Escolar Documentos
Profissional Documentos
Cultura Documentos
Hematologic Disorders
Enviado por
Cernan OliverosDescrição original:
Direitos autorais
Formatos disponíveis
Compartilhar este documento
Compartilhar ou incorporar documento
Você considera este documento útil?
Este conteúdo é inapropriado?
Denunciar este documentoDireitos autorais:
Formatos disponíveis
Hematologic Disorders
Enviado por
Cernan OliverosDireitos autorais:
Formatos disponíveis
Medical- Surgical Nursing
Hematologic Disorders
HEMATOLOGIC DISORDERS
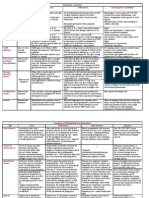
I. Disorders of the RBC A. Anemias A.1 Hypoproliferative - Caused by decreased RBC production. This type of anemia can result from the inability of the bone marrow to properly produce RBCs or the failure of the body to make or absorb substances needed for PBC production A.1.1 Iron Deficiency Anemia - Results when the intake of dietary iron is inadequate for hemoglobin synthesis. - Microcytic, hypochromic
PATHOPHYSIOLOGY
ASSESSMENT FINDINGS
INTERVENTIONS
MEDICATIONS
Blood loss, poor intestinal absorption, inadequate diet iron stores become depleted RBCs become microcytic manifestation s of anemia
y Decreased levels of hemoglobin and MCV, which measures the size of RBC y Hematocrit and RBC levels are also low y Vinson- Plummers Syndrome y Stomatitis y Dysphagia y Atrophic glossitis (small, sore tongue) y Cheilosis- cracks at the side of the lips y Koilonychia- spoon- shaped or concave finger nails y Pica- craving of non-edible substances. y Tinnitus- ringing of the ear y If HGB= 7.5g/dL or below- increased PR, chest pain, SOB, CHF
Medical Management 1. Colonoscopy, endoscopy or x-ray examination of GIT to detect ulcerations, gastritis, polyps or cancer 2. Oxygen therapy 3. Blood transfusion as needed Nursing interventions 1. Preventive education 2. Promote healthy diet. Iron-rich foods like organ meat, lean meat, egg yolk, beans, GLV, raisins, dried fruits 3. Promote rest 4. Provide good skin and oral care.
y Oral iron preparations y Ferrous sulfate y Ferrous gluconate y Ferrous fumarate y IV or IM dextran
A.1.2 Vit B12 Deficiency Anemia - Caused by faulty absorption of Vitamin B12 in the GIT. May be caused by Chrons disease, gastric surgery, autoimmune gastric mucosal atrophy Decreased intrinsic factor production - Pernicious Anemia - Megaloblastic anemia - Macrocytic, Hyperchromic A.1.3 Folic Acid Deficiency Anemia - May be caused by inadequate dietary intake of folic acid, malabsorption, chronic alcoholism and drugs
Decreased production of INTRINSIC FACTOR Decreased absorption of Vitamin B12 Decreased DNA synthesis in maturing RBC (megaloblastic cells) Decreased RBC production
y Signs of anemia y Neurologic manifestations such as paresthesia (numbness and tingling in the feet and lower legs), uncoordinated balance, poor sense of position y Jaundice y Beefy red tongue y Mild diarrhea
Collaborative Management 1. Encourage increased intake of foods rich in vitamin B12 2. Blood transfusion as needed 3. Hematologic and GI evaluation every 6 months 4. Schilling test
y y y y
Monthly vitamin B12 IM for life Folic acid Ferrous sulfate Diluted HCl
Decreased availability of folic acid Impaired DNA synthesis in maturing RBC (megaloblastic cells) Decreased RBC production
y y y y
Cracked lips, sore tongue Decreased RBC, HGB, HCT Increased MCV and MCHC Absence of neurologic problems unlike in pernicious anemia
Collaborative Management 1. Promote healthy diet. Encourage increased intake of GLV, fruits and meat 2. Tell patients to avoid over- cooking of vegetables
y Folic acid per orem
Prepared by: | Aljon R Pelayo/USTSN
- Megaloblastic anemia - Macrocytic, Hyperchromic
A.1.4 Aplastic Anemia -Deficiency of the circulating RBC because of the failure of the bone marrow to produce these cells. - Can be caused by a decrease in or damage to marrow stem cells, damage to the microenvironment within the marrow, and replacement of the marrow with fat - Results in bone marrow aplasia, markedly reduced hematopoeisis - nuetropenia and thrombocytopenia are also seen
- Can be congenital or acquired, but most cases are idiopathic - May also be triggered by medications, chemicals, or radiation damage.
