Escolar Documentos
Profissional Documentos
Cultura Documentos
Universal Precautions
Enviado por
Ratha VilanirashiyaDescrição original:
Direitos autorais
Formatos disponíveis
Compartilhar este documento
Compartilhar ou incorporar documento
Você considera este documento útil?
Este conteúdo é inapropriado?
Denunciar este documentoDireitos autorais:
Formatos disponíveis
Universal Precautions
Enviado por
Ratha VilanirashiyaDireitos autorais:
Formatos disponíveis
1
Universal precautions 1 2 A set of procedures and guidelines designed to both prevent the infection of the health care worker and to break chains of transmission are together referred to as the universal precautions. 3 4 Blood: 1 2 In particular these procudures are employed to prevent the transmission of blood (and other body fluid)-borne pathogens such as HIV and hepatitis B virus. However, faithful following of these procedures will interfere with the trasmission of most pathogens. 3 "Universal Precautions apply to the following body fluids: blood, semen, and vaginal, tissue, cerebrospinal, synovial (joint cavity), pleural, peritoneal, pericardial, and amniotic fluids. The CDC has stated that Universal Precautions do not apply to feces, nasal secretions, sputum, sweat, tears, urine, and vomitus, as long as these do not contain visible blood. This is not to imply that no viruses are present in these fluids but rather that the risk of transmission is either very low or unproved." (p. 439, Black, 1996) 5 Generally, one: 4 should avoid direct contact with patients, fomites, or, especially, body fluids 5 should wear barriers such as gloves when contact is necessary or expected 6 should avoid puncturing oneself with anything and therefore should minimize exposure to sharp instruments, especially body fluid-contaminated sharp instruments 7 should not expose patients to the body fluids (or substances, e.g., "weeping dermatitis") of others, such as that of health care workers Preventing nosocomial infections 6 7 Methods of prevention of nosocomial infection (and breaking the chain of transmission ) include: 8 observance of aseptic technique 9 frequent hand washing especially between patients 10 careful handling, cleaning, and disinfection of fomites 11 where possible use of single-use disposable items 12 patient isolation 13 avoidance where possible of medical procedures that can lead with high probability to nosocomial infection 14 various institutional methods such as air filtration within the hospital 15 general awareness that prevention of nosocomial infection requires constant personal surveillance 16 active oversight within the hospital
Prevention
Hospitals have sanitation protocols regarding uniforms, equipment sterilization, washing, and other preventative measures. Thorough hand washing and/or use of alcohol rubs by all medical personnel before and after each patient contact is one of the most effective ways to combat nosocomial infections.[19] More careful use of antimicrobial agents, such as antibiotics, is also considered
vital.[20] Despite sanitation protocol, patients cannot be entirely isolated from infectious agents. Furthermore, patients are often prescribed antibiotics and other antimicrobial drugs to help treat illness; this may increase the selection pressure for the emergence of resistant strains.
[edit]Isolation
Isolation precautions are designed to prevent transmission of microorganisms by common routes in hospitals. Because agent and host factors are more difficult to control, interruption of transfer of microorganisms is directed primarily at transmission.
[edit]Handwashing and gloving
Handwashing frequently is called the single most important measure to reduce the risks of transmitting skin microorganisms from one person to another or from one site to another on the same patient. Washing hands as promptly and thoroughly as possible between patient contacts and after contact with blood, body fluids, secretions, excretions, and equipment or articles contaminated by them is an important component of infection control and isolation precautions. Although handwashing may seem like a simple process, it is often performed incorrectly. Healthcare settings must continuously remind practitioners and visitors on the proper procedure in washing their hands to comply with responsible handwashing. Simple programs such as Henry the Hand, and the use of handwashing signals can assist healthcare facilities in the prevention of nosocomial infections. All visitors must follow the same procedures as hospital staff to adequately control the spread of infections. Visitors and healthcare personnel are equally to blame in transmitting infections.[citation needed] Moreover, multidrug-resistant infections can leave the hospital and become part of the community flora if steps are not taken to stop this transmission. In addition to handwashing, gloves play an important role in reducing the risks of transmission of microorganisms. Gloves are worn for three important reasons in hospitals. First, gloves are worn to provide a protective barrier and to prevent gross contamination of the hands when touching blood, body fluids, secretions, excretions, mucous membranes, and nonintact skin. In the USA, theOccupational Safety and Health Administration has mandated wearing gloves to reduce the risk of bloodborne pathogen infection.[21] Second, gloves are worn to reduce the likelihood that microorganisms present on the hands of personnel will be transmitted to patients during invasive or other patient-care procedures that involve touching a patient's mucous membranes and nonintact skin. Third, gloves are worn to reduce the likelihood that hands of personnel contaminated with microorganisms from a patient or a fomite can transmit these microorganisms to another patient. In this situation, gloves must be changed between patient contacts, and hands should be washed after gloves are removed. Wearing gloves does not replace the need for handwashing, because gloves may have small, nonapparent defects or may be torn during use, and hands can become contaminated during removal of gloves. Failure to change gloves between patient contacts is an infection control hazard.
