA. The Spinoglenoid Ligament: Anatomy, Morphology, and Histological Findings. IBJS 2005; 87: 361-365 Waters PM. Obstetric Brachial Plexus Injuries: Evaluation and Management. JAAOS 1997; 5: 20~14
An
The Arm
Chris Bales, M.D. Embryology • Upper limb bud develops around day 26 e Develops proximodistally " Limb buds composed of mesenchyme, derived from lateral plate mesoderm, covered by a layer of ectoderm .. Preaxial border = thumb side e Postaxial border = little finger side " Dorsal mass muscles = extensors and supinators Ventral mass muscles = flexors and pronators " The palms initially face each other such that the preaxial border faces cranially and the postaxial border faces caudally ('<praying" embryo) " The upper limb rotates 90 degrees laterally around the 8thweek so that the preaxial border now faces laterally and the postaxial border faces medially, this brings the ventral mass anteriorly and the dorsal mass posteriorly
11>
Osteology - Humerus .. Primary center of ossification in shaft present at 8-9th week (fetal) and fuses by birth .. Proximally there are 3 secondary centers of ossification o Head-- ossifies at 6months o Greater tuberosity - ossifies at 3 years o Lesser tuberosity - ossifies at 5 years o All coalesce at 6-7 years; physeal closure at 14-17yrs for girls and 1618yrs for boys o Proximal humeral physis responsible for 80% of growth Distally there are 4 secondary centers of ossification o Capitulum - ossifies at 2 years o Medial epicondyle - ossifies at 6 years o Trochlea - ossifies at 8 years o Lateral epicondyle- ossifies at 12 years • Bony landmarks/structures o Articular surface - retroverted (-20-30deg) and directed superiorly o Anatomic neck (epiphysis) - at lateral margin of articular surface, separates head and tuberosities, serves as an attachment site for the shoulder capsule o Greater tuberosity - lateral o Lesser tuberosity - anterior o Intertubercular groove (bicipital groove) o Surgical neck - just below tuberosities o Deltoid tuberosity - located anterolaterally
to
41
o o o
Spiral groove - oblique groove extends inferolaterally on posterior aspect of the shaft just distal to deltoid tuberosity, for radial n. and profunda brachii a. Epicondyles - medial larger, projects from trochlea; lateral projects from capitulum Supracondylar ridges - bony ridge running proximally from the epicondyles Distal humerus inclines laterally 5 -8deg creating the valgus-carrying angle; the hurnerocapitellar angle in the adult is 30degrees~
..
Upper extremity growth
AFPEA.RANCE
CLOSURE
20!'
, RADlUS~ULNA
Fig. 1 P0rruolage of contribution ,to Specific bone isshown on the left and p¢rcentage of contrIbufion toilie entire UrJPeJ' extr€mily is
fig. 2 TIn~;tjmes.of ~Jpe4mnCe (left) andd~SlJre (rigflU Qr tile , ,,"
seconda~1ossl!lcatf.on centers" of
the tll1t\(.If extremity,;\, =VeaJs, " '1"I..IW
!,
shown on the right
m =: !nonths} M ::: males,
F ::: females.. '
42
3 Borders o Anterior o Lateral border ~continuous with lateral supracondylar ridge o Medial border - continuous with medial supracondylar ridge
3 Surfaces
o
o
anteromedial anterolateral posterior
Anatomic variations o Size of bicipital groove o Supracondylar process - from anteromedial surface, Scm proximal to medial epicondyle, 1% greater than 3mm, tip points towardsjoint, tip of osteochondroma will point away frcmjoint o Ligament of Struthers - from supracondylar process to medial epicondyle, origin for portion of pronator teres o Median nerve and brachial artery pass posterior to process then deep to ligament of Struthers (site of median nerve compression, arcade of Struthers associated with ulnar nerve compression) Blood Supply o Proximal - via anterior and posterior circumflex humeral arteries, main blood supply to head via arcuate arterior off anterior circumflex; also get minor contribution via soft tissue attachments (rotator cuff) o Shaft - nutrient artery, normally arises from the brachial a. around midshaft and enters nutrient canal on anteromedial.surface; the artery and ," canal run toward the elbow (~!i>,"1he elbow we go from the knee we flee) o Distal ~ via three general arcades, medial, lateral and posterior Medial arcade - formed by superior and inferior ulnar collateral branches from the brachial artery which anatomose with the posterior ulnar recurrent branch of the ulnar artery about the medial epicondyle .. Lateral arcade - formed by descending radial and middle collateral arteries which anastomose with the ascendinginterosseous and radial recurrent arteries on the posterior aspect of the lateral epicondyle; supplies PQ.$te:l1ioLsurface of capitellum and lateral epicondyle Posterior arcade - formed in the olecranon fossa by contributions from the superior ulnar, radial and middle collateral arteries proximally and the interosseous recurrent distally
II Ii
43
Superficial Anatomy: Skin/Fascia • Skin - dennatomaI innervation o Superior lateral cut. n. of arm (branch of axillary C5,6) -:-skin over deltoid 6 Intercostobrachial n.(T2) - skin of proximal medial arm, not anesthetized with axillary block o Medial brachial cut. n. of arm (C8, T'I ,2) - off of medial cord of plexus, skin of media! arm o Inferior lateral cut. n. (C5,6) - branch of radial n., skin oflateral ann o Posterior cut. n. (C5 ,6,7,8) - branch of radial n., skin of posterior ann • Superfical vessels o Cephalic vein - distally is in the superficial fascia along anterolateral, surface of biceps, here it will be in association with lateral antebrachial D. which pierces deep fascia near musculotendinous jxn of the bicepsbrachii, proximally runs in deltopectoral groove and empties into axillary vein .... o Basilio vein - distally runs in medial bicipital groove with the medial antebrachial cut. n., proximally it penetrates the brachial fascia at the jxn of the middle and inferior third of the ann (this is also where the medial antebrachial cut, n. emerges) and runs. superiorly to the axilla to become the axillary vein • Fascia o Superficial fascia (tela subcutanea) -loose layer o Brachial fascia (deep fascia) - is loose anteriorly over biceps, firmly attached to triceps o Two intermuscular septa extend from the brachial fascia and are attached to the supracondylarridges of the humerus, they divide the ann into anterior and posterior compartments o Medial fntermuscular septum .. Continuous with pectoralis major and deltoid .. Between coracobrachialiaand brachialis.anteriorly and triceps posteriorly .. Extends from medial supracondylar ridge it? insertion of. coracobrachialis .. Pierced by ulnar nerve and superiorulnarcollateral artery passing from ant to post compartment ~8~10cm proximal to medical epicondyle • Origin for portions of brachialis and triceps o Lateral iniermuscularseptums .. Extends from insertion-of deltoid to attach to lateral supracondylar ridge and epicondyle .. Between brachialis, brachioradialis and ECR anteriorly and triceps posteriorly and serves as origin for portions of these muscles • Pierced by radial nerve and radial collateral branch of profunda artery passing from post to ant -7 -Scm proximal to the lateral epicondyle
!,
44
Anterior compartment Muscles - Coracobrachialis, biceps brachii, brachialis • Nerves - Median, ulnar proximally and radial distally .. Brachial artery o Posterior compartment • Muscles - Triceps, anconeus • Nerves - ulnar distally and radial proximally '" Profunda brachii artery
III
Muscles • Biceps brachii o Origin - Short head: coracoid process; Long head: supraglenoid tubercle o Insertion - biceps tendon inserts onto posterior portion of tuberosity of radius and is separated from anterior portion of tuberosity by radial bicipital burase; bicipital aponeurosis (lacertus fibrosis) joins with deep fascia of flexor/pronator mass and inserts onto ulna o Action - flexor of forearm and main supinator of forearm; minimally involve in flexion of the pronated forearm; can act as a weak shoulder flexor via short head of biceps o Innervation - musculocutaneous n. (C5,6) e Coracobrachialis o Origin - tip of coracoid process . o Insertion - medial midshaft of humerus o Action.- helps flex and adduct arm o Innervation - musculocutaneous n, (CS,6),ipierces this muscle -5cm distal to coracoid splitting it into two parts . o Variations - can extend to insert on medial epicondyle, rarely third head coracobrachialis brevis Brachialis o Origin - distal 112 to 2/3 of anteromedial and anterolateral humerus, medial and lateral intermuscular-septa, proximal portion divided by deltoid insertion o Insertion - coranoid process and tuberosity of ulna o Action - elbow flexion o Innervation - musculocutaneous n. (C5,6);, occasionally radial nerve can innervate lateral portion however some believe this is just a sensory branch) e Triceps brachii o Origin .. Long head - infraglenoid tubercle • Lateral head - posterior surface of humerus proximal to radial n. and lateral intermuscular septum • Medial (deep) head- posterior surface of humerus distal to radial n. and medial intermuscular septum, also lateral intermuscular septum distal to radial n.
II
45
Insertion - olecranon over subtendinous bursa of triceps and deep fascia of forearm o Action- chief extensor of forearm; shoulder extension and weak adduction o Innervation - radial n. (C6-8); ulnar.collateral.n. is a branch of the radial. n. which innervates medial head of triceps allowing longitudinal splitting of medial head without denervation o Articularis cubiti muscle - slip of triceps onto synovial membrane of elbow Anconeus o Origin -lateral epicondyle 0' Insertion -lateral olecranon, covers posterolateral elbow capsule, annular ligament and proximal ulna ." .0 Action - elbow extension, stabilizer of elbow joint o Innervation - nerve to anconeus (C7,8), from radial nerve which passes thru medial head of triceps
Nerves • Musculocutaneous o C5,6 (+/~C7) o Terminal branch of lateral cord of brachial plexus o Pierces coracobrachialis -5-8cm distal-eo coracoid process then travels between the biceps and brachialis.and becomes the lateral antebrachial cutaneous n.at about the level of the musculotendinous jxn of the biceps (this is also where it pierces the deep fascia) o Motor to biceps, brachialis and coracobrachialis • Median
o ;iC5"T}
o o
o •
Formed by portions of lateral and.medial cord of brachial plexus Travels down the ann deep to the short head of the biceps and lateralto the brachial artery. At midbrachium it crosses to the medial side of the " brachial artery In the antecubital fossa it lies deep to the bicipital aponeurosis medial to the antecubital vein, and medial to the brachial.artery making it the most medialstrugNry~n.c8~lI1tere9 Gives no motor Or sensory above elbow, however branches have seen as far as 4cm proximal to elbow
Ulnar o C8,Tl(+/ .. 7) C o Terminal branch of medial cordof-brachial plexus o Travels deep to the pee major and courses medial to the brachial artery emerging from beneath the pec majo¥;I.l1y~jflJW thecoracobrachialis and anterior.to the longliead'bfthe tricepso Pierces the medial intermuscular septum ~ 1Ocm proximal to the medial epicondyle (along with superior ulnar collateral a.) to enter posterior
compartment where it lies on the anterior border of the medial head of the
triceps
o o
Passes behind medial epicondyle where it is encased within a fibrous sheath (Osborne's ligament) laterally and the head of the FeU posteromedially (these two structures fOnTI the cubital tunnel) it then passes between the humeral and ulnar heads of FeU to enter the forearm First branch of the ulnar nerve provides sensory innervation to the elbow capsule. No motor branches in arm Arcade of Struthers is a thick fascial band that connects the medial head of the triceps to the intermuscular septum and crosses the ulnar nerve ~8cm proximal to the epicondyle (found in ~70%ofpopulation)
.,
Radial C5-8 Arises from posterior cord of brachial plexus o Emerges thru triangular interval-deep to long head of triceps, inferior to teres major and between long and medial heads of triceps o Passes into arm anterior to the latissimus insertionand dives into the triceps to lie on the posterior surface of the humerus about 1O-14cm distal to the acromion close to the spiral groove resting on origin of medial head of triceps o Crosses the midline at avg. of 15crn from the distal articular surface and with radial collateral a-pierces lateral intermuscular septum ~ 10-12cm from the lateral epicondyle (during lateral approach to the humerus is located 7.5-1 Oem proximal to epicondyle) o Enters forearm between brachialis and brachioradia1is/ECR muscles anterior to the lateral epf~ondyi~ .:. o Branches Posterior brachial cutaneous n. to skin of proximal posterior 1/3 of ann Inferior lateral brachial cutaneous n. (upper branch of post antebrachial cut. n.) to distal V;.,lateral and anterior ann • Posterior antebrachial cutaneous n. to posterior forearm and dorsum of wrist " Motor branches to triceps muscle, medial portion of medial head of triceps supplied by 'ulnar collateral n.'. there are many branches to the triceps therefore fxs are unlikely to be assoc. with loss of triceps fxn.. Brachialis has dual innervation from radial nerve (lateral fibers) and musculocutaneous nerve (media] fibers), Abrams et al. reported only 50% of specimens demonstrated this dual innervati on Nerve to anconeus Muscular branches to brachioradialis and ECRL (innervation of EeRB 55% of time via radial and 45% of time via PIN)
o o
If II! Il II
47
Arteries and Veins • Brachial artery o Axillary a. ends at lower border of teres major to become the brachial a., travels medial to biceps in ant. compartment then deep to lacertus fibrosus to become the radial and ulnar arteries; is medial to median n. proximally and lateral distally in the antecubital fossa. o Profunda.brachii - largest branch, arises from posteromedial aspect of brachial artery -18-25cm proximal to mediaL~J?~condyle, travels with radial n. between medial and lateral heads of triceps' . middle collateral a., descends within the medial head of the triceps, anastomoses with interosseous recurrent a. radial collateral a. pierces septum with radial n. and descends between brachialis and brachioradialis!ECRto anastomose with radial recurrent a. anterior to lateral epicondyle • deltoid branch; anastomoses.with post. circumflex humeral a. • nutrient a. to humerus (more commonly arises from brachial a.] o Ulnar collateral arteries Superiorulnar collateral a.arises near middle of.arm and pierces septum with ulnar nerve to posterior aspect of medial epicondyle and anastomoses with posterior ulnar recurrenta. and often with inferior ulnar collateral a. • InferIor ulnar collateral a, (supratrochlear a.) b~gjR!i<;;:;;?~5cm proximal to medial epicondyle and travels ant. to epicondyle to anastomose with ant. ulnar recurrent a. o Nutrient branch enters anterornedial humerus in mid-arm to travel towards elbow, there is a watershed area seen betweel)ci!:h~,nutrientartery supply proximally and the distal local circulation· . II Superficial arteries of the ann o Can arise in axilla or ann, course is superficial to median nerve o Most common is supenic;tal br.ac?ial.q.. • Veins - two brachial veins accompany the brachial artery, formed by union of venae comitantes of the ulnar and radial arteries (L"1dnd in the axillary vein e
II II II!
Approaches to the Humerus: • Anterior approach o Incision runs from tip of coracoid in line with deltopectoral groove to insertion of deltoid then along lateral border of biceps to Scm proximal to flexion crease of the elbow'; o Internervous plane - proximally between the deltoid {axillary n.j-and pee.", r.gajor (medial and lateralpectoraln.) and distally between the medial fibers ofthKJ~:r:flchialis (musculocutaneous n.) and lat~rfllfib~Tsofthe brachilis (radial n.) o Identify cephalic vein in groove and develop plane down to insertion of deltoid and pectoralis major on lateral lip of bicipital groove.
48
Identify interval between biceps and brachialis and incise deep fascia. Split fibers of brachialis longitudinally along its midline to expose anterior humeral shaft. o Dangers: Radial nerve is vulnerable in the spiral groove on the posterior middle third of the humerus (keep dissection subperiosteal in this area). Also in danger in distal third as nerve pierces lateral intermuscular septum and lies between brachioradialis and brachialis (avoid by splitting brachialis in midline) • Axillary nerve can be damaged by retraction of the deltoid • Anterior circumflex vessels cross in interva1 between pee. major and deltoid in upper third Anterolateral approach o Incision is a curved, longintudinal one over the lateral border of the biceps from IOcm proximal to flexion crease to just above the crease: Used to expose distal half of the humerus. o No true internervous plane as both brachioradialis and lateral half of brachialis supplied by radial nerve. o Retract biceps medially and incise fascia between BR and brachialis. Find radial nerve between these two muscles at the level of the elbow joint. Retract the nerve laterally. Incise the lateral border of the brachialis. o Can extend proximally developing in plane between brachialis and lateral head of triceps. Distally can extend into and anterior approach to the elbow between the BR and pronator teres (median n.) o Dangers: .. Radial nerve .. Lateral antebrachial cut. n. runs roughly in line of approach Posterior approach CHerny) o Incision in midline of posterior aspect of ann o No true intemervous plane. o Separate heads of triceps identifying gap between long and lateral heads proximally (radial nerve actually separates their origins). Innervation of these muscles is proximally near their origin so you do not denervate them. Incise medial head in its midline. Keep dissection subperiosteal remembering that ulnar nerve pierces intermuscular septum in lower third of the ann o Can extend this distally over the olecranon. Approach is not effective above the spiral groove due to the radial nerve o Dangers: " Radial nerve. Crosses midline about 15cm above the elbow joint. .. Ulnar nerve lies deep to the medial head of the triceps in rower third. s Profunda brachii artery lies with radial nerve.
II
49
Lateral approach o Incision over lateral supracondylar ridge o Interval between the brachioradialis and the triceps. Incise deep fascia and cut down to bone between these two-muscles. o Can extend distally by using interval between anconeus and BCU. Cannot go proximally because radial nerve pierces septum 7 -8cm proximal to epicondyle. o Dangers: • Radial nerve safe as long as you don't go proximally.
