Escolar Documentos
Profissional Documentos
Cultura Documentos
Celiac Neurological Manifestations Pike 2011
Enviado por
service109443Descrição original:
Direitos autorais
Formatos disponíveis
Compartilhar este documento
Compartilhar ou incorporar documento
Você considera este documento útil?
Este conteúdo é inapropriado?
Denunciar este documentoDireitos autorais:
Formatos disponíveis
Celiac Neurological Manifestations Pike 2011
Enviado por
service109443Direitos autorais:
Formatos disponíveis
Neurological manifestations of celiac
Running head: NEUROLOGICAL MANIFESTATIONS OF CELIAC
Neurological and Psychiatric Manifestations of Celiac Disease and Gluten Sensitivity Christina M. Pike University of Washington
Neurological manifestations celiac 2 Psychiatric/Neurological Manifestations of Celiac Disease/Gluten Sensitivity Celiac disease/gluten sensitivity has long been considered a disease of the gut. Current research and theory suggests it may be more likely to manifest as a neurological/psychiatric disorder in its early disease stages. Although a full understanding of the pathophysiology has yet to be discovered, there is ample evidence to associate celiac/gluten sensitivity to certain neurological/psychiatric conditions. These include but are not limited to ataxia, neuropathy, migraines, schizophrenia, depression, attention deficit, and autism spectrum. People suffering from these conditions often initially present to primary care or psychiatric providers. Therefore, primary care practitioners and psychiatric providers should have a basic understanding of celiac/gluten sensitivity to assist with early detection and diagnosis.
Neurological manifestations of celiac
Celiac disease is an autoimmune disorder completely dependent on the ingestion of the gluten protein, gliadin, found in wheat, rye, and barley. Gluten sensitivity is considered to be the beginning stages of celiac but also may exist as a separate disorder (Sapone et al. 2011). Physicians are trained to spot only a small subset of symptoms, including malabsorption, diarrhea, wasting and failure to thrive. These are considered to be classic signs of celiac along with damage to the villi of the small intestine. Gluten sensitivity rarely manifests in this fashion, making diagnosis more challenging. It is suggested that, only one-third of patients will present with diarrhea (Rampertab et al. 2006) and 53% will have a BMI in the overweight or obese category (Dickey and Kearney 2006). Over the past 15 years the understanding of celiac and gluten sensitivity has improved significantly. Once believed to be a disorder of the gut, celiac/gluten sensitivity is now understood to be much more complex and continues to be a diagnostic challenge. Some common presentations include liver and biliary tract disorders, recurrent miscarriages, dental enamel defects, recurrent sinus infections, anemia, migraines, peripheral neuropathy, and several psychiatric disorders. Also, it is quite common for celiac to co-occur with many other autoimmune disorders (Collin et al. 2002). This makes it almost impossible to diagnose celiac/gluten sensitivity in the typical 15-minute practitioner visit. Celiac disease is reported to affect roughly 1% of the population (Sanders et al. 2003, West et al. 2003). When combined with gluten sensitivity and wheat allergy the numbers are suggested to be as high as 10% (Sapone et al. 2011, Catassi and Fasano
Neurological manifestations celiac 4 2008, Anderson et al. 2007). The mean age of diagnosis ranges from 40 to 50 and the average number of years from first presenting in primary care to diagnosis is 4.6 years (Rampertab et al. 2006). Because of the myriad of symptoms and possible co-occurring disorders, out of 3 million people suspected of having the disease, only 100,000 are correctly diagnosed (Ravikumara, Nootigattu and Sandhu 2007). Undiagnosed celiac complications include osteoporosis, malignancies, and secondary autoimmune disease. When a gluten free diet is implemented there is clinical improvement in the gut mucosa and a decreased mortality (Corrao et al. 2001, Murray et al. 2004). Understanding that untreated celiac/gluten sensitivity puts the patient at risk for other autoimmune disease and dangerous complications makes it important for practitioners to have a better understanding of the early signs of celiac/gluten sensitivity. This review will focus on the neurological/psychiatric manifestations of celiac/gluten sensitivity and the proposed theoretical connection as well as appraise the current diagnostic tools available. The connection Research in the field of celiac disease has grown in exponentially over the last few years. As the pathophysiology behind this disease becomes better understood the comprehension of its complexity also grows. Acceptance of the idea of celiac as a multifactorial disease, which manifests in a multitude of ways, allows for a deeper understanding of the current proposed theories. Gliadin, the offending protein in gluten, causes an initial insult at the intracellular tight junctions located on the luminal side of the intestine. These tight junctions are
Neurological manifestations of celiac
responsible for maintaining the integrity of the intestinal wall and keeping out macromolecules. Gliadin binds with CXCR3, a chemokine receptor responsible for leukocyte recruitment and eventually involvement of T-helper cells. Lammers and colleagues (2008) reported a higher concentration of CXCR3 in the gut epithelium of those with celiac disease as compared to those without. CXCR3 recruits myD88, an adaptor protein, allowing the release of zonulin to the apical side of the epithelium (Lammers et al. 2008, Clemente et al. 2003). Zonulin, in celiac, is responsible for the changes in cellular structure and arrangement of the cytoskeleton which allows for increased gut permeability. Interestingly, in non-celiac intestinal epithelium, zonulin strengthens the tight junctions (Drago et al. 2006). While both celiac and non-celiac tissue reacted to gliadin, only the celiac epithelial membrane up-regulated the production of the mRNA for CXCR3 gene expression at a 9.6 fold increase. When gliadin was removed, the expression of the CXCR3 in the tissues of celiac patients decreased to what was seen in those without celiac disease (Lammers et al. 2008). It is important to note that CXCR3 is expressed in several other cells including natural killer cells, and CD3+/CD8+ T cells which could account for the instigation of the innate immune response associated with celiac disease. In addition, toll like receptors, which are also responsible for innate immune response, have been reported to be increased in the duodenum of children with celiac as compared to healthy controls (Szebeni et al. 2007). In gluten sensitivity it is suggested that adaptive suppressor T cells may help to stop the toll like receptor process before damage is done to the intestinal villi (Sapone et al. 2011).
