Escolar Documentos
Profissional Documentos
Cultura Documentos
Dermatological History and Examination - Leaflet Print - Patient UK
Enviado por
Nadeem KhanDescrição original:
Direitos autorais
Formatos disponíveis
Compartilhar este documento
Compartilhar ou incorporar documento
Você considera este documento útil?
Este conteúdo é inapropriado?
Denunciar este documentoDireitos autorais:
Formatos disponíveis
Dermatological History and Examination - Leaflet Print - Patient UK
Enviado por
Nadeem KhanDireitos autorais:
Formatos disponíveis
Dermatological History and Examination - leaflet print - Patient UK
Page 1
Generated by Foxit PDF Creator Foxit Software http://www.foxitsoftware.com For evaluation only.
This is a PatientPlus article. PatientPlus articles are written for doctors and so the language can be technical, however some people find that they add depth to the patient information leaflets. You may find the abbreviations record helpful.
Dermatological History and Examination
Skin disease is marked by its variety and visibility. Dermatology is a field where pattern recognition and analysis are critical so experience is key - having seen something previously makes it much easier to recognise it in the future. Accurate history taking and examination are as important as in any other field of medicine. A systematic approach is required, although this may become truncated with experience; however, even the most experienced doctor will have the occasional difficult case where it is necessary to go back to basics. The diagnosis and management of skin disease makes up a large component of Primary Care and most GPs develop diagnostic and surgical skills to deal with this demand. In recent years, nurses have been more involved in the provision of dermatological care as well as having to make diagnoses in circumstances such as a walk-in clinic.
2 1
History
As always, this is the starting point:
Note basic demographics of the patient: Age - infectious diseases are more common in children but malignancy gets more common with advancing age. Sex - some conditions are more common in men or more common in women. Race and country of origin. Current residence - important in an infectious outbreak. Consider the lesion: Duration: Onset - sudden versus gradual? Is this an acute presentation or an ongoing chronic problem? Previous episodes, e.g. photodermatoses tend to reoccur every spring with the onset of good weather. Change - fluctuation versus persistence? Consider variation in severity, e.g. occupational contact allergic dermatitis may improve when on holiday. Urticaria may be quite dynamic in its presentation but others are much more static. Location: as well as skin, remember mucous membranes. The site of lesions is important. Eczema tends to be on flexural surfaces (in adults and older children) whilst psoriasis tends to be on extensor parts. Lesions may have a specific distribution - around the genitals, in sweaty regions or sun-exposed areas. Has the lesion spread? Provoking or relieving factors, e.g. heat and cold may be either aggravating or relieving factors, especially with urticaria, repeated drug exposures with fixed drug eruptions. Associated symptoms: Itch - some lesions are renowned for being itchy and others for not being so but this can be misleading. Psoriasis is said to be non-itchy but there may be pruritus in the genital area. Tenderness - inflammation is often tender. Bleeding or discharge - bleeding may indicate malignancy and discharge may occur with an infected lesion. Systemic symptoms such as pyrexia, malaise, joint pain and swelling or weight loss. Some skin lesions are markers for underlying malignancy.
3
Response to treatment - both patient and doctor initiated. A number of treatments may have been tried prior to consultation e.g. antiseptic lotions, calamine, antihistamines, over-thecounter (OTC) steroid or antifungal creams, herbal remedies or medication prescribed for another family member or friend. Complementary medicines such as chinese herbs may have unknown ingredients and potency. Partially treated lesions are the most difficult to diagnose. Do not forget to cover:
4
Past medical history, which is often relevant, e.g. diabetes may suggest necrobiosis lipoidica.
http://www.patient.co.uk/printer.asp?doc=40000992
6/9/2011 12:37:24 AM
Dermatological History and Examination - leaflet print - Patient UK
Family history, which may indicate a familial trend for the disease. Other family members will have been given a diagnosis. A genetic predisposition is important in many diseases including eczema and psoriasis. Alternatively, concurrent and recent affliction of other members of the family suggest a contagious or environmental aetiology. Familial atypical mole and melanoma (FAMM) syndrome should be considered where several family members have multiple melanocytic lesions, some atypical, with at least one case of melanoma in the family. Occupation, hobbies and pastimes, where there may be exposure to chemicals or a very hot environment, for example.