Pathology • Holstein-Lewis fx - distal 113 spiral fx of humerus associated with radial nerve injury (5-10%) " Thesupratrochlear a.(inferior ulnar collateral a.) is least flexible of the collateral vessels around the elbow and binds the brachial a. against the spike in extension type supracondylar humerus fxs " Humeral shaft fxs - deforming forces o Fx above pee, major insertion: proximal fragment ER by-rotator-cuff distalfragment displace medial and proximal by deltoid and pee. major o Fx between pee. major and deltoid tuberosity: proximal fragment displaced medial(ADD) by pec. major, teres major and latissimus, distal fragment ABD by deltoid o Fx distal to deltoid tuberosity: proximal fragment ABD by deltoid, distal fragment displaced medial(ADD) and proximal by biceps and triceps
50
References .. Abrams RA, Zeits RJ, Lieber RL, et al: Anatomy of the radial nerve motor branches in the forearm. J Hand Surg 22A: 232-237, 1997. .. Hollinshead, AH: Anatomy for Surgeons. Vol. 3, Harper Row, Philadelphia, 1982. .. Hoppenfeld S, deBoer P; Surgical Exposures in Orthopaedics. The Anatomic Approach. Lippincott, Philadelphia, pp 51-82, 1994. .. Mazurek MT, Shin AY: Upper Extremity Peripheral Nerve Anatomy. Clin. Ortho. & ReI. Res. 383: 7-20, 2001 .. Miller MD: Review of Orthopaedics. Third Edition. W.B Saunders Company, Philadelphia,2000. .. Moore KL: Clinically Oriented Anatomy. Third Edition. Williams & Wilkins, Baltimore, pp 539-53. 1985. .. Thompson le, Netter FH: Netter's Concise Atlas of Orthopaedic Anatomy. Icon Learning Systems LLC, New Jersey, 2002 • Yamaguchi K, Sweet FA, Bindra R, Morrey BF, Gelberman RH: The Extraosseous and lntraosseous Arterial Anatomy of the Adult Elbow. J Bone Joint Surg 79-A(11): 1653-62,1997.
51
The Elbow
NickDutcheshen, M.D.
• Developmental 'Anatomy: o Secondary ossification centers appear on X-Ray at predictable age: • capitellum: 6 rno-Z years, includes the lateral crista of the tubercle • .radial head: 4 years • medial epicondyle: 6-7 years • -trochlea: 8 years • olecranon: 8-10 years; often multiple centers, which ultimately fuse • lateral epicondyle: 12 years • *mnemonic CRMTOL (Come Rub My Tool Of Love) o Medial epicondyle is last to fuse. Its closure indicates that maturation is complete Osseous anatomy: o Trochoginglymoid or hinge joint with three articulations (radioulnar) ulnohumeral, radiohumeral) o Capitellum (little head)- hemispheric, palpable in flexion; blood supply is through a posterior branch that enters the lateral crista o Trochlea • spool-shaped • trochlear groove is directed lateral and posterior; this results in: the lateral deviation of the ann in extension • supplied by a medial arterial branch that enters along the nonarticular medial crista and by a lateral branch that crosses the physis (no anastomotic connection exists between vessels of trochlea and capitellum) o Medial and lateral columns of humerus join at trochlear notch o Medial epicondyle: origin flexor-prenetermuscles o Lateral epicondyle: origin of the extensor-supinator muscles o Coronoid: provides stability to ulnohurneral articulation and serves as attachment site for anterior band of MeL on the sublime tubercle, as well as the brachialis and anterior capsule o Semilunar notch/trochlear notch/greater sigmoid notch of olecranon: • provides primary stability to elbow • forms an ellipse with an arc of -190de'g • articulates with apex of trochlear sulcus !' • Valgus stress is primarily resisted by proxima] halfand varus stress by the distal half o The articulating surfaces of the capitellum and trochlea project distally and anteriorly at an angle of approximately 45 degrees
or
52
Carrying angle is influenced by the obliquity of the distal humeral physis; this averages 6 degrees in females and 5 degrees in males and it is important in assessing angular growth disturbances Range of motion is 0-150 degrees of flexion, 85 degrees of supination, 80 degrees of pronation; functionally one requires 30-130 flexion arc, and 50 degrees of pronation and supination
Oi
Fibrous Capsule and ligaments o Ulnar collateral ligament (medial collateral ligament) 3 bundles: anterior) posterior and transverse ligament Anterior bundle • originates on the anteroinferior lateral two thirds of the medial epicondyle • inserts onto the coronoid process at the sublime tubercle an avg. of 18mm distal to 'the coronoid tip,(the brachialis and capsule insert an avg. of 11mm and 6mm distal respectively) ., this is the most important ligament in resistance to a valgus load (focus of reconstruction for MeL instability, aka "Tommy John surgery") • taut throughout most of the entire arc of flexion • avg. load to failure 260N • posterior bundle is a thickening of the posterior capsule that inserts along the semilunar notch transverse bundle originates and inserts on the ulna, therefore plays no role in elbow stability; often not identified during gross dissection
II II II
Anterior band
Posterior band
Transverse
:::@L.;;........~-
Jig ament
of Gdoper
53
Lateral collateral ligament .. Four components: annularligament.radial collateral ligament, lateral ulnar collateral ligament (LUCL) and accessory LCL •. originates off the anterior inferior aspect of the lateral epicondyle which is at the center of the trochlea and capitellum which is the axis of rotation of the elbow the radial collateral ligament terminates indistinguishably in the annular ligament • LUCL blends with fibers of annular ligament but also arches superficial and distal to it to insert on the tubercle of the supinator crest of the ulna the supinator tendon crosses this ligament complex obliquely from distal to proximal at its ulnar attachment .. fibers of the annular ligament blend with this ligament near its insertion
II
Accessory lateral collate rar '[jgameril
.Articl1f<ir '
ca.psule
Supinator crest Laieral ulnar co!lateralligameri1
o
r~HUU
.I.
Tubercle
--'"1-at
1~__ ~ --~. lLl;;i:HUCUl.
"::-_ ..
iUWJ
-}C:4h~..,£ a. UJA•.u,,·lJ.L
circle: alLal.>W; -5" ~0 .1 a.utvk10r: -~- - L 11(,;1:;;;, ~ne~ -'A'
'1' J a£lu
posterior radial notch and ulna; forms the capsule of the proximal radioulnar joint o Anterlnr capsule • covered by brachialis • is taut in extension • is a significant stabilizer to pure varus stress (32% of stability) and valgus stress (38%) in extension but not at 90deg of flexion o Posterior capsule - thin, covered by triceps o Synovial membrane: reflected into fossae; fat pads within fossae can be displaced with hemarthroses o Anterior fat pad is more sensitive to displacement with small effusions than the posterior fat pad., which is displaced with moderate to large effusions
54
Elbow Stability ., The Ulnohumeral articulation provides ~55% of varus stability in extension and up to 75% in 90deg of flexion, at less than 20deg of extension and greater than 120deg of flexion it provides the greatest contribution to elbow stability against varus and valgus stress • Anterior bundle of the MCL is the primary restraint to valgus stress contributing 55-70%, rupture of-this ligament results in gross instability at all degrees of flexion short of fu1l extension .. Valgus stability is equally divided among the MeL, anterior capsule and radiohumeral articulation in full extension LUCL - deficient in posterolateral rotatory instability, allows a transient rotatory subluxation of the ulnohumeral j oint and a secondary dislocation of the radiocapitellar joint The olecranon process of the ulna contributes a significant amount of varus and valgus stability of the elbow Radial head may contribute up to 30% of valgus stability even with an intact MeL, with tear ofMCL up to 75% of resistance to valgus stress is seen in the radial head, also up to 60% of a longitudinally applied force is transmitted through the radial head Dynamic stability .. Brachialis
II III OJ III
" • " "
Tri~;B,B,. Medial side - FeU (humeral head) and to lesser extent FDS may augment the MeL Lateral side - extensor muscle origin
Blood Supply o Rich from collateral circulation; see blood supply to trochlea and capitellum above o Medial: superior and inferior ulnar collaterals anastomose with posterior recurrent arid anterior ulnar recurrent arteries respectively o Lateral: radial collateral and middle collateral anastamose with radial recurrent and interosseous recurrent arteries respectively o Brachial artery splits into radial and ulnar arteries just distal to elbow joint Injuries o Medial elbow pain: 1. Medial epicondylitis - Golfers elbow 2. Medial collateral ligament sprain or tear; elbow may open up laterally with valgus stress done with elbow flexed 30deg ·3. Ulnar nerve irritation; pain/parathesias/weaknes in ulnar nerve distribution
"
55
Lateral elbow pain: 1. Osteochondritis dissecans of capitellum (must differentiate from Parmer's disease; Parmer's pt usually <8y.o., OeD older child; Parmer's is an osteochondrosis and is self limited, OCDcart be progressive and very limiting)' . 2. Lateral epicondylitis (Tennis elbow): ERCB origin 3. Lateral collateral ligament sprain/tear 4. Other: PIN syndrome, lateral antebrachial cutaneous nerve lesion, cervical disc, tumor of radial head or capitellum)
o Anterior elbow pain: 1. acute: possible intraarticular pathology, distal biceps injuries, chondromalacia or loose bodies 2. chronic: pronator teres syndrome, capsular strain, inflammation, secondary contracture o Posterior elbow pain: 1. olecranon bursitis 2. triceps tendonitis 3. valgus extension overload with fragmentation of olecranon and osteophyte formation with possible loose bodies (osteochondromatosis) o Distal Biceps Rupture: 1. Biceps tendon passes deep into antecubital fossa to insert at radial tuberosity 2. Bicipital aponeurosis (lacertus fibrosis) passes distally and medially across fossa to.blend with fascia and insert on SQ border of ulna 3. Biceps muscle is strongest supinator of the forearm and assists brachialis with flexion '. 4. Modified Boyd-Anderson two incision technique a. Transverse incision in flexion crease b. Lateral antebrachial cut. nerve needs to be protected. Lateral antebrachial cut nerve isterminal branch of musculocutaneous n. Pierces deep fascia of arm near musculotendinous jxn of biceps and lies in SQ tissues of antecubital fossa c. Incise deep fascia d. Identify biceps tendon and mobilize. e. If aponeurosis is intact tendon will remain in sheath if not it will retract proximally. f. Minimally debride tendon and place nonabsorbable suture through tendon g. Blunt finger dissection is used to identify radial tuberosity h. With forearm in supination to protect PIN a blunt hemostat is advanced along medial border of tuberosity to dorsolateral aspect of proximal forearm taking care not to violate periosteum of the ulna
56
i, Remember TAN - from lateral to medial - Tendon, Artery,
Nerve j .Brachial artery bifurcates at lvl of radial head; radial recurrent a. branches from radial a. and passes laterally and proximally across the fossa k. Radial nerve enters fossa laterally between brachialis and brachioradialis 1. Divides into superficial and deep (PIN) branches m. PIN courses around the lateral side of the radius and enters supinator bw its humeral and radial heads (arcade of Froshe) n. Second incision made over the hemostat. Common extensor muscle mass and supinator are split down to the radial tuberosity with forearm in maximal pronation to protect PIN o. Biceps tendon fixed to radial tuberosity via drill holes or suture anchors o Fractures: 1. Supracondylar humerus fx: flexion and extension types 2. Intercondylar humerus fx 3. Medial or lateral condyle fxs 4. Medial epicondyle fx 5. Lateral epicondyle fx 6. Olecranon fx 7. Radial head fx Dislocations 1. Posterior or posterolateral account for -90%, secondary to hyperextension; both collateral ligaments are usually disrupted at there humeral origin; surgery indicated if maintenance requires flexion beyond -50-60deg 2. Once relocated stability provided by articular congruence and the muscular flexor and extensor origins acting as secondary stabilizers 3. Can be associated with fractures (12-62%); medial epicondyle fxs most common (fragment can become trapped within joint) 4. terrible triad: elbow dislocation, coronoid fracture, and radial head fracture 5. nursemaids elbow: not usually radial head dislocation, but rather entrapment of portion of annular ligament within joint that can be reduced with supination, flexion and pressure on the radial head Complications of elbow injuries: 1. heterotopic ossification/myositis ossificans 2. stiffness: very common and reason for moving elbows quickly after an injury 3. nerve injury to median or ulnar nerve 4. vascular injury
57
Approaches to the Elbow . .-, o Posterior: "front door to the elbow is through the back"; provides the best possible view of the·humeral articular surface through an olecranon osteotomy (occasionalJy may be done with retraction of triceps, avoiding osteotomy) 1. Pt positioned prone with shoulder abducted 90 degrees and arm hanging over board/side of table 2. Posterior incision, at proximal tip of the olecranon, curve laterally avoiding the incision directly over the olecranon '3. no true internervous plane (tnceps~radial nerve) 4. incise deep fasia, and note the ulnar nerve medially, lying just posterior to the groove of the medial epicondyle (may transpose nerve if needed) 5. can do a triceps splitting or sparing approach depending on amount of exposure needed 6. Olecranon osteotomy: triceps insertion is isolated and the joint capsule freed from both sides of the olecranon. Chevron osteotomy made with the ...apex pointing distally providing a broa:de?SUrface ~ cancellous bone more rapid union. Osteotomy made in midportlOn'of olecranon where the hyaline cartilage is not continuous (bare area). The osteotomy is completed with an osteotome to produce a more irregular surface for later reduction. Predrilling of the olecranon is done priorto the osteotomy. The olecranon and triceps are retracted proximally. 7-. Radial nerve crosses from posterior compartment t~or compartment approXimately 7-1 Ocm above lateral epicondyle through the lateral intermuscular sepfum, proximally me nerve IS encountered m tfi."e' spiral groove -13"" 15cm above the lOmt line -.
0:
---
Anterior: useful in neurovascular repairs, some tumors and repair of distal biceps tendon ruptures 1. usually transverse incision over Langer's ·lines of antecubital fossa or "boat"race'rcurveoJl1crst0111ittmg anterior aspect of elbow 2. internervous plane is between the brachialis (Me nerve) and brachioradialis (Radial nerve) proximally and the brachioradialis and pronator teres (Median nerve) distally 3. note the superficial veins and lateral antebrachial cutarieous (terminal branch of Me nerve) nerve as-is crosses operative field superficiaUy 4. brachial artery and median nerve lie just medial and deep to lacertus fibrosis 5. blunt dissection is used in this area to avoid damage to important neurovascular structures
--
Medial: 1. 8~1Ocm incision centering over the medial epicondyle 2.r."internervous plane is between brachial is (Me nerve) and triceps (Radial nerve) proximally, and brachiahs and pronator teres (median nerve) distally 3. avoid branches of the medial antebrachial cutaneous nerve of the forearm 4. dissect out ulnar nerve if needed to transpose Anterolateral: not used frequently 1. curved incision over the anterior aspect of the elbow joint 2. internervous plane between the brachtahs (MC nerve) and brachiradialis (Radial nerve) proximally and between brachioradialis and pronator teres (Median nerve) distally 3. identify lateral antebrachial cutaneous nerve superficially 4. i~ detachl~g the supinator ~roximally off of radius, supinate arm to aVOIddamaging the postenor interosseous nerve
..
"..
----
---
--
Posterolateral (Kocher): used for access to lateral joint and radial head 1. incision is based over the posterior surface of the lateral humeral epicondyle '72. mtemefVous plane is between the aconeus (radial nerve) and the extensor carpi ulnaris (posterior interosseous nerve); dIssect between these -tWo muscles down to lateral joint ligaments and capsule 3. Arthrotomy -anterior to the LUCL, make a Z arthrotomy centered over the annular ligament, this way l1umeroulnar stability is not violated; the anterior capsular flap can be released from the humerus because the LUCL remains intact; if extra exposure is needed (eg. for a RH prosthesis) the posterior capsular flap is released from the humerus, since the LUCL is violated this must be . with transosseous sutures
Annular
liga:ment
L$.teraI ulnar c'oliaferal iigarnent
~. ~tl1e
if dissecting distal to annular ligament, pronation of the foreann__geps posterior interosseous nerve away from the operative field
59
Elbow Arthroscopy o Understanding elbow anatomy is crucial for safe placement of portals o Ulnar nerve lies in direct contact with the posteromedial aspect of the joint, therefore there are no posteromedial elbow portals 0 Radial nerve (the nerve most at risk in elbow arthroscopy) lies ,anteromedially between brachialis and brachioradialis, approximately 6nun from the anteriof capsule o Median nerve lies between the pronator teres and brachialis and is located 12m.m from the elbow capsule o Portals are most commonly made with the elbow flexed, taking tension off the anterior nerves and allowing them to displace further anteriorly avoiding damage o When making portals incise only the skin (use an I 1 blade) and dissect bluntly down to capsule to avoid damaging nerves o Portals: four anterior and four posterior • Anterolatyal: 1cm ant and 1~3cm distal to lateral epicondyle; the ""'posterior antebrachial cut n. is withm 2mm of thIS portal, with ann in 90deg flexion the radial nerve is on avg. 5-9mm from the portal • .Anteromedial: 1crn anfand lcm distal (as originally described, recommended now to place it I em proximally2Jo-m.e.diai epicondyle; medial antebrachial eut n. at risk, with portal 1em proximally median nerve is 22mm from portal • Superomedial: also called proximal medial portal;_2cm proximal to rued epicondyle, just ant to medial 1M septum (must stay , anterior to protect ulnar nerve), the posterior branch of the medial antebrachial cutaneous nerve is at highest risk for injury • Superolateral: 1..2 em superior and l cm anterior to Iat epicondyle, may be used as initial viewing portal and provides complete visualization of the anterior aspect of the j oint; maintain contact with anterior humerus as trocar is advanced; posterior branch of lateral antebrachial cutaneous nerve lies on avg. 6mm from trocar, radial nerve is 1O-14n1ffi with elbow in flexion • Posterior: 1-2 em superior to tip of olecranon in midline • Posterolateral: 3crn proximal to olecranon tip and just lateral to lateral edge of triceps tendon • Midlateral: also called direct-lateral portal; space between olecranon, radial head and lateral epicondyle ('soft spot' = same position as injection of joint) • Posteromedial: (described in the literature, but not used secondary to risk of damaging ulnar nerve)
/'
60
.i.