[edit]Surface sanitation
Sanitizing surfaces is an often overlooked, yet crucial component of breaking the cycle of infection in health care environments. Modern sanitizing methods such as NAV-CO2 have been effective against gastroenteritis, MRSA, and influenza. Use of hydrogen peroxide vapor has been clinically proven to reduce infection rates and risk of acquisition. Hydrogen peroxide is effective against endospore-forming bacteria, such as Clostridium difficile, where alcohol has been shown to be ineffective.[22] A Bio-Intervention process is effective for hard surface disinfection, providing a 6-log kill (99.9999%)for many organisms including MRSA, VRE, Psudomonas aeruginosa, Staphylococcus aureus, Rhinovirus, Salmonella enterica, H1N1, HIV-1 and Hepatitis A. The unique kill mechanism is new to the market and will be an effective method against mutation and resistance of organizations.
[edit]Aprons
Wearing an apron during patient care reduces the risk of infection.[citation needed] The apron should either be disposable or be used only when caring for a specific patient.
[edit]Mitigation
The most effective technique of controlling nosocomial infection is to strategically implement QA/QC measures to the health care sectors and evidence-based management can be a feasible approach. For those VAP/HAP diseases (ventilator-associated pneumonia, hospital-acquired
pneumonia), controlling and monitoring hospital indoor air quality needs to be on agenda in management [23] whereas for nosocomial rotavirus infection, a hand hygiene protocol has to be enforced.[24][25][26] Other areas that the management needs to be covered include ambulance transport.[citation needed]
Você também pode gostar
- L A R G e - S C A L e M e T H A M P H e T A M I N e M A N U F A C T U R eDocumento21 páginasL A R G e - S C A L e M e T H A M P H e T A M I N e M A N U F A C T U R eDaria Schka100% (1)
- Manual of GardeningDocumento812 páginasManual of GardeningPrakash PatelAinda não há avaliações
- Library PDFDocumento74 páginasLibrary PDFfumiAinda não há avaliações
- Business PlanDocumento17 páginasBusiness PlanChester Cortez50% (2)
- Infection Control Policies and ProceduresDocumento9 páginasInfection Control Policies and ProceduresKelly J WilsonAinda não há avaliações
- Floret Fall Mini Course Dahlia Sources Updated 211012Documento3 páginasFloret Fall Mini Course Dahlia Sources Updated 211012Luthfian DaryonoAinda não há avaliações
- Infection Control ModuleDocumento12 páginasInfection Control ModuleFreida Michelle BonnitAinda não há avaliações
- Notes On Infection PreventionDocumento9 páginasNotes On Infection PreventionDipti PunjalAinda não há avaliações
- Fundamental Aspects of Infection Prevention and ControlNo EverandFundamental Aspects of Infection Prevention and ControlAinda não há avaliações
- Basic Concepts in Infection Prevention and Control 2023Documento44 páginasBasic Concepts in Infection Prevention and Control 2023Tannov SiregarAinda não há avaliações
- Infection Control: IntroductionDocumento17 páginasInfection Control: Introductionsuman gupta100% (1)
- Kontrol Infeksi Dalam Praktek Kedokteran GigiDocumento7 páginasKontrol Infeksi Dalam Praktek Kedokteran GigiBefalia AisarahmadaniAinda não há avaliações
- Chapter 12 Healthcare EpidemiologyDocumento10 páginasChapter 12 Healthcare EpidemiologyRegiena Tamargo100% (1)
- Rle Isolation WardDocumento6 páginasRle Isolation WardJinaan MahmudAinda não há avaliações