y Bone Marrow Aspiration: extremely hypoplastic or even aplastic (very few to no cells) marrow replaced with fat. y Pancytopenia y Anemia y Infection y Bleeding
Medical Management 1. Bone Marrow Transplantation (BMT) 2. Peripheral Blood Stem Cell Transplantation (PBSCT) 3. Immunosuppressive therapy 4. Blood transfusion as needed Nursing Intervention 1. Assess carefully for signs of tissue hypoxia, infection and bleeding 2. Promote rest 3. Minimize risk for infection 4. Minimize risk for bleeding
y y y y y y
Corticosteroids Clyclosporine Cyclophosphamide Antithymocyte globulin Antilymphovyte globulin Azathioprine
A.2 Bleeding - RBC loss due to bleeding from GIT, menorrhagia (excessive menstrual flow), epistaxis (nose bleed), or wound
Bleeding Blood loss Excessive RBC loss Manifestations of anemia
y y y y y y y
Pallor Weakness Anorexia Weight loss Headache/ Dizziness Tachycardia/ Palpitations Syncope
Collaborative Management 1. Treat the cause of bleeding 2. Hold drugs that may further cause bleeding 3. Blood transfusion as needed 4. Cryoprecipitate or platelet transfusion
y Erythropoetin
A.3 Hemolytic A.3.1 Sickle Cell Anemia - a severe hemolytic anemia that results from inheritance of the sickle cell hemoglobin gene
Low oxygen tension p Crystal like formation of RBCs p erythrocyte containing HbS loses its round, pliable, biconcave disk shape p adhere to each other p decreased blood flow
y y y y y y y y y
Pain Swelling Fever Anemia Jaundice Expansion of bone marrows Enlarged heart Dysrythmias Heart failure
Medical Management 1. Pharmacologic Therapy 2. Transfusion Therapy 3. Supportive Therapy Nursing Interventions 1. Manage pain 2. Monitor for signs and symptoms of infection 3. Promote coping 4. minimizing deficient knowledge 5. Monitoring and managing potential complications
y Analgesics y Antibiotics
B. Polycythemias B.1 Polycytemia vera - Hyperplasia of the bone marrow - compensatory response to chronic hypoxia Hypoxia increased erythropoietin production stimulation of the bone marrow Increased RBC production y y y y y y y increased RBC, WBC, platelet Ruddy complexion Headache Dizziness Fatigue Blurred vision Hepatosplenomegaly Collaborative Management 1. Increase fluid intake 2. Monitor for signs and symptoms of bleeding and thromboembolism 3. Therapeutic phlebotomy 4. Chemotherapy 5. Radiation therapy y Analgesics y Antihistamine
2 Prepared by: | Aljon R Pelayo/USTSN
II.
Disorders of the WBC A. Leukopenia and Nuetropenia y A condition in which there are fewer than normal WBCs.
y This may be due to a decrease in production or an increase in destruction. Patients with this condition are at greater risk for infections.