Neurological manifestations celiac 6 Tight junctions in the epithelial wall are critical for maintaining the integrity of the gut. The increased permeability seen in celiac disease appears to be associated with the onset of other autoimmune disorders (Drago et al. 2006, Sapone et al. 2006, and Watts et al. 2005). Initially celiac symptoms were thought to be a result of the gut reacting to the whole gliadin molecule. We now understand that there are several areas within the gliadin chain and each sets off very diverse reactions depending on the HLADQ (HLA-DQ2/DQ8 are most commonly seen in celiac) variant and its peptide-binding properties (Vader et al. 2002). Without the proper functioning of the tight junction, peptides up to three amino acids long are allowed to enter circulation (Lammers et al. 2008). Innate Immune Response to Acquired Immune Response Once allowed access, roaming gliadin peptides cause stimulation of the innate and acquired immune system. In the innate response, a portion of the offending peptide stimulates peripheral CD4+ T cells, which activates apoptosis of the epithelial tissue, initiates macrophages, and IL-15(Londei et al. 2005, Maiuri et al. 2003). In acquired immunity, tissue-transglutaminase (TG2 or tTG), which is normally responsible for intermolecular bonding, apoptosis, and reinforcement of the cell matrix, deamidates gliadin. This process creates a positively charged molecule and increases the affinity of binding to the HLA-DQ2 DQ-8. Once bound there is a cyclical and progressive reaction. The HLA DQ2/8 positive individuals can present the gliadin molecule on their antigen presenting cells and relay the message to the CD4+ T-cells. The CD4 cells then
Neurological manifestations of celiac
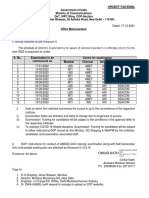
releases INF, an immunostimulator, which boosts HLA production. With continued insult and tissue inflammation, TG2 is produced to help reconstruct the damaged areas of the epithelium. More TG2 increases the rate of deamediation, which stimulates a greater CD4 response, and so on. It is important to note the presence of TG2 is generally in the gut, TG3 is associated with the skin and TG6 is primarily found in the brain. In patients with neurological disorders in combination with celiac, anti-TG6 has been reported to be produced intrathecally (Schrdl et al. 2004). The disease process related to celiac/gluten sensitivity is complex and vast. Science has come a long way in researching this disease but much remains to be learned. Fortunately, what we do know may help us understand how immune process of celiac is related to neurological/psychiatric disorders and why their prevalence is up to 10-25% times higher in this disease (Hadjivassiliou et al. 1996). Diagnosis The first step in diagnosis is to test the patient for antibodies related to the autoimmune reaction when gluten is ingested. Initially tTG (TG2), IgA-AGA, IgG-AGA, and total IgA should be ordered (See Table 1: Diagnostic Tests). If any tests are above the normal limit, the patient should be forwarded to a gastrointestinal specialist for an upper endoscopy (EGD). If total IgA is below normal range there could be an IgA deficiency, rendering all IgA type testing unreliable. If this is the case or all tests are within normal limits, halotype testing can be done to rule out celiac but not gluten sensitivity. Having HLA DQ8, DQ2, or DQ1 is not indicative of celiac but may help with differential diagnosis (Hadjivassiliou et al. 2010).
Neurological manifestations celiac 8 During the EGD, samples of the small bowel are taken and then analyzed for injury to the villi of the small intestine. If the histological results are Marsh Grade 0 with normal villous architecture it would be prudent to request IgA tTG tests be performed on the tissue sample. This test can catch celiac disease before mucosal damage is done. Unfortunately, these tests are not widely available. Marsh grade 1 changes consist of some lymphocytic infiltration of the mucosa which is considered to be predictive of celiac if there are more than 20 enterocytes per 100 villi. Marsh Grade 2 shows lymphocytic infiltration as well as crypt hyperplasia and is considered to be pre-celiac or celiac depending on amount of damage. Marsh grade 3 shows lymphocytic infiltration, crypt hyperplasia and villous blunting to total villous atrophy. Marsh grade 3 is considered full blown celiac (Oberhuber et al. 1999, Sapone et al. 2011). It is important to note that the patient must be consuming gluten for valid testing. If gluten has already been removed from the diet a gluten challenge may be necessary for diagnosis. This consists of consuming the equivalent of 4 or more slices of bread per day for at least six weeks. If the patient has already had positive results from a gluten free diet, this reintroduction may not be ideal. Even if gluten has not yet been removed from the diet some people choose not to undergo the biopsy procedure because of the associated risks. It is now understood and becoming increasingly accepted that gluten sensitivity can exist without histological changes, making the endoscopy somewhat unreliable but still considered the gold star diagnosis. Hadjivassiliou et al. 2006a, b, reported
neurological dysfunction related to gluten sensitivity with and without histological
Neurological manifestations of celiac changes in the mucosa.
As evidence of this phenomenon is accumulating, many
practitioners are beginning to rely less on the biopsy and more on blood tests and trial of the gluten free diet. Understanding the complexities of celiac helps the practitioner to think outside of the box when formulating a diagnosis. Celiac/gluten sensitivity should be thought of as a multitude of different diseases brought on by the ingestion of gluten, manifesting in distinct ways, all requiring the same treatment, a gluten free diet.
