Escolar Documentos
Profissional Documentos
Cultura Documentos
New Approaches For The Evaluation of Renal Vascular Function in Diabetes
Enviado por
Mahmoud DiaaDescrição original:
Título original
Direitos autorais
Formatos disponíveis
Compartilhar este documento
Compartilhar ou incorporar documento
Você considera este documento útil?
Este conteúdo é inapropriado?
Denunciar este documentoDireitos autorais:
Formatos disponíveis
New Approaches For The Evaluation of Renal Vascular Function in Diabetes
Enviado por
Mahmoud DiaaDireitos autorais:
Formatos disponíveis
Diabetologia DOI 10.
1007/s00125-011-2225-2
COMMENTARY
New approaches for the evaluation of renal vascular function in diabetes
G. Jerums & R. J. MacIsaac
Received: 28 April 2011 / Accepted: 24 May 2011 # Springer-V erlag 2011
Abstract In this issue of Diabetologia, two new approaches are described for the assessment of intra-renal blood flow in people with diabetes. The first approach used the technique of dynamic assessment of the resistance index (RI) in the renal interlobar arteries before and after administration of sublingual glyceryl trinitrate, and the second used MRI to assess total renal blood flow in relation to mean arterial pressure, thereby enabling direct measurement of overall renal RI. The results of the first study raise the possibility that dynamic evaluation of the intra-renal RI could be used as an early detector of vascular alterations in type 2 diabetes, before the onset of microalbuminuria. The results of the second study suggest that decreases in renal blood flow in people with longstanding type 1 diabetes reflect intra-renal vascular stiffening and raise the possibility that in microalbuminuric patients it may also reflect increased intraglomerular pressure. Keywords Chronic kidney disease . Diabetes . Nephropathy . Magnetic resonance imaging . Microalbuminuria . Renal resistance index Abbreviations ACR Albumin to creatinine ratio
CKD RI RVR
Chronic kidney disease Resistance index Renal vascular resistance
G. Jerums (*) Endocrine Centre, Austin Health & University of Melbourne, Heidelberg Repatriation Hospital, Heidelberg West, PO Box 5444, VIC 3081, Australia e-mail: ah-endo@unimelb.edu.au R. J. MacIsaac Department of Endocrinology and Diabetes, St Vincents Hospital & University of Melbourne, Fitzroy, VIC, Australia
Non-invasive assessment of intra-renal blood flow has traditionally been performed using renal duplex Doppler ultrasound of the interlobar cortical arteries. The ratio of the difference between peak systolic and end diastolic velocity divided by peak systolic velocity, termed the intra-renal resistance index (RI), has provided an index of intra-renal arterial stiffness. In type 2 diabetes, intra-renal RI increases with age, blood pressure, BMI, the severity of markers of systemic atherosclerosis and left ventricular diastolic dysfunction, and decreased glomerular filtration rate (GFR) [13]. This association between increased intrarenal RI with decreased GFR remains after allowance for age, blood pressure and the degree of albuminuria [1]. Furthermore, higher baseline intra-renal RI measurements are associated with a greater subsequent decline in GFR [4]. There is also some evidence to suggest that the intra-renal RI differs depending on the underlying renal disease and is increased to a greater extent in people with diabetic renal diseases compared with non-diabetic renal diseases even after adjustment for multiple clinical variables, including creatinine clearance [5]. Two new approaches have recently been described for the assessment of intra-renal blood flow in people with diabetes. The first approach used the concept of dynamic assessment of RI in the renal interlobar arteries. This method has previously been used to assess intra-renal blood changes induced by the administration of reninangiotensin system blocking agents [6]. However, in this instance, intrarenal RI was assessed by Bruno et al. [7] before and after administration of sublingual glyceryl trinitrate. In the second
Diabetologia
study, by Thelwall et al. [8], MRI was used to assess total renal blood flow in relation to mean arterial pressure, thereby enabling direct measurement of overall renal RI. The study by Bruno et al. [7] involved 27 control participants, 49 participants with essential hypertension, and 32 participants with type 2 diabetes and normoalbuminuria. Ages were 51, 52 and 53 years and estimated GFRs were 89, 92 and 87 ml min1 1.73 m2 in the three study groups, respectively. The median albumin to creatinine ratio (ACR) in participants with type 2 diabetes was 0.88 mg/ mmol (7.8 mg/g), which was approximately fivefold greater than the median ACR for participants with essential hypertension or those in the control group, but was well below the accepted microalbuminuric range of 335 mg/ mmol (30300 mg/g). The mean basal intra-renal RI was higher in diabetic (0.65) than in hypertensive