y There are no definite symptoms until the patient becomes infected y CBC can reveal neutropenia before the onset of infection
Medical Management 1. If neutropenia is medication induced, the offending agent must be stopped 2. Bone marrow recovery treatment 3. Withholding or reducing the dose of chemotherapy or radiation may be required 4. Blood, urine and sputum cultures Nursing Interventions 1. Assess for the severity of the neutropenia 2. Preventing and managing infections 3. Early detection of infection must be done
y Granulocyte/ Macrophage stimulating factor y Corticosteroids
B. Luekocytosis and the Leukemias B.1 Acute Lymphocytic Leukemia - results from an uncontrolled proliferation of immature cells (lymphoblast) derived from the lymphoid stem cell y Immature lymphocytes proliferate crowd the normal development of myeloid cells normal hematopoeisis is inhibited Decreased numbers of leukocytes, erythrocytes and thrombocytes y Increased number of lymphocytes y Decreased numbers of leukocytes, erythrocytes and thrombocytes y High proportion of immature cells y Pain y Enlarged liver or spleen y Bone pain y Headache y vomiting Medical Management 1. Goal: complete remission 2. Prophylaxis with cranial irradiation and intrathecal chemotherapy 3. Bone Marrow transplantation (BMT) 4. Peripheral Blood Stem Cell Transplantation (PBSCT) y Wide variety of chemotherapeutic agents
B.2 Chronic Lymphocytic Leukemia
y Derives From a malignant clone of B lymphocytes
y Most leukemia cells are fully mature y Increased lymphocyte count (lymphocytosis) is always present y Lymphadenopathy y Pain y Splenomegaly y B symptoms y Fever y Drenching sweating y Unintentional weight loss
Medical Management 1. In early stages, CLL does not require any treatment 2. When symptoms become severe or progress to later stages, chemotherapy with corticosteroids and chlorambucil is often used.
y y y y
Chlorambucil Corticosteroids Fludarabine Monoclonal Antibodies
B.3 Acute Myeloid Leukemia - Results from a defect in the hematopoietic stem cell that differentiates into myeloid cells: monocytes, granulocytes, erythrocytes and platelets
y Defect in the hematopoietic stem cell that differentiates into myeloid cells will result into pancytopenia
y Insufficient production of normal blood cells y CBC results may show decrease in erythrocytes and thrombocytes; although leukocyte count can be low, normal or high y Bone marrow analysis may show
Medical Management 1. Goal: achieve complete remission in which there is no detectable evidence of residual leukemia remaining in the bone marrow 2. Aggressive administration of chemotherapeutic agents
y y y y y y
Cytarabine Daunorubicin Mitoxantrone Idarubicin G- CSF GM- CSF
Prepared by: | Aljon R Pelayo/USTSN
increased numbers of blast cells y Fever and infection that results from neutropenia y Bleeding tendencies from thrombocytopenia y Enlarged liver and spleen y Hyperplasia of gums y Bone pain B.4 Chronic Myeloid Leukemia - Arises from a mutation in the myeloid stem cell. Normal myeloid cells continue to be produced, but there is a preference for immature (blast) forms.
3. Bone Marrow transplantation (BMT) 4. Peripheral Blood Stem Cell Transplantation (PBSCT)
Mutation in the myeloid stem cell p overproduction in blast cells p expansion of marrow into the cavities of long bones p formation of cells in the liver and spleen p enlargement of these organs
y WBC count commonly exceeds 3 100,000/mm y Shortness of breath y Decreased capillary perfusion to the lungs and brain from leukostasis y Enlarged and tender spleen y Enlargement of the liver y Malaise, anorexia and weight loss
