Escolar Documentos
Profissional Documentos
Cultura Documentos
Phytophotodermatitis
Enviado por
jaggu5005Descrição original:
Direitos autorais
Formatos disponíveis
Compartilhar este documento
Compartilhar ou incorporar documento
Você considera este documento útil?
Este conteúdo é inapropriado?
Denunciar este documentoDireitos autorais:
Formatos disponíveis
Phytophotodermatitis
Enviado por
jaggu5005Direitos autorais:
Formatos disponíveis
Phytophotodermatitis: Treatment & Medication
Author: William P Baugh, MD, Assistant Clinical Professor of Dermatology, University of California Irvine School of Medicine and Western School of Medicine; Medical Director, Full Spectrum Dermatology; Consulting Staff, Department of Dermatology, St Jude Medical Center Coauthor(s): David Barnette Jr, MD, Voluntary Associate Clinical Professor, University of California San Diego School of Medicine;Walter D Kucaba, DO, Private Family Practice, Simpsonville, South Carolina; Cynthia L Chen, Western University of Health Sciences College of Osteopathic Medicine of the Pacific Contributor Information and Disclosures Updated: Oct 16, 2009
Print This Email This
Overview Differential Diagnoses & Workup Treatment & Medication Follow-up Multimedia
References Keywords
Treatment
Medical Care
Patient reassurance is essential once the diagnosis is made. Phytophotodermatitis (PPD) is a selflimited problem that resolves with removal of the offending agent. Patients should avoid the offending agent (furocoumarin). Cool wet compresses may be used for acute lesions. Topical steroids may be used if the eruption is severe and edematous. Indomethacin (50-75 mg PO qd) may be used for adults.
Consultations
Referral to a dermatologist may be useful.
Activity
Use of UV-A sunscreens may help prevent further phototoxic reactions from occurring when exposed to sunlight.
Medication
The goals of pharmacotherapy are to reduce morbidity and to prevent complications.
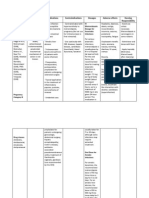
Corticosteroids
These agents have anti-inflammatory properties and cause profound and varied metabolic effects. In addition, these agents modify the body's immune response to diverse stimuli. Low-to-high potency topical steroids may be applied to affected areas to reduce local inflammation induced by the photoactivated psoralens. They may help to relieve the burning sensation associated with phytophotodermatitis as well as to reduce the associated postinflammatory hyperpigmentation.
Hydrocortisone valerate 0.2% cream (Westcort)
Treats inflammatory dermatosis responsive to steroids. Decreases inflammation by suppressing migration of polymorphonuclear leukocytes and reversing capillary permeability.
Adult
Apply to affected areas bid; may be useful face or intertriginous areas for short periods
Pediatric
Apply as in adults
Pregnancy
C - Fetal risk revealed in studies in animals but not established or not studied in humans; may use if benefits outweigh risk to fetus
Precautions
Prolonged use, applying over large surface areas, applying potent steroids, and using occlusive dressings may increase systemic absorption of corticosteroids and may cause Cushing syndrome, reversible HPA-axis suppression, hyperglycemia, and glycosuria
Clobetasol (Temovate)
Class I superpotent topical steroid; suppresses mitosis and increases synthesis of proteins that decrease inflammation and cause vasoconstriction.
Adult
Apply bid for up to 2 wk; not to exceed 50 g/wk
Pediatric
Not established; use with caution
Pregnancy
C - Fetal risk revealed in studies in animals but not established or not studied in humans; may use if benefits outweigh risk to fetus
Precautions
May suppress adrenal function in prolonged therapy; not recommended for face or intertriginous areas; can cause atrophy of groin, face, and axillae; if infection develops and is not responsive to antibiotic treatment, discontinue until infection under control
Betamethasone topical (Diprolene, Betatrex)
For inflammatory dermatosis responsive to steroids. Decreases inflammation by suppressing migration of polymorphonuclear leukocytes and reversing capillary permeability.
Adult
Apply thin film bid/qid until response
Pediatric
Not established; use with caution
Pregnancy
C - Fetal risk revealed in studies in animals but not established or not studied in humans; may use if benefits outweigh risk to fetus
Precautions
Can cause atrophy of groin, face, and axillae; if infection develops and is not responsive to antibiotic treatment, discontinue until infection under control
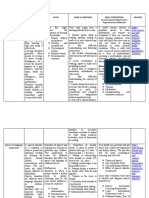
Nonsteroidal anti-inflammatory drugs
These agents are most commonly used for relief of mild to moderate pain. Indomethacin is an analgesic and NSAID medication that may offer some protection against acute UV-Ainduced epidermal apoptosis as well as provide some relief of skin discomfort.