participants (0.59, p<0.05) and controls (0.58, p<0.05). However the expected decrease in RI induced by the administration of sublingual glyceryl trinitrate was greatest in controls (11.1 %), diminished in hypertensive participants (9.0 %, p<0.05) and further attenuated in participants with diabetes (7.1%, p<0.05 compared with hypertensive participants). In the overall population, changes in RI induced by glyceryl trinitrate were independently related to serum glucose, reactive hyperaemia and aortic pulse wave velocity. In contrast, brachial artery response to glyceryl trinitrate was similar in the three study groups. Based on these results, the authors raise the possibility that dynamic evaluation of the intra-renal RI could be used as an early detector of vascular alterations in type 2 diabetes, before the onset of microalbuminuria. The study by Thelwall et al. [8] was performed in ten control participants, nine normotensive participants with type 1 diabetes and normoalbuminuria, and eight participants with type 1 diabetes and microalbuminuria. Ages were 40, 40 and 43 years and estimated GFRs were >60, 83 and 72 ml min1 1.73 m2 in the three study groups, respectively. Mean duration of diabetes for the participants with type 1 diabetes was 27 and 28 years for the normoalbuminuria and microalbuminuric groups, respectively. All microalbuminuric participants were taking at least one reninangiotensin system inhibitor with six also taking additional antihypertensive therapy. Renal MRI was used to assess renal perfusion, tissue oxygenation and kidney size in the three groups. Mean renal artery flow (per single kidney) was lower in the whole diabetes cohort than in the control group (591 vs 740 ml min1 1.73 m2, p<0.05) when assessed by phase contrast angiography. Renal vascular resistance (RVR) was calculated as mean arterial pressure (mmHg) divided by total renal blood flow (ml min1 1.73 m2). RVR increased from control to normoalbuminuric subgroup to microalbuminuric subgroup of type 1 diabetic people (0.061 vs 0.077 vs 0.093 mm Hg ml1 min1.73 m2, p=0.01,
respectively). RVR correlated inversely with estimated GFR in normo- but not in microalbuminuric people. The authors suggest that decreases in renal blood flow in longstanding type 1 diabetes reflects intra-renal vascular stiffening and raise the possibility that in microalbuminuric patients it may also reflect increased intraglomerular pressure. However, since mean arterial pressure was 17% higher in the microalbuminuric than in the normoalbuminuric and control participants, this in itself could explain the increase in RVR in the microalbuminuric group. Both of the above studies demonstrate that changes in renal blood flow are demonstrable in patients with type 2 or type 1 diabetes before the onset of microalbuminuria, as currently defined. Both studies demonstrate changes in renal blood vessel function independent of increases in albuminuria. However, small increases in ACR were already evident in the normoalbuminuric individuals studied by Bruno et al. [7]. Both studies have certain limitations, in particular the small sample sizes. In addition, the lack of longitudinal data does not allow differentiation of cause, effect or association for the relationship of RI or RVR to the multiple clinical and vascular variables that were measured and included in the analyses. Furthermore, renal MRI remains a complex procedure that is not suited for large-scale application. Despite these limitations, the above studies have potential clinical importance since normoalbuminuric renal insufficiency occurs in both type 1 [911] and type 2 diabetes [1214], and may explain up to 25% of chronic kidney disease (CKD) in patients with type 2 diabetes [12, 13]. Normoalbuminuric renal insufficiency is not confined to diabetes and has also been described in large scale community studies [15]. The above studies raise the possibility that acute and long-term changes in blood vessels may contribute to the development of CKD in type 2 diabetes. Larger studies are needed in order to differentiate the separate roles of ischaemia, fibrosis, blood pressure, dyslipidaemia and glycaemic control in the evolution of CKD in both types of diabetes. Further dynamic renal RI studies that assess the effects of other endothelium-modulating agents, apart from glyceryl trinitrate, also need to be performed.
Acknowledgements Research in the authors departments has been supported by grants from the National Health and Medical Research Council, The Austin Medical Research Foundation, the Diabetes Australia Research Trust and a Cardio-V ascular-Lipid research grant from Pfizer. Both authors interpreted the data described in this commentary and contributed to the drafting and revising of the article. Both have approved the final version of the article. Duality of interest The authors declare that there is no duality of interest associated with this manuscript.