Medical Management 1. Goal: Less aggressive therapeutic approach that focuses on reducing the WBC count to normal level, but does not alter cytogenetic changes 2. Correction of the chromosomal abnormality (conversion of the malignant stem cell population back to normal) 3. Chemotherapy 4. Bone Marrow transplantation (BMT) 5. Peripheral Blood Stem Cell Transplantation (PBSCT)
y y y y
Imatinib Interferon alpha Busulfan Hydroxyurea
Nursing Interventions (for all types of Leukemia) 1. Preventing and managing infection and bleeding 2. Provide good skin and oral care 3. Improving nutritional intake 4. Easing pain and discomfort 5. Decreasing fatigue and deconditioning 6. Maintaining fluid and electrolyte imbalance 7. Improving self- care 8. Managing anxiety and grief 9. Encouraging spiritual well- being 10. Monitoring and managing potential complications III. The Lymphomas A. Hodgkins Disease - neoplastic disorder affecting the lymphnodes Reed-Sternberg cells p Initiates in single node p contiguous extension along the lymphatic system y y y y y y y y y y Reed- Sternberg cells Fever, chills, malaise Night sweats Weight loss Pruritus Edema Abdominal pain Splenomegaly Hepatomegaly Cough and dyspnea Medical Management 1. Radiation therapy 2. Chemotherapy 3. Bone Marrow Transplantation Nursing Interventions 1. Prevention of infection 2. Small frequent feeding 3. Encourage patient to avoid alcohol, tobacco, spices, and extreme food temperatures y y y y y y y y Mustargen Oncovin Procarbazine Prednisone Adriamycin Bleomycin Vinblastine Dacarbazine
4 Prepared by: | Aljon R Pelayo/USTSN
B. Non- Hodgkins Lymphomas (NHL) y Lymphosarcoma or Burkitts sarcoma
Neoplastic growth of lymphoid tissue p spread of these malignant lymphoid cells
y Lymphadenopathy y B symptoms (recurrent fever, drenching night sweats, unintentional weight loss of 10% or more)
Medical Management 1. Radiation therapy 2. Chemotherapy Nursing Interventions 1. Prevention of infection
y y y y y
Cytoxan Adriamycin Oncovin Prednisone Blenoxane
C. Multiple Myeloma y Proliferation of abnormal plasma cells in the bone marrow
Malignant plasma cells produce an increased amount of a specific immunoglobulin that is nonfunctional They also stimulate the creation of new blood vessels to enhance the growth of these clusters of plasma cells
y y y y y y y y
Elevated monoclonal protein spike in the serum or urine- Bence- Jones Protein Bone lesions in x-ray Severe bone pain Fatigue and weakness Hyperviscosity of the blood Bleeding Proteinuria Hypercalcemia and hyperuricemia
Collaborative Management 1. Chemotherapy 2. Plasmapheresis
y y y y
Cytoxan Alkeran Corticosteroids Alpha interferon
IV.
The Bleeding Disorders
A. Thrombocythemia A.1 Primary - Also called Essential Thrombocythemia - stem cell disorder within the marrow - A marked increase in platelet production occurs, with platelet count consistently 3 greater than 600,000/mm
Exact cause is unknown
y y y
Asymptomatic CBC reveals elevated levels of platelet Bane Marrow (by aspiration or biopsy) shows a marked increase in megakaryocytes (platelet precursors)
Medical Management 1. Platelet pheresis 2. Lower platelet production Nursing Interventions 1. Instruct the patient about the risk of hemorrhage and thrombosis 2. Inform patient about signs and symptoms of thrombosis, particularly the neurologic manifestations, such as visual changes, numbness, tingling, and weakness 3. Reduce risk factors for bleeding and thrombosis
A.2 Secondary - Reactive thrombocytosis B. Thrombocytopenia B.1 Primary - Decreased production of platelet within the bone marrow, increased destruction of platelets, or increased consumption of y Bone marrow aspiration may show increased megakaryocytes and normal or even increased platelet production as the body attempt to compensate for the