5 6,7
Page 2
Generated by Foxit PDF Creator Foxit Software http://www.foxitsoftware.com For evaluation only.
Travel, particularly to exotic locations, may increase the risk of rarer tropical diseases. Consider cumulative exposure to sunlight or sunbeds and history of sunburn as these increase the risk of skin malignancies. Drugs, prescribed, over-the-counter or other therapies. Drug eruptions can be highly variable. Illegal drug use may have dermatological manifestations, e.g. anabolic steroids and acne.
9 8
Smoking and alcohol- alcohol use has an association with psoriasis and smoking increases the risk of some malignancies and has a close association with palmoplantar pustular psoriasis. Allergies. Psychological and social sequelae - people with severe, chronic, visible and disfiguring skin disease may suffer from anxiety, depression and social isolation, these issues require exploration. Psychological problems may also cause skin disease, e.g. dermatitis artefacta. See separate article Living with Skin Disease.
10
Examination
In general, a thorough examination of the whole skin is considered best practice but may not be warranted, e.g. diagnosis of a verruca. First just look:
Does the patient look ill or well? Are there any clues as to systemic illness? Wipe off any calamine, makeup or anything else that may obscure the true nature of the lesions.
Now focus on the lesion(s): Note the position of lesions: Is the distribution symmetrical or asymmetrical? (Symmetrical distribution suggests an endogenous condition such as psoriasis, whilst asymmetry is more typical of an exogenous condition such as tinea.) Some rashes have a characteristic distribution such as with shingles. Flexor or extensor surfaces? Areas of friction or pressure? Sweaty regions? Exposed regions? Related to sexual contact? (consider genital lesions but also the lower abdomen and upper thighs). Note the size of the lesion. Measure for accuracy. Is it single or multiple? If a rash exists, what is its morphology? Are individual lesions: Macular? Papular? Vesicular? Crusty? Urticarial? Note colour, shape, regularity or irregularity. Are there areas of inflammation around it? Is the edge clearly demarcated or poorly defined? The use of dermatoscopy may aid diagnosis beyond naked eye examination but should only be used by those with appropriate training. Now touch:
Feel for: Tenderness. Warmth. Site within the skin. Thickness.
http://www.patient.co.uk/printer.asp?doc=40000992
6/9/2011 12:37:24 AM
Dermatological History and Examination - leaflet print - Patient UK
Consistency (hard, soft, firm, fluctuant).
Page 3
Generated by Foxit PDF Creator Foxit Software http://www.foxitsoftware.com For evaluation only.
Does firm pressure lead to blanching? Is it friable? Does it bleed easily? Scaling - disorders of the epidermis may produce scale, which may be visible, or gentle scratching of the skin may make it apparent. If appropriate, look to see if there is any evidence of infestation, e.g scabies' burrows. Note hair in the local skin and on the head. Look at the nails.
11 12
Are mucous membranes involved? Examine the genitals where appropriate. Are there regional lymph nodes? This may be relevant for infectious or malignant lesions.
Differential diagnosis
Having completed the full history and examination, it is usually possible to make a firm diagnosis but, if not, it is certainly possible to distil a great deal of information about the condition. Very often the impressive names that dermatologists give to unusual conditions are nothing more than a description in Latin. Beware of the 'great mimickers', e.g. amelanotic melanoma, lupus erythematosus, sarcoid, mycobacteria and cutaneous T-cell lymphoma. Diagnostic tables and algorithms have been developed to complement clinical acumen - see DERMIS: Skin Disease Recognition Calculator for an example. Where a firm diagnosis cannot be made with a reasonable degree of confidence, investigations may be helpful and even a therapeutic trial may be beneficial. However, steroid cream can mask some aspects of a disease and dermatologists often complain of the difficulties of diagnosing partially treated disease. Teledermatology is fundamentally changing primary care's access to an expert opinion on a skin condition although concerns persist about reduced diagnostic reliability and the ongoing need for faceto-face consultations, particularly in the diagnosis of skin malignancies.