Diagnostic Tests Tests tTG-IgA (TG2) IgA-AGA CD/GS CD Sensitivity 95% Specificity 90% Notes
If positive it is villous atrophy highly likely but a negative does not rule out CD or GS Can positive with extra-intestinal symptoms, a negative does not rule out CD/GS Can positive with extra-intestinal symptoms, a negative does not rule out CD/GS False positive in Crones, wheat protein allergy, and with recent diarrhea Shows CD before intestinal damage occurs
GS
53-100%
65-100%
IgG-AGA
GS
57-100%
42-100%
Antideaminated gliadin-IgA/IgG
CD CD/GS GS
90&92%
Respectively
98&75%
Respectively
Total IgA TG6
No Data No Data
No Data No Data
IgA deficiency can cause all AGA tests to show false negative Associated with neurological symptoms Not readily available yet
Neurological manifestations celiac 10 Tests Genetic HLA-DQ8 HLA-DQ2 HLA-DQ1
Biopsy results
CD/GS CD/GS CD/GS CD/GS GS
Increased intraepithelial lymphocytes
Sensitivity % in CD 95% 5% 0
Crypt Hyperplasia
Specificity % in GS 50% 9% 1%
Villous Atrophy
Notes Notes
30% of the general population will have this halotype, Helps with inconclusive serology Helps with inconclusive serology Helps with inconclusive serology
Notes
Marsh Grade I Marsh II Marsh Grade III
Present
Not present Present
Not Present Not Present / Partial Total
Found in pre-celiac and GS
Present
Pre-Celiac/CD
Present
Present
Celiac Disease
Table 1: Diagnostic Tests
Neurological Presentation Ataxia Ataxia is one of the most predominant neurological presentations of gluten sensitivity. In 1996, Hadjivassiliou et al. coined the term gluten ataxia to represent sporadic ataxia found in combination with celiac markers. The research included 500 patients over a 13 year time span. Of the 500 patients, 215 had idiopathic sporadic ataxia and 101 of those patients had serological evidence of gluten sensitivity. In 2008, Hadjivassiliou examined 400 patients presenting with ataxia. Of the 400, 91 had
Neurological manifestations of celiac
idiopathic sporadic ataxia. When the two groups were compared, the autoimmune prevalence in the genetic ataxia group was reported to be 6%, while the idiopathic sporadic ataxia group was 47%. Anti-cerebellar antibodies were also found in 60% of the idiopathic ataxia group and 5% of those with genetic ataxia. HLA DQ2, commonly associated with autoimmune disease, was found in 71% of the sporadic ataxia, 34% in genetic, 36% in the general population (Hadjivassiliou et al. 2008b). While an exact understanding of the disease process is unknown, there are some clues to suggest a gluten related inflammatory process. Researchers took serum from patients with gluten ataxia and analyzed the effect on brain tissue samples. The serum was found to have antibodies directed toward neuronal Purkinje cells, cortical neurons and the brain stem (Hadjivassiliou et al. 2002, Boscolo et al. 2007). In the mouse model, serum from celiac subjects with and without ataxia caused transient ataxia (Boscolo et al. 2007). Post-mortum autopsy preformed on patients suffeing from gluten ataxia showed damage to the cerebellum from lymphocytic infiltration, some damage to the periphrial nerves and posterior spinal column (Cooke and Smith 1966, Hadjivassiliou et al. 1998). In addition, parivascular cuffing and anti-TG6 has been reported in the brains of patients with gluten ataxia, an indication of an immune response (Hadjivassiliou et al. 2008a). The immune process involved in gluten ataxia is progressive in the presence of gliadin. Therfore, prompt diagnosis and treatment with gluten free diet is essential. Symptoms should be expected to remiss depending on the amount of damage done to the Purkinje cells and continuation of gluten free diet (Hadjivassiliou et al. 2003). It is
Neurological manifestations celiac 12 essential that there is strict adhearance to the diet as reaction to gliadin can occur with as little as 20ppm exposure. Serum testing is a good indication of adherence but it is important to note that antibodies will continue to circulate for 6-12 months after gluten is removed.
Neuropathy Neuropathy is the second most common neurological disorder associated with gluten sensitivity. The connection has been coined gluten neuropathy and encompasses a combination of serological evidence of gluten sensitivity and sporadic idiopathic neuropathy with no alternative cause. There are several different neuropathies correlated with celiac including sensory ganglionopathy, asymmetrical neuropathy, and small fiber neuropathy but the most prevalent is peripheral neuropathy (Hadjivassiliou et al. 2010, Kelkar, Ross and Murray 1996, Chin et al. 2006). In a Swedish general population study, 84,000 people with celiac were identified. Of those there was a 3-4 fold increase of polyneuropathy when compared to the general public (Ludvigsson et al. 2007). In 2006, Hadjivassiliou and team reported 34% of 140 people who had idiopathic sporadic neuropathy also had significant level of IgG or IgA antibodies (Hadjivassiliou et al. 2006a). Chin et al. report the prevalence of biopsy proven celiac with neuropathy to be 2.5-8% as compared to the suggested 1% of the healthy population. This data was gathered from a retrospective study of 400 people presenting with neuropathy and does not include those who have gluten sensitivity without intestinal damage (Chin et al. 2003).
Neurological manifestations of celiac
Unfortunately, to date, neuropathological evidence is limited to a few case studies but the findings are similar and consistent with an inflammatory process. In the 2006 Hadjivassiliou study, cited previously, 2 sural-nerve biopsies and one autopsy were examined. The first endoneurial biopsy showed signs of inflammatory
degenerative process with axonal damage. The second biopsy also showed nerve damage but lacked the inflammatory cells. The samples provided evidence of decreased Purkinje cells, slight decrease of neurons in the olivary nucleus and perivascular cuffing from lymphocytic infiltration (Hadjivassiliou et al. 2006a). For most people with gluten neuropathy, a gluten free diet will improve symptoms. In a study consisting of 35 patients with gluten neuropathy, 25 were placed on a gluten free diet while 10 refused treatment. There was a statistically significant improvement in the treatment group and a progressive decline in the non-treatment. Also, there was a correlation between disease progression and improvement. Those who displayed symptoms for a longer period of pre-diet time and those with more severe neuropathy experienced the least amount of improvement (Hadjivassiliou et al. 2006b).