Collaborative Management 1. Treatment is aimed at the underlying disorder
Medical Management 1. Treatment of the underlying disease 2. Platelet transfusion
y Steroids y IV immunoglobulin y Avoid use of ASA and NSAIDs
Prepared by: | Aljon R Pelayo/USTSN
platelets y
decreased platelet in the circulation Splenomegaly
Nursing Intervention 1. Prevent and control bleeding 2. Prevent complications 3. Monitor for signs of bleeding
B.2 ITP - platelets clump together abnormally in the capillaries and too few platelets remain in the circulation
y y
Autoimmune disorder Sulfa drugs, pregnancy and SLE may iduce ITP
y y y y
Isolated decrease in platelet, less tham 3 20,00/ mm They may also have an increase in megakaryocytes within the marrow Easy bruising Hemoptysis
Medical Management 1. Goal: safe platelet count 2. Immunosuppressive agents 3. Platelet transfusion 4. Splenectomy Nursing Interventions 1. Bleeding precautions
y Corticosteroids y IV immunoglobulin y Danazol y Immuran y Oncovin y Velban
C. Platelet Defects y Platelet level may be normal but nonfunctional
y y y
Prolonged bleeding time Increased PT and PTT Ecchymoses
Collaborative Managemant 1. Platelet transfusion 2. Bleeding precautions 3. Control and management of bleeding
y Aminocaproic acid
D. Hemophilia - Inherited bleeding disorder - Absence of a specific clotting factor, either factor VIII or factor IX
Autosomal recessive disorder wherein there is a lack of a clotting factor that is essential for the clotting cascade to pursue
y y y
Bleeding Hematomas Joint pain
Collaborative Management 1. Administration of factor VIII or factor IX concentrates 2. Bleeding precautions 3. Instruct the patient to avoid contact sports 4. Avoid medications that may further aggravate the patients condition
y Aminocaproic acid y Desmopressin
E. Von Willebrands Disease y It is an inherited, autosomal dominant, disorder characterized by a decrease in the Von Willebrand factor and prolonged bleeding time V. The Coagulation Disorders A. Vitamin K Deficiency y Vitamin K is essential in the formation of some clotting factors. Absence of this vitamin will interfere the normal clotting cascade
y Epistaxis y Normal platelet count but slightly prolonged PTT y Heavy menses
Collaborative Management 1. Factor VII replacement via infusions of cryoprecipitate 2. Bleeding precautions
y Aminocaproic acid y Desmopressin
y Prolonged PT y Prolonged bleeding time
Collaborative Management 1. Administration of Vitamin K 2. Bleeding precaution
y Vitamin K
B. Dissemintaed Intravascular Coaggulation - Acquired thrombolytic and hemorrhagic syndrome
Widespread bleeding clotting in small vessels of the body with consumption of clotting factors and platelets, so that bleeding and thrombosis occurs simultaneously
y y
Signs of abnormal clotting y Coolness and mottling of extremities y Acrocyanosis y Hematuria y Altered mental status y Pain Signs of abnormal bleeding ]oozing, bleeding from sites of
Collaborative Management 1. Bleeding precautions 2. Replacement therapy (fresh frozen plasma, platelet transfusion, cryoprecipitate) 3. Fluid replacement 4. Oxygen therapy 5. Maintenance of BP
y Heparin
6 Prepared by: | Aljon R Pelayo/USTSN
y y y y
procedures Internal bleeding Low platelet count Prolonged PT, PTT Decreased fibrinogen level
7 Prepared by: | Aljon R Pelayo/USTSN
Você também pode gostar
- Hematologic ProblemsDocumento26 páginasHematologic Problemsapi-3735995100% (2)
- Anemia NotesDocumento6 páginasAnemia NotesElstella Eguavoen Ehicheoya100% (2)