13
One of the most important decisions to make about a skin lesion is whether or not it is malignant. There must be a high index of suspicion and absolute certainty is rare. For pigmented lesions, change is an important element in diagnosing malignant melanoma. Current guidelines suggest assessing on a weighted 7-point scale:
15
14
Major features of the lesions: (score 2 points each)
Change in size Irregular shape Irregular colour Minor features of the lesions: (score 1 point each)
Largest diameter 7 mm or more Inflammation Oozing Change in sensation
Suspicion is greater for lesions scoring 3 points or more but, if there are strong concerns, any one feature is sufficient to prompt urgent referral, as should: Any new solitary nodule or plaque regardless of colour where a benign diagnosis (e.g. a dermatofibroma) cannot be made with confidence. Half of nodular melanomas are hypomelanotic or amelanotic and may present as a pink nodule. A new pigmented line in a nail. Lesions growing under a nail. Pigmented lesions on mucosal surfaces.
Investigations16
Swabs
These can be taken for bacteriology and virology.
http://www.patient.co.uk/printer.asp?doc=40000992
6/9/2011 12:37:24 AM
Dermatological History and Examination - leaflet print - Patient UK
Skin scrapings
Page 4
Generated by Foxit PDF Creator Foxit Software http://www.foxitsoftware.com For evaluation only.
Skin scrapings for microscopy can be useful to diagnose fungal infections, pityriasis versicolor and ectoparasitic infections such as scabies. For dermatophyte infections, scrape the advancing edge of the scaly lesion carefully. Nail clippings - ensure a good-sized clipping and scrape from the under the surface of the nail. Hair root samples can be useful in suspected tinea capitis. Most laboratories will supply appropriate specimen containers - usually small envelopes with a black interior as it is much easier to see the sample against such a background.
Wood's light
This is an ultraviolet light (wavelength 360-365 nm) used in a darkened room. It should be held at least 10-15 cm from the skin and time should be allowed for dark accommodation to occur. When shone on some fungal infections, the light causes fluorescence.
Tinea versicolor fluoresces with subtle gold colours. Erythrasma due to Corynebacterium minutissimum fluoresces a bright coral red. Tinea capitis caused by Microsporum canis and Microsporum audouinii fluoresce a light bright green but most tinea capitis infections are caused by Trichophyton species that do not fluoresce.
Pseudomonas aeruginosa infection, especially in burns, may provide green-yellow fluorescence. Vitiligo also fluoresces. Its associated depigmentation can be differentiated from hypopigmented lesions by the ivory-white colour under Wood's light. Wood's light can also be used in the evaluation of pigmented lesions, marking out areas of lentigo maligna or melasma. 17
Skin biopsy
Biopsy may be used to provide a histopathological specimen to aid diagnosis and guide further management. Always provide relevant history, description and differential diagnosis to assist the histopathologist. Histology may not be able to differentiate between some cases of dysplastic naevi and melanoma so that any case of incompletely excised 'dysplastic naevus' should be referred for a further excision. Shave and punch biopsy techniques can be used. Shave excisions are less demanding technically, and are useful when the lesion is small and the risk of malignancy is low. Punch biopsies remove a core of skin from the epidermis to subcutaneous fat. Ideally the biopsy should include normal skin, part of the lesion and the transition zone. Excisional biopsies aim to remove the entire lesion, with a margin dependent on the risk of malignancy. Its advantage is that the procedure can provide treatment as well as diagnosis for many lesions but it is more demanding of time, equipment and expertise. Biopsy can also be used for immunofluorescence and culture (e.g. mycobacterium, leishmaniasis).
Patch and skin prick tests
These are used for the investigation of contact allergic dermatitis and suspected latex and other allergies.