,.
"
The Forearm
Nick Dutcheshen, M.D. ~ Osteology: o Radius Bowed laterally, 3 borders (medial, anterior and posterior) "' Chief nutrient foramen: anterior surface.junction of the upper and middle 113 entering in an oblique fashion from distal to proximal ("to the elbow Igo, to the knee I flee") .. Tuberosity and styloid are 180 degrees from each other, and seen only on AP view .. Radial head ossifies at 3-5, fuses by age 6; distal radial epiphysis ossifies at ] 2 months and fuses at 18 years .. Normal angulation of the radial head with respect to the neck is between 0 to 15 degrees laterally and from 10 degrees anterior to 5 degrees posterior ., Lateral 90 degrees of the radius is non-articulating with the ulna, this area is lies roughly between the radial styloid and Lister's tubercle, therefore is a safe location for placement of hardware Ulna Straight, 3 borders (anterior, posterior, interosseous) .. Coronoid and styloid seen on lateral, but not AP X Rays "' Distal ulna epiphysis appears at age 5; fuses at 18 Interosseous membrane " Fibers run obliquely, proximal radius to distal ulria; tightest in neutral Gap proximally for common interosseous artery to split into anterior and posterior, which lie directly on its surface Anomalies Absence of radius (TAR, Holt-Oram Syndrome, Fanconis anemia) Radioulnar synostosis: usually fixed in pronation. Can be bilateral and familial MadeJungs deformity: volar-ulnar deviation of distal radius secondary to growth disturbance of distal radial physis
It II II OJ iii Il
&
Superficial Anatomy o Cutaneous innervation: Lateral antebrachial cutaneous nerve; superficial and lateral to biceps tendon (commonly seen on anterior approach to elbow for biceps repair), terminal branch of musculocutaneous nerve, pierces deep fascia of ann near musculotendinous jxn of biceps and lies in SQ tissues of antecubital fossa Medial antebrachial cutaneous nerve; from medial cord of brachial plexus (commonly seen in medial approach to elbow for ulnar nerve transposition) • Posterior antebrachial cutaneous nerve
II II
61
Fascia • Superficial (tela subcutanea); contains superficial veins (basilic, cephalic, and median veins), cutaneous nerves and lymphatics • Deep {antebrachial fascia); attached to subcutaneous border of ulna and sends septum to radius forming anterior and posterior compartments i) anteriorly and distally it divides into two layers with respect to the PL, FCU, and FCR,superficial portion forms portion of retinaculum over Guyons canal (volar carpal ligament) and deep portion forms transverse carpal ligament (flexor retinaculum) ii) posteriorly it forms the extensor retinaculum (dorsal carpal ligament) with septa to radius and ulna forming six dorsal compartments
Flexor Muscles o 3 layers; superficial, intermediate and deep o Superficial muscle layer • Pronator teres: forms medial border of cubital fossa • origin- two heads, humeral{rnedialsupracondylar ridge, medial intermuscular septum, and common flexor tendon) and ulnar head' (coronoid process), median nerve lies between two heads • insertion-lateral midshaft of the radius • action- pronation and weak elbow flexion • innervation- median nerve (C6,C7:just proximal to where it passes through the muscle • variation- absent ulnar head 9% • Flexor carpi radialis • origin- common flexor tendon and deep fascia
e Hl::;e!
!-,__.c..!
UOH'"
,.,.-
.LL.,
Ul1
gruv-ve-lll-.w:.q.lcL,l-uffillJ.-LO
.~,..._...,-
~r,~""
............:," .........
.,,_
;:':,,\,;U1.1
""' ..... -.-..
.....
lHCI.4Cal jJ4J
~.L.~
~--.'
base • action- wrist flexor • innervation- median nerve (C6, C7),. • variation- flexor carpi radialis brevis may be present, from deep fibro-osseous structures on the radial forearm to insert with the FCR Palmaris longus • origin- common flexor tendon and deep fascia • insertion-flexor retinaculum and palmar aponeurosis • action- weak wrist flexor • innervation- median nerve (C6, C7) • variation- absent 13%,to check if present, have pi. touch thumb to little finger while flexing wrist against resistance
62
Ii!
Flexor Carpi Ulnaris e fibrous arch between two heads forming cubital tunnel for ulnar nerve • origin- two heads, humeral (common flexor tendon, deep fascia, and intermuscular septum on radial side of FeU) and ulnar head (medial olecranon, posterior three fifths of ulna with the FDP • insertion- pisiform co action- wrist flexor and ulnar deviation • innervation- ulnar nerve (e8, Tl)
Intermediate muscle layer • Flexor digitorum superficialis (sublimis) • Functionally four separate muscles, unlike the FDP • origin- two heads with a dense membrane between them, under which.passes the median nerve; humeralulnar head (common flexor tendon, ulnar collateral ligament, medial border of coronoid process) and radial head (proximal two thirds of the anterior radius) • insertion- via four tendons to middle phalanx of digits 2-5 .. action- primary PIP joint flexion • innervation- median nerve (C8, Tl) Deep muscle layer Flexor digitorum profundus • origin- proximal anterornedial one-half to two-thirds of the anteromediaI ulna, interosseous membrane .. insertion- distal phalanx eo action- primarily flex the DIP co innervation- anterior interosseous nerve (e8, Tl) to radial one-half and ulnar nerve to ulnar one-half .. Flexor pollicis longus e origin- radial portion of middle interosseous membrane, middle one-third of radius • insertion- distal phalanx of thumb " action- flex IP joint of thumb • innervation- anterior interosseous nerve via 2 branches • variation- accessory head of origin from common flexor mass (called Gantzer's muscle and present in two-thirds of people) " Pronator quadratus • origin- distal one-fourth of anterior ulna • insertion- distal one-fourth of anterior radius • action- pronation, especially with elbow flexion • innervation- anterior interosseous nerve
II
o'
63
Extensor. Muscles o 3 mus.cle groups: mobile wad of Henry, superficial group from humerus and deep group from radius and ulna o Mobile-wad ~ Brachioradialis • origin- lateral supracondylar ridge (upper 2/3), forms lateral border of cubital fossa • insertion- lateral distal radius • action-elbow flexor, pronator when arm supinated and vice versa • innervation-radial nerve (C5, Co-nerve between brachialis and BR)'~ ,·c·· • Extensor carpi radialis longus • origin- lateral supracondylar ridge • insertion- dorsal base index metacarpal • action- forearm flexor, wrist extensor and radial abductor • innervation- radial nerve (C6, C7, at lateral epicondyle) • Extersor carpi radialis brevis • origin- common extensor origin • insertion-base oflong metacarpal • action- chief neutral strong dorsiflexor of wrist • innervation- radial nerve (C6, C7, can be innervated by PIN approximately 36% of time) , o Superficial group of extensor muscles • Extensor digitorum communis • origin- common extensortendon with origin ofEDM • insertion- central slip to middle-and lateral bands to distal phalanges • action- digit extension, abduction ~ innervation- posterior interosseous nerve (C,6.~ C7, C8, ";IIa 3~4 branches) • Extensor digitorum minimi • origin- septum between EDC and EDM; lateral epicondyle • insertion-little finger extensor mechanism, ulnar to EDC • action-extension of digit and abduction • innervation- PIN (C6, C7, C8) • Extensor carpi ulnaris ~ • origin- two heads; lateral epicondyle and posterior border of ulna and overlying fascia • insertion- medial side base of small metacarpal • action- wrist extension and ulnar abduction • innervation- PIN (C6,C7,C8)
<
64
OJ
Anconeus .. origin- lateral epicondyle e insertion-lateral olecranon; covers posterolateral elbow capsule, annular ligament and proximal ulna .. action- weak elbow extension " innervation- nerve to aconeus from radial nerve which is given off in proximal 113 of arm and passes thru medial head of triceps (C7, C8)
Deep group of extensor muscles "' Supinator " origin- lateral epicondyle, radial collateral and annular ligaments, ulna; thickened edge of proximal border of superficial laminae.is.Arcade of Froshe), under which passes the PIN • insertion- lateral anterior radius • action- supination ~ innervation- PIN' • Abductor poUicis longus .. origin- posterior ulna distal to supinator, interosseous membrane, middle 1/3 posterior radius distal to supinator " insertion-base of thumb metacarpal .. action- extension, radial abduction, external rotation of thumb, radial wrist deviation, wrist flexion " innervation- PIN Extensor pollicis brevis " origin- posterior radius, interosseous membrane distal to EPL " insertion- base of proximal phalanx of thumb .. action- extension of Mep joint of thumb • innervation- PIN Extensor pollicis longus e origin- middle 1/3 posteriorulna and interosseous membrane • insertion- tendon ulnar to Lister's tubricle then to distal phalanx of thumb • action- thumb IP joint extension, thumb retroposition and adduction • innervation- PIN • tendon can rupture secondary to avascular necrosis (chronic attritional rupture) following CoUes Fx " Extensor indicis proprius ., origin- distal to EPL on posterior surface of ulna, interosseous membrane
III II!
65
• • • •
insertion- travels deep/ulnartoEf.C to index finger, to extensor mechanism action- index extension, adduction innervation- PIN (distal branch)
\Tasculature o At the level of the elbow, the brachial artery divides into radial and ulnar branches just distal to it passing deep to the lacertus fibrosis, medial to the biceps tendon o,~fldial Artery ; " • Travels to wrist between the FCR and BRt then deep to APL and EPB into snuffbox • Branches: i) radial recurrent arteryanastamoses with radial collateral branch of profundus brachii alongside the radial nerve ii) muscular branches to forearm muscles iii) superficial palmar branch into thenar muscles iv) palmar carpal branch o Ulnar Artery • Dives deep to the 2 heads of the pronator teres muscle and then joins the median nerve between the two heads of the FDS • Relationship at wrist from radial to ulnar: artery, nerve, FCU tendon. • Branches: irulnar recurrent artery: anterior branch travels anterior to medial epicondyle then anastarnoses with inferior ulnar collateral artery anterior to the elbow; posterior branch travels with Ulnar nerve and anastamoses with superior ulnar collateral artery iijcommon interosseous divides into anterior and posterior branches -anterior: ...travels anterior to the interosseous. membrane between FDP and FPL; median nerve is radial to artery, then with anterior interosseous nerve; provides nutrient branches to radius and ulna and terminates into anterior and posterior branches at the proximal border of the pronator quadratus -posterior: dives deep between oblique cord and interosseous membrane, and provides the primary blood supply to dorsal forearm; reinforced by the anterior interosseous artery at the wrist; recurrent interosseous artery is the branch which travels thru supinator to anastamose with middle collateral branch of profunda brachii artery
66
Nerves o Median nerve (C6, C7, C8) Medial to brachial artery in the cubital fossa, travels between the two heads of the pronator teres and FDS, then deep to the FDS and superficial to the FDP and in distal 1/3 of forearm emerges from beneath the FDS to lie ulnar to the FCR and .radia! to the palmaris longus; " In the antecubital fossa it lies deep to the lacertus fibrosis, medial to the antecubital vein and medial to the brachial artery; only structure more medial in the fossa is the origin of the flexorpronator tendons • Branches: Muscular branch to pronator teres i) To FeR, PL, and FDS ii) Anterior interosseous nerve "- comes off at level of jxn iii) of the two heads of the pronator teres then travels with the anterior interosseous artery on volar surface of 10M and provides innervation to the FPL, PQ, and radial 'ii ofthe'FDP and terminates as sensory fibers to the volar capsule of the carpus Palmar cutaneous branch; from radial side of nerve and IV) on ulnar side of FCR,S5 em proximal to the radial styloid Branches to thenar muscles: APB, OP, superficial head v) of the flexor pollicis brevis Lumbricals 1 and'Z vi) Sensory to skin on lateral side of palm, and the palmar vii) side ofthe lateral 3 and Yt digits, as well as the dorsal side of the index, middle and ring finger Communication with the ulnar nerve is called the Marrin-Gruber anastarnosis viii) motor nerve may cross over from the median to ulnar nerve in the forearm IX) it can occur in two patterns: from median nerve in proximal forearm to ulnar nerve in middle to distal third of forearm, & from Am to ulnar nerve x) occurs in 10-25% of people Other anastomoses between median nerve & ulnar nerve includes xi) motor branch of median nerve to superficial head of FPB & ulnar nerve to the deep head of the FPB xii) anastomosis of median nerve & ulnar motor branches thru first lumbrical or thru innervation of adductor pollicis xiii) branch of median nerve to third lumbrical joining neural branch to this muscle from deep branch of ulnar nerve
IE 111
67
xiv)
xv)
median nerve may also form anastomoses wi branch of radial nerve in the vicinity of APB and have radial nerve innervate this muscle first dorsal interosseous, adductor pollicis, or even abductor digiti minirni may be innervated by the median nerve
o Ulnar nerve' (C7, e8, Tl) • Enters posterior compartment lOcm proximal to medial epicondyle then found posterior to the medial epicondyle at the elbow when it is encased in a fibrous sheath (Osborne's ligament), it enters the forearm between humeral and ulnar heads of the FCU (cubital tunnel) and lies on the anterior surface of the FDP, it is joined in midforeann (~12cm distal to medial epicondyle) by the ulnar artery then a straight course to Guyon's canal • Branches: 2,motorbranches to FCB, 4 em distal to epicondyle, the xvi) motor branches come off posteriorly from the nerve xvii) branch to ulnar 'Ii ofFDP, 6.5 em distal to epicondyle xviii) dorsal cutaneous branch originates 6-8 em proximal to ulnar styloid and emerges from beneath the FCU -Scm proximal to the pisiformand becomes SQ small palmar sensory branch = Nerve on Henle, arises xix) -5-11 em distal to medial epicondy Ie and gives sensation to hypothenar skin terminates in the superficial and deep palmar branches xx) (see wrist and hand chapter) Two connections between ulnar and median nerves xxi) a. Martin-Gruber anastomosis b. Riche-Cannieu anastomosis - corrununication between the palmar cutaneous branches
o
Radial • • • •
nerve (C5, C6, C7, C8) See ann outline Nerve to anconeus given off in mid arm Proximal to the lateral epicondyle, it supplies the BR and ECRL as it lies between the brachialis and BR Divides 1-3cm distal to the lateral epicondyle into xxii) Superficialbranch: may supply the ECRB(58%), travels an the deep surface of the BR to exit at the ulnar aspect in the mid-distal 113 junction (lO em proximal to the radial styloid) between the BR and ECRL, to supply skin over the dorsum of the wrist and hand; need to find branches when placing pins for ex-fix of distal radius fx or release of 1st dorsal compartment
i
68
xxiii)
Posterior interosseous nerve (deep branch of Radial nerve) a. No cutaneous distribution, but supplies the ECRB 36% and enters the supinator muscle under the arcade of Frosbe, then splits just prior to leaving the cover of the supinator into terminalbranches (supplies supinator) b. Located 2 finger breaths distal to the radial. capitellar joint c. Can lie directly on the radius at the level of the tuberosity on the dorsalradial aspect, when the deep and superficial heads of the supinator do not lie on the bone here (25%) d. One major sub-division to superficial extensors: EDC, EDM, ECU) e. Other major branch to the outcroppers (APL, EPL, EPB, ElP) f. The branch to the EDC is recurrent g. Terminal fibers are to either EPL or ElP (varies in the literature) h. Sensory branch to dorsal wrist capsule lies in radial aspect of floor of 4th dorsal compartment
..
Common Forearm Problems o Anterior interosseous nerve syndrome .. Involves motor loss without sensory involvement to the muscles innervated by the AIN (FPL;PQ, radial ~ ofFDP) .. Patients will commonly have forearm pain, no sensory loss Bilateral AIN palsy may indicate Paronage- Turner syndrome (brachial plexus neuritis associated with a virus) " If only FPL is weak, must rule out a Mannerfelt lesion (FPL rupture) Sources of compression include: fiberous bands within the pronator teres, FDS arcade, edge of lacertus fibrosis, enlarged biciptial bursa, Gantzer's muscle (accessory head of the FPL) ., Test the nerve by asking pt to do "OK sign", also called KilohNevin sign (tests FPL) .. Usually tx conservatively, but may occasionally need decompression o Pronator syndrome • Sites of median compression include: supracondylar process (occurs in 1% of population), ligament of Struthers, bicipital aponeurosis, deep to the arch of the pronator teres, under the origin of the FDS, anomalous FPL (Gantzer's muscle) or palmaris profundus or flexor carpi radialis brevis
IJ II!