- Blood Disorders AnemiaDocumento6 páginasBlood Disorders AnemiaFreeNursingNotesAinda não há avaliações
- Practice Teaching On Anemia: Presented By: Mr. Hari Singh Nagar M. SC Nursing 1 YearDocumento44 páginasPractice Teaching On Anemia: Presented By: Mr. Hari Singh Nagar M. SC Nursing 1 YearSundarAinda não há avaliações
- Anemia: Ch. 31 Hematologic ProblemsDocumento36 páginasAnemia: Ch. 31 Hematologic Problemshops23100% (3)
- All Objectives HematologyDocumento45 páginasAll Objectives HematologyNursing200980% (5)
- Hematologic Disorders NotesDocumento19 páginasHematologic Disorders Notesmikkagreen95% (22)
- Hematologic SystemDocumento81 páginasHematologic Systemseigelystic100% (23)
- HEMATOLOGYDocumento10 páginasHEMATOLOGYJo Marchianne Pigar100% (8)
- Hematologic Diseases OverviewDocumento11 páginasHematologic Diseases OverviewPerrilyn Perey100% (2)
- Hematologic DisordersDocumento32 páginasHematologic DisordersQuolette ConstanteAinda não há avaliações
- Hematologic DisorderDocumento16 páginasHematologic Disorderjulesubayubay5428Ainda não há avaliações
- Summary of All AnemiaDocumento2 páginasSummary of All Anemiabenlarsena93% (14)
- Management of Tuberculosis: A guide for clinicians (eBook edition)No EverandManagement of Tuberculosis: A guide for clinicians (eBook edition)Ainda não há avaliações
- Hematologic DisorderDocumento7 páginasHematologic Disordermawel100% (2)
- Blood Disorders - HandoutDocumento8 páginasBlood Disorders - Handoutapi-335571917100% (1)
- Transfusion Reaction - DRGSPDocumento42 páginasTransfusion Reaction - DRGSPGaurav PawarAinda não há avaliações
- Problem-based Approach to Gastroenterology and HepatologyNo EverandProblem-based Approach to Gastroenterology and HepatologyJohn N. PlevrisAinda não há avaliações
- Hematologic DisordersDocumento40 páginasHematologic DisordersMary Grace LeronAinda não há avaliações
- Hematology NotesDocumento17 páginasHematology NotesEly Sibayan100% (2)
- 2013-Oncology New QuestionsDocumento5 páginas2013-Oncology New QuestionsHarley Justiniani Dela CruzAinda não há avaliações
- Mastectomy patient chemotherapy side effects NCLEX reviewDocumento4 páginasMastectomy patient chemotherapy side effects NCLEX reviewTinAinda não há avaliações
- Hematologic System and DisordersDocumento68 páginasHematologic System and DisordersRellie Castro100% (1)
- Approach To Diagnosis of Haemolytic AnaemiasDocumento2 páginasApproach To Diagnosis of Haemolytic AnaemiasGerardLumAinda não há avaliações
- Hematology QuestionsDocumento7 páginasHematology QuestionsRaven Atisha100% (1)
- LupusDocumento28 páginasLupusRiin IrasustaAinda não há avaliações
- 80 TOP Hematology MCQADocumento25 páginas80 TOP Hematology MCQASelva Kumaran100% (2)
- Hematology Tables Morphology of RBCsDocumento5 páginasHematology Tables Morphology of RBCsGlydenne Glaire Poncardas GayamAinda não há avaliações
- Hemolytic AnemiaDocumento9 páginasHemolytic AnemiaTheeya QuigaoAinda não há avaliações
- Hematology QuestionsDocumento13 páginasHematology QuestionsGlazel TulaganAinda não há avaliações
- Iron Deficiency AnemiaDocumento5 páginasIron Deficiency AnemiaLoiegy PaetAinda não há avaliações
- PHM - Hematologic DrugsDocumento3 páginasPHM - Hematologic DrugsJeanne Rodiño100% (2)
- Prothrombin Time: Reference Range, Interpretation, Collection and ..Documento3 páginasProthrombin Time: Reference Range, Interpretation, Collection and ..Francis Polycarp DiazAinda não há avaliações
- Hemotology Pathology PDFDocumento15 páginasHemotology Pathology PDFMorgan PeggAinda não há avaliações
- Lymphoid NeoplasmsDocumento52 páginasLymphoid NeoplasmsAmalia Riska GAinda não há avaliações
- Immunology & Oncology Review 2Documento99 páginasImmunology & Oncology Review 2Melchor Felipe SalvosaAinda não há avaliações