- Infection PreventionDocumento64 páginasInfection PreventionAnonymous Iyf0Rjmdm3Ainda não há avaliações
- 0907 UniversalDocumento6 páginas0907 UniversalRenisa HutahaeanAinda não há avaliações
- Hand Hygiene in Haemodialysis UnitsDocumento16 páginasHand Hygiene in Haemodialysis Unitsk.haynanaaAinda não há avaliações
- Am HCW Safety enDocumento2 páginasAm HCW Safety en<_>Ainda não há avaliações
- NosocomialDocumento3 páginasNosocomialHamid IqbalAinda não há avaliações
- Chapter 08Documento10 páginasChapter 08Sachin MadhukarAinda não há avaliações
- INTRODUCTIOm 2Documento7 páginasINTRODUCTIOm 2shakeebrabi326Ainda não há avaliações
- Biological Hazards ControlsDocumento4 páginasBiological Hazards ControlsAbhijeet SinghAinda não há avaliações
- Arrabaca - Prelim Journal - CPHDocumento6 páginasArrabaca - Prelim Journal - CPHREXINNE GLARIAN ARRABACAAinda não há avaliações
- Professor Panna Lal Saha BGC Trust Medical College ChittagongDocumento39 páginasProfessor Panna Lal Saha BGC Trust Medical College ChittagongPanna SahaAinda não há avaliações
- Nursing Manangement and Administration Assignment ON Standard Protocol of The UnitDocumento9 páginasNursing Manangement and Administration Assignment ON Standard Protocol of The UnitNisha MwlzAinda não há avaliações
- Isolation Precautions in Health Care Facilities - Docx Day 8Documento14 páginasIsolation Precautions in Health Care Facilities - Docx Day 8Amal ElnashartyAinda não há avaliações
- Hand WashingDocumento11 páginasHand Washinglo99988Ainda não há avaliações
- Mc3g5report Bsn1aDocumento58 páginasMc3g5report Bsn1aJhon Mhark GarinAinda não há avaliações
- Project Report On Nosocomial Infection ADocumento9 páginasProject Report On Nosocomial Infection AIdris AhmedAinda não há avaliações
- Washing Our Hands of Healthcare: Hospital-Acquired Infections and How To Avoid ThemDocumento5 páginasWashing Our Hands of Healthcare: Hospital-Acquired Infections and How To Avoid ThemEncompass HealthCare and Wound MedicineAinda não há avaliações
- Infection Prevention: A Patient Safety Imperative For The Perioperative SettingDocumento3 páginasInfection Prevention: A Patient Safety Imperative For The Perioperative SettingKryza Dale Bunado BaticanAinda não há avaliações
- LEARNING OBJECT-WPS OfficeDocumento11 páginasLEARNING OBJECT-WPS OfficeDanielle TengAinda não há avaliações
- Routine PracticesDocumento4 páginasRoutine PracticesRobins DhakalAinda não há avaliações
- Review of Related Literature: Staphylococci, Corynebacterium SPP, and Propionibacterium SPP Rarely Cause InfectionDocumento8 páginasReview of Related Literature: Staphylococci, Corynebacterium SPP, and Propionibacterium SPP Rarely Cause InfectionBincay LaurizzeAinda não há avaliações
- Group 1Documento2 páginasGroup 1Harieth NardoAinda não há avaliações
- Guide To Infection Control in The Hospital: Isolation of Communicable DiseasesDocumento17 páginasGuide To Infection Control in The Hospital: Isolation of Communicable DiseasesMatt ryioAinda não há avaliações
- Arjumand Zargar Anp@AARUSIMIDocumento69 páginasArjumand Zargar Anp@AARUSIMIArjumand ZargarAinda não há avaliações
- Healthcare and Public HealthDocumento3 páginasHealthcare and Public HealthDesiree Jeanne BLASCOAinda não há avaliações
- Hospital Associated Infections (HAI)Documento19 páginasHospital Associated Infections (HAI)Asmaa MostafaAinda não há avaliações
- Introduction To Infection Prevention and ControlDocumento8 páginasIntroduction To Infection Prevention and ControlElaine MacalandaAinda não há avaliações