Diabetologia
References
1. Taniwaki H, Nishizawa Y Kawagishi T et al (1998) Decrease in , glomerular filtration rate in Japanese patients with type 2 diabetes is linked to atherosclerosis. Diabetes Care 21:18481855 2. MacIsaac R, Panagiotopoulos S, McNeil K et al (2006) Is nonalbuminuric renal insufficiency in type 2 diabetes related to an increase in intrarenal vascular disease? Diabetes Care 29:15601566 3. MacIsaac RJ, Thomas MC, Panagiotopoulos S et al (2008) Association between intrarenal arterial resistance and diastolic dysfunction in type 2 diabetes. Cardiovasc Diabetol 7:15 4. Nosadini R, V elussi M, Brocco E et al (2006) Increased renal arterial resistance predicts the course of renal function in type 2 diabetes with microalbuminuria. Diabetes 55:234239 5. Ohta Y Fujii K, Arima H et al (2005) Increased renal resistive , index in atherosclerosis and diabetic nephropathy assessed by Doppler sonography. J Hypertens 23:19051911 6. Taniwaki H, Ishimura E, Kawagishi T et al (2003) Intrarenal hemodynamic changes after captopril test in patients with type 2 diabetes: a duplex Doppler sonography study. Diabetes Care 26:132137 7. Bruno RM, Daghini E, Landini L et al (2011) Dynamic evaluation of renal resistive index in normoalbuminuric patients with newly diagnosed hypertension or type 2 diabetes. Diabetologia. doi:10.1007/s00125-011-2148-y 8. Thelwall PE, Taylor R, Marshall SM (2011) Non-invasive investigation of kidney disease in type 1 diabetes by magnetic
resonance imaging. Diabetologia. doi:10.1007/s00125-0112163-z 9. Caramori ML, Fioretto P Mauer M (2003) Low glomerular , filtration rate in normoalbuminuric type 1 diabetic patients: an indicator of more advanced glomerular lesions. Diabetes 52:1036 1040 10. Lane PH, Steffes MW, Mauer SM (1992) Glomerular structure in IDDM women with low glomerular filtration rate and normal urinary albumin excretion. Diabetes 41:581586 11. Molitch ME, Steffes M, Sun W et al (2010) Development and progression of renal insufficiency with and without albuminuria in adults with type 1 diabetes in the Diabetes Control and Complications Trial and the Epidemiology of Diabetes Interventions and Complications Study. Diabetes Care 33:15361543 12. Kramer HJ, Nguyen QD, Curhan G, Hsu CY (2003) Renal insufficiency in the absence of albuminuria and retinopathy among adults with type 2 diabetes mellitus. JAMA 289:32733277 13. MacIsaac RJ, Tsalamandris C, Panagiotopoulos S, Smith TJ, McNeil KJ, Jerums G (2004) Nonalbuminuric renal insufficiency in type 2 diabetes. Diabetes Care 27:195200 14. Tsalamandris C, Allen TJ, Gilbert RE et al (1994) Progressive decline in renal function in diabetic patients with and without albuminuria. Diabetes 43:649655 15. Thomas MC, Macisaac RJ, Jerums G et al (2009) Nonalbuminuric renal impairment in type 2 diabetic patients and in the general population (National Evaluation of the Frequency of Renal impairment cO-existing with NIDDM [NEFRON] 11). Diabetes Care 32:14971502
Você também pode gostar
- Prismaflex User ManualDocumento287 páginasPrismaflex User ManualMahmoud Diaa78% (9)
- The Yellow House: A Memoir (2019 National Book Award Winner)No EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Nota: 4 de 5 estrelas4/5 (98)
- Prevention and Treatment of Systemic Glucocorticoid Side EffectsDocumento10 páginasPrevention and Treatment of Systemic Glucocorticoid Side EffectsMahmoud DiaaAinda não há avaliações
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeNo EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeNota: 4 de 5 estrelas4/5 (5795)
- Retained Catheter Fragment From A Fractured Tunneled Catheter-A Rare and Potentially Lethal ComplicationDocumento4 páginasRetained Catheter Fragment From A Fractured Tunneled Catheter-A Rare and Potentially Lethal ComplicationMahmoud DiaaAinda não há avaliações