Document references
1. Courtenay M, Carey N; Nurse-led care in dermatology: a review of the literature. Br J Dermatol. 2006 Jan;154(1):1-6. [abstract] 2. Ersser SJ, Lattimer V, Surridge H, et al; An analysis of the skin care patient mix attending a primary care-based nurse-led NHS Walk-in Centre. Br J Dermatol. 2005 Nov;153(5):992-6. [abstract] 3. Kleyn CE, Lai-Cheong JE, Bell HK; Cutaneous manifestations of internal malignancy: diagnosis and management. Am J Clin Dermatol. 2006;7(2):71-84. [abstract] 4. Ramsay HM, Goddard W, Gill S, et al; Herbal creams used for atopic eczema in Birmingham, UK illegally contain potent corticosteroids. Arch Dis Child. 2003 Dec;88(12):1056-7. [abstract] 5. Slodownik D, Nixon R; Occupational factors in skin diseases. Curr Probl Dermatol. 2007;35:173-89. [abstract] 6. Lupi O, Madkan V, Tyring SK; Tropical dermatology: bacterial tropical diseases. J Am Acad Dermatol. 2006 Apr;54(4):559-78; quiz 578-80. [abstract] 7. Lupi O, Tyring SK, McGinnis MR; Tropical dermatology: fungal tropical diseases. J Am Acad Dermatol. 2005 Dec;53(6):931-51, quiz 952-4. [abstract] 8. Valeyrie-Allanore L, Sassolas B, Roujeau JC; Drug-induced skin, nail and hair disorders. Drug Saf. 2007;30(11):1011-30. [abstract]
http://www.patient.co.uk/printer.asp?doc=40000992
6/9/2011 12:37:24 AM
Dermatological History and Examination - leaflet print - Patient UK
9. Dika E, Bardazzi F, Balestri R, et al; Environmental factors and psoriasis. Curr Probl Dermatol. 2007;35:118-35. [abstract] 10. Picardi A, Pasquini P, Abeni D, et al; Psychosomatic assessment of skin diseases in clinical practice. Psychother Psychosom. 2005;74(5):315-22. [abstract] 11. Hinds G, Thomas VD; Malignancy and cancer treatment-related hair and nail changes. Dermatol Clin. 2008 Jan;26(1):59-68, viii. [abstract] 12. Scully C; A review of common mucocutaneous disorders affecting the mouth and lips. Ann Acad Med Singapore. 1999 Sep;28(5):704-7. [abstract] 13. Bowns IR, Collins K, Walters SJ, et al; Telemedicine in dermatology: a randomised controlled trial. Health Technol Assess. 2006 Nov;10(43):iii-iv, ix-xi, 1-39. [abstract] 14. Bruce AJ, Brodland DG; Overview of skin cancer detection and prevention for the primary care physician. Mayo Clin Proc. 2000 May;75(5):491-500. [abstract] 15. Referral for Suspected Cancer CG27; NICE Guidance 16. Chuh AA, Wong WC, Wong SY, et al; Procedures in primary care dermatology. Aust Fam Physician. 2005 May;34(5):347-51. [abstract] 17. Paraskevas LR, Halpern AC, Marghoob AA; Utility of the Wood's light: five cases from a pigmented lesion clinic. Br J Dermatol. 2005 May;152(5):1039-44. [abstract]
Page 5
Generated by Foxit PDF Creator Foxit Software http://www.foxitsoftware.com For evaluation only.