- Nursing Manangement and Administration Assignment ON Standard Protocol of The UnitDocumento9 páginasNursing Manangement and Administration Assignment ON Standard Protocol of The UnitNisha MwlzAinda não há avaliações
- Evaluation of Infection Control at Butiru Chrisco Hospital in Manafwa District, Eastern UgandaDocumento13 páginasEvaluation of Infection Control at Butiru Chrisco Hospital in Manafwa District, Eastern UgandaKIU PUBLICATION AND EXTENSIONAinda não há avaliações
- Prevention of Healthcare Associated Infections - Bundled ApproachDocumento2 páginasPrevention of Healthcare Associated Infections - Bundled ApproachShivani Yoana SinglaAinda não há avaliações
- Infection Prevention - General Principles - UpToDateDocumento25 páginasInfection Prevention - General Principles - UpToDatemayteveronica1000Ainda não há avaliações
- Glove Utilization in The Prevention of Cross Transmission - A Systematic Review 2015Documento12 páginasGlove Utilization in The Prevention of Cross Transmission - A Systematic Review 2015CTAinda não há avaliações
- Infection Control: WWW - Health.gov - AuDocumento3 páginasInfection Control: WWW - Health.gov - Auwewe.trillanesAinda não há avaliações
- Biosecurity Measures in Clinical PracticeDocumento11 páginasBiosecurity Measures in Clinical PracticeAlmendra Montes De OcaAinda não há avaliações
- Chapter Five Summary of Findings, Conclusion and RecommendationsDocumento5 páginasChapter Five Summary of Findings, Conclusion and RecommendationsKojo AduAinda não há avaliações
- Guidelines On Infection Control in Dental ClinicsDocumento10 páginasGuidelines On Infection Control in Dental ClinicsHare RamAinda não há avaliações
- Hand Hygiene Study - PITTET !!! 1-s2.0-S0195670109001868-MainDocumento11 páginasHand Hygiene Study - PITTET !!! 1-s2.0-S0195670109001868-MainAgil DaruAinda não há avaliações
- Infectious Disease Control in The WorkplaceDocumento8 páginasInfectious Disease Control in The WorkplaceMaga42Ainda não há avaliações
- MICROBIOLOGYDocumento9 páginasMICROBIOLOGYAmr Ramazan IbrahimAinda não há avaliações
- Needle Stick InjuryDocumento6 páginasNeedle Stick InjuryNikitaAinda não há avaliações
- Chapter Two Literature ReviewDocumento11 páginasChapter Two Literature ReviewKojo Adu100% (1)
- Infection ControlDocumento14 páginasInfection ControlShiba AbdullahAinda não há avaliações
- Ssi Protocol 2015Documento11 páginasSsi Protocol 2015Megersa AleneAinda não há avaliações
- Dental Clinics DesinfeccionDocumento23 páginasDental Clinics DesinfeccionOrtodoncia UNAL 2020Ainda não há avaliações
- Microbio (6114)Documento2 páginasMicrobio (6114)PRINCESS JULIENNE YUAinda não há avaliações
- Ams Ipc SlidesDocumento36 páginasAms Ipc SlidesHarriet TembaAinda não há avaliações
- Assessment of Infection Control Measures and Risk Factors at Kampala International University Teaching Hospital in Bushenyi District A Study On Staff Awareness and ImplementationDocumento15 páginasAssessment of Infection Control Measures and Risk Factors at Kampala International University Teaching Hospital in Bushenyi District A Study On Staff Awareness and ImplementationKIU PUBLICATION AND EXTENSIONAinda não há avaliações
- Document Ambulance - Guidelines Reducing Infection in Prehospital FINAL 271Documento10 páginasDocument Ambulance - Guidelines Reducing Infection in Prehospital FINAL 271Agustinus BethaAinda não há avaliações
- Infection ControlDocumento23 páginasInfection ControlAnne TjanAinda não há avaliações