- Never Split the Difference: Negotiating As If Your Life Depended On ItNo EverandNever Split the Difference: Negotiating As If Your Life Depended On ItNota: 4.5 de 5 estrelas4.5/5 (838)
- Acute Hypercapnic Respiratory Failure Associated With HemodialysisDocumento3 páginasAcute Hypercapnic Respiratory Failure Associated With HemodialysisMahmoud DiaaAinda não há avaliações
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceNo EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceNota: 4 de 5 estrelas4/5 (895)
- 3 1 - N U M B e R 2 - 2 0 1 1: Official Publication of The Spanish Society of NephrologyDocumento117 páginas3 1 - N U M B e R 2 - 2 0 1 1: Official Publication of The Spanish Society of NephrologyMahmoud DiaaAinda não há avaliações
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersNo EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersNota: 4.5 de 5 estrelas4.5/5 (345)
- Avoiding Common Technical Errors in Subclavian Central Venous Catheter PlacementDocumento6 páginasAvoiding Common Technical Errors in Subclavian Central Venous Catheter PlacementMahmoud DiaaAinda não há avaliações
- The Value of Failure: The Discovery of TNF and Its Natural Inhibitor Erythropoietin, A. CeramiDocumento8 páginasThe Value of Failure: The Discovery of TNF and Its Natural Inhibitor Erythropoietin, A. CeramiMahmoud DiaaAinda não há avaliações
- Flash Pulmonary Oedema and Bilateral Renal Artery Stenosis: The Pickering SyndromeDocumento8 páginasFlash Pulmonary Oedema and Bilateral Renal Artery Stenosis: The Pickering SyndromeMahmoud DiaaAinda não há avaliações
- The Little Book of Hygge: Danish Secrets to Happy LivingNo EverandThe Little Book of Hygge: Danish Secrets to Happy LivingNota: 3.5 de 5 estrelas3.5/5 (400)
- Belco Formula User ManualDocumento386 páginasBelco Formula User ManualMahmoud Diaa100% (21)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureNo EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureNota: 4.5 de 5 estrelas4.5/5 (474)
- Composition and Clinical Use of HemodialysatesDocumento14 páginasComposition and Clinical Use of HemodialysatesMahmoud DiaaAinda não há avaliações
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryNo EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryNota: 3.5 de 5 estrelas3.5/5 (231)
- Gambro AK 96® Dialysis Machine Operator's ManualDocumento506 páginasGambro AK 96® Dialysis Machine Operator's ManualMahmoud Diaa90% (67)
- Nephrology Underpinning For The Young DoctorsDocumento7 páginasNephrology Underpinning For The Young DoctorsMahmoud DiaaAinda não há avaliações
- The Emperor of All Maladies: A Biography of CancerNo EverandThe Emperor of All Maladies: A Biography of CancerNota: 4.5 de 5 estrelas4.5/5 (271)
- Locking Solutions For Hemodialysis Catheters Heparin and Citrate - A Position Paper by ASDIN.Documento3 páginasLocking Solutions For Hemodialysis Catheters Heparin and Citrate - A Position Paper by ASDIN.Mahmoud DiaaAinda não há avaliações
- Biology 9 Science Al-Raza Institute Paper I Group-I Time Allowed: 20 Min Objective Marks: 12Documento3 páginasBiology 9 Science Al-Raza Institute Paper I Group-I Time Allowed: 20 Min Objective Marks: 12Anonymous WDvB6A0Ainda não há avaliações
- Mother's Class BFDocumento55 páginasMother's Class BFriz04_fortitudessa5178Ainda não há avaliações
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaNo EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaNota: 4.5 de 5 estrelas4.5/5 (266)
- Acute Coronary Syndrome: An Essential & Practical ApproachDocumento35 páginasAcute Coronary Syndrome: An Essential & Practical ApproachGinawidiyastutiAinda não há avaliações
- The Unwinding: An Inner History of the New AmericaNo EverandThe Unwinding: An Inner History of the New AmericaNota: 4 de 5 estrelas4/5 (45)
- Class 11 Compiled Chintu Notes ..Documento76 páginasClass 11 Compiled Chintu Notes ..Mohammed ArifuddinAinda não há avaliações