Indomethacin (Indocin)
Has anti-inflammatory properties due to inhibition of prostaglandin synthesis and/or leukocyte migration into inflamed areas. Rapidly absorbed; metabolism occurs in liver by demethylation, deacetylation, and glucuronide conjugation.
Adult
25 mg PO bid/qid with food
Pediatric
Not established; in general, should not be used in patients <14 y
Interactions:
Coadministration with aspirin increases risk of inducing serious NSAID-related adverse effects; may decrease effects of beta-blockers, hydralazine, and captopril; may decrease diuretic effects of furosemide and thiazides; coadministration with anticoagulants may prolong PT (monitor and watch for signs of bleeding); may increase risk of methotrexate toxicity, which can manifest as stomatitis, bone marrow suppression, or nephrotoxicity; coadministration may increase phenytoin levels; probenecid may increase toxicity of NSAIDs
Pregnancy
B - Fetal risk not confirmed in studies in humans but has been shown in some studies in animals
Precautions
Category D in third trimester of pregnancy; acute renal insufficiency, hyperkalemia, hyponatremia, interstitial nephritis, and renal papillary necrosis may occur; increases risk of acute renal failure in patients with preexisting renal disease or compromised renal perfusion; reversible leukopenia may occur, (discontinue if leukopenia, granulocytopenia, or thrombocytopenia persists)
Você também pode gostar
- Francis Peteros Drug Study 2 BetamethasoneDocumento8 páginasFrancis Peteros Drug Study 2 BetamethasoneFrancis PeterosAinda não há avaliações
- Naplex Complete Study Outline A Topic-Wise Approach DiabetesNo EverandNaplex Complete Study Outline A Topic-Wise Approach DiabetesNota: 4 de 5 estrelas4/5 (2)
- Acne VulgarisDocumento5 páginasAcne VulgarisVinh Đỗ ĐìnhAinda não há avaliações
- Flutibact Skin OintmentDocumento12 páginasFlutibact Skin OintmentSowndarya100% (1)
- Health Advice and Immunizations for TravelersNo EverandHealth Advice and Immunizations for TravelersAinda não há avaliações
- AzithromycinDocumento10 páginasAzithromycinShaina MentangAinda não há avaliações
- Suicide Attempt Pseudotumor Cerebri, Stevens-Johnson Syndrome Toxic Epidermal NecrolysisDocumento10 páginasSuicide Attempt Pseudotumor Cerebri, Stevens-Johnson Syndrome Toxic Epidermal NecrolysisPrecious C. MamaradloAinda não há avaliações
- Flutivate e CreamDocumento9 páginasFlutivate e Creamseema sharmaAinda não há avaliações
- Betnelan TabletsDocumento7 páginasBetnelan TabletsAstro GuruAinda não há avaliações
- BETNESOL™ Tablets: Data SheetDocumento4 páginasBETNESOL™ Tablets: Data Sheetsmargo171100% (1)
- Betamethasone Valerate Cream 0.1% W/W Betamethasone Valerate Ointment 0.1% W/WDocumento6 páginasBetamethasone Valerate Cream 0.1% W/W Betamethasone Valerate Ointment 0.1% W/WAgapa Yagamo GamikaAinda não há avaliações
- Docetaxel - 40mg/ml Injection: InstructionDocumento11 páginasDocetaxel - 40mg/ml Injection: InstructionywAinda não há avaliações
- Betnesol Oral DropsDocumento8 páginasBetnesol Oral DropsAnamika VatsalAinda não há avaliações
- Cancer Drug StudyDocumento14 páginasCancer Drug StudyIamanamay Trinidad100% (1)
- Neomycin and Prednisolone Acetate Ophthalmic SuspensionDocumento10 páginasNeomycin and Prednisolone Acetate Ophthalmic SuspensionInne Widya UtamiAinda não há avaliações
- SMPC Polyderm CreamDocumento6 páginasSMPC Polyderm CreamAxmed MaxamedAinda não há avaliações
- DexamethasoneDocumento4 páginasDexamethasoneMits Valencia Karlsson0% (2)
- Pharmacy Communications I Top 200 Drugs: List 5: AlbuterolDocumento13 páginasPharmacy Communications I Top 200 Drugs: List 5: AlbuterolTodd JacksonAinda não há avaliações