Migraines/Headache There is a growing body of evidence suggesting the association of migraines to gluten sensitivity/celiac. In a retrospective study composed of 357 children with celiac disease, 88 reported headaches before diagnosis. After implementation of a gluten free diet the kids were asked about the quantity and quality of their headaches. Of the 88,
Neurological manifestations celiac 14 24.7% had full resolution, 50% improved, 24.9 had no change. Incidentally, 47.6 of the no change were noncompliant with diet based on self-report. In the prospective part of the same study, 79 children who presented with headache were tested for celiac. Four patients were positive according to their biopsy results (5% of study population, compared to 1% of general population). Three had total regression of headaches after diet, 1 had marked improvement. None of the 79 subjects had classic signs (Lionetti et al. 2009). In a smaller study of 10 patients with episodic headache and IgG and/or IgA positive, 7 of 10 had full remission, 2 had partial recovery and 1 refused diet. All had wide range of white matter abnormalities (Hadjivassiliou et al. 2001). Similar results suggest that in 4.4-5.5% of people who present with headaches, gluten may be the trigger. In addition, the removal of gluten can decrease or ameliorated headache symptoms (Gabrielli et al. 2003). Although a complete understanding of the headache/celiac correlation is unknown, there is evidence suggesting problems with regional cerebral blood flow and cortical hypoperfusion. In several studies symptoms improved with a gluten free diet (Addolorato et al. 2004, Leggio et al. 2004, Abenavoli, Gasbarrini and Addolorato 2008). Addolorato et al. (2004) reported brain hypoperfusion in 73% of untreated celiac patients who had no neurological symptoms. Interestingly, the treated celiac patients had a slightly lower percentage of hypoperfusion than healthy controls. These reported brain abnormalities suggest an inflammatory process where a gluten free diet may be beneficial and non-treatment may be detrimental.
Neurological manifestations of celiac Schizophrenia
The connection between schizophrenia and celiac/gluten sensitivity has been controversial since it was first suggested in 1966. However, within the last few years researchers have made significant leaps in understanding the complexity of the, now accepted, association. In 1966 Dr. Curtis Dohan, a psychiatrist for the VA, reported a decrease in schizophrenia admissions during the WWII grain shortage (Dohan 1966). Shortly after his initial findings, another study was conducted using patients on a locked VA ward. Patients were assigned either a high grain and milk diet or a grain/milk free diet. Improvement was measured by the number of days before the patient was allowed full ward privileges. Over 175 day, 62% of the grain/milk free diet patients were allowed full privileges compared to 36% who were on the high grain/milk diet. Furthermore, when grains were added back to the diet almost 75% of the grain/milk free patients decompensated and were returned to the locked ward (Dohan et al. 1969). In 1997, a 33 year old presented with persistent diarrhea and a previous diagnosis of schizophrenia. Single proton emission computed tomography (SPECT) analysis was preformed and she was found to have hypoperfusion of the left frontal cortex. She was put on a gluten free diet and the follow up SPECT showed normalization of flow and regression of psychiatric symptoms (De Santis et al. 1997). This was the first study to show perfusion abnormalities in celiac. It is estimated that celiac and schizophrenia separately affects 1% of the population. Yet, according to a Danish National Registry study, people with celiac are at
Neurological manifestations celiac 16 a 3.2% increased risk for developing schizophrenia (Eaton et al. 2006). Other population studies from the UK report conflicting results and suggest there is no connection between schizophrenia and celiac (Wei and Hemmings 2005, West et al. 2006). It is important to note that these two studies only looked for classic celiac disease and limited their serological evidence to anti-EMA and anti-tTG. If anti-gliadin antibodies were included, there may be a more accurate picture. Several more recent studies found moderate to high anti-gliadin antibodies in patients with schizophrenia. Cascella (2011) used AGA, tTG, and EMA to assess 900 serum samples from the Clinical Antipsychotic Trials of Intervention Effectiveness (CATIE). They reported 23.1% of serum was positive for AGA compared to 3.1 of the control population. tTG, was elevated in 5.4% of the CATIE population and 0.08% of the controls. There was no difference in the percentage positive for EMA (Cascella et al. 2011, Dickerson et al. 2010, Samaroo et al. 2010). A smaller, yet similar, study of 129 patients with recent onset psychosis yielded similar results of increased IgA and IgG (Dickerson et al. 2010). In 2010 researchers took serum from schizophrenia patients who also had high anti-gliadin antibodies. They describe a very specific set of gluten peptide chains caused an anti-gliadin reaction in this set of subjects. Interestingly, the offending peptide is not the same set that causes a reaction in classic celiac disease. The team suggests schizophrenia with gluten sensitivity is completely different disease than classic celiac (Samaroo et al. 2010).