69
-.r
• •
Differences from CTS (carpal tunnel syndrome) include: sensory disturbance over the distribution of the palmar cutaneous branch of the median nerve; pain in the anterior forearm, Tinel's in the proximal forearm and usually no night symptoms Provocative tests: resisted elbow flexion with forearm supination (bicipital aponeurosis), resisted forearm pronation with elbow extended (two heads of P'T), isolated long finger PIP flexion (FBS origin) Must. order elbow films and get EMG If conservative tx fails, must decompress all potential sites of compression
o o
Cubital tunnel syndrome .. Compression of the ulnar nerve'can occur anywhere from the arcade of Struthers through the cubital tunnel retinaculum to the point where the nerve proceeds through the two heads of the FeU Sites that need to be decompressed • Arcade of Struthers • Medial intermuscular septum • Osborne's ligament • Where it enters between the two heads of Feu • Anomalous anconeus epitrochlearis Presents with parathesias over the small finger and ulnar half of ring finger. Weakness of the intrinsics may cause a positive Froment's sign (PPL compensating for weak hand intrinsics/paralyzed thumb adductor ... have pt hold piece of paper between thumb pad and pad to index finger. ..ifweak or pt uses FPL to trap paper, then positive sign) • Pts commonly have a positive Tinel's sign and symptoms when the elbow is flexed for a minute or more • Sources of compression include: fascial bands, tumors, ganglions, the aneoneus-epitrochlearis, cubitus valgus, bony-spurs and a medial epicondyle nonunion • EMG is helpful in establishing the diagnosis • Treated conservatively if mild, but if weakness is present or there is evidence of hand clawing, tx may become more aggressive • Poor prognosis if there is intrinsic atrophy at time of Dx Ulnar tunnel syndrome: see wrist/hand chapters Posterior interosseous nerve syndrome • Sx include pain at the lateral elbow and weakness with radial drift with wrist extension (EeRL innervated higher than takeoff of PIN) • No sensory fibers for cutaneous innervation, but does have fibers to the dorsal wrist capsule • EMG is usually diagnostic
II II
70
.~ .~
Sites of compression include: thickened fascia at the radiocapitellar joint, radial artery, recurrent Leash of Henry, edge of ECRB, arcade of Frohse and distal edge of supinator Can also be caused from chronic radial head dislocation, fractured radial head or neck, rheumatoid synovitis, ganglion or lipoma .. Conservative tx usually relives sx Wartenberg's syndrome .. Compressive neuropathy of the sensory branch of the radial nerve .. Compressed as it passes between the BR and ECRL and is exacerbated by forearm pronation Some pts have a split brachioradialis tendon and the nerve emerges between the slips making it vulnerable to compression Radial tunnel syndrome • Pain only, without a sensory or motor dysfunction " Same nerve as PIN syndrome and sites of compression, but different response to tx EMG is not helpful .. May be easily confused with tennis elbow (pain with lateral epicondylitis is located at epicondyle versus 6~7cm distal over the belly of the BR with radial tunnel syndrome) .. Difference is that there is maximum tenderness distal to the radial head in a line from the lateral epicondyle through the radial head, to a point 2-3 cm more distal over the radial tunnel • Operative tx is often disappointing (51 % good to excellent results)
II OJ II
"
(>
Fractures o Both bone forearm fxs o Nightstick fxs o Monteggia fxs o Galleazzi fractures o Radial head fx.s o Essex-Lopresti fx Approaches to the Forearm o Anterior approach to the radius (Henry) Incise skin lateral to the biceps tendon, along the shaft of the radius to the styloid process (or as large as you need the incision) .. Internervous plane is between the BR (radial nerve) and the flexor pronator group (median) Incise the deep fascia and develop the plane between the FeR and
II II;
III
BR
II
.,
A leash of vessels are traveling from the radial artery to the BR, which must be cauterized; also retract the superficial radial nerve laterally with the BR muscle Deep, from proximal to distal, lie the supinator, the pronator teres, and FDS and PQ
71
• • •
o
thePT .. '
If proximal access is needed, supinate the arm as the distal origin of the supinator is exposed (protecting the PIN) Middle part of radius can be exposed by detaching the insertion of
More distal, the FDS, FPL and PQ may be taken off the radius to expose it at the appropriate levels.
Posterior approach to the radius (Thompson) Ii Start anterior to the lateral epicondyle and. curve over the dorsal aspect of the forearm to a point just distal to the ulnar side of Lister's tubricle • lnternervous plane • Proximally: ECRB (radial) and EDC (PIN) • Distally: ECRB (radial) and EPL (PIN) • Incise the deep fascia and develop a plane between the ECRB and EDC (identification is easier distal to proximal) • Deep dissection • Proximal 1/3: either identify PIN through arcade of Frohse and retract or supinate the forearm and carefully detach the origin of the supinator muscle • Middle 113: separate the APL and EPB • Distal 1/3: Doing superficial dissection already separates the ECRB and EPL, exposing the lateral border of the radius Exposure to the shaft of the ulna • Incise over the subcutaneous border of the ulna • Internervous plane is between ECU (PIN) and FeU (ulnar n) • Dissect thru common aponeurosis over bone ., Stay on the bone to avoid injuring the ulnar nerve and artery
72
·;:'.
References: • ~
e
Ball eM, GaJatz LM, Yamaguchi K. Elbow emerging concepts. TeL 2002; 51: 61
Instability:
Treatment
strategies
and
II
Browner BD, Jupiter JB, Levine AM, Trafton PG. Skeletal Trauma. Basic science, Jlrflinagement, and Reconstruction. 3rd Edition. Saunders, Philadelphia. Cohen MS, Bruno RJ. The Collateral Ligaments of the Elbow. CORR 2001; 383: 123-130 Cohen MS, Hastings H. Acute Elbow Dislocation: Evaluation and Management. JAAOS 1998; 6: 15-23 Hollinshead, AH: Anatomy for Surgeons. Vol. 3, Harper Row, Philadelphia, 1982. . Hoppenfeld S, deBoer P: Surgical Exposures in Orthopaedics. Approach. Lippincott, Philadelphia, pp 83 -146, 1994. De Jesus R, Dellon AL. Historic Origin of the "Arcade The Anatomic J Hand Surg
.. ..
e
of Struthers".
2003; 28: 528-531
Lubahn JD, Cermak MD, Uncommon Nerve Compression Syndromes of the Upper Extremity. JAAOS 1998; 6:378-386 Lyons TR, Field LD, Savoie III PH. Basics of Elbow Arthroscopy. TeL 2005 Mazurek MT, Shin AY. Upper Extremity Peripheral Nerve Anatomy. Current Concepts and Applications. CORR 2001; 383: 7-20 Mehta JA, Bain G1. Posterolateral Rotatory Instability of the Elbow. JA.A..OS 2004; 12:405-415 Morrey BF. Complex Instability of the Elbow. JBJS 1997; 79: 460-9 Noonburg GE, Baker CL. Elbow Arthroscopy. rCL 2006; 55:87-93 O'Driscoll SW, Jaloszynski R,Morrey BF, An KN. Origin of the medial ulnar collateral ligament. J Hand Surg Am 1992; 17: 164-168 Posner MA. Compressive Ulnar Neuropathies at the Elbow: I. Etiology and Diagnosis. JAAOS 1998; 6:282-288
..
..
e
• ..
II
73
Anatomy of the Wrist
Kevin Malone; M.D. 1. Landmarks a. Dorsal Lister's Tubercle - bony prominence on dorsal aspect of distal radius. Approximately 0.5 em proximal to the dorsal margin of the articular surface of the distal radius. In line with the cleft between the index and long metacarpals. EPL in groove lateral to Lister's, turns radialward just dista1 to Lister's on its way to thumb. ECRB lies just radial to Lister's (Lord Joseph Lister - English surgeon 1827 - 1912). 11. Anatomic Snuff-Box - borders include EPL dorsoulnarly and APL + EPE radially. Contains dorsal branch of radial artery and one or more branches of radial sensory nerve. lll. Lunate Fossa - palpable central depression on dorsum of wrist just ulnar and distal to Lister's. Begins immediately distal to dorsal margin or the radius. Marks the location of the lunate. IV. Styloid Process of Middle Finger Metacarpal- points to the joint between capitate and the trapezoid. Also is just proximal to the point of insertion ofECRB. v. Radial Styloid - palpable both palmar and dorsal to APL and EPB tendons, which course across its apex. VI. Distal Head of Ulna - ulnar head is most visible and palpable in pronation. Ulnar styloid is most visible and palpable in supination. Apex ifTFCC attaches to a sulcus located on the palmar I radial base of the styloid. ECU runs along dorsal aspect of head. b. Palmar 1. Hook of Hamate - located 1 ern radial and 1 em distal to pisiform. Lies between carpal tunnel and Guyon's canal, Landmark for location of ulnar nerve and artery (ulnar to hook) and ulnar boundary of carpal tunnel 11. Scaphoid Tubercle - palpable just distal to distal palmar wrist crease. More palpable with wrist in radial deviation. HI. Pisiform - palpable landmark to locate the FeU tendon, ulnar neurovascular bundle and hook of hamate. IV. Thenar and Hypothenar eminences - Thenar eminence formed by abductor and flexor pollicis brevis, which overlie the opponens pollicis. Atrophy suggests chronic median nerve dysfunction. The hypothenar eminence is formed by the corresponding muscles on the little finger. v. Flexion Creases - skin flexion lines in the vicinity of underlying joints where the skin is attached to the underlying fascia. 1. Thenar crease proximally lies over the scaphoid tubercle then courses over the capitate towards the base of the 3 rd
1.·
74
metacarpal then turns back towards the radial side of the hand outlining the ulnar border of the thenar muscles. 2. Distal wrist crease lies over the proximal carpal row and at the level of the scaphoid waist. Typica!1y the lunate lies entirely proximal to the crease. Ulnarly, the pisiform usually lies directly under the crease. 2. Skeletal Anatomy a. Distal Radius and Ulna - Distal radius has an average radial inclination of 22°, radial length of 11 mm, ulnar variance of 0 ±2 mrn and volar tilt of 11°. (Clinically - these numbers can be altered by fracture and affect carpal mechanics ultimately leading to carpal instability and arthritis. A positive ulnar variance has been associated with Kienbock's disease and carpal abutment.) 1. Scaphoid Fossa (radius) articulates with proximal pole of scaphoid. Extends from radial styloid to interfossal ridge. Triangular shaped. 11. Lunate Fossa (radius) articulates with lunate. Extends from inrerfossal ridge to the sigmoid notch. Quadrangular shaped. Ill. Sigmoid Notch (radius) is area for articulation with the distal ulna. Has a larger arc of curvature than the ulnar head. IV. Distal ulna has no direct articulation with carpal bones. Triangular fibrocartilage (TFC) is interposed in this space.' b. Carpal Bones- eight bones divided into proximal and distal rows. An eight bones compromise the wrist joint - subdivided into radiocarpal joint and midcarpal joint. Proximal row made up of scaphoid, lunate, triquetrum and pisiform, Distal row made up of trapezium, trapezoid, capitate and hamate. All bones in distal row articulate with metacarpal base distally and proximal row bone proximally. Order of ossificationcapitate (2m), hamate (3m), triquetrum (3y), lunate (4y), scaphoid (4-5y), trapezium and trapezoid (4-5y), pisiform (9-12y). 1. Scaphoid - from Greek scaphe meaning light boat (boat shaped) 1. Bony - shaped like a kidney bean, Arises from a single ossification center. Divided into proximal pole, waist and distal pole. Dorsal surface has oblique ridge running from proximal ulnar to distal radial at the level of the scaphoid waist. Ridge serves as attachment site for dorsal capsule and entry site for vessels. 80% surface covered with articular cartilage. 2. Ligaments - radial aspect of scaphoid serves as attachment for radioscaphocapitate, dorsal intercarpal and scaphotrapeziurn-trapezoid ligaments. Palmar surface of proximal pole serves as attachment for palmar region of scapholuate interosseous ligament. Scapholunate interosseus ligament has crescent shaped attachement along ulnar border of proximal pole. Dorsal ridge serves as
'~
75
v. Trapezium - from Latin trapezion meaning four sided 1. Bony - Contains three articular surfaces. Proximal surface for articulation.with scaphoid. Dorsoulnar surface for articulation with trapezoid. Distal surface is saddle shaped and articulates with thumb metacarpal. Anterolateral edge forms an overhang that is part of the fibroosseous tunnel for the FCR.Overhanging ridge also origin of portion of the transverse carpal ligament ". 2. Ligaments - Strong ligament attachments distally that also attach to base of thumb metacarpal. There are no ligaments immediately deep to the APL tendon. Distal and dorsally the dorsoradial and posterior oblique ligaments of the CMC joint attach. Palmar surface serves as attachment for the superficial and deep anterior oblique ligaments (palmar beak ligament) and the palmar trapezoitrapezoid ligament. Only the ulnar collateral ligament of CMC joint covers the distal surface on the ulnar border. Proximally, the scaphtrapeziotrapezoid (STT) ligament partially attaches on the radial surface. 3. Blood supply - multiple nutrient foramina along dorsal, palmar and radial surfaces for branches of the radial artery and palmar and dorsal carpal arches. Dorsal vascular supply is dominant and. there are communications between the dorsal, palmar and radial sources. Vi. Trapezoid - from Latin trapezoides meaning table shaped 1. Bony - From a single ossification center. Articulates with scaphoid proximally, trapezium and capitate on radial and ulnar sides and second metacarpal distally. The ulnar aspect is "notched" to accept the articulation with the capitate. 2. Ligaments - Dorsally the dorsal trapeziocapitate and trapeziotrapezoid the distally oriented dorsal carpometacarpal ligaments attach. The dorsal intercarpal ligament also has attachments to the dorsal surface. Palmarly, a similar set of ligaments are found. In the ulnar "notch" the deep trapeziocaptiate ligament attach. 3. Blood supply - numerous foramina on dorsal and palmar surfaces for branches of the dorsal intercarpal arch, basal metacarpal arch and radial recurrent artery. Dorsal source is dominant and thete is no intraosseous communication between dorsal and palmar sources. VB. Capitate - from Latin caput meaning head 1. Bony - From one ossification center. Largest carpal bone, divided into head, neck and body regions. Head is covered with articular cartilage and convex to fit the concavity of the lunate and scaphoid. Neck is narrowed and exposed to
78
_"'_'~"~"~_"""·""''''''''''''''~'''~'''''_''C
•••
'
..... ,~'".
·~·'···"3:"·~B'lo(ra~supply~-=·Blo()t:rstipp1yff()ih·bfahcnes'offa:dilirarferS"
enter bone along terminal aspect of dorsal ridge. There are also foramens along palmar surface of distal pole. There are very rarely perforating vessels at attachment of scapholunate ligament on proximal pole. Dorsal vascular supply accounts for 70 -: 80% of vascularity, especially to the proximal pole. In 70% of cases, the dorsal vessel arises directly from the radial artery. In 23%, the dorsal vessel arises from the intercarpalarch, No vessels enter the proximal pole at the insertion of the scapholunate interosseous ligament. The palmar artery to the pole provides 20 - 30% of the vascularity, particularly to the distal pole. In 75% of cases, the palmar scaphoid branch arises directly from the radial artery. The other 25% come from the superfi cial palmar branch of the radial artery. There are no apparent intraosseous anastomoses between the palmar and dorsal blood vessels of the scaphoid. 4. Clinical+ Most commonly fractured carpal bone. Fracture classification based on location. More proximal fractures have higher risk of nonunion and A VN because of tenuous blood supply. Bipartate scaphoid _. controversial whether this represents a true congenital development or a pseudarthrosis following a scaphoid waist fracture. Bilateral appearance is more likely congenital than posttraumatic. Lunate - from Latin luna meaning moon 1. Bony - Arises from a single ossification center. Proximal surface convex, distal surface concave. Covered in articular cartilage except for ligamentous insertions. Articulates with scaphoid, radius, TFC, triquetrum and capitate. 2. Ligaments - Palmar surface serves as attachment of the long and short radio lunate ligaments, ulnolunate ligament, and palmar regions of scapholunate and lunotriquetral interosseous ligaments. Dorsal surface serves as attachment to dorsal regions of scapholunate and lunotriquetral interosseous ligaments, and deep fibers of dorsal radiocarpal ligament 3. .Blood supply - perforating vessels insert on palmar and dorsal surface at sites of1igament insertions. Most blood supply within long and short radiolunate ligaments palmarly. 80% from palmar and dorsal sources. 20% from palmar alone. Palmar vessels are consistently larger than dorsal vessels. There are intraosseous communications
attachment for dorsal capsule and dorsal intercarpal ligaments.
11.
76
~ .... -~.+---,"-".-
between palmar and dorsal vessels in one of three patterns. A"Y" pattern is most common (29%) and the base of the Y ~~Y~~~~i~p,~.-.E.~t!B.~: gI~~~tQL"~~I!._ ..;An..:;~'_J:~.~~pa.ttem.:.'O,c"cln:s<jnC", , .. ·'-~"·-:=~~~~'=~~-~~'·--'----30% and consists ofa single palmar and a single dorsal
.. ..... ".c.• ",__
~~.";;.no~~'."~,.~.cr_c._
.•o..•
~.".,·~.<····'~··"·"~;''-'
111.
IV.
vessel.that anastomose with each other. The "X" pattern occurs in 10% and consists of two dorsal and two palmar vessels that anastomose in the center of the lunate. Triquetrum - from Latin term for "threecornered" 1. Bony - Arises from one ossification center. Articulates with pisiform, hamate; lunate. Three tubercles on proximal, ulnar and dorsal surfaces. Proximal tubercle covered with hyalinecartilage for articulation with triangular disc. Other tubercles serve as ligament attachment sites. 2. Ligaments - Dorsal tubercle serves as attachment for dorsal radiocarpal andintercarpal ligaments. Ulnar tubercle attachment site for ulnotriquetral ligament, Triquetrohamate and triquetrocapitate ligaments insert alongpalmar distal edge. The palmar region of the lunotriquetral and ulnocapitate ligaments attach along the palmar and radial edge; Dorsal and-radial edge serves as attachment site for dorsal region of lunotriquetralligament. Horseshoe shaped region of the palmar aspect for attachment of pi sotriquetra 1ligament. 3. Blood supply - blood enters triquetrum through dorsal and ulnar tubercles from branches of ulnar artery, dorsal and palmar intercarpal arches.iMajor blood supply is dorsal along ridge where dorsal ligaments attach. There are intraosseous communications between palmar and dorsal blood supplies. Pisiform - from Latin pisum meaning pea 1. Bony - From a single ossification center. Oval bane with flat articular facet covering distal half of dorsal surface for articulation with triquetrum. Majoraxis of bone is in the proximo distal direction. 2. Ligaments - Completely enveloped in FCU tendon except for lunotriquetral ligament on dorsal surface. Serves as a proximal origin of flexor digiti minimi muscle. 3. Blood supply - encircled by a vascular ring from the ulnar artery. There are two basic networks of vessels, One enters at the proximal aspect at the site ofFCU .insertion. The distal source enters inferior to the facet for the triquetrum. There are communications between the proximal and distal systems.
77
midcarpal joint without any ligamentous attachments. Body has articular surfaces on the radial, ulnar and distal aspects for articulation with trapezoid, hamate and base of third metacarpal. Radial surface is offset to fit in the notch of the trapezoid. 2. Ligaments - Large flat palmar and dorsal surfaces for 'attac1unent sites. No ligaments on the head and neck (allowing for head to rotate up to 1800 when fractured). Dorsally, the dorsal trapeziocapitate and capitohamate ligaments attach and the distally oriented carpometacarpal ligaments. Palmar attachments can be divided into proximal and distal. Proximally the scaphocapitate, radioscaphocapitate, ulnocapitate and triquetrocapitate ligaments attach. Distally, the palmar trapeziocapitate, carpometacarpal and capitoharnate ligaments attach. The deep trapeziocaptiate ligament attaches on the offset radial aspect. There is a recess on the ulnar surface that serves as attachment for deep capito hamate and carpometacarpal ligaments. 3. Blood supply - No foramina on the head of the capitate. Numerous foramina along sites of ligamentous attachments for branches of the palmar and dorsal carpal arches. Major source from dorsal intercarpal and dorsal basal metacarpal arches that insert onto the body and neck. These then branch and travel retrograde towards the head. 4. Clinical - capitate is rarely fractured because of its protected position within carpus. Scaphocapitate syndrome occurs with a fracture of the capitate that results in the proximal capitate fragment rotating 90 - 1800•
VIle
Hamate - from Latin hamulus, meaning hook 1. Bony - From one ossification center. Divided into pole, body and hamulus. Pole is a conical proximally tapering projection that is covered with articular cartilage and articulates with triquetrum, capitate and lunate. The body has two distal facets for articulation with the fourth and fifth metacarpal bases. The radial facet of the body articulates with the capitate. The dorsal and palmar surfaces serve as ligament attachment sites except the most medial aspect of the palmar surface where the hamulus arises. Hamulus forms a palmarly directed projection that curves slightly radially. 2. Ligaments - Palmar capitohamate and carpometacarpal ligaments attach on palmar surface. Triquetrohamate ligament also attaches along the proximal aspect of palmar surface. Dorsal surface serves as attachment site for dorsal
79
.capitohamate and carpometacarpal ligaments. The deep capitohamate ligament attaches in a recess on the radial surface. The-hamulus serves as an attachment site for the pisohamate ligament (extension of the FCU tendon) and the transverse carpal ligament. 3. Blood supply - no foramina on proximal pole of hamate. Rest .of body and hamulus contain numerous foramina. Three major sources: the dorsal intercarpal arch, the ulnar recurrent artery and the ulnar artery. The vessels that enter through the tip of the hook to not anastomose with the vessels in the body and pole and leave a watershed area that is typically at the site of fracture. 4, Clinical- fractures of the hook can occur in sports with racquets, clubs and bats. These can be difficult to diagnose radiographically and often need CT or special views. Untreated fractures can lead to rupture of the small finger profundus tendon and irritation of the deep motor branch of the ulnar nerve. 3. Joint Anatomy - Wrist joint is composed of radiocarpaljoint, midcarpal joints, interosseous joints distal radioulnar joint and joints with the bases of the metacarpals a. Radiocarpal joint - formed by the concave surface of the distal radius and the TFC and the convex surface of the proximal carpal row. There are often communications with the pisotriquetral joint. . b. Midcarpal joint - formed by convex proximal surface of distal row and ; concave distal surface of proximal row. Under normal circumstances there is no communication with the radiocarpal joint or the first CMC joint. c. Interosseous joints 1. Proximal row - small joints that allow motion in the flexionextension.plane between articulating bones. 11. Distal row - cpmplex and rigid joints that allow for less motion between bones in the distal row than is seen in the proxima~w. d. Distal radioulnar joint 1. Osseous anatomy - DRUJ is uniaxial pivot joint between concave sigmoid notch of the distal radius and the convex ulnar head. The distal ulna is covered with articular cartilage for 270° of its, circumference. The radius of curvature of the sigmoid notch is ~ater than that of the ulnar head. Because of this, pronation and. supination of the forearm consist of a sliding motio~ \fotatIOn. There is sigmhcant translation of the distal ulna in ine paImar-dorsal plane because of the differences in the radius of curvature. The maximums of motion have been measured at 2;.8 _E11l1 dorsal and 5.4 mm palmar when the forearm IS l~' I~ion. In this position, 60 - 800 of the ulna is in co~t with ~e
80
sigmoid notch.· 11!~s o£xotation, less than 10% oft4e ulna is in contact ~th the dorsal CiU_QronatiQ12)_or palmar (in supination) margins of the sigmoid notch. The flat distal surface of the ulna is bare of articular cartilage and faces the TFC. There 1s an eccentricconcayity (fovea) at the base of tbe ulnar styloid_ where the TFCand ulnocarpal ligaments attach. This concavity is confluent dorsally onto the head-shaft junction with the groove for the ECU tendon. The ulnar styloid extends distally for a distance of 2 to 6 mm, There are three distinct margins oftbe sigmoid notch: dorsal, palmarand distal. The prominent palmar beak seen on lateral radiographs represents the sigmoid notch and the lunate facet of the distal nid'iuS: Thus a fracture that involves the lunate facet wIll also ll1volve the DRUJ and vice versa. The sigmoid 110tchand the lunate facet of the distal radius are separated by the
T__.
11.
Ligamentous anatomy - Comprised of radioulnar ligaments, TFC and ulnocarpal ligaments J. Radioulnar ligaments - Dorsa! and palmar DRUJ ligaments are the major stabilizers of theDRUJ. ~ form the dorsal and palmar margins of the TFCC between_ the sigmoid notch and the styloid process of the ulna. The palmar DRUJ ligament runs from th~almar margin oUbe sigmoid notch to the fovea at the base of the ulnar stylQU;!. This ligament has connections with the palmar ulnocarpal ligaments. The dorsal DRUJ ligament runs from the dorsal margin of the sigmoid notch to the tip of the ulnar stykilif. This ligament integrates with the sheath of the ECU tendon. 2. Triangular Fibrocartilage Complex (TFCC) - comprised of the TFC and the ulnocarpal ligaments a. Triangular Fibrocartilage (TFC) - arises fTom the distal margin of rue sigmoid DQtch,cups the ulnar .~ ~ect bfthe lunate and the triquetrum and spansJ",o the fovea of the ulnar szyloid with connections to -the palmar and dorsal radioulnar ligamws. ~ Triangular in shape and ~m thick at radial margin and up to 5 mm thick at ulna insertion. Biconcave body for articulation with carpal bones distally and ulnar head proximally is very thin and often referred to as the articular disc. It is made up of chondroid fibrocatilage tissue to bear coinpressive loads as opposed to the lamellar collagen tissue seen in the palmar and dorsal radioulnar ligaments to bear tensile loading~ central area is avascular and has poor to nohealing potential whereas the periphery is well vasculari~d.
81
111.
IV.
h. Ulnocarpal ligaments - arise from thepalmar ;nargin of the TEC, the, palmar radioulnar ligament and .partially from the head of the ulna:-lli!£ common origin with three distinct insertions 1. Ulnolunate - continuous with the short radio lunate ligament and forms a complete p,!!lmar capsule between the TFC and the lunate. 11. Ulnotriquetral - From TFC to palmax: rim of the triquetrum. In 60 - 70% of individuals thefe is a small orifice in the distal substance of the ulnotriquetralligament which lea~ ,- a communication between the railiD.carp.l!J ;Wd pisotriqnetra1 joints. Just proximal and ulnar to this orifice is the prestyloid recess which is lined with synovium and communicates with the underlying ulnar styloid process. 111. Ulnocapitate - from the fovea of the distal ulna to inderdigitate with fibers from the radioscaphocapitate ligament. Runs palmarly to the ulnolunate and ulnotriquetral ligaments. c. Meniscus - When present lies in the ulnocarpal l£int. .It is concave and has a free margin similar to meniscus of knee. When fully developed, it overlies the TFCC and styloid and extends from the dorsal aspect of the TFC to the almar and ulnar'__' as ect e tri uetrum. May contain an ossicle (os lanula) that may be confused or misdiagnosed as a styloid fracture. Arterialanatomy ~ Vascular supply from the anterior interosseous and ulnar arteries. The AlA divides into palmar and dorsal branches proximal to the DRUJ which supply the palm~r and dorsal margins oftheTFC.Dorsal and palmar branches of the ulnar artery supply the ulnar styloid and the ulnar half of the palmar margin of the TFC. Only the outer 15 - 20% of the TFC is Pg!Ytrated by vessels leaving the central area avasc~ DRUJ stability - contributing factors include TFC, ulnocarpal ligaments, radioulnar ligaments, bony anatomy, interosseous membrane of the forearm, extensor retinaculum, dorsal carpal ligament complex and the dynamic forces of the BCU and the PQ.
82
)r
.0:
4. Ligament Anatomy - all are fibrous thjckening!; Gfth.e..fGi111 capsllJes exc.eptfor the mterosseous ligaments be.tw${ffi-eB:Fp@l bORes ofth@ s.ame row. Palmar c3jJsular ligaments are more numerous and stronger than the dm:sal ~arligaments. a. Palmar radiocarpal ligaments - Arise from the palmar margin of the distal radius and course towards the scaphoid, lunate and capitate. They are best appreciated from inside the joint. l. RadioscaphocaRitateligament QZSC) - originates from the radial styloid .Nocess,fonns the radial wall of the radiocarpal joint:-attaches to the scaphoid waist and distal pole, and passes palmar to the capitate head to interdigitate with fibers from the ulnocapitate ligament. Serves as the a)~bumpback" defonnity seen scaphoid fractures. 11. Long Radiolunate ligament (LRI..) - Arises just ulnar to the RSC and passes palmar to the proximal pole of the scaphoid and the scapholunate interosseous ligament to attach to the radial and palmar mar in of the lunate. Has historically beencalled the radio iinotriquetral ligament because of a few insignificant fibers that extend toward the triquetrum. iii. Radioschapholunate ligament - emerges from_palmar margin of radius ulnar to LRL and merges with the scapholunate interosseous ligament to cany blood vessels and nerve fibers from the radial artery and anterior interosseous neurovascular bundle. Very minimal contribution to mechanics of joint. Also know as ligament of Testut. IV. SiiOrf"Radiolunate ligament (SRL) - runs from palmar margin of lunate facet and runs distally to proximal and palmar margin of the lunate. h. Dorsal Capsular ligaments - dorsa] capsule reinforced by two wen defined ligaments. Remainder of capsule is inherently weak. 1. Dorsal Radiocarpal1igament (DlZC) - arises from ~f radius on both sides of Lister's tubercle and attaches to dorsal surface oftrique~m. Also sends some fibers to the lunate as it passes over. 11. Dorsal Intercarpal ligament (DIC) - arises from dorsal surface of .. ~ ,__ the ~trum, crosses the midcarpal joint and_2ends fibers to th,e ~hoid, trapezQid and capitate. c. Ulnocarpal ligaments - see previous section on DRUJ. d. Midcarpal ligaments - run along palmar surface of carpus and rigidly connect bones across a single joint space. I. Scaphotrapezium-trapezoid ligament (STT) - forms the palmar C"apsulebeginning of the STT joint R1!n§._from distal pole of s~ the palmar surfaces of the trapezium and trapezoid. Lies immediately deep to FCR tendon and arthritis and i"hf1ammation of this joint may spread along the FeR tendon and present at tendonitis.
i_;
83
ii. Scaphocapitate ligament .- thick ligament interposed between the ·~d RSC ligament. Runs from scaphoid waist to body capitate, There are no fomYi!1connections between the lunate and the capitate. .. 111. Iriquetrocapit.§,te ligament - analogous to the scaphocapitate ligament. Runs from distal margin of triquetrum to the body of the capitate. IV. Triquetrohamate ligament ~ forms the ulnar wall of the midcarpal joint and is augmented ulnarly by fibers of the TFCC.· e. Proximal Row Interosseous ligaments - Run between the scaphoidlunate and the lunate - triquetrum. They form barriers between the radiocarpal joint and the midcarpal joint. They connect the proximal, palmar and dorsal surfaces of the adjacent bones and leave. the distal edges without ligamentous connections. i. ScaphQlunate interosseous ligament - ThiCKest dorsally. Merges <distally with DIC ligament and proximally with fib;;Cartilaginous membrane of the scapholunate ligament. Fibrocartilaginous membrane forms proximal region ofseapholunate ligament and extends into cleft between scaphoid and lunate, like a meniscus. Palmar! . the se holunate ligament is thin and shares fibers with the RSC ligament. 1l.Lunotriquetral interosseous ligament - Thickest palmarly and interdigitates withfi!?ets ufthe ulnocapi1a!e ligament. Dorsally the ligament is thin and merges wit~e overlying dorsal radiocarpal ligaments. There is a proximal portion analogous to the fibrocartilaginous membrane of the scapholunate ligament. f. Distal Row Interosseous ligaments - Comprise a rigid system of ligaments that link the four bones of the distal row together to move and act as a single unit. ( 1. Trapeziotrapezoid interosseous ligament - Composed of parallel palmar and dorsal sheets of tissue that span from dorsal and palmar cortices of the respective bones. ii. Trapeziocapitateinterosseous ligament - Has palmar and dorsal fibers similar to trapeziotrapezoid ligament but also contains a deep ligament that runs midway between the dorsal and palmar limits of the joint. Roughly 3 m.m in diameter. 111. Capitohamate interosseous ligament - Also contains palmar, dorsal and a deep component that is 5 nun in diameter.
or
W.
5. Retinacular anatomy and the carpal canal a. Flexor retinaculumL Divided into three sections. Proximally it is continuous with the deep investing forearm fascia. The transverse carpal ligament (TeL) represents the central portion and runs from the pisiform and hook of hamate to the tuberosityof the scaphoid and trapezium ridge. This structure serves as the roof of the carpal tunnel. The
84
",
distal portion of the flexor retinaculum is composed of an aponeurosis between the thenar and hypothenar muscles. 11. There are two separate layers of fascia present over the palmar aspect of the carpal tunnel. The superficial layer is the thickened antebrachial fascia proximally and the palmar fascia distally. The deeper layer is the flexor retinaculum (see above). On the radial and ulnar aspects the two layers become separated: Ulnarly, the FeU and ulnar neurovascular bundle run between the two layers. The FCR runs between the two layers on the radial side, 111. The TCL begins on average 11 rnm distal to the capitate-lunate junction and extends an average of 10 mm distal to the CMC joint of the long finger. The mean width of the carpal tunnel is 25 ± 1.2 mm proximally, 20 ± 1.2 rum at the haole of the hamate, and 25 ± 1.5 nun at its distal extent. The TeL is on average 1.5 nun thick. IV . Fibers of the antebrachial fascia are oriented longitudinally and fibers of the TeL are oriented transversely. v. Median nerve compression can occur at one of two locations within carpal tunnel. First at the proximal edge of the TeL where wrist flexion may produce compression (Phalen's test). The second area is adjacent to the hook of the hamate where the TeL has an indentation and the tunnel is narrowest. b. Carpal Canal 1. Bounded by the hook of hamate, triquetrum and pisiform ulnarly; scaphoid, trapezium and FeR tendon sheath radially. The floor is formed by scaphoid, lunate, capitate, hamate and trapezoid. The roof is formed by TeL. 11. Contains FDP and FDS to four fingers, FPL and the median nerve. The median nerve is most palmar structure and the FPL is most radial. The FDS to the long and ring run palmar to the FDS of the index and small fingers. The FDP tendons are the most dorsal structures. The FDP and FDS tendons are covered by a common flexor sheath and theFPL is covered by its O\VI1 synovial sheath. The sheaths begin 2.5 em proximal to the proximal edge of the TeL There can be communication between the sheaths of the thumb and other fingers in Parona's space palmar to the PQ. "Horseshoe abscess" based on proximal connection of thumb and small finger flexor sheaths in Parona's space between PQ and FDP tendons. 111. Carpal tunnel is open proximally and distally but can physiologically act as a distinct compartment from the forearm and hand. When canal pressure rises above a critical threshold, capillary blood flow is reduced in the median nerve and ischemia and irreparable nerve damage may occur.
85
c. FCR ~ Bipennate muscle originating from proximal radius and 10M. Tendon travels ina fibroosseous tunnel formed by distal pole of scaphoid and trapezial ridge and then inserts onto base of index metacarpal. RUhS adjacent to carpal tunnel. STT arthritis can lead to FeR tendonitis. d. FeU - Unipennate muscle originating from medial epicondyle and proximal ulna. Travels between transverse carpal ligament and superficial layer of flexor retinaculum. It is not contained in a fibroosseous tunnel unlike other wrist motors. Inserts onto the pisiform and ultimately continues as the pisohamate ligament. 6. Vascular anatomy a. Carpus - Comprised of three dorsal and three palmar arches that receive contributions from radial, ulnar, anterior and posterior branches of anterior interosseous artery. Arches named based on their relationship to carpal bones and send many communicating branches to each other. All carpal bones receive blood supply from dorsal and palmar entry sites from branches of the arches except the pisiform. There are typically well established intraosseous communications between the dorsal and palmar nutrient vessels. 1. Radial .artery - supplies most consistent carpal blood supply. Gives seven branches as it courses through the anatomic snuff box and over the dorsum of the thumb CMC joint and then terminates into the deep palmar arch. First branch is superficial palmar artery. This leaves 5 - 8 nun proximal to radial styloid and runs between FCRand BR then contributes to superficial palmar arch. Next branch leaves 5 rnm distally and contributes to palmar radiocarpal arch. Third branch originates at level of radiocarpal joint and courses dorsally to run deep to the extensor tendons and contribute to the dorsal radiocarpal arch. Fourth branch originates at level of S:r.joint and directly supplies distal pole of scaphoid and the trapezium before it anastomoses with superficial palmar artery. Fifth branch either originates from radial artery at level of ST joint (75%) or from the dorsal carpal or intercarpal arches (25%). This branch directly supplies the dorsal ridge of the scaphoid, Sixth branch originates over the trapezium and anastomoses with dorsal intercarpal arch. Seventh branch originates over trapezium and supplies dorsal trapezium then travels along the radial aspect of the thumb metacarpal. Radial artery then courses back into the deep palmar compartment of the hand and terminates into the deep palmar arch n. Ulnar artery - Gives offthree major branches at the level of the distal ulna. The first courses around the ulna deep the BCU tendon before it anastomoses with the dorsal radiocarpal arch. Proximal to the ulnar styloid, it gives off a branch to the palmar radiocarpal arch and a branch to the pisiform and triquetrum. Distally, the ulnar artery gives off branches to the palmar intercarpal arch and
86
then a branch that travels ulnarly between the pisiform and hook of the hamate. This gives off small branches to the pisiform and hamate before it courses to the dorsal wrist and terminates into the dorsal intercarpal arch. More distally, the ulnar artery gives off branches to the overlying hypothenar muscles and then gives off a branch those courses dorsally around the base of the fifth Me base before terminating into the basal metacarpal arch. The ulnar artery terminates by sending branches to the deep and superficial palmar arches. 111. Anterior Interosseous artery ~ At the proximal border of the PQ, the AlA bifurcates into dorsal and palmar branches. The dorsal branch penetrates the rOM and anastomoses with the dorsal radiocarpal arch. It may continue past the dorsal radiocarpal arch and give off a branch to the lunate and one that anastomoses with the radial artery branch that supplies the dorsal ridge of the scaphoid. The dorsal AlA then terminates at the intercarpal level by sending branches to the dorsal intercarpal arch and a series of branches that anastomose with recurrent vessels of the basal metacarpal arch. The palmar AlA runs deep to the PQ and contributes to the palmar radiocarpal arch before anastomosing with recurrent vessels from the deep palmar arch. IV. Dorsal Radiocarpal arch - Rresent 80% of the time. Located at the level of the radiocarpal joint deep to the extensor tendons. Provides main nutrient vessels to lunate and triquetrum. Typically receives contributions from radial, ulnar and AlA (see above). v. Dorsal Intercarpal arch - Largest and most consistent of dorsal arches. Runs between proximal and distal rows. Supplies the distal row and with the radiocarpal arch it gives blood to the lunate and triquetrum. Most common arrangement is contributions from radial, ulnar and AlA (53%). Other variations include radial and ulnar alone (20%) and radial and AlA (7%). VI. Basal Metacarpal arch - Smallest and most variable of dorsal arches. Lies distal to CMCs of index to small finger. Is absent in 27% of the time. Most common variation is one that is incomplete ulnarly (46%). Receives contributions from radial, ulnar and AlA arteries and communicates with intercarpal arch to supply the distal carpal row. Also communicates with perforating vessels from the deep palmar arch that run in the second to fourth web spaces between the heads of the dorsal interossei muscles. Ultimately, this arch gives rise to the dorsal metacarpal arteries. VlL Palmar Radiocarpal arch - Lies in the wrist capsule and runs transversely at the level of the distal metaphysis of the radius and ulna. Gives off branches to the lunate and the triquetrum. Most common arrangement is contributions from radial, ulnar and AlA (87%). Other variation is radial arid ulnar arteries (13%).
87
viii. Palmar Intercarpal arch - Present only 53 % of the time. Runs between two carpal rows. Formed by radial, ulnar and ALA in 75% and radial and ulnar alone in 25%. Not a major source of blood for the carpus. IX. Deep Palmar arch - 5 - 10 rnm distal to CMC joints. Most consistently present of all palmar arches and major source of blood for distal row. Receives contribution from radial and ulnar arteries. Sends branches to distal carpal row via the radial and ulnar recurrent arteries and also sends perforating branches through the deep web spaces to communicate with the basal metacarpal arch. Ultimately serves as the origin of the palmar metacarpal arteries. b. Clinical significance of carpal blood supply - Bones with vessels entering on one surface or bones with large intraosseous areas dependent on one artery are at greatest risk for AVN. These include scaphoid (proximal pole), capitate (head) and lunate (when supplied by only one palmar vessel. . 1. Preiser's Disease (scaphoid) - typically associated with a traumatic event that may not present as a fracture. ii. Kienbock's Disease (lunate) - unclear etiology. Several authors . suggest that this is a result of repetitive microtrauma that disrupts the internal vascularity of the lunate. Abnormal radiocarpal loading (as seen in ulnar negative patients) may lead to increased forces across the radio lunate joint and has been shown a causative factor. Those lunates with a single palmar blood supply most at risk. 4 stages: 1) normal radiograph, decreased vascularity on MRI and bone scan. 2) bony sclerosis and collapse of radial border. 3) fragmentation, collapse, loss of carpal height with proximal migration of capitate and scapholunate dissociation. 4) advanced collapse with changes in radiocarpal joint. c. Vascular supply to the distal radius and ulna ~ Consistent blood supply from radial, ulnar, AlA andPl.A. i. Dorsal blood supply - Two compartmental arteries (in the 4th.and 5th extensor compartment) and two intercompartmental supraretinacular arteries (superficial to ER and found between the 1st and 2nd compartment and between the 20d and 3rd compartments) send nutrient vessels into the dorsal distal radius. Dorsal distal ulna supplied by oblique dorsal artery of the distal ulna which is a branch of the ulnar artery. The 1, 2 rCSRA takes off directly from the radial artery about 50 nun proximal to radiocarpal joint. After is crosses the ER, it either rejoins the radial artery in the snuffbox (52%), the dorsal radiocarpal arch or both. This vessel has utility for vascularized bone grafting for carpal bone nonunion and AVN. The 2,3 ICSRA originates from the anterior or posterior division of the ALA. This vessel courses directly over Lister's tubercle and then between the 2nd and 3rd compartments before anastomosing
88
II.
with the radiocarpal arch or the intercarpal arch, The 4th extensor compartmental artery runs with the PIN in the radial aspect of the 4th compartment. This artery is usually a branch of the posterior division of AlA and terminates into the intercarpal arch or radiocarpal arch. The 5th extensor compartmental artery is usually the largest of the dorsal vessels and runs along the radial border of the 5th compartment It is a branch of the posterior division of the AlA and terminates into the intercarpal arch. There are often a number of anastomoses between the compartmental and intercompartmental arteries distal to the extensor retinaculum. Palmar blood supply - Palmar blood to radius and ulna come from one of two transverse arches that course between the radial and AlA artery and between the anterior division of the ALA. and ulnar artery, These arches lie at the level of the PQ.
7. Anomalies
Carpal coalition - typically asymptomatic incidental findings, More common in blacks than whites and bilaterality is common. Lunotriquetral is most common and can be subdivided into fibrous pseudarthrosis, bony bridge or complete fusion. b. Accessory ossicles - Most common is os centrale carpi which is located at the distal and ulnar border of the scaphoid. This represents an anomalous ossification center that fails to fuse with body of scaphoid, Surgical Approaches a. Dorsal Approach - exposes extensor tendons, radiocarpal, intercarpal, metacarpal and distal radioulnar joints, and distal ulna and radius for fracture management. I. Incicion ~ inline with middle finger metacarpal II. Management of the extensor retinaculum depends on type of surgery. ER can be incised and extensor tendons retracted to gain access to a particular location. When going through the 3rd compartment, it is recommended to leave the EPL tendon out of the ER when closing the wound. If larger exposure is needed, the ER can be reflected as a unit from the ulnar aspect of the wrist b. Bowers Approach to the DRUJ - for exposure of the DRUJ, dorsa1 ulnar head and TFCC. L Incision - proximally in line with the ulnar shaft and curves gently around the ulnar head to end at the mid-carpus. Incision lies just dorsal to the dorsal sensory branch of the ulnar nerve which must be identified and protected, 11. The proximal and ulnar half of the ER is released at its ulnar margin and reflected radially to uncover ECU and EDM, EDM is retracted radially to reveal sigmoid notch, To get to the TFCC, the distal and ulnar half of the ER can be divided over the EDM tendon and retracted ulnarly. It is important to restore the anatomic position of the BCU tendon. a.
8.
89
c. Palmar Radial Approach to the wrist -FeR approach as popularized by Orbay.for ORIF distal radius. Can alsobe used for bone grafting the scaphoid. 1. Incision - carried over the FeR tendon and deep dissection between FCRand radial.artery. FDP and FPL retracted ulnarly and PQ is elevated off of radius metaphysis. Avoid taking off the, palmar wrist capsule from the volar margin of the distal radius. The capsule can be incised longitudinally to gain access to the scaphoid. d. Palmar Central Approach to the wrist - for access to the median nerve and lunate facet of the distal radius. i. Incision made over PL if present; otherwise begin at intersection of thenar crease and wrist flexion crease. Carry incision distally to intersection of radial border of ring finger and ulnar border of abducted thumb. Incision should follow contour of thenar eminence. Identify median nerve and palmar cutaneous branch on radial aspect of median nerve. Release-the transverse carpal ligament and gently retract median nerve to either side to reveal flexor tendons. Tendons can be retracted in either direction. Identify ALA. e. Approach to Guyon's-Canal= To expose FeU, ulnar neurovascular bundle, pisiform and hook of hamate .Incision - Along radial border of FCU, across wrist flexion crease and carried distally in the interval between the pisiform and hook of hamate. The ulnar artery lies radial to the ulnar nerve and runs on the deep and radial border of the FeU between the FCU and FDS to the ring and small fingers. Bundle enters the hand superficial to the transverse carpal ligament and radial to the pisiform bone. May need to incise the palmaris brevis and overlying palmar carpal ligament.to continue exposure. See section on palmar hand for details of course and branching of ulnar nerve and artery.
90
The Hand - Dorsal Anatomy
Kevin Malone, M.D.
I. Skin
a. Dorsal skin is thin and pliable due to the lack of fibrous tissue attachments to the underlying fascia. This allows the skin to accommodate flexion of the wrist, MP and IP joints. b. Dorsal skin characteristics make it less likely to form an undesirable scar when placed at right il:.l_!gl~st~n exte'nsion folds.-·· ..---~. --'~"" _
~~
.~
._____,
..
-.-'-~--~- .. .. -.~.-,--.,
2.
Fascia - Six layers a. Two superficial lay_ersco:g~an_~.ous._l}.~.ITI;_~,.4orsal venous network and lymphatics (fatty layer and fibrous layer). '-_~'-"-'-""
b. Two deep layers form c.2_".mpartm~!_§.!:'Q_l1)}cl __.JSJeD~()Ttendons e (extensor
r~iDaculum). The deep fascia is fuseg to index anQJi~le _~Cs and then extends around the hand to become continuous with the thenar and hypothenar fascia in the palm (superficial / supratendinous layer, deep I infratendinous layer). c. Two muscle layers L Intermediate layer between the two deep layers connects and may be the embryologic origin of the extensor tendons. 11. The dorsal interosseous fascia is a_fuin"aud.dissQutiull:2US layer that covers dorsal interossei mu_~k.L__ '-.' ,_ 3. Venous Drainage of the Digits a. Dorsal Digital Veins - more variable than arterial system but still has a fairly consistent pattern. 1!1.ostconsjstenLv.e.ssel.is_.asmalLY~iI)in_th~ dorsal midline 2f111eg!§.!~J]1halaDX-thaLar:borizedover111~surface of the nail mi!.tri~.(dorsal terminal vein). Proximally there are dorsal radial and dorsal ulnar veins that are joined by transverse connections that form a dorsal ladder that ends at the digital cleft Tjl.l:proximal...ar.chJermjE:~!~~jn veins in the dorsal weE.~ces ol'!._~i!her_.~4~_gfJh~_MPj9ints, hich in w turn coalesce to form a venous network on the dorsum of the hand. These vJj:us...co.ru:l:@e{-j3ro.;o;dmaUy..-to.-tllwasilic-an.d-eep.halic_v:einsat the level the wrist There are a number of communicating veins from the superficial palmar venous system that pass obliquely, proximally and dorsally to dump into the dorsal digital system. These communications are largest in size and number at the level of P 1. Entire venous system contains valves that direct blood from palmar to dorsal, distal to proximal and radial to ulnar. The thumb drains into the ceghalic v.r;ejJl_Q!:!t other the m.etacamal venous aicadc:s E!.~~~~eE:!~~!}L~to_~h(;_1?a.~~lic ~~[n-on-the ulnar side of the wri~!_:___._ b. Thumb - dominant palmar veins in pulp and that then drain into dorsal system by way of the 9Jili.g_uecommunicating veins. Many communicating veins found along radial aspect of IP joints (reliable source of veins in replantation surgery). Dorsal system begins at the base
or-"
91
of the nail and coalesce to form >4 at l~vel ofIP. As they move proximally they communicate and decrease in number but increase in size at the level of the MP. c. Clinical significance - Superficial and deep palmar veins and neurovascular bundles are located to escape compression during grasp of pinch. When pressure is applied to palm, blood travels to the dorsal sys~m by comm~cating veins and re.!!~ i~ prevenied-byvaIves. Communicating veinsmciSfnuinerous at P l-leve-fwnlcllIs--area of least compression when making a fist. All veins liiive valves - need to be aware iftak~ng a vein graft for revascularization of digit. 4. Extensor Retinaculum a. Fibrous structure from anterolateral border of the distal radius to the pisiform and triquetrum (does not attach to ulna - would restrict about 30% of rotation). Divided into six fihroosseous tunnels which allow passage of extensor tendons into hand and prevent bowstringing with wrist extension. Divided into supratendinous and infratendinous layers. Infratendinous layers only present in the ulnar three compartments. Radial thfee compartments C1irectlyon dIstal radiUs. Slxdorsal-compartments separated by septa that arise from supratendinous layer and insert onto radius. Histologically, the extensor retinaculum is similar to flexor pulleys and can be used for pulley reconstruction. 1. APL & EPB - form radial border of snuff-box. De Quervain's tenosynovitis (Fritz de Quervain - Swiss surgeon 1868 - 1940) tenosynovitis of first dorsal compartment. Common to have septa between APL and EPB that needs to be released during decompression. Be aware 0_[ multiple slips of APL~d that superficial sensory branch 01' radial nerve often lies directly superficial to this compartment. 11. EeRB & EtRL - ECRL inserts on base of index Me, ECRB onto , ~,-----base of long MC. iu, EPL - wraps around Lister's tubercle on way to base of P2 of thumb. Forms dorsal border of snuff-box. EPL rupture following distal radius fractures typically related to a vascular insult and does not occur acutely after the injury. To test for EPL -lay palm on table and ask patient to lift thumb off table. iv. EDC & EIP - ElP lies deep and ulnar at wrist (ElP muscle belly also found more distally at wrist). Join at extensor hood over index MP. Terminal sensory branch of PIN lies on floor of compartment. EDC to small finger inserts ulnarly to the EDM. Most surgical apProaches to the radiocarpal joints~ through'this compartment. v. EDM - Lays directly over head on distal ulna. EDC to small fing~E-®sent in ~ 50% and very small in ~ 20% of population. Maybe ruptured by synovitis and subluxation ofDRUJ as seen in rheumatoid arthritis (Vaughn Jackson syndrome).
Ire
'.
92
VI.
BCU - Inserts on base oflittle Me. Can sublux over ulnar styloid during pro! sup and be a source of pain and snapping.
5. Extensor Tendons - see forearm section
for discussion on origin, insertion and innervation .. There are multiple described variations of arrangement of extensor tendons and anatomic variants. The most common arrangement is: single ElP inserting ulnar to EDC of index; a single EDC to the index; a single EDC to the 'long; to the ring; abs'ent EDC to tFie sman; a double EDM to the small with dual insertion and connection to EDC of the ring by juncturetendinum. a. Zone·s ofinjury Thumb: ..-----~~-- .. -----~~-.-----.------. ~
doUb1e"EDC
1.
111.
EPL insertion
n, Over P 1 shaft
OverMP joint IV. Over 1i~ft v, Over Carpus Zones of injuryFI~ger i. Lateral band insertion base ofP3 (mallet finger) 11. Over P2 shaft iii. Over PIP joint tv. Over PI shaft v: OverMP joint VI. Over Me shaft VII. Over Carpus VllI. Distal forearm ix. Proximal forearm Extensor Apparatus at ~t - Central slip invests a fibrocartilage pl'!_te just proximal to its insertion on b~of P2 (dorsal plate). Acts to increase stability of the extensor tendon, to increase the movement arm of the tendon (like patella) and prevent attrition of the tendon at its insertion. Juncturae Tendinum - extensor tendons interconnected on dorsum of hand by juncture and intertendinous fascia. The fascia is present between all . tendons in 4 ili. compartment and attaches to the paratenon. Juncturae are narrow connective tissue bands that extend between EDC and EDM (but not ElP). Limit independent extension of ulnar three fingers. Account for finger extension after an extensor tendon laceration. Also can p,revell! proximal migm1iou of telldom; after j§Qtgalion. Sagital Bands - extensor tendon a(MP joint held in place over dorsum of joint by conjoined tendons of the intrinsic muscles and the transverse lamina or sagital band. Sagital bands arise.ir:o.rn_p-almaLplat~andJh~. intennetacarpaUig~Q!S at the neck of the metacarpals. RlJ.~QLthe .. r<!~al sagital bands lead to u~~!.~.'§}J.blu_J£ationf the ~~t~nS_QLtendQnsand o loss of abilIty to act1Ve!yext~n~tMP_j_oints. Sagital bands also prevent bowstringing of11ieextens-ortendons during hyperextension. Functional Dynamics of Extensor Mechanism - Finger extension is complex act and driven by rac,!ia~nnervated extensor tendons and ulnar J median innervated intrinsic tendons. At MP level, intrinsic tendons
b.
c.
d.
e.
f.
93
are volar to axis of joint rotation. At PIP joint they are dorsal to the joint axis. Extensor mechanism at PIPj oint includes trifurcation of the extensor tendon into central slip which attaches to base of P2 and two lateral bands :vhic~xtend and merge to ins~lleCIO£S~I!?i~~.~J}>~~-Lateral "b<i"nds held in position relative to PIP joint by ~sverse retinacular ligaments that originate from flexor tendon sheath. Obli lie retinacUJ.a[·Ilgaments (Landsmeer) run from A3 pulley to lateral bands distal to insertion 0 transverse retinacular ligame1}.!gnd act to llri.kPIP-aiidDIP~moti~n. Extensor mechanism achieves simult;neous PIP and DIP e~ when central slip extends PIP and lateral bands extend DIP. Need to recreate nOID1al alance of central slip and lateral bands during repair to recreate b simultaneous extension of PIP and DIP. There is no direct insertion onto base of PI and MPJ extension is created by extensor tendon excursion which pulls on sagital band and thus extends MP by its insertion onto palmar plate. g. Patterns of Imbalance 1. Boutonniere lesion -central slip disruption and volar migration of lateral bands leads to :PJ,.I> flexiotl and hJlperextension of DIP. Can Occur after laceration or avulsion of central slip, and centr-aJ slip attenuation as seen in inflammatory arthritides. Elson test can be used to diagnose early - PIP joint is bent 90deg over the edge of a table, with resisted P2 extension will also cause rigid extension of DIP because all forces are distributed to the terminal tendon via the intact lateral bands. Proximal migration of extensor mechanism and sagital bands can lead to hyperextension ofMP joints. As condition becomes chronic, transverse and oblique retinacular ligaments become contracted and scarred leading to a fixed deformity, 11. Pseudoboutinniere - PIP flexion contracture with associated restricted flexion of the DIP joint. Usually a result-~nyperextensIOn injury at the PlP-·that leads to inflammation and a c~~tracture of.the retinacula!" ligaments and the pulleys al~~ ultimately a PIP flexion contracture as well as loss of flexion of the DIP because of the contracture of the oblique retinacular ligaments. 111. ~anet fingeC loss of active extension at DIP because of disruption of extensor mechanism insertion into P3. Proximal midline migration oflateral bands brings lateral bands dorsal to axis of rotation of PIP and can lead to attenuation of retinacular ligamel},ts and swan neck deforrniJ;y_ IV. §.wan neck de.foanity - P?sition of PIP hXE~~n and DIP flexion. Seen in conditions when lateral bands move:._dor.§ilLto llxis ohotation of PIP and act to hyp~!e~.:tenilI~ and allow ~E.?_p.p_?sed fl~_I£Jzy FOY.Due to imbalance of forces at PIP]_ Causes include MPJ volar subluxation, mallet finger, laceration ofFDS
t
94
and intrinsic contracture, sYJlovitis ofPIPJ (most common, seen withRA) h. Differential Diagnosis of Extensor Lag 1. Tendon rupture II. MP joint dislocation (unable to passively extend) 111. Sagital band rupture and ulnar subluxation of extensor tendons at MP joints (able to maintain passive extension) IV. Posterior interosseous nerve palsy (tenodesis effect still QresJ~I!_0 v, Trigger finger ' VI. Flexion contracture. vii. Proximal nerve root or eNS lesion 6. Dorsal Nerves a. Radial Nerve (superficial branch) - passes dorsal/ulnar to brachioradialis in distal forearm and gives off multiple branches that provide cuta~~ou~~ innervation to dorsum of hand, thumb, index and radial half of long finger out to the PIP level. Communicates with the lateral anteQ[achiat cl.!.~~eous n_~IY~J9j!lP:~~liJ~:t_h.~r.~9:i(lJ_~i.Q~ .. )fJl1eJhllmb. Can also ( communicate with the dorsal sensory branch of ulnar nerve. Nerve branches sensitive to trauma and pr9pe to develoI!ing painful nel!IQ1}"la.:~. ALea 0 f ~l!ton_9!!!g~s~jf1I.1~~~tio_~j§_9..QnmlJ~!_.welLs.pace. ~.. - .. . b. Ulnar Nerve (dorsal sensory branch) - enters dorsal forearmdeep to FelL. appro~mately 10 cm P!Qximal!C0E.~_ll}!l~~~!:YlqiQ_~gg exte~ds superficial to extensor retinaculum onto dorsum of hand. Supplies sensation to small finger, ring finger and ulnar half of long finger, 7. Dorsal Arteries (radial artery) - radial artery enters the dorsum of the hand proximal to the thumb metacarpal, deep to APL and EPB tendons' in the -a""D.~tomic snuff box. It runs over the dorsum of the trapezium and"fuenruns~hrough-tEe-1Wo heads of the 1sl dorsal interossei muscle to return to the palm. It gives off several branches in the dorsum of the hana~---~------~--~·-"--"-·~--" a. Dorsal radiocarpal arch - runs along the radiocarpal joint line and communicates with the dorsal branch of the ALA and the branch to the dorsal radiocarpal arch from the ulnar artery. b. Nutrient arteries to the scaphoid, trapezium c. Dorsal intercarpal arch - runs along the dorsum of the distal carpal row and communicates with the dorsal carpal branch from the ulnar artery and also the dorsal radiocarpal arch. Provided origin for nutrient arteries to carpal bones and also will communicate distally with the basal metacarpal arch. d. D?rsi!LPollicis artery - alo?:_g ~~~~~lo~()rd~!-2f .~_!h~IJ?~.Q!~_t9:qil,m~L, th~.. ~ e. Basal metacarpal arc11-=runs-:~rongJhe bas~s~Qfth~J~~J().5llimetacarpals and communicates with the dorsal intercarpal arch proximally, ··Thisarch provides the origin for the dorsal ITl~_ta~~lI:pillarteries. I. Three dorsal metacarpal arteries (sec_()!l~L_.t~rd1_tQl:1J1b}GQurse distally in the second, third and fourth interrnetacarpal spaces
95
11.
dorsal to the interossei muscles. The first dorsal metacarpal artery typically arises from radial artery distal to the basal metacarpal arch but just before it runs between the two heads of the 15t dorsal interossei muscle. This artery will branch to send arteries along the ulnar side of the thumb metacarpal and the radial side of the index metacarpal. The fifth dorsal metacarpal artery typically arises from the dorsal carpal branch of the ulnar artery. It passes distally along the ulnar border of the fifth metacarpal and usually extends as far as the PIP joint. At the level of the basal metacarpal arch, there are several communicating branches with the deep palmar arch that run between the two heads of the dorsal interossei muscles near their ongm.
8. Nail Unit a. Nail plate -homologous to the stratum corneum of the epidermis and consists of compacted., keratin filled squames. The lunula is a white opacity immediately distal to the. central aspect of the proximal nail fold and is said to be due to comparatively poor vascularization of the germinal matrix. b. Nail fold - proximally, the nail plate extends under the semilunar nail fold, which is lined with dorsal and palmar epidermis. The stratum corneum layer of the dorsal epidermis extends distally over the nail plate to form the cuticle or eponychium. c. Nail Bed - soft tissue immediately beneath the nail plate that contributes to nail generation and migration. Proximally, it forms the germinal matrix and distally it forms the sterile matrix. The distal margin of the lunula is approximately at the junction between the germinal and sterile matrix. The matrix has longitudinal grooves along the dorsal surface that match a similar pattern on the undersurface of the nail Elate and~a.ya:-roleln nail stabilization. The deep surface of the nail bed is anchorecrio the --,_ Reriosteumofthe distaLp1.1alruTI.The area of epidermis under the distal edge of the nail plate is called the hyponychium and is an important barrier against the entry of bacteria.' 1. A smooth nail bed in essential for regrowth of a normal nail plate. Edges need to be reapproximated primarily. If a scar occurs in the sterile matrix, there will be a groove in the nail. If a scar occurs in the germinal matrix then the nail may be split. d. Blood supply and drainage - arterial blood supply from two dorsal branches from the common palmar digital artery on each side of the finger. The proximal vessel is a dorsal branch to the nail fold and the distal vessel courses along the lateral nail plate margin and sends branches to the nail bed. Venous drainage is by a coalescence of veins in the skin proximal to the nail fold. e. Nerve supply - branches from the paired digital nerves. Most typical pattern included a branch that entered nail bed at the level of the lunula
96
t.
f.
with a second .branch that passed distally to end at the hyponychial area. There are numerous Merkel and Meisner sensory organelles in the nail bed. Nail plate growth - determined by the turnover rate of the germinal matrix, which varies with age, digit (long finger fastest), temperature, season, time of day and nutritional status. Rate of growth is approximately 0.1 mm/day.
9. Dorsal Hand Masses a. De Quervain's Tenosynovitis - tenosynovitis of 1st dorsal c011?~I1~~l_1t b. Dumbbell Tumor - synovitis of the extensor tendons that becomes constricted as tendons pass in extensor compartments, giving it an hourglass appearance. c. Ganglions - cystic swellings that typically arise from underlying joint capsules or tendon sheaths. Most common origin is scapholunate joint. At level of DIP j oi_I1_t.~t~~~e_~e cal~~r.!!_l!9_i?:Us~ys.!§ ~DdncanJeadJQn(;lil plate deformity (under~at~~~ i~_I?!pgr~hi~j()iE!). d. Metacarpal Boss .: prominence of the base'ofthe index and long metacarpals at the insertion of ECRB and ECRL.
10. Anatomic Variations
a. Extensor Medii Proprius - analogous to the ElP in that is has a similar origin but it inserts onto the extensor aponeurosis of the middle finger. Found in ~1O% of hands, typical1Y_geep to EDh Innervated by PIN. b. Extensor Indicis et Medii Communis - anomalous EIP that splits and inserts into both the index and middle fingers. Found in ~ 3%. Split occurs roughly at myotendinous junction. Insertion on the index finger is same as EIP, but ill~~!iion on middle finger {Sinto joint cap~~ieoTMr-' joint. InnerVatedby PIN. .---~-"-.. ... ~ "~"'~--~~', c. Extensor Digitorum-Brevis Manus - aberrant muscle on dorsum of hand, incidence ~3%. Originates from proximal portion of posterior radiocarpal ligament near the lunate and can see fibers coming off distal radius. Inserts onto extensor aponeurosis of index finger. Innervated by PIN. Its presence may alter the presence or morphology of EIP. _.--
97
The Hand - Palmar Anatomy
.Kevin Maione, M.D. 1. Landmarks a. Digital skin creases - distal and middle skin creases are consistently located proximal to their corresponding DIP and PIP joints. The proximal digital skin creases are consistently located distal to the corresponding Mep joints and are at approximate right angles from the longitudinal arc of motion. In the thumb, the IP joint flexion crease is located proximal to the IP joint and the Mep crease is found obliquely and directly over the Mep joint. b. Palmar skin creases - there is significant variability of the proximal and distal palmar creases. The distal crease originates from the ulnar aspect of the palm and travels obliquely and distally across hand. The proximal crease originates from the radial aspect of the palm and travels obliquely and proximally across the hand. A line drawn from the ulnar most aspect of the distal crease to the radial most aspect of the proximal crease will overlie the metacarpal necks in most hands. c. Thenar crease and distal wrist crease discussion in the wrist chapter d. Re1ationship of deeper structures to superficial landmarks - Kaplan' described a system of lines drawn on the palm of the hand that coincide with deeper structures. 1. Kaplan's cardinal line - a line drawn along the ulnar border of the fully abducted thumb represents the deep palmar arch and lies just distal to the transverse carpal ligament.
Digital n. to little finger
Hook of hamate
Deep palmar arch
Cardinal llne
Crest of trapezium
Feu tendon
Ulnar
a. Median n.
98
t.,
.,
2. Skeletal anatomy "', a: Thumb - a continuation of the lateral column of the carpus fanned by the scaphoid and trapezium. The longitudinal axis of these two carpal bones deviates 45° from the axis of the index metacarpal. This position and the configuration of the thumb CMC joint allow for thumb opposition for pinch. b. Fingers - In flexion, the centrally positioned long finger flexes in a line parallel with the long axis of the hand, whereas the index, ring and small fingers converge towards the middle finger. 1. Index metacarpal is longest and has the largest base. The shaft is con caved towards the palm. The ECRL inserts on the dorsal base. The FeR inserts on the palmar base. 11. Long finger metacarpal is similar to the index metacarpal. The ECRB inserts on the dorsal base. lll. Ring metacarpal is shorter and thinner than index and long but is shaped similarly. IV. Small finger metacarpal is the shortest and receives the BCD on the dorsal base. The terminal fibers of the Feu insert on the volar base after first inserting on the pisiform. v. The vo1ar concavities of the metacarpal shafts as well as the arc of motion of the wrist and fingers contribute to create a longitudinal arch of the hand. A transverse.arch is established by the orientation of the carpal bones and the metacarpal shafts and is further exaggerated by the thenar and hypothenar eminences of the hand and the convergent actions of the thumb and small finger. vi. The thumb metacarpal is the most mobile followed by the small and ring metacarpals. The increased motion of these fingers is explained by the anatomy of the CMC joints. vn. There are 14 phalanges in the hand that all have longitudinally concave palmar surface. c. Thumb carpometacarpal joint L Joint type - Classified as a sellar joint, meaning a convex articular surface in one plane and a concave articular surface in anther plane which is orthogonal to the first plane. Motion occurs in primarily two planes (flexion I extension and abduction I adduction) but articular shape also allows for rotation (pronation J supination) which is important in opposition. Sellar surfaces are only truly congruent in one position. in the thumb this position is fun opposition. 11. Joint axes - the axis of flexion I extension lies in the trapezium. The axis of abduction I adduction lies in the base of the thumb metacarpal.
99
Stabilizing ligaments - primary source of stability during pinch and grasp. Loss of ligament support may be primary cause for development of basal joint arthritis. 1distinct Iigaments have been described 1. Superficial anterior oblique Iigament-. tight in extremes of rotation when joint is extended. Also limits palmar subluxation of metacarpal. 2. Deep anterior oblique ligament - also known as palmar beak ligament. Lies immediately deep to SAOL,in an intraarticular position and lies in the concavity of the trapezium. This is the closest ligament to the center of the joint and serves as a pivot point for rotation. Becomes tight in wide abduction and extension as well as in pronation. Works with SAOL to prevent palmar subluxation of metacarpal. This ligament remains attached to the palmar ulnar fragment in a Bennett's fracture. The DAOL and SAOL appear to be the most important in CMC stability and are commonly attenuated in arthritic conditions. 3. Ulnar collateral ligament - extracapsular ligament that is tight in extension, abduction and pronation. Lies immediately ulnar to SAOL 4. Palmar intermetacarpalligament - extracapsular ligament that runs from base of index metacarpal to base of thumb metacarpal. Tight in abduction, opposition and supination. S. Dorsal intermetacarpal ligament= lies immediately dorsal toPIML Becomes tight in pronation and with dorsal! radial translation of the base of the thumb metacarpal. 6. Posterior oblique ligament - lies deep to the EPLtendon as it crosses the joint. Tight in extremes of abduction, opposition and supination and resists ulnar translation of the metacarpal. 7. Dorsoradial ligament - widest and thickest of the capsular ligaments has a narrow insertion on the trapezium and fans out as it inserts on the metacarpaL Tight with dorsal or dorsoradial sub luxating forces in all positions except full extension. Serves mainly as a check-rein to lateral CMC subluxation d. Index to small finger CMC joints 1. The comparative stability of the index and middle finger CMC joints with a more mobile ring and small finger CMC joints can be explained by the way that the bases of the index and middle finger metacarpals are recessed into the distal carpal row. 11. Dorsal ligaments - index to ring finger supported dorsally by two CMC ligaments to each metacarpal while small finger only has one dorsal ligament
Ill.
100
:'~
Palmar ligaments - index and ring finger have two palmar ligaments, middle finger has three and small finger has only one. IV. Interosseous ligaments ---' There are interosseous ligaments between the distal aspect of the capitate and hamate and the adjacent surfaces of the ring and small finger metacarpals. e. Intermetacarpal joints - the second to fifth metacarpal bases articulate with each other by small cartilage covered facets. These articulations are connected by dorsal, palmar and interosseous ligaments. f. Thumb metacarpophalangeal joint 1. Ligaments1. Palmar plate - thick structure runs from metacarpal neck to base of P 1. The collateral ligaments are found on either side. Palmar plate contains radial and ulnar sesamoids that articulate with the palmar surface of the thumb metacarpal. Dorsal surface of sesamoids are covered with hyaline cartilage. The ulnar sesamoid is larger and its exposed palmar surface serves as an attachment for a portion of the adductor pollicis. The radial sesamoid serves as an attachment for a portion of the superficial head of the flexor pollicis brevis. 2. Collateral ligaments - Divided into proper and accessory collateral ligaments. Proper collateral ligaments arise from the posterior tubercle and adjacent pit on the side of the metacarpal bead, and insert on the palmar aspect of the adjacent phalanx. The accessory collateral ligaments span between the cordlike proper collateral ligaments and the palmar plate. The proper collateral ligaments become taut '. in flexion because of the camlike arrangement of the metacarpal head (the palmar surface is wider than the dorsal surface). In contrast, the accessory collateral ligaments are slack in full flexion. ' a. Gamekeepers thumb - injury to the ulnar collateral ligament at the thumb MP joint. Typically the ligament is torn at the distal aspect. This ligament lies deep to the aponeurosis of the adductor pollicis tendon. A significant deforming force will produce a "Stener lesion" where the proximal stump of the UeL is pulled out from under the adductor tendon and will not heal back down to bone without surgery. g. Finger metacarpophalangeal joints i, Ligaments1. Palmar plate - thick structure runs from metacarpal neck to base ofPl. Has a complex attachment to the metacarpal that consists of (a) vertical fibers of the accessory collateral ligaments, which span between the lateral and medial
111.
i
101
margins of the palmar plate and attach to the palmar side of the proper collateral1igaments and the site of origin of the proper collateral ligament; (b) the deep transverse .intermetacarpal ligaments.which are contiguous with the palmar plate on each side; and (c) the obliquely oriented fibers that arise, from the proximal comers of the palmar plate and attach to the interosseous fascia. The palmar plate makes up the dorsal surface of the AI pulley. 2. ' Transverse intermetacarpalligaments - three short, wide fibrous bands connect the palmar plates of the index to small finger MCP joints and prevent the metacarpals from spreading. These are not to be confused with the superficial transverse metacarpal ligaments (a.k.a. natatory ligaments ). 3. Collateral ligaments ~ Like the thumb MCP joint as wen as the IP joints in the hand, the collateral ligaments are divided into proper and accessory collateral ligaments. The proper collateral ligaments arise from the posterior tubercle and adjacent pit on the side of the metacarpal head-and insert on the palmar aspect of the adjacent phalanx. The accessory collateral ligaments are more vertically oriented and course from the proper collateral ligaments to the palmar plate. Like the thumb MCP joint, the proper collateral ligaments are taut in flexion and explain why side to side motion of the MCP joints is limited in flexion and free in extension. This is also why Mep joints should be immobilized in flexion. h. Proximal interphalangeal joint 1. Joint type ~ uniaxial hinge joints. Unlike MCP joints the PIP and DIP joints are stable in all positions because of strong and symmetric proper collateral ligaments, the palmar plate, and the osseous architecture in the form of side by side concentric condyles that articulate with matching glenoid concavities .. 11. Ligaments1. Palmar plate / check-rein ligament - runs from neck of PI to base ofP2. The attachment on P2 is confluent with the . attachment of the collateral ligaments. The attachment on PI (the check-rein ligament) arise from bone and begin just inside the distal edge of A2 pulley. The origins of the Cl pulley are on the outside of the A2 pulley. Branches of the digital arteries travel deep to the check-rein ligaments to reach the vincula for blood supply to the flexor tendons. The major static resistance to hyperextension is provided by the confluent distal lateral insertion of the palmar plate and collateral ligament complex where it cups the flared margin of the phalangeal condyle. The palmar plate and
102
I.
collateral ligament complex insertion onto the middle phalanx must be disrupted to allow for dorsal dislocation. 2. Collateral ligaments - The proper collateral ligaments arise from a concave fossa on the lateral aspect of each condyle and pass obliquely to insert on the palmar side of the middle phalanx and the distal/lateral margin of the palmar plate. The accessory collateral ligaments span from the proper collateral ligament and the palmar plate. The collateral ligaments are equally tight in flexion and extension. The PIP joints should be immobilized in fun' extension to avoid flexion contractures that may arise from hypertrophy and contracture of the check-rein ligaments. Distal interphalangeal joints - essentially similar to the PIP joints but allow for hyperextension during forceful pinch.
3. Arterial supply in hand - There is significant variability in the blood supply to the hand and the relative dominance of the superficial and deep palmar arches. Most of the blood supply comes from the radial and ulnar arteries. Other sources include the median artery (exists-in 10%, and the interosseous arteries. See other chapters for discussions on the carpal arches and dorsal metacarpal arteries. a. Radialartery- At the level of the radial styloid, lies on the radial side of FeR and gives off a palmar carpal branch and the superficial palmar artery. The main component of the radial artery passes dorsally beneath the APL and EPB tendons to enter the anatomic snuffbox. At this level it gives off the dorsal carpal branch and then runs distally beneath the EPL and courses to the palm through the 1st dorsal interosseous muscle and ends as a contributor to the deep palmar arch: b. Ulnar artery - Courses in the distal forearm radial to the ulnar nerve and in the interval between the FeU and the FDS to the ring and small fingers. It enters the hand with the ulnar nerve on top of the transverse carpal ligament and radial to the pisiform inGuyon's canal. The artery gives off a branch in the canal that supplies thehypothenar muscles. More distally, the deep branch of the ulnar artery arises and runs dorsally between the flexor sheath of the small finger and the flexor digiti minimi to join the course of the deep motor branch of the ulnar nerve in the mid-palmar space (the deep motor branch of the ulnar nerve arises more proximally in Guyon's canal (see description of Guyon's canal in section on ulnar nerve) and dives dorsally under the fibrous arch of the FDM to enter the midpalmar space more proximally than the deep arterial branch}. Just distal to the branch to the deep arch, the ulnar artery gives off the proper digital artery to the ulnar border of the small finger. The main stem of the ulnar artery then turns radially to cross the palm as the superficial palmar arch. c. Superficial palmar arch - Termination of the main stem of the ulnar artery. May receive contribution from superficial palmar branch of radial artery. Lies beneath the palmar fascia and superficial to the FDS tendons. Gives rise to three common palmar digital arteries that goto the three digital web
103
Você também pode gostar
- 1 - Head and Neck Anatomy Review LiteDocumento34 páginas1 - Head and Neck Anatomy Review LiteDiana MitreaAinda não há avaliações
- Hip Joint Anatomy - Overview, Gross AnatomyDocumento14 páginasHip Joint Anatomy - Overview, Gross AnatomyZuraedha ZamilAinda não há avaliações
- St. Luke's College of Medicine - William H. Quasha Memorial: AnatomyDocumento4 páginasSt. Luke's College of Medicine - William H. Quasha Memorial: AnatomyMavic VillanuevaAinda não há avaliações
- Gross Anatomy-Review NotesDocumento56 páginasGross Anatomy-Review NotesJohnAinda não há avaliações
- 9.gluteal RegionDocumento43 páginas9.gluteal RegiondenekeAinda não há avaliações
- PONS: NeuroanatomyDocumento20 páginasPONS: NeuroanatomyHassan IlyasAinda não há avaliações
- Upper Limbs NOTES - BRS Anatomy, Table of Muscles and BRS Questions With Answers ExplainedDocumento14 páginasUpper Limbs NOTES - BRS Anatomy, Table of Muscles and BRS Questions With Answers ExplainedJustyna PoznanskaAinda não há avaliações
- Elbow Complex (Kinesiology)Documento2 páginasElbow Complex (Kinesiology)Kimmybee Garcia50% (2)
- Gross Anatomy of Fourth VentricleDocumento16 páginasGross Anatomy of Fourth VentricleRafique AhmedAinda não há avaliações
- Axillary Artery: Branches First (1 Branch) Second Part (2 Branches) Third (3 Branches) 1 2 4Documento14 páginasAxillary Artery: Branches First (1 Branch) Second Part (2 Branches) Third (3 Branches) 1 2 4foster18Ainda não há avaliações
- Nerves in Lower LimbDocumento21 páginasNerves in Lower LimbTom WuAinda não há avaliações
- Thoracic and Lumbar Spine Anatomy: DR .S.NizamudeenDocumento57 páginasThoracic and Lumbar Spine Anatomy: DR .S.NizamudeenPogo LocoAinda não há avaliações
- BIO 201 Upper Limbs Muscles of The Upper Limbs Brachial PlexusDocumento5 páginasBIO 201 Upper Limbs Muscles of The Upper Limbs Brachial PlexusKelly TrainorAinda não há avaliações
- Gross Anatomy of Posterior Compartment of The ThighDocumento20 páginasGross Anatomy of Posterior Compartment of The ThighOnah ArinzeAinda não há avaliações
- Histology Practical Manual Part 1 2021Documento124 páginasHistology Practical Manual Part 1 2021khushikumari1407Ainda não há avaliações
- Muscles of The Neck PDFDocumento1 páginaMuscles of The Neck PDFEdreyn DellosaAinda não há avaliações
- Nervous Tissue NotesDocumento3 páginasNervous Tissue NotesTulibas Karl Jade J - BSN 1EAinda não há avaliações
- Aldwin A. Yaneza, MD Course Director. Gross AnatomyDocumento40 páginasAldwin A. Yaneza, MD Course Director. Gross AnatomyfilchibuffAinda não há avaliações
- St. Luke's College of Medicine - William H. Quasha Memorial: PhysiologyDocumento3 páginasSt. Luke's College of Medicine - William H. Quasha Memorial: PhysiologyMavic VillanuevaAinda não há avaliações
- Anterior Compartment of Arm & Cubital FossaDocumento24 páginasAnterior Compartment of Arm & Cubital FossaSky StoneAinda não há avaliações
- HSB - Head: Anterior: Supraorbital Margin Posterior: Superior Nuchal LineDocumento19 páginasHSB - Head: Anterior: Supraorbital Margin Posterior: Superior Nuchal LineRaki IliganAinda não há avaliações
- Brainstem (Pons, Medulla, Midbrain) : Dr. MariaDocumento23 páginasBrainstem (Pons, Medulla, Midbrain) : Dr. MariaMuhammad Mustaqeem100% (1)
- SGDDocumento7 páginasSGDJanine Vega Calayo100% (1)
- Surface Anatomy of HeartDocumento23 páginasSurface Anatomy of HeartKhush Bakht100% (1)
- Anatomy TMJ CinioDocumento3 páginasAnatomy TMJ CinioGren May Angeli MagsakayAinda não há avaliações
- 15 PharynxDocumento9 páginas15 Pharynxapi-3757921Ainda não há avaliações
- Histology PlacentaDocumento26 páginasHistology Placentakhiks34100% (2)
- Bone Marking Table KpattonDocumento4 páginasBone Marking Table Kpattonapi-255334265Ainda não há avaliações
- Shoulder Dislocation Case FileDocumento2 páginasShoulder Dislocation Case Filehttps://medical-phd.blogspot.comAinda não há avaliações
- H 4.2 Histology Urinary SystemDocumento52 páginasH 4.2 Histology Urinary SystemF N100% (2)
- Vertebral Arteries, and Their Divisions. Arteries Fuse To Form The Basilar ArteryDocumento6 páginasVertebral Arteries, and Their Divisions. Arteries Fuse To Form The Basilar Arterymurali_bharadwazAinda não há avaliações
- The Axilla: Norah AlmudawiDocumento14 páginasThe Axilla: Norah AlmudawiF-med440 imamAinda não há avaliações
- Upper Limb Exercise - LamuDocumento2 páginasUpper Limb Exercise - LamuLem A SharAinda não há avaliações
- Immobilization SyndromeDocumento2 páginasImmobilization SyndromeJuanitoCabatañaLimIII0% (1)
- ANATOMY: Pelvic 2Documento16 páginasANATOMY: Pelvic 2Nur Liyana MohamadAinda não há avaliações
- Gross Anatomy (Lower Limb)Documento11 páginasGross Anatomy (Lower Limb)toogaa7537Ainda não há avaliações
- Intramedullary Spinal Cord TumorsDocumento7 páginasIntramedullary Spinal Cord TumorsmutalimAinda não há avaliações
- Nerve Injuries of Upper Limb: Dr. Mujahid KhanDocumento41 páginasNerve Injuries of Upper Limb: Dr. Mujahid KhanElton NdhlovuAinda não há avaliações
- Bilaminar and Trilaminar Germ DiscDocumento40 páginasBilaminar and Trilaminar Germ DiscjabirAinda não há avaliações
- Muscle Origin Insertion Innervation Blood Supply Action: Hip and ThighDocumento6 páginasMuscle Origin Insertion Innervation Blood Supply Action: Hip and ThighAndika Anjani AgustinAinda não há avaliações
- 397.001 - Orthopedics) Rotator Cuff TearDocumento11 páginas397.001 - Orthopedics) Rotator Cuff Tearvkpremiyahoo.comAinda não há avaliações
- A Guide To LU3 PDFDocumento54 páginasA Guide To LU3 PDFMigs MedinaAinda não há avaliações
- Ultrasound of The Ankle: IndicationsDocumento6 páginasUltrasound of The Ankle: IndicationsElloide PajutanAinda não há avaliações
- Cranial Nerves DiagramDocumento15 páginasCranial Nerves DiagramSpellkingAinda não há avaliações
- Ankle Joints and LigamentsDocumento8 páginasAnkle Joints and LigamentskristinaAinda não há avaliações
- DR Bhatia Medical Coaching Institute: NeuroanatomyDocumento3 páginasDR Bhatia Medical Coaching Institute: NeuroanatomyAastha JainAinda não há avaliações
- Lower Limb Lab SheetDocumento3 páginasLower Limb Lab SheetKelly TrainorAinda não há avaliações
- L15 CerebrumDocumento27 páginasL15 CerebrumEvilneko1Ainda não há avaliações
- Brachial Plexus: Summary Mnemonics Clinical RelationsDocumento19 páginasBrachial Plexus: Summary Mnemonics Clinical RelationsGulmehr NoorAinda não há avaliações
- Histology Notes 2Documento13 páginasHistology Notes 2Lukas BüchlerAinda não há avaliações
- Peritoneal Anatomy Lecture NotesDocumento4 páginasPeritoneal Anatomy Lecture Noteschc300Ainda não há avaliações
- Chapter 10 - The Lower Limb: Snell 9 EdDocumento138 páginasChapter 10 - The Lower Limb: Snell 9 EdFerjie Angelica DalandaoAinda não há avaliações
- General Histology PDFDocumento110 páginasGeneral Histology PDFrudra narayanAinda não há avaliações
- Anatomy-1 PDFDocumento50 páginasAnatomy-1 PDFSaransh Ghimire100% (1)
- Muscles ShoulderDocumento3 páginasMuscles ShoulderGreys SalacupAinda não há avaliações
- Upper Extremity (Anatomy)Documento17 páginasUpper Extremity (Anatomy)Margareth Christine CusoAinda não há avaliações
- Biochemistry FinalsDocumento11 páginasBiochemistry FinalsKc CalderonAinda não há avaliações
- Anatomy of Spinal CordDocumento3 páginasAnatomy of Spinal CordHamed SabryAinda não há avaliações
- The Shoulder Anatomy & Approaches: Abdulaziz F. Ahmed, MBBS PGY-2Documento61 páginasThe Shoulder Anatomy & Approaches: Abdulaziz F. Ahmed, MBBS PGY-2Abdulaziz Al-Akhras100% (1)
- BonesDocumento27 páginasBonesADELAJA SAMUELAinda não há avaliações