- Chronic Urticaria and Treatment Options: Cme ArticleDocumento8 páginasChronic Urticaria and Treatment Options: Cme ArticleYogi SanjayaAinda não há avaliações
- Drug StudyDocumento7 páginasDrug StudyPeetah PanAinda não há avaliações
- Adrenocortical AgentsDocumento14 páginasAdrenocortical AgentsFredie O HadjimudinAinda não há avaliações
- Gentamicin SulfateDocumento4 páginasGentamicin Sulfateapi-3797941Ainda não há avaliações
- Drug StudyDocumento9 páginasDrug StudyAlexander Chavez Alto100% (1)
- Acne Vulgaris Management: What's New and What's Still True?: Review ArticleDocumento5 páginasAcne Vulgaris Management: What's New and What's Still True?: Review ArticleAlmuizzu NurjannahAinda não há avaliações
- Drug Study 408Documento13 páginasDrug Study 408Jheryck SabadaoAinda não há avaliações
- Drug Analysis: Submitted By: GALICINAO, Gretta Shalou GDocumento9 páginasDrug Analysis: Submitted By: GALICINAO, Gretta Shalou GggalicinaoAinda não há avaliações
- Flutivate Skin Cream 1. Generic Name: For The Use Only of Registered Medical Practitioners or A Hospital or A LaboratoryDocumento11 páginasFlutivate Skin Cream 1. Generic Name: For The Use Only of Registered Medical Practitioners or A Hospital or A LaboratoryManas MishraAinda não há avaliações
- Prednisone TabDocumento10 páginasPrednisone TabrantiadrianiAinda não há avaliações
- Drug Card Solu-MEDROLDocumento2 páginasDrug Card Solu-MEDROLBenAinda não há avaliações
- Psoriasis Management May 2018Documento13 páginasPsoriasis Management May 2018ShamlazaghAinda não há avaliações
- Drug Study (Lidocaine HCL) - TorresDocumento6 páginasDrug Study (Lidocaine HCL) - TorresbabiAinda não há avaliações
- DIPROGENTA Cream/Ointment: Schering-PloughDocumento2 páginasDIPROGENTA Cream/Ointment: Schering-PloughWalter Macasiano GravadorAinda não há avaliações
- Betnovate Cream Product SummaryDocumento8 páginasBetnovate Cream Product SummaryMeraz AhmedAinda não há avaliações
- MethylprednisoloneDocumento4 páginasMethylprednisoloneadryananestesiAinda não há avaliações
- Cutivate Krim 0,05% Flutikason Propionat DKL1732005829A1 2017Documento6 páginasCutivate Krim 0,05% Flutikason Propionat DKL1732005829A1 2017Retno Tri RahayuAinda não há avaliações
- DrugsDocumento2 páginasDrugsgailannreyesAinda não há avaliações
- DrugsDocumento2 páginasDrugsgailannreyesAinda não há avaliações
- Maxitrol (Neomycin and Polymyxin B Sulfates and Dexamethasone Ophthalmic Ointment) Sterile Description: MaxitrolDocumento6 páginasMaxitrol (Neomycin and Polymyxin B Sulfates and Dexamethasone Ophthalmic Ointment) Sterile Description: Maxitroldjilal430Ainda não há avaliações
- Hydrocortisone TabDocumento7 páginasHydrocortisone TabXee JayAinda não há avaliações
- VitiligoDocumento13 páginasVitiligoFebyan AbotAinda não há avaliações
- Dilantin Group Presentation, PharmDocumento23 páginasDilantin Group Presentation, Pharmapi-282992446Ainda não há avaliações
- Phenytoin Drug StudyDocumento1 páginaPhenytoin Drug StudyIvy Mae Evangelio Vios86% (7)
- Nicu Drug StudyDocumento8 páginasNicu Drug StudyMike SoySauce LibrojoAinda não há avaliações
- 使ってもらえるだけで嬉しいそれだけで十分ですDocumento11 páginas使ってもらえるだけで嬉しいそれだけで十分ですLANCE CHRISTIAN CUENCAAinda não há avaliações
- PREDNISONEDocumento4 páginasPREDNISONECay SevillaAinda não há avaliações
- OtodexDocumento2 páginasOtodexadelin ransunAinda não há avaliações
- Acne Course - NotesDocumento11 páginasAcne Course - NotesMartin MaherAinda não há avaliações
- ) Pharmacology Drug StudyDocumento8 páginas) Pharmacology Drug StudyFatima KateAinda não há avaliações