Other Psychiatric Disorders
Neurological manifestations of celiac
Increased risk of depression has been reported in both the pre and post diagnosis of celiac (Huser et al. 2010, Addolorato et al. 2004). Although there is a limited amount of available research and few case studies, several theories have emerged. According to Hallert et al., (2009) loss of intestinal villi decreases nutrient absorption causing a reduction in vitamin and mineral assimilation. The argument is supported by a reduction of depressive symptoms and an increase in total homocyctine levels in patients with celiac disease given supplemental B vitamins for 6 months. A small, 30-person study reported a decrease in sleep quality for pre and post diagnosis celiac patients, which could contribute to depressive symptoms (Zingone et al. 2010). Pynnonen et al. (2005) discovered pre-diet, low tryptophan levels, in celiac patients with depressed/anxious and aggressive behavior. After 3 months following a gluten free diet there was an increase in tryptophan levels and a significant decrease in psychiatric symptoms (Pynnnen et al. 2005). In addition, increased anti-gliadin antibodies were more common in depressed elderly patients without celiac, than in healthy subjects. This suggests gluten sensitivity may also play a role in depressive symptoms (Ruuskanen et al. 2010). Research assessing the effect of a gluten free diet on ADHD symptoms reported a significant improvement in daily functioning and behavioral issues. In addition, 74% of patients expressed a desire to continue with the diet, due to a noticeable increase in concentration and decrease in distractibility (Niederhofer and Pittschieler 2006). Others have described a reduction in behavioral issues with a gluten free diet but the studies were much smaller (Pynnnen et al. 2005). Regardless of the outcome of the gluten
Neurological manifestations celiac 18 free diet on symptoms there appears to be an increased risk of having celiac if ADHD is present (Niederhofer and Pittschieler 2006, Young 2008). In autism spectrum disorder (ASD), a gluten free diet continues to be surrounded by conflicting evidence. A small study found no relationship between ASD and celiac (Pavalone et al. 1997). This is in contrast to a larger study, done in 2008, which reported celiac to have a prevalence of 3.3% in pervasive developmental disorders. While evidence is mounting towards a connection between ASD and prevalence in celiac, it is unclear if a gluten free diet would alleviate symptoms (Hill et al. 2004). That being said, there is an association of a gluten free diet to regression of autistic symptoms being reported (Genuis and Bouchard 2010). Furthermore, the recent focus of the immunology component of ASD, allows for a new understanding of the probable association. A few reports indicate an immune reaction in the gut of a subset of ASD patients. These patients showed increased lymphocytic infiltration of the villi with mild to moderate damage (Ashwood et al. 2003, Ashwood et al. 2004). Vojdani and colleagues, found an increased anti-gliadin antibody as well as autoantibody reactions in cerebellar peptides related to gluten using sera from ASD patient (Vojdani et al. 2004a, Vojdani et al. 2004b). This suggests an immune mediated association between the ingestion of gluten and symptoms of ASD.
Conclusion While celiac disease and gluten sensitivity are complex disorders they have a simple cure. The person afflicted must stop eating gluten. Diseases like ataxia,
Neurological manifestations of celiac
neuropathy, and migraines are often of unknown origin and treatment is focused on minimizing the severity of symptoms. If gluten sensitivity or celiac is the etiology of these symptoms, for even a small subset of patients, it is imperative to test each patient. Schizophrenia is a severe and debilitating mental disorder that affects approximately 24 million people worldwide. The cost to society is approximately 65 million dollars a year and in the United States, it is the 2 nd leading cause of disability. The person afflicted with schizophrenia has a decrease in life expectancy and an increased probability of homelessness and/or prison time. If even the most modest numbers of celiac disease presenting as schizophrenia are accurate, we owe it to our patients to make screening a priority. This is equally true for depression, ADHD and autism. While these diseases might not have the same impact as schizophrenia, they are costly and have a huge influence on a persons quality of life. The connection between autoimmune disorders like celiac and a systemic inflammatory process is gaining increasingly convincing evidence. Celiac/gluten sensitivity therefore, should not be considered a disease of the gut but a neurological disorder. While it may begin in the gut, damage is certainly not limited to that area. Understanding the pathophysiology, tests, and extra-intestinal manifestations of celiac will assist in diagnosis and management of these complex diseases.
Neurological manifestations celiac 20 Abenavoli, L., G. Gasbarrini & G. Addolorato (2008) Subclinical neurological abnormalities in patients with celiac disease: are they associated by brain hypoperfusion? J Pediatr Gastroenterol Nutr, 46, 470. Addolorato, G., D. Di Giuda, G. De Rossi, V. Valenza, M. Domenicali, F. Caputo, A. Gasbarrini, E. Capristo & G. Gasbarrini (2004) Regional cerebral hypoperfusion in patients with celiac disease. Am J Med, 116, 312-7. Anderson, L. A., S. A. McMillan, R. G. Watson, P. Monaghan, A. T. Gavin, C. Fox & L. J. Murray (2007) Malignancy and mortality in a population-based cohort of patients with coeliac disease or "gluten sensitivity". World J Gastroenterol, 13, 146-51. Ashwood, P., A. Anthony, A. A. Pellicer, F. Torrente, J. A. Walker-Smith & A. J. Wakefield (2003) Intestinal lymphocyte populations in children with regressive autism: evidence for extensive mucosal immunopathology. J Clin Immunol, 23, 504-17. Ashwood, P., A. Anthony, F. Torrente & A. J. Wakefield (2004) Spontaneous mucosal lymphocyte cytokine profiles in children with autism and gastrointestinal symptoms: mucosal immune activation and reduced counter regulatory interleukin-10. J Clin Immunol, 24, 664-73. Boscolo, S., A. Sarich, A. Lorenzon, M. Passoni, V. Rui, M. Stebel, D. Sblattero, R. Marzari, M. Hadjivassiliou & E. Tongiorgi (2007) Gluten ataxia: passive transfer in a mouse model. Ann N Y Acad Sci, 1107, 319-28. Cascella, N. G., D. Kryszak, B. Bhatti, P. Gregory, D. L. Kelly, J. P. Mc Evoy, A. Fasano & W. W. Eaton (2011) Prevalence of celiac disease and gluten sensitivity in the United States clinical antipsychotic trials of intervention effectiveness study population. Schizophr Bull, 37, 94-100. Catassi, C. & A. Fasano (2008) Celiac disease. Curr Opin Gastroenterol, 24, 687-91. Chin, R. L., H. W. Sander, T. H. Brannagan, P. H. Green, A. P. Hays, A. Alaedini & N. Latov (2003) Celiac neuropathy. Neurology, 60, 1581-5. Chin, R. L., V. G. Tseng, P. H. Green, H. W. Sander, T. H. Brannagan & N. Latov (2006) Multifocal axonal polyneuropathy in celiac disease. Neurology, 66, 19235. Clemente, M. G., S. De Virgiliis, J. S. Kang, R. Macatagney, M. P. Musu, M. R. Di Pierro, S. Drago, M. Congia & A. Fasano (2003) Early effects of gliadin on enterocyte intracellular signalling involved in intestinal barrier function. Gut, 52, 218-23. Collin, P., K. Kaukinen, M. Vlimki & J. Salmi (2002) Endocrinological disorders and celiac disease. Endocr Rev, 23, 464-83. Cooke, W. T. & W. T. Smith (1966) Neurological disorders associated with adult coeliac disease. Brain, 89, 683-722. Corrao, G., G. R. Corazza, V. Bagnardi, G. Brusco, C. Ciacci, M. Cottone, C. Sategna Guidetti, P. Usai, P. Cesari, M. A. Pelli, S. Loperfido, U. Volta, A. Calabr, M.