Internet and further reading
DermNet New Zealand Terminology in dermatology. Also some good pictures to illustrate terminology University of Wisconsin Nomenclature of skin lesions; Tutorials and photos aimed at improving description of skin lesions Primary Care Society for Dermatology
Acknowledgements EMIS is grateful to Dr Chloe Borton for writing this article. The final copy has passed scrutiny by the independent Mentor GP reviewing team. EMIS 2010. Document ID: 2041 Document Version: 24 Document Reference: bgp992 Last Updated: 1 Sep 2010 Planned Review: 31 Aug 2013
http://www.patient.co.uk/printer.asp?doc=40000992
6/9/2011 12:37:24 AM
Você também pode gostar
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeNo EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeNota: 4 de 5 estrelas4/5 (5794)
- Duties of Room AttendantDocumento2 páginasDuties of Room AttendantNadeem KhanAinda não há avaliações
- The Yellow House: A Memoir (2019 National Book Award Winner)No EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Nota: 4 de 5 estrelas4/5 (98)
- Housekeeping Training MaterialsDocumento67 páginasHousekeeping Training MaterialsAgung Prasetyo Wibowo100% (3)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryNo EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryNota: 3.5 de 5 estrelas3.5/5 (231)
- Housekeeping Training MaterialsDocumento67 páginasHousekeeping Training MaterialsAgung Prasetyo Wibowo100% (3)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceNo EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceNota: 4 de 5 estrelas4/5 (895)
- Peshawar (Pakistan) Prayer TimesDocumento1 páginaPeshawar (Pakistan) Prayer TimesNadeem KhanAinda não há avaliações
- The Little Book of Hygge: Danish Secrets to Happy LivingNo EverandThe Little Book of Hygge: Danish Secrets to Happy LivingNota: 3.5 de 5 estrelas3.5/5 (400)
- CPT CodesDocumento1.020 páginasCPT CodesNadeem KhanAinda não há avaliações
- AsthmaDocumento19 páginasAsthmaNadeem Khan100% (1)
- Never Split the Difference: Negotiating As If Your Life Depended On ItNo EverandNever Split the Difference: Negotiating As If Your Life Depended On ItNota: 4.5 de 5 estrelas4.5/5 (838)
- Anas Umar Internal Defence SlidesDocumento23 páginasAnas Umar Internal Defence SlidesAnas UmarAinda não há avaliações
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureNo EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureNota: 4.5 de 5 estrelas4.5/5 (474)
- Pediatric ShockDocumento19 páginasPediatric ShockdarlingcarvajalduqueAinda não há avaliações
- CP100MEDICALtermPSAbbr. 2Documento78 páginasCP100MEDICALtermPSAbbr. 2RAISA N. RASIDAinda não há avaliações
- What S in A Case Formulation PDFDocumento10 páginasWhat S in A Case Formulation PDFNicole Flores MuñozAinda não há avaliações
- The Emperor of All Maladies: A Biography of CancerNo EverandThe Emperor of All Maladies: A Biography of CancerNota: 4.5 de 5 estrelas4.5/5 (271)
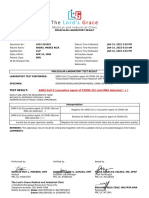
- Sars-Cov-2 (Causative Agent of Covid-19) Viral Rna Detected (+)Documento1 páginaSars-Cov-2 (Causative Agent of Covid-19) Viral Rna Detected (+)Dominica PalacioAinda não há avaliações
- Rheumatic Heart Disease Abx Prophylaxis For Young PatientsDocumento2 páginasRheumatic Heart Disease Abx Prophylaxis For Young PatientsFathima Sheik KatherAinda não há avaliações
- Team of Rivals: The Political Genius of Abraham LincolnNo EverandTeam of Rivals: The Political Genius of Abraham LincolnNota: 4.5 de 5 estrelas4.5/5 (234)
- NCP MakingDocumento2 páginasNCP MakingMinakaAinda não há avaliações
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaNo EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaNota: 4.5 de 5 estrelas4.5/5 (266)
- Mid Term-Essay On Drug AddictionDocumento12 páginasMid Term-Essay On Drug AddictionShubho Dev nathAinda não há avaliações