- Intophthalmolclin2006462141 64Documento24 páginasIntophthalmolclin2006462141 64Laura BortolinAinda não há avaliações
- Drug Study - Feb 16Documento9 páginasDrug Study - Feb 16ciela00034Ainda não há avaliações
- Product Name: New Zealand Data Sheet Apo-PrednisoneDocumento13 páginasProduct Name: New Zealand Data Sheet Apo-PrednisonedomAinda não há avaliações
- Drug Study Risperidone and Ascorbic AcidDocumento3 páginasDrug Study Risperidone and Ascorbic AcidElcid PimentelAinda não há avaliações
- DactinomycinDocumento4 páginasDactinomycinKeith MadarangAinda não há avaliações
- Drug Study PNPGHDocumento2 páginasDrug Study PNPGHJoseph Francis G. SazonAinda não há avaliações
- ErythromycinDocumento1 páginaErythromycinKenneth Robert Abrantes0% (1)
- Dilantin Capsules PM E 222333 23jan2019Documento29 páginasDilantin Capsules PM E 222333 23jan2019Anonymous BU4ZiA9qjAinda não há avaliações
- Drug Study - HydrocortisoneDocumento5 páginasDrug Study - HydrocortisoneryanAinda não há avaliações
- Drug Study Clindamycin, Ipatropium BromideDocumento8 páginasDrug Study Clindamycin, Ipatropium Bromidepaupaulala100% (2)
- Therapeutic Relationship Is Between Therapist and Patient and Has Always Been Viewed As SacredDocumento3 páginasTherapeutic Relationship Is Between Therapist and Patient and Has Always Been Viewed As Sacredcbargrad100% (1)
- 50 Item Psychiatric Nursing Exam IDocumento11 páginas50 Item Psychiatric Nursing Exam Iɹǝʍdןnos98% (40)
- Pharmaceuticals Manufacturing - What Do We Know About The Occupational Health and Safety Hazards For Women Working in The Industry PDFDocumento61 páginasPharmaceuticals Manufacturing - What Do We Know About The Occupational Health and Safety Hazards For Women Working in The Industry PDFCostas JacovidesAinda não há avaliações
- Chapter 2 Lesson 1Documento3 páginasChapter 2 Lesson 1John Carldel VivoAinda não há avaliações
- AcupunctureDocumento10 páginasAcupunctureAngel Iulian Popescu0% (2)
- Nejmra 2023911Documento8 páginasNejmra 2023911Merry LeeAinda não há avaliações
- Curriculum Vitae Professor Ngai Ngan-pun (魏雁滨教授)Documento22 páginasCurriculum Vitae Professor Ngai Ngan-pun (魏雁滨教授)api-26075761Ainda não há avaliações
- Safety Pocket Guide Web 061808Documento534 páginasSafety Pocket Guide Web 061808hombre911100% (1)
- Overcoming Obesogenic Environments: A Qualitative Study Exploring Mechanisms of Healthy EatersDocumento10 páginasOvercoming Obesogenic Environments: A Qualitative Study Exploring Mechanisms of Healthy EatersCristina Saldias PorrasAinda não há avaliações
- Components of Fitness, PARQ and TestingDocumento29 páginasComponents of Fitness, PARQ and TestingLynAinda não há avaliações
- Food StampsDocumento80 páginasFood StampsAnvitaRamachandranAinda não há avaliações
- Bassam Osman ResumeDocumento4 páginasBassam Osman ResumeBassam OsmanAinda não há avaliações
- Position Paper de l'UEFA Sur L'interdiction Du Gazon Synthétique Par l'ECHA 19 Juillet 2019Documento8 páginasPosition Paper de l'UEFA Sur L'interdiction Du Gazon Synthétique Par l'ECHA 19 Juillet 2019LeMonde.frAinda não há avaliações
- Arterial Events, Venous Thromboembolism, Thrombocytopenia, and Bleeding After Vaccination With Oxford-Astrazeneca Chadox1-S in Denmark and Norway: Population Based Cohort StudyDocumento10 páginasArterial Events, Venous Thromboembolism, Thrombocytopenia, and Bleeding After Vaccination With Oxford-Astrazeneca Chadox1-S in Denmark and Norway: Population Based Cohort StudyFemale calmAinda não há avaliações
- Professions and Occupations in BoliviaDocumento7 páginasProfessions and Occupations in BoliviaMaribel Jarata JulianAinda não há avaliações