- Team of Rivals: The Political Genius of Abraham LincolnNo EverandTeam of Rivals: The Political Genius of Abraham LincolnNota: 4.5 de 5 estrelas4.5/5 (234)
- About HyenaDocumento24 páginasAbout HyenaRiswan Hanafyah Harahap0% (1)
- Trilemma Adventures BestiaryDocumento17 páginasTrilemma Adventures BestiaryZamak50% (2)
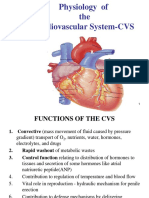
- Physiology of The Cardiovascular System-CVSDocumento56 páginasPhysiology of The Cardiovascular System-CVSAmanuel MaruAinda não há avaliações
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyNo EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyNota: 3.5 de 5 estrelas3.5/5 (2259)
- The Endocrine SystemDocumento12 páginasThe Endocrine Systemmagma_pt9888Ainda não há avaliações
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreNo EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreNota: 4 de 5 estrelas4/5 (1091)
- Macro - Micronutrients and Their Sources and FunctionsDocumento12 páginasMacro - Micronutrients and Their Sources and FunctionsClayohj Alliana0% (1)
- BeekeepingDocumento17 páginasBeekeepingApollon Phebo0% (1)
- Cholesterol PresentationDocumento28 páginasCholesterol Presentationapi-240098169Ainda não há avaliações
- Protozoa PowerpointDocumento36 páginasProtozoa PowerpointHarriza Macapundag Haron-GangcoAinda não há avaliações
- Casos Clinicos de Hematopatología IiDocumento5 páginasCasos Clinicos de Hematopatología IiRicardo LaraAinda não há avaliações
- Andy SmithDocumento14 páginasAndy SmithNational Academies of Science, Engineering, and MedicineAinda não há avaliações
- Bryonia Phosphorus Sepiaand MedorrhinumDocumento39 páginasBryonia Phosphorus Sepiaand Medorrhinummihaipopescu0100% (1)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)No EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Nota: 4.5 de 5 estrelas4.5/5 (121)
- Philippine Dental Association Covid 19 Monitoring FormDocumento1 páginaPhilippine Dental Association Covid 19 Monitoring Formrhusolano rhusolanoAinda não há avaliações
- n213 Unit 2 BDocumento390 páginasn213 Unit 2 BJeonghwa Park100% (1)
- Gas Exchange in Humans (Multiple Choice) QP PDFDocumento12 páginasGas Exchange in Humans (Multiple Choice) QP PDFSyakir Fahmie100% (2)
- Pulmonary Physiology of The NewbornDocumento39 páginasPulmonary Physiology of The NewbornADAinda não há avaliações
- Sexual SelfDocumento19 páginasSexual SelfErica SisgonAinda não há avaliações
- Roland Barthes - Steak and ChipsDocumento3 páginasRoland Barthes - Steak and ChipsmishaiolandaAinda não há avaliações
- Newborn Nursing CareplanDocumento7 páginasNewborn Nursing CareplanSamantha MillerAinda não há avaliações
- John W. Campbell - Who Goes There-Rosettabooks (2001)Documento56 páginasJohn W. Campbell - Who Goes There-Rosettabooks (2001)Manuel KlosterAinda não há avaliações
- Color Therapy GeneralDocumento39 páginasColor Therapy GeneralNowo BudirahardjoAinda não há avaliações
- Eipecs - Eipisi:z) : Vârf, CulmeDocumento4 páginasEipecs - Eipisi:z) : Vârf, CulmeAlina CimpeanuAinda não há avaliações
- Jurnal Striktur NcbiDocumento5 páginasJurnal Striktur NcbiYohana Elisabeth GultomAinda não há avaliações
- Cranial Nerves Assessment FormDocumento3 páginasCranial Nerves Assessment FormCristina CenturionAinda não há avaliações
- Most Expected Vocabulary Ebook by Prashant SirDocumento35 páginasMost Expected Vocabulary Ebook by Prashant SirPriya GuptaAinda não há avaliações
- Determination of ParasitemiaDocumento4 páginasDetermination of ParasitemiaDoctorKawaiiAinda não há avaliações
- Comparison of The YMCA Cycle SubDocumento2 páginasComparison of The YMCA Cycle SubBryan Allen Q. ValleAinda não há avaliações
- LIT: Life Ignition Tools: Use Nature's Playbook to Energize Your Brain, Spark Ideas, and Ignite ActionNo EverandLIT: Life Ignition Tools: Use Nature's Playbook to Energize Your Brain, Spark Ideas, and Ignite ActionNota: 4 de 5 estrelas4/5 (404)