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersNo EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersNota: 4.5 de 5 estrelas4.5/5 (344)
- The Journey of Antibody and Antigen Test During COVID-19 Pandemic in Indonesia, The Advantages & DisadvantagesDocumento34 páginasThe Journey of Antibody and Antigen Test During COVID-19 Pandemic in Indonesia, The Advantages & DisadvantagesEldo TaufilaAinda não há avaliações
- CIRCI Guidelines 2015Documento6 páginasCIRCI Guidelines 2015Wissam SleimanAinda não há avaliações
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyNo EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyNota: 3.5 de 5 estrelas3.5/5 (2259)
- Daftar PustakaDocumento6 páginasDaftar Pustakasatria divaAinda não há avaliações
- Sample Subspecialty Census FormatDocumento3 páginasSample Subspecialty Census FormatMon FabileAinda não há avaliações
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreNo EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreNota: 4 de 5 estrelas4/5 (1090)
- ID For ABIM - Parham 2014Documento140 páginasID For ABIM - Parham 2014Jeronim H'gharAinda não há avaliações
- 300+ TOP CASE MANAGER Objective Questions and AnswersDocumento29 páginas300+ TOP CASE MANAGER Objective Questions and AnswersHANEESH JOHNAinda não há avaliações
- Open Jejunostomy: Steven J. Hughes, MD and A. James Moser, MDDocumento8 páginasOpen Jejunostomy: Steven J. Hughes, MD and A. James Moser, MDAndres BernalAinda não há avaliações
- The Unwinding: An Inner History of the New AmericaNo EverandThe Unwinding: An Inner History of the New AmericaNota: 4 de 5 estrelas4/5 (45)
- TNCC Study GuideDocumento6 páginasTNCC Study Guidekristinekat96% (24)
- Nursing History: Biographic DataDocumento2 páginasNursing History: Biographic DatayounggirldavidAinda não há avaliações
- NutrigenomicsDocumento8 páginasNutrigenomicsGabriel MarcosAinda não há avaliações
- Cesarean BirthDocumento35 páginasCesarean BirthJhonny Paul RamosAinda não há avaliações
- Eastern Health 30 Minute 4 Hour Rule 2017 PDFDocumento1 páginaEastern Health 30 Minute 4 Hour Rule 2017 PDFprastiaAinda não há avaliações
- Nbme 30 2021 ADocumento200 páginasNbme 30 2021 AUsama Bilal100% (3)
- Colorectal Cancer Case StudyDocumento1 páginaColorectal Cancer Case StudyNur'aini Elita PutriAinda não há avaliações
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)No EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Nota: 4.5 de 5 estrelas4.5/5 (121)
- Penile Inversion Vaginoplasty TechniqueDocumento2 páginasPenile Inversion Vaginoplasty Techniquecathylamont816Ainda não há avaliações
- Maya Semrau - Service User and Caregiver Involvement in Mental Health System Strengthening in Low - and Middle-Income Countries Systematic ReviewDocumento18 páginasMaya Semrau - Service User and Caregiver Involvement in Mental Health System Strengthening in Low - and Middle-Income Countries Systematic ReviewsukmarahastriAinda não há avaliações
- Assessment: Facial ShavingDocumento2 páginasAssessment: Facial ShavingA CAinda não há avaliações
- Chiropractic Principles:: Ancient Foundations of Manual Medicine, Metaphysics and ScienceDocumento3 páginasChiropractic Principles:: Ancient Foundations of Manual Medicine, Metaphysics and Scienceapi-301357653Ainda não há avaliações
- Report 1690018110488Documento2 páginasReport 1690018110488Krishna ChaitanyaAinda não há avaliações
- Normal Respiratory Rate and Heart Rate in Children - UpToDateDocumento2 páginasNormal Respiratory Rate and Heart Rate in Children - UpToDateKrishn DsAinda não há avaliações
- Congenital Muscular Torticollis - A Proposal For Treatment and PhysiotherapyDocumento10 páginasCongenital Muscular Torticollis - A Proposal For Treatment and PhysiotherapyevinovianiAinda não há avaliações
- Assessment 4 (BE)Documento9 páginasAssessment 4 (BE)Aryan Judith DoloresAinda não há avaliações