- Hematological NursingDocumento4 páginasHematological Nursingkhaeydianco100% (5)
- Acute Lymphoblastic Leukemia Pathophysiology DiagramDocumento3 páginasAcute Lymphoblastic Leukemia Pathophysiology DiagramChris FacundoAinda não há avaliações
- Hemophilia Nursing CareDocumento10 páginasHemophilia Nursing CareEla 15Ainda não há avaliações
- Quiz Hematology Oncology Part 2 of 2Documento60 páginasQuiz Hematology Oncology Part 2 of 2MedShare100% (5)
- Hemolytic AnemiaDocumento99 páginasHemolytic AnemiaSagar Chandrakant Mhetre100% (3)
- 81 HematologyDocumento18 páginas81 HematologyLuis Perez100% (5)
- Blood & Blood Products GuideDocumento52 páginasBlood & Blood Products Guidewellawalalasith100% (1)
- White Blood Cell DisordersDocumento9 páginasWhite Blood Cell DisordersDocAxi Maximo Jr AxibalAinda não há avaliações
- Hematology I Final Study GuideDocumento28 páginasHematology I Final Study GuideLauren Napoli100% (1)
- UrinalysisDocumento3 páginasUrinalysisKim MoranoAinda não há avaliações
- Cardiac MarkersDocumento23 páginasCardiac MarkersAsmaaYLAinda não há avaliações
- Syphilis: Etiology, Pathogenesis, Transmission, Stages, Manifestations and TreatmentDocumento39 páginasSyphilis: Etiology, Pathogenesis, Transmission, Stages, Manifestations and TreatmentEINSTEIN2D100% (1)
- Acute Lymphoblastic Leukemia QuestionsDocumento22 páginasAcute Lymphoblastic Leukemia Questionsđoàn lươngAinda não há avaliações
- Hodgkin's DiseaseDocumento58 páginasHodgkin's Diseasealibayaty1Ainda não há avaliações
- Coagulation TestsDocumento25 páginasCoagulation Testsdave_1128Ainda não há avaliações
- Blood Products: Product DescriptionDocumento3 páginasBlood Products: Product Descriptionkaychi zAinda não há avaliações
- Iron Deficiency AnaemiaDocumento132 páginasIron Deficiency AnaemiaHectorAinda não há avaliações
- Fluid, Electrolyte, and Acid-BaseDocumento6 páginasFluid, Electrolyte, and Acid-BaseRaquel MonsalveAinda não há avaliações
- Management of Patient With AnemiaDocumento58 páginasManagement of Patient With AnemiaDoaa HussainAinda não há avaliações
- Anemia Nursing Care Plan: Presented by Edi Purwanto School of Nursing University of Muhammadiyah MalangDocumento26 páginasAnemia Nursing Care Plan: Presented by Edi Purwanto School of Nursing University of Muhammadiyah MalangSevina Eka ChannelAinda não há avaliações
- Blood DisordersDocumento72 páginasBlood DisordersAngel Bar100% (1)
- Anemia During PregnancyDocumento39 páginasAnemia During PregnancyBhawna JoshiAinda não há avaliações
- Slus 008.96Documento5 páginasSlus 008.96Cernan OliverosAinda não há avaliações
- Unit 1 C H N: A O: What Is A Community ?Documento43 páginasUnit 1 C H N: A O: What Is A Community ?Marcus, RN96% (49)
- Intracranial BleedingDocumento18 páginasIntracranial BleedingCernan OliverosAinda não há avaliações
- HistoReview 1stshift PDFDocumento17 páginasHistoReview 1stshift PDFCernan OliverosAinda não há avaliações
- Hematologic DisordersDocumento7 páginasHematologic DisordersCernan Oliveros100% (2)
- Nursing Memory JoggersDocumento2 páginasNursing Memory JoggersMarcus, RN96% (24)
- RC Course SyllabusDocumento9 páginasRC Course SyllabusCernan OliverosAinda não há avaliações
- Recent Developments in Ultrasonic NDT Modelling in CIVADocumento7 páginasRecent Developments in Ultrasonic NDT Modelling in CIVAcal2_uniAinda não há avaliações
- Asus X553MA Repair Guide Rev2.0Documento7 páginasAsus X553MA Repair Guide Rev2.0UMA AKANDU UCHEAinda não há avaliações
- GSMA Moile Money Philippines Case Study V X21 21Documento23 páginasGSMA Moile Money Philippines Case Study V X21 21davidcloud99Ainda não há avaliações
- 6470b0e5f337ed00180c05a4 - ## - Atomic Structure - DPP-01 (Of Lec-03) - Arjuna NEET 2024Documento3 páginas6470b0e5f337ed00180c05a4 - ## - Atomic Structure - DPP-01 (Of Lec-03) - Arjuna NEET 2024Lalit SinghAinda não há avaliações
- GEHC DICOM Conformance CentricityRadiologyRA600 V6 1 DCM 1030 001 Rev6 1 1Documento73 páginasGEHC DICOM Conformance CentricityRadiologyRA600 V6 1 DCM 1030 001 Rev6 1 1mrzdravko15Ainda não há avaliações
- MF-QA-001 PDIR ReportDocumento2 páginasMF-QA-001 PDIR ReportBHUSHAN BAGULAinda não há avaliações
- Axel LeijonhufvudDocumento7 páginasAxel LeijonhufvudDario CoceresAinda não há avaliações
- Gantt Chart Engr110 - Gantt Chart Template 3Documento1 páginaGantt Chart Engr110 - Gantt Chart Template 3api-375485735Ainda não há avaliações
- Amna Hameed: ObjectiveDocumento2 páginasAmna Hameed: ObjectiveSabrina GandapurAinda não há avaliações
- Download 12,000 Shed PlansDocumento27 páginasDownload 12,000 Shed PlansRadu_IS100% (2)
- 20comm Um003 - en PDocumento270 páginas20comm Um003 - en PRogério BotelhoAinda não há avaliações
- OTGNNDocumento13 páginasOTGNNAnh Vuong TuanAinda não há avaliações
- Variolink Esthetic Brochure 673400Documento6 páginasVariolink Esthetic Brochure 673400wuhan lalalaAinda não há avaliações
- Seminar 6 Precision AttachmentsDocumento30 páginasSeminar 6 Precision AttachmentsAmit Sadhwani67% (3)
- Symasym BBDocumento37 páginasSymasym BBChandraRizkyAinda não há avaliações
- Prodelin 1385Documento33 páginasProdelin 1385bebebrenda100% (1)
- Nataraja Stotram - A Hymn Without 'CharaNa' and 'ShRi~NgaDocumento8 páginasNataraja Stotram - A Hymn Without 'CharaNa' and 'ShRi~NgaSiva Krishna100% (1)
- Turabian Sample PaperDocumento9 páginasTurabian Sample Paperemme_lopez908133% (3)
- Litz Wire Termination GuideDocumento5 páginasLitz Wire Termination GuideBenjamin DoverAinda não há avaliações
- Unitisation of Legal Methodsalsdkgh GHNJFKL A SDFG LKJH Asdfgf Lkjhasdfg LKKJ Asdfg LKJH A Slkjfs Aaaaaaaaaaaaslkdfj Asldkjf SLDKFJDocumento3 páginasUnitisation of Legal Methodsalsdkgh GHNJFKL A SDFG LKJH Asdfgf Lkjhasdfg LKKJ Asdfg LKJH A Slkjfs Aaaaaaaaaaaaslkdfj Asldkjf SLDKFJKailashnath Reddy AjjuguttuAinda não há avaliações
- The Daily Tar Heel For September 18, 2012Documento8 páginasThe Daily Tar Heel For September 18, 2012The Daily Tar HeelAinda não há avaliações
- L P 10Documento13 páginasL P 10Bình Minh HoàngAinda não há avaliações
- HCCM System Technical Specification v1Documento12 páginasHCCM System Technical Specification v1Ankita ChowdhuryAinda não há avaliações
- Andrew Linklater - The Transformation of Political Community - E H Carr, Critical Theory and International RelationsDocumento19 páginasAndrew Linklater - The Transformation of Political Community - E H Carr, Critical Theory and International Relationsmaria luizaAinda não há avaliações
- Active Disturbance Rejection Control For Nonlinear SystemsDocumento8 páginasActive Disturbance Rejection Control For Nonlinear SystemsTrần Việt CườngAinda não há avaliações
- Remembrance 23 Names PDFDocumento1 páginaRemembrance 23 Names PDFJennifer ThuncherAinda não há avaliações
- RA For Installation & Dismantling of Loading Platform A69Documento15 páginasRA For Installation & Dismantling of Loading Platform A69Sajid ShahAinda não há avaliações
- Project Planning and Management Unit 1Documento13 páginasProject Planning and Management Unit 1Savant100% (1)
- Samuel Vizcaino: Professional ProfileDocumento3 páginasSamuel Vizcaino: Professional ProfileVizcaíno SamuelAinda não há avaliações
- Surface water drainage infiltration testingDocumento8 páginasSurface water drainage infiltration testingRay CooperAinda não há avaliações