- Antiinflammatorydrugs: Beatriz Monteiro,, Paulo V. SteagallDocumento19 páginasAntiinflammatorydrugs: Beatriz Monteiro,, Paulo V. SteagallYohan Oropeza VergaraAinda não há avaliações
- Philippine Saviours: Narratives of Filipino Intensive Care Nurses and Their Ways On Handling Chronically Ill PatientsDocumento38 páginasPhilippine Saviours: Narratives of Filipino Intensive Care Nurses and Their Ways On Handling Chronically Ill PatientsHannah SampianoAinda não há avaliações
- Profile of Osteopathic Practice in Spain Results FDocumento11 páginasProfile of Osteopathic Practice in Spain Results FBerenice LimarkAinda não há avaliações
- Types Causes Signs and Symptomps Intellectual DisabilityDocumento2 páginasTypes Causes Signs and Symptomps Intellectual DisabilityMae Ann Jean JustolAinda não há avaliações
- Calories Needed For A 17 Year Old, 70 KG MaleDocumento7 páginasCalories Needed For A 17 Year Old, 70 KG Maleboom boomAinda não há avaliações
- Anxiety Disorder by SlidesgoDocumento55 páginasAnxiety Disorder by SlidesgoShey DraftsAinda não há avaliações
- Uti StudiesDocumento10 páginasUti Studiesapi-302840362Ainda não há avaliações
- Medical Surgical Nursing 3 BulletsDocumento4 páginasMedical Surgical Nursing 3 BulletsQueen ElizabethAinda não há avaliações
- TheraDocumento4 páginasTheramaircusAinda não há avaliações
- Improving Lives of South Sudanese Communities Through Water and Sanitation: The Story of Salva DutDocumento1 páginaImproving Lives of South Sudanese Communities Through Water and Sanitation: The Story of Salva DutUNICEF South SudanAinda não há avaliações
- Chalmers Stressful Life Events: Their Past and PresentDocumento15 páginasChalmers Stressful Life Events: Their Past and PresentAna Rivera CastañonAinda não há avaliações
- Unit - 1 Concepts and Definitions 1.1 Disaster (I)Documento25 páginasUnit - 1 Concepts and Definitions 1.1 Disaster (I)RISHITHA LELLAAinda não há avaliações
- Physiological Changes Postpartum PeriodDocumento2 páginasPhysiological Changes Postpartum PeriodEurielle MioleAinda não há avaliações
- Disability MatrixDocumento21 páginasDisability MatrixAngelika MendozaAinda não há avaliações
- Hauber 2019Documento10 páginasHauber 2019Laura HdaAinda não há avaliações
- The Obesity Code: Unlocking the Secrets of Weight LossNo EverandThe Obesity Code: Unlocking the Secrets of Weight LossNota: 4 de 5 estrelas4/5 (6)
- By the Time You Read This: The Space between Cheslie's Smile and Mental Illness—Her Story in Her Own WordsNo EverandBy the Time You Read This: The Space between Cheslie's Smile and Mental Illness—Her Story in Her Own WordsAinda não há avaliações
- Think This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BeNo EverandThink This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BeNota: 2 de 5 estrelas2/5 (1)
- The Age of Magical Overthinking: Notes on Modern IrrationalityNo EverandThe Age of Magical Overthinking: Notes on Modern IrrationalityNota: 4 de 5 estrelas4/5 (24)
- The Body Keeps the Score by Bessel Van der Kolk, M.D. - Book Summary: Brain, Mind, and Body in the Healing of TraumaNo EverandThe Body Keeps the Score by Bessel Van der Kolk, M.D. - Book Summary: Brain, Mind, and Body in the Healing of TraumaNota: 4.5 de 5 estrelas4.5/5 (266)
- Summary: Outlive: The Science and Art of Longevity by Peter Attia MD, With Bill Gifford: Key Takeaways, Summary & AnalysisNo EverandSummary: Outlive: The Science and Art of Longevity by Peter Attia MD, With Bill Gifford: Key Takeaways, Summary & AnalysisNota: 4.5 de 5 estrelas4.5/5 (42)
- Summary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedNo EverandSummary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedNota: 5 de 5 estrelas5/5 (80)
- ADHD is Awesome: A Guide to (Mostly) Thriving with ADHDNo EverandADHD is Awesome: A Guide to (Mostly) Thriving with ADHDNota: 5 de 5 estrelas5/5 (1)
- Self-Care for Autistic People: 100+ Ways to Recharge, De-Stress, and Unmask!No EverandSelf-Care for Autistic People: 100+ Ways to Recharge, De-Stress, and Unmask!Nota: 5 de 5 estrelas5/5 (1)
- Raising Mentally Strong Kids: How to Combine the Power of Neuroscience with Love and Logic to Grow Confident, Kind, Responsible, and Resilient Children and Young AdultsNo EverandRaising Mentally Strong Kids: How to Combine the Power of Neuroscience with Love and Logic to Grow Confident, Kind, Responsible, and Resilient Children and Young AdultsNota: 5 de 5 estrelas5/5 (1)
- Outlive: The Science and Art of Longevity by Peter Attia: Key Takeaways, Summary & AnalysisNo EverandOutlive: The Science and Art of Longevity by Peter Attia: Key Takeaways, Summary & AnalysisNota: 4 de 5 estrelas4/5 (1)
- Dark Psychology & Manipulation: Discover How To Analyze People and Master Human Behaviour Using Emotional Influence Techniques, Body Language Secrets, Covert NLP, Speed Reading, and Hypnosis.No EverandDark Psychology & Manipulation: Discover How To Analyze People and Master Human Behaviour Using Emotional Influence Techniques, Body Language Secrets, Covert NLP, Speed Reading, and Hypnosis.Nota: 4.5 de 5 estrelas4.5/5 (110)
- Gut: the new and revised Sunday Times bestsellerNo EverandGut: the new and revised Sunday Times bestsellerNota: 4 de 5 estrelas4/5 (392)
- Why We Die: The New Science of Aging and the Quest for ImmortalityNo EverandWhy We Die: The New Science of Aging and the Quest for ImmortalityNota: 4 de 5 estrelas4/5 (3)
- Raising Good Humans: A Mindful Guide to Breaking the Cycle of Reactive Parenting and Raising Kind, Confident KidsNo EverandRaising Good Humans: A Mindful Guide to Breaking the Cycle of Reactive Parenting and Raising Kind, Confident KidsNota: 4.5 de 5 estrelas4.5/5 (169)
- Cult, A Love Story: Ten Years Inside a Canadian Cult and the Subsequent Long Road of RecoveryNo EverandCult, A Love Story: Ten Years Inside a Canadian Cult and the Subsequent Long Road of RecoveryNota: 4 de 5 estrelas4/5 (44)
- Mindset by Carol S. Dweck - Book Summary: The New Psychology of SuccessNo EverandMindset by Carol S. Dweck - Book Summary: The New Psychology of SuccessNota: 4.5 de 5 estrelas4.5/5 (328)
- The Ritual Effect: From Habit to Ritual, Harness the Surprising Power of Everyday ActionsNo EverandThe Ritual Effect: From Habit to Ritual, Harness the Surprising Power of Everyday ActionsNota: 3.5 de 5 estrelas3.5/5 (3)
- When the Body Says No by Gabor Maté: Key Takeaways, Summary & AnalysisNo EverandWhen the Body Says No by Gabor Maté: Key Takeaways, Summary & AnalysisNota: 3.5 de 5 estrelas3.5/5 (2)
- Sleep Stories for Adults: Overcome Insomnia and Find a Peaceful AwakeningNo EverandSleep Stories for Adults: Overcome Insomnia and Find a Peaceful AwakeningNota: 4 de 5 estrelas4/5 (3)
- Gut: The Inside Story of Our Body's Most Underrated Organ (Revised Edition)No EverandGut: The Inside Story of Our Body's Most Underrated Organ (Revised Edition)Nota: 4 de 5 estrelas4/5 (378)
- To Explain the World: The Discovery of Modern ScienceNo EverandTo Explain the World: The Discovery of Modern ScienceNota: 3.5 de 5 estrelas3.5/5 (51)
- The Marshmallow Test: Mastering Self-ControlNo EverandThe Marshmallow Test: Mastering Self-ControlNota: 4.5 de 5 estrelas4.5/5 (58)