Neurological manifestations of celiac
Certo & C. d. T. S. Group (2001) Mortality in patients with coeliac disease and their relatives: a cohort study. Lancet, 358, 356-61. De Santis, A., G. Addolorato, A. Romito, S. Caputo, A. Giordano, G. Gambassi, C. Taranto, R. Manna & G. Gasbarrini (1997) Schizophrenic symptoms and SPECT abnormalities in a coeliac patient: regression after a gluten-free diet. J Intern Med, 242, 421-3. Dickerson, F., C. Stallings, A. Origoni, C. Vaughan, S. Khushalani, F. Leister, S. Yang, B. Krivogorsky, A. Alaedini & R. Yolken (2010) Markers of gluten sensitivity and celiac disease in recent-onset psychosis and multi-episode schizophrenia. Biol Psychiatry, 68, 100-4. Dickey, W. & N. Kearney (2006) Overweight in celiac disease: prevalence, clinical characteristics, and effect of a gluten-free diet. Am J Gastroenterol, 101, 2356-9. Dohan, F. C. (1966) Wheat "consumption" and hospital admissions for schizophrenia during World War II. A preliminary report. Am J Clin Nutr, 18, 7-10. Dohan, F. C., J. C. Grasberger, F. M. Lowell, H. T. Johnston & A. W. Arbegast (1969) Relapsed schizophrenics: more rapid improvement on a milk- and cereal-free diet. Br J Psychiatry, 115, 595-6. Drago, S., R. El Asmar, M. Di Pierro, M. Grazia Clemente, A. Tripathi, A. Sapone, M. Thakar, G. Iacono, A. Carroccio, C. D'Agate, T. Not, L. Zampini, C. Catassi & A. Fasano (2006) Gliadin, zonulin and gut permeability: Effects on celiac and nonceliac intestinal mucosa and intestinal cell lines. Scand J Gastroenterol, 41, 40819. Eaton, W. W., M. Byrne, H. Ewald, O. Mors, C. Y. Chen, E. Agerbo & P. B. Mortensen (2006) Association of schizophrenia and autoimmune diseases: linkage of Danish national registers. Am J Psychiatry, 163, 521-8. Gabrielli, M., F. Cremonini, G. Fiore, G. Addolorato, C. Padalino, M. Candelli, M. E. De Leo, L. Santarelli, M. Giacovazzo, A. Gasbarrini & P. Pola (2003) Association between migraine and Celiac disease: results from a preliminary case-control and therapeutic study. Am J Gastroenterol, 98, 625-9. Genuis, S. J. & T. P. Bouchard (2010) Celiac disease presenting as autism. J Child Neurol, 25, 114-9. Hadjivassiliou, M., P. Aeschlimann, A. Strigun, D. S. Sanders, N. Woodroofe & D. Aeschlimann (2008a) Autoantibodies in gluten ataxia recognize a novel neuronal transglutaminase. Ann Neurol, 64, 332-43. Hadjivassiliou, M., S. Boscolo, G. A. Davies-Jones, R. A. Grnewald, T. Not, D. S. Sanders, J. E. Simpson, E. Tongiorgi, C. A. Williamson & N. M. Woodroofe (2002) The humoral response in the pathogenesis of gluten ataxia. Neurology, 58, 1221-6. Hadjivassiliou, M., S. Boscolo, E. Tongiorgi, R. A. Grnewald, B. Sharrack, D. S. Sanders, N. Woodroofe & G. A. Davies-Jones (2008b) Cerebellar ataxia as a possible organ-specific autoimmune disease. Mov Disord, 23, 1370-7.
Neurological manifestations celiac 22 Hadjivassiliou, M., G. A. Davies-Jones, D. S. Sanders & R. A. Grnewald (2003) Dietary treatment of gluten ataxia. J Neurol Neurosurg Psychiatry, 74, 1221-4. Hadjivassiliou, M., A. Gibson, G. A. Davies-Jones, A. J. Lobo, T. J. Stephenson & A. Milford-Ward (1996) Does cryptic gluten sensitivity play a part in neurological illness? Lancet, 347, 369-71. Hadjivassiliou, M., R. A. Grnewald, A. K. Chattopadhyay, G. A. Davies-Jones, A. Gibson, J. A. Jarratt, R. H. Kandler, A. Lobo, T. Powell & C. M. Smith (1998) Clinical, radiological, neurophysiological, and neuropathological characteristics of gluten ataxia. Lancet, 352, 1582-5. Hadjivassiliou, M., R. A. Grnewald, R. H. Kandler, A. K. Chattopadhyay, J. A. Jarratt, D. S. Sanders, B. Sharrack, S. B. Wharton & G. A. Davies-Jones (2006a) Neuropathy associated with gluten sensitivity. J Neurol Neurosurg Psychiatry, 77, 1262-6. Hadjivassiliou, M., R. A. Grnewald, M. Lawden, G. A. Davies-Jones, T. Powell & C. M. Smith (2001) Headache and CNS white matter abnormalities associated with gluten sensitivity. Neurology, 56, 385-8. Hadjivassiliou, M., R. H. Kandler, A. K. Chattopadhyay, A. G. Davies-Jones, J. A. Jarratt, D. S. Sanders, B. Sharrack & R. A. Grnewald (2006b) Dietary treatment of gluten neuropathy. Muscle Nerve, 34, 762-6. Hadjivassiliou, M., D. G. Rao, S. B. Wharton, D. S. Sanders, R. A. Grnewald & A. G. Davies-Jones (2010) Sensory ganglionopathy due to gluten sensitivity. Neurology, 75, 1003-8. Hallert, C., M. Svensson, J. Tholstrup & B. Hultberg (2009) Clinical trial: B vitamins improve health in patients with coeliac disease living on a gluten-free diet. Aliment Pharmacol Ther, 29, 811-6. Hill, I. D., M. H. Dirks, G. S. Liptak, R. B. Colletti, A. Fasano, S. Guandalini, E. J. Hoffenberg, K. Horvath, J. A. Murray, M. Pivor, E. G. Seidman & H. p. a. N. North American Society for Pediatric Gastroenterology (2005) Guideline for the diagnosis and treatment of celiac disease in children: recommendations of the North American Society for Pediatric Gastroenterology, Hepatology and Nutrition. J Pediatr Gastroenterol Nutr, 40, 1-19. Huser, W., K. H. Janke, B. Klump, M. Gregor & A. Hinz (2010) Anxiety and depression in adult patients with celiac disease on a gluten-free diet. World J Gastroenterol, 16, 2780-7. Kawashti, M. I., O. R. Amin & N. G. Rowehy (2006) Possible immunological disorders in autism: concomitant autoimmunity and immune tolerance. Egypt J Immunol, 13, 99-104. Kelkar, P., M. A. Ross & J. Murray (1996) Mononeuropathy multiplex associated with celiac sprue. Muscle Nerve, 19, 234-6. Lammers, K. M., R. Lu, J. Brownley, B. Lu, C. Gerard, K. Thomas, P. Rallabhandi, T. Shea-Donohue, A. Tamiz, S. Alkan, S. Netzel-Arnett, T. Antalis, S. N. Vogel & A. Fasano (2008) Gliadin induces an increase in intestinal permeability and zonulin
Neurological manifestations of celiac
release by binding to the chemokine receptor CXCR3. Gastroenterology, 135, 194-204.e3. Leggio, L., L. Abenavoli, C. D'Angelo, D. Di Giuda, G. Gasbarrini & G. Addolorato (2004) Gluten-related cerebral hypoperfusion and neurologic disorders in coeliac patients. Aliment Pharmacol Ther, 20, 821-2; author reply 822. Lionetti, E., R. Francavilla, L. Maiuri, M. Ruggieri, M. Spina, P. Pavone, T. Francavilla, A. M. Magist & L. Pavone (2009) Headache in pediatric patients with celiac disease and its prevalence as a diagnostic clue. J Pediatr Gastroenterol Nutr, 49, 202-7. Londei, M., C. Ciacci, I. Ricciardelli, L. Vacca, S. Quaratino & L. Maiuri (2005) Gliadin as a stimulator of innate responses in celiac disease. Mol Immunol, 42, 913-8. Ludvigsson, J. F., T. Olsson, A. Ekbom & S. M. Montgomery (2007) A population-based study of coeliac disease, neurodegenerative and neuroinflammatory diseases. Aliment Pharmacol Ther, 25, 1317-27. Maiuri, L., C. Ciacci, I. Ricciardelli, L. Vacca, V. Raia, S. Auricchio, J. Picard, M. Osman, S. Quaratino & M. Londei (2003) Association between innate response to gliadin and activation of pathogenic T cells in coeliac disease. Lancet, 362, 30-7. Murray, J. A., T. Watson, B. Clearman & F. Mitros (2004) Effect of a gluten-free diet on gastrointestinal symptoms in celiac disease. Am J Clin Nutr, 79, 669-73. Niederhofer, H. & K. Pittschieler (2006) A preliminary investigation of ADHD symptoms in persons with celiac disease. J Atten Disord, 10, 200-4. Oberhuber, G., G. Granditsch & H. Vogelsang (1999) The histopathology of coeliac disease: time for a standardized report scheme for pathologists. Eur J Gastroenterol Hepatol, 11, 1185-94. Pavone, L., A. Fiumara, G. Bottaro, D. Mazzone & M. Coleman (1997) Autism and celiac disease: failure to validate the hypothesis that a link might exist. Biol Psychiatry, 42, 72-5. Pynnnen, P. A., E. T. Isomets, M. A. Verkasalo, S. A. Khknen, I. Sipil, E. Savilahti & V. A. Aalberg (2005) Gluten-free diet may alleviate depressive and behavioural symptoms in adolescents with coeliac disease: a prospective follow-up caseseries study. BMC Psychiatry, 5, 14. Rampertab, S. D., N. Pooran, P. Brar, P. Singh & P. H. Green (2006) Trends in the presentation of celiac disease. Am J Med, 119, 355.e9-14. Ravikumara, M., V. K. Nootigattu & B. K. Sandhu (2007) Ninety percent of celiac disease is being missed. J Pediatr Gastroenterol Nutr, 45, 497-9. Ruuskanen, A., K. Kaukinen, P. Collin, H. Huhtala, R. Valve, M. Mki & L. Luostarinen (2010) Positive serum antigliadin antibodies without celiac disease in the elderly population: does it matter? Scand J Gastroenterol, 45, 1197-202. Samaroo, D., F. Dickerson, D. D. Kasarda, P. H. Green, C. Briani, R. H. Yolken & A. Alaedini (2010) Novel immune response to gluten in individuals with schizophrenia. Schizophr Res, 118, 248-55.
Neurological manifestations celiac 24 Sanders, D. S., D. Patel, T. J. Stephenson, A. M. Ward, E. V. McCloskey, M. Hadjivassiliou & A. J. Lobo (2003) A primary care cross-sectional study of undiagnosed adult coeliac disease. Eur J Gastroenterol Hepatol, 15, 407-13. Sapone, A., L. de Magistris, M. Pietzak, M. G. Clemente, A. Tripathi, F. Cucca, R. Lampis, D. Kryszak, M. Carten, M. Generoso, D. Iafusco, F. Prisco, F. Laghi, G. Riegler, R. Carratu, D. Counts & A. Fasano (2006) Zonulin upregulation is associated with increased gut permeability in subjects with type 1 diabetes and their relatives. Diabetes, 55, 1443-9. Sapone, A., K. M. Lammers, V. Casolaro, M. Cammarota, M. T. Giuliano, M. De Rosa, R. Stefanile, G. Mazzarella, C. Tolone, M. I. Russo, P. Esposito, F. Ferraraccio, M. Carteni, G. Riegler, L. de Magistris & A. Fasano (2011) Divergence of gut permeability and mucosal immune gene expression in two gluten-associated conditions: celiac disease and gluten sensitivity. BMC Med, 9, 23. Schrdl, D., F. Kahlenberg, K. Peter-Zimmer, W. Hermann, H. J. Khn & T. Mothes (2004) Intrathecal synthesis of autoantibodies against tissue transglutaminase. J Autoimmun, 22, 335-40. Szebeni, B., G. Veres, A. Dezsofi, K. Rusai, A. Vannay, G. Bokodi, B. Vsrhelyi, I. R. Korponay-Szab, T. Tulassay & A. Arat (2007) Increased mucosal expression of Toll-like receptor (TLR)2 and TLR4 in coeliac disease. J Pediatr Gastroenterol Nutr, 45, 187-93. Vader, W., Y. Kooy, P. Van Veelen, A. De Ru, D. Harris, W. Benckhuijsen, S. Pea, L. Mearin, J. W. Drijfhout & F. Koning (2002) The gluten response in children with celiac disease is directed toward multiple gliadin and glutenin peptides. Gastroenterology, 122, 1729-37. Vojdani, A., M. Bazargan, E. Vojdani, J. Samadi, A. A. Nourian, N. Eghbalieh & E. L. Cooper (2004a) Heat shock protein and gliadin peptide promote development of peptidase antibodies in children with autism and patients with autoimmune disease. Clin Diagn Lab Immunol, 11, 515-24. Vojdani, A., T. O'Bryan, J. A. Green, J. Mccandless, K. N. Woeller, E. Vojdani, A. A. Nourian & E. L. Cooper (2004b) Immune response to dietary proteins, gliadin and cerebellar peptides in children with autism. Nutr Neurosci, 7, 151-61. Watts, T., I. Berti, A. Sapone, T. Gerarduzzi, T. Not, R. Zielke & A. Fasano (2005) Role of the intestinal tight junction modulator zonulin in the pathogenesis of type I diabetes in BB diabetic-prone rats. Proc Natl Acad Sci U S A, 102, 2916-21. Wei, J. & G. P. Hemmings (2005) Gene, gut and schizophrenia: the meeting point for the gene-environment interaction in developing schizophrenia. Med Hypotheses, 64, 547-52. West, J., R. F. Logan, P. G. Hill, A. Lloyd, S. Lewis, R. Hubbard, R. Reader, G. K. Holmes & K. T. Khaw (2003) Seroprevalence, correlates, and characteristics of undetected coeliac disease in England. Gut, 52, 960-5.
Neurological manifestations of celiac
West, J., R. F. Logan, R. B. Hubbard & T. R. Card (2006) Risk of schizophrenia in people with coeliac disease, ulcerative colitis and Crohn's disease: a general population-based study. Aliment Pharmacol Ther, 23, 71-4. Young, J. (2008) Common comorbidities seen in adolescents with attentiondeficit/hyperactivity disorder. Adolesc Med State Art Rev, 19, 216-28, vii. Zingone, F., M. Siniscalchi, P. Capone, R. Tortora, P. Andreozzi, E. Capone & C. Ciacci (2010) The quality of sleep in patients with coeliac disease. Aliment Pharmacol Ther, 32, 1031-6.
Você também pode gostar
- Celiac Disease: GeneticsDocumento10 páginasCeliac Disease: Geneticslotp12Ainda não há avaliações
- Celiac Disease (Gluten-Sensitive Enteropathy)Documento6 páginasCeliac Disease (Gluten-Sensitive Enteropathy)Cricket Trick & FitnessAinda não há avaliações
- CELIAC DISEASE REVIEW EXAMINES DIAGNOSIS AND TESTINGDocumento3 páginasCELIAC DISEASE REVIEW EXAMINES DIAGNOSIS AND TESTINGkmaher8256Ainda não há avaliações
- Celiac Disease: Clinical PracticeDocumento8 páginasCeliac Disease: Clinical PracticeRo RojasAinda não há avaliações
- Celiac DiseaseDocumento11 páginasCeliac DiseaseXela AviàAinda não há avaliações
- Diseases: The Role of Environmental Factors in The Development of Celiac Disease: What Is New?Documento12 páginasDiseases: The Role of Environmental Factors in The Development of Celiac Disease: What Is New?Mayda AfAinda não há avaliações
- Complementary and Alternative Medical Lab Testing Part 14: ImmunologyNo EverandComplementary and Alternative Medical Lab Testing Part 14: ImmunologyAinda não há avaliações
- Celiac Disease and The Potential of Stems Cells As TreatmentDocumento9 páginasCeliac Disease and The Potential of Stems Cells As TreatmentAthenaeum Scientific PublishersAinda não há avaliações
- Doença Celíaca Revisão 2017Documento14 páginasDoença Celíaca Revisão 2017Bianca CorreaAinda não há avaliações
- Doença Celíaca - Revisão Lancet 2018Documento12 páginasDoença Celíaca - Revisão Lancet 2018Bianca CorreaAinda não há avaliações
- Cross Edit Neