Escolar Documentos
Profissional Documentos
Cultura Documentos
Chronic Osteomyelitis (M&R)
Enviado por
RizMarieDescrição original:
Direitos autorais
Formatos disponíveis
Compartilhar este documento
Compartilhar ou incorporar documento
Você considera este documento útil?
Este conteúdo é inapropriado?
Denunciar este documentoDireitos autorais:
Formatos disponíveis
Chronic Osteomyelitis (M&R)
Enviado por
RizMarieDireitos autorais:
Formatos disponíveis
Introduction M.I, a 35 year old male, was involved in a vehicular accident.
He was admitted on November 19, 2010 at Armed Forces of the Philippines Medical Center. He had severe injuries on his left lower extremity. Patient was immediately brought to a private hospital wherein Xray done. The xray showed fracture of the left tibia and fibula. Patient underwent scenes of operations, which he tolerated well without any transverse affect. His initial diagnosis was Chronic Osteomyelitis, tibia , left, resolved, non-union fibula, left; infected wound at left iliac area. As student nurses, we will study this case in order to be familiar with the manifestations of Osteomyelitis and how we will able to help the patient to be independent in performing activities of daily living within capabilities. Pathophysiology Over 50% of bone infections are caused by Staphylococcus aureus. Other pathogens that are frequently found in osteomyelitis include gram-positve organisms that include streptococci and enterococci, followed by gram-negative bacteria that include Pseudomonas species. The initial response to infection is inflammation, increased vascularity, and edema. After 2 or 3 days, thrombosis of the local blood vessels occurs, resulting in ischemia with bone necrosis. The infection extends into the medullary cavity and under the eriostemon and may spread into adjacent soft tissues and joints. Unless the infective process is treadted promptly, a bone abscess forms. The resulting abscess cavity contains dead bone tissue, which does not easily liquefy and drain. Therefore, the cavity cannot collapse and heal, as it does in soft tissue abscesses. New bone growth forms and surrounds the squirm. Although healing appears to take
place, a chronically infected sequestrum remains and produces recurring abscessess throughout the patients life. The onset of chronic osteomyelitis may be insidious, taking months or even years to develop. It is diagnosed when there is a relapse of a previously treated or untreated infection, if clinical signs persist after 10 days and there is an associated bone necrosis. The presence of a Brodies abscess on X-ray increases the risk of repeat infections. The abscess forms when an infected area is partly overcome by the bodys defences, leaving a pocket of infected material dormant within an abscess lined by cortical bone. The high risk of bone and soft tissue destruction requiring extensive surgery and long-term therapy indicates the need for patients to be referred to specialist centers for treatment. When the infection is blood borne, the onset is usually sudden, occurring often with the clinical and laboratory manifestations of sepsis. The systemic symptoms at first may overshadow a=the local signs. As the infection extends through the cortex of the bone, it involves the eriostemon and the soft tissues. The infected area becomes painful, swollen, and extremely tender. The patient may describe a constant, pulsating pain that intensifies with movement as a result of the pressure of the collecting purulent material. When osteomyelitis occurs from spread of adjacent infection or from direct contamination, there are no symptoms of sepsis. The area is swollen, warm, painful, and tender to touch. The patient with chronic osteomyelitis presents with a nonhealing ulcer that overlies the infected bone with a connecting sinus that will intermittently and spontaneously drain pus. Nursing Physical Assessment
M.I. was conscious, coherent, and not in cardio respiratory distress. The patient has anicteric sclera, pink palpebral conjunctiva, and moist buccal mucosa. He has symmetrical chest expansion, clear breath sounds without restrictions. On his left lower extremity, there is an infected wound with 1x1cm round with regular borders and bloody, purulent discharge on left iliac area. There are irregular shapes scar measuring 10x10 cm on anterior aspect of left leg. There is also a 20cm vertical surgical scar on lateral aspect of leg. Positive bony deformity on left knee. There is pain, tenderness and loss of motion on left lower extremity. There is no sensor motor deficit. Pulses are full and equal. His height is 55ft and weighs 170 lbs. Patients vital signs were 36.5 degree Celsius for temperature, 110/80 mmgH for blood pressure, 82 bpm for pulse rate, and 20 bpm for respiratory rate. Related Treatments The patient was requested to have an MRI (Magnetic Resonance Imaging) to reveal tissue edema, areas of periosteal elevation, and if the bone necrosis are evident. In this case, the patient was done an MRI on his left knee. It shows an altered configuration in the anterior aspect of the lateral femoral condyle, latreral tibial condyle, intercondylar region with cortical irregularities, low signal foci, and minimal edema in the bone marrow. There is a minimal joint effusion. Blood culture and sensitivity was also done to reveal leukocytosis. RBC and WBC count was normal. ESR was 15mm/hr, which was found normal. There was a light growth of Staphylococcus Aureus. Also sensitivity test was done to eliminate resistant medications. He was drug-resistant to Erythromycin, Penicillin, Vancomycin, Clidamycin, and Cloxacillin.
On 19 November 2010, he was given Ciprofloxacin 400mg via IV OD. On 07 January 2011, his IV taken off and was given Ciprofloxacin 500mg tablets every 12 hours for 14 days. He has no allergies to latex, iodine, or adhesives. Nursing Diagnosis M.I nursing diagnosis is impaired physical mobility related to the pain or discomfort due to the presence of wound. The patients left lower extremity has an infected wound (1x1 cm, round with regular borders, with bloody, purulent discharged) on the left iliac area. He has an internal fixator in the tibial diaphysis. After a few months, he was done a would culture and detected a light growth of staphylococcus aureus. This shows an infection in his wound that needs to be controlled. Nursing Diagnosis: Impaired mobility related to pain or discomfort due to the presence of wound. Expected Outcome: Patient verbalizes relief or reduction in pain and appears comfortable. Actions/Interventions: Immobilize limb. Use care and support when moving affected extremity. Rationale: Motion can aggravate pain. y Encourage patient to verbalize pain and discomfort. Observe for body language and facial grimace. Rationale: This aid the assessment of the location, quality, and intensity of pain. y Perform the prescribe treatment regimen for the underlying condition. Rationale: To assess the effectiveness of the treatment.
Encourage the patient in active movements by using assistive devices. Rationale: To increase muscle tone.
Implement ROM exercises every shift after pain medication unless medically contraindicated; progress from passive as tolerated. Rationale: This prevents muscle atrophy and joint contracture.
y y
Reposition patient every 2 hours. Rationale: To prevent skin breakdown. Encourage patient to verbalize feelings and concerns about his altered state of mobility. Rationale: To reduce anxiety and promote compliance. Nursing Intervention According to Brunner & Suddarths, the nursing intervention is monitoring the patients
response to the antibiotic therapy and observers the IV access site for evidence of phlebitis, infection, or infiltration. With long-term, intensive antibiotic therapy, the nurse monitors the patient for signs of super infection. If surgery is necessary, the nurse takes measures to ensure adequate circulation to the affected area (wound suction to prevent fluid accumulation, elevation of the area to promote venous drainage, avoidance of pressure on the grafted area), to maintain needed immobility, and to ensure the patients adherence to weight- bearing restrictions. The nurse changes dressings using aseptic technique to promote healing and to prevent crosscontamination. The nurse continues to monitor the general health and nutrition of the patient. A diet high in protein promotes a positive nitrogen balance and healing. The nurse encourages adequate hydration as well.
Evaluation Caring for a patient with chronic osteomyelitis posses a challenge for the nursing team. The patient can have a lenghtly hospital stay, repeat admissions or required an extensive period of care at home. They can be faced with changes in their body image from the surgery, scarring or amputation of the affected limb. The pain experienced will become chronic in nature, requiring different approaches to pain management to enable the patient to come with the potentially long-term condition and possible disability. Recommendations The patient and family should be taught about the importance of strictly adhering to the therapeutic regimen of antibiotics and preventing falls or other injuries that could result in bone fracture. The affected part may be immobilized with a splint to decrease pain and muscle spasm. The wounds are frequently very painful and the extremity must be handled with great care and gentleness. Elevation reduces swelling and associated discomfort. Pain is controlled with prescribed analgesic agents and other pain-reducing techniques. Improving physical mobility restrict activity. The bone is weakened by the infective process and must be protected by immobilization devices and b avoidance of stress on the bone. The patient must understand the rationale for the activity restrictions. The joints above and below the affected part should be gently moved through their range of motion.
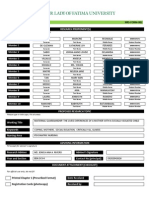
OUR LADY OF FATIMA UNIVERSITY MAIN CAMPUS VALENZUELA CITY
CHRONIC OSTEOMYELITIS
Submitted to: Ms. Barrio Submitted by: Austria, Rizza Marie A. Bacsa, Maycinth Katherine A. BSN 3y3-4 07 February 2011
References Brunner & Suddarth 12th Edition, Chronic Osteomyelitis. Volume II. Page 2069-2072. Steven Schmitt, MD. Chronic Osteomyelitis. http://www.merckmanuals.com/home/sec05/ch065/ch065b.html. Wikipedia. Chronic Osteomyelitis http://en.wikipedia.org/wiki/Osteomyelitis Avigdor Heyroni, MD and Benjamin Z. Koplewitr, MD, Bone with Bone Chronic Osteomyelitis. The New England of Journal of Medicine.