- Infection Control in the Dental Office: A Global PerspectiveNo EverandInfection Control in the Dental Office: A Global PerspectiveLouis G. DePaolaAinda não há avaliações
- BCA2006 BCA GuideDocumento507 páginasBCA2006 BCA GuidePatrick LiaoAinda não há avaliações
- Universal ING - LA.Boschi Plants Private LimitedDocumento23 páginasUniversal ING - LA.Boschi Plants Private LimitedAlvaro Mendoza MaytaAinda não há avaliações
- Mdp36 The EndDocumento42 páginasMdp36 The Endnanog36Ainda não há avaliações
- Drawing Submssion Requirements - September - 2018Documento66 páginasDrawing Submssion Requirements - September - 2018Suratman Blanck MandhoAinda não há avaliações
- My Public Self My Hidden Self My Blind Spots My Unknown SelfDocumento2 páginasMy Public Self My Hidden Self My Blind Spots My Unknown SelfMaria Hosanna PalorAinda não há avaliações
- FSSC 22000 V6 Guidance Document Environmental MonitoringDocumento10 páginasFSSC 22000 V6 Guidance Document Environmental Monitoringjessica.ramirezAinda não há avaliações
- PV2R Series Single PumpDocumento14 páginasPV2R Series Single PumpBagus setiawanAinda não há avaliações
- RMP ContractDocumento181 páginasRMP ContractHillary AmistosoAinda não há avaliações
- Total Elbow Arthroplasty and RehabilitationDocumento5 páginasTotal Elbow Arthroplasty and RehabilitationMarina EAinda não há avaliações
- Datasheet MEC MPS200 v1 2018Documento4 páginasDatasheet MEC MPS200 v1 2018Cepi Sindang KamulanAinda não há avaliações
- Beckhoff Service Tool - USB StickDocumento7 páginasBeckhoff Service Tool - USB StickGustavo VélizAinda não há avaliações
- Cyber Safety PP Presentation For Class 11Documento16 páginasCyber Safety PP Presentation For Class 11WAZ CHANNEL100% (1)
- Online Games and Academic AchievementDocumento25 páginasOnline Games and Academic AchievementJasmine GamoraAinda não há avaliações
- Free Higher Education Application Form 1st Semester, SY 2021-2022Documento1 páginaFree Higher Education Application Form 1st Semester, SY 2021-2022Wheng NaragAinda não há avaliações
- L04-課文單片填空 (題目) (Day of the Dead)Documento3 páginasL04-課文單片填空 (題目) (Day of the Dead)1020239korrnellAinda não há avaliações
- 2-Product Spec PDFDocumento10 páginas2-Product Spec PDFMhooMOoChaappHteenAinda não há avaliações
- Boeco BM-800 - User ManualDocumento21 páginasBoeco BM-800 - User ManualJuan Carlos CrespoAinda não há avaliações
- MAOH600 Ropu 48 Presentation Script and ReferencesDocumento10 páginasMAOH600 Ropu 48 Presentation Script and ReferencesFano AsiataAinda não há avaliações
- Dissertation On: To Asses The Impact of Organizational Retention Strategies On Employee Turnover: A Case of TescoDocumento44 páginasDissertation On: To Asses The Impact of Organizational Retention Strategies On Employee Turnover: A Case of TescoAhnafTahmidAinda não há avaliações
- Geography - Development (Rural - Urban Settlement)Documento32 páginasGeography - Development (Rural - Urban Settlement)jasmine le rouxAinda não há avaliações
- 21A Solenoid Valves Series DatasheetDocumento40 páginas21A Solenoid Valves Series Datasheetportusan2000Ainda não há avaliações
- Probni Test 1. Godina - Ina KlipaDocumento4 páginasProbni Test 1. Godina - Ina KlipaMickoAinda não há avaliações
- E10b MERCHANT NAVY CODE OF CONDUCTDocumento1 páginaE10b MERCHANT NAVY CODE OF CONDUCTssabih75Ainda não há avaliações
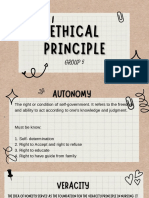
- Group 5 - Ethical PrinciplesDocumento11 páginasGroup 5 - Ethical Principlesvirgo paigeAinda não há avaliações