Você também pode gostar
- Common Lab Values With Normals and Critical Values PDFDocumento2 páginasCommon Lab Values With Normals and Critical Values PDFRizMarie100% (7)
- Fluids and ElectrolytesDocumento6 páginasFluids and ElectrolytesRizMarie100% (1)
- Testing StrategiesDocumento1 páginaTesting StrategiesRizMarie100% (2)
- CNS Stimulants and Depressants PDFDocumento5 páginasCNS Stimulants and Depressants PDFRizMarie100% (1)
- RESPIRATORYDocumento3 páginasRESPIRATORYRizMarie67% (3)
- ONCOLOGYDocumento6 páginasONCOLOGYRizMarie100% (2)
- Chronic Arterial Vs Chronic Venous PDFDocumento1 páginaChronic Arterial Vs Chronic Venous PDFRizMarieAinda não há avaliações
- NEUROLOGICALDocumento3 páginasNEUROLOGICALRizMarie100% (4)
- Psychiatric NursingDocumento5 páginasPsychiatric NursingRizMarie100% (4)
- ORTHODocumento2 páginasORTHORizMarie50% (2)
- Pathophysiology: Our Lady of Fatima UniversityDocumento2 páginasPathophysiology: Our Lady of Fatima UniversityRizMarieAinda não há avaliações
- RenalDocumento3 páginasRenalStefanie HenryAinda não há avaliações
- PEDIATRICSDocumento5 páginasPEDIATRICSRizMarie75% (4)
- ENDOCRINEDocumento5 páginasENDOCRINERizMarie100% (3)
- FINALTHOUGHTSDocumento5 páginasFINALTHOUGHTSRizMarieAinda não há avaliações
- TestDocumento6 páginasTestRizMarieAinda não há avaliações
- BURNSDocumento4 páginasBURNSRizMarie100% (2)
- CARDIODocumento7 páginasCARDIORizMarie100% (7)
- MANAGEMENTDocumento3 páginasMANAGEMENTRizMarie50% (4)
- NP Test - 350 Items Key AnswerDocumento56 páginasNP Test - 350 Items Key AnswerRizMarie100% (1)
- NELEC2Documento2 páginasNELEC2RizMarieAinda não há avaliações
- ACIDDocumento2 páginasACIDRizMarie100% (2)
- Thesis FrontDocumento2 páginasThesis FrontRizMarieAinda não há avaliações
- C CCC CCCCCC C C C (C C+ CCC CC) Cãc CCCCC CC CC, CCCC C (C C) CC CC CCCC CC C CC C C (CC) CDocumento5 páginasC CCC CCCCCC C C C (C C+ CCC CC) Cãc CCCCC CC CC, CCCC C (C C) CC CC CCCC CC C CC C C (CC) CRizMarieAinda não há avaliações
- NRes FormDocumento1 páginaNRes FormRizMarieAinda não há avaliações
- Asian CivDocumento4 páginasAsian CivRizMarieAinda não há avaliações
- The Yellow House: A Memoir (2019 National Book Award Winner)No EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Nota: 4 de 5 estrelas4/5 (98)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeNo EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeNota: 4 de 5 estrelas4/5 (5795)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureNo EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureNota: 4.5 de 5 estrelas4.5/5 (474)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryNo EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryNota: 3.5 de 5 estrelas3.5/5 (231)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceNo EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceNota: 4 de 5 estrelas4/5 (895)
- Never Split the Difference: Negotiating As If Your Life Depended On ItNo EverandNever Split the Difference: Negotiating As If Your Life Depended On ItNota: 4.5 de 5 estrelas4.5/5 (838)
- The Little Book of Hygge: Danish Secrets to Happy LivingNo EverandThe Little Book of Hygge: Danish Secrets to Happy LivingNota: 3.5 de 5 estrelas3.5/5 (400)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersNo EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersNota: 4.5 de 5 estrelas4.5/5 (345)
- The Unwinding: An Inner History of the New AmericaNo EverandThe Unwinding: An Inner History of the New AmericaNota: 4 de 5 estrelas4/5 (45)
- Team of Rivals: The Political Genius of Abraham LincolnNo EverandTeam of Rivals: The Political Genius of Abraham LincolnNota: 4.5 de 5 estrelas4.5/5 (234)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyNo EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyNota: 3.5 de 5 estrelas3.5/5 (2259)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaNo EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaNota: 4.5 de 5 estrelas4.5/5 (266)
- The Emperor of All Maladies: A Biography of CancerNo EverandThe Emperor of All Maladies: A Biography of CancerNota: 4.5 de 5 estrelas4.5/5 (271)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreNo EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreNota: 4 de 5 estrelas4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)No EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Nota: 4.5 de 5 estrelas4.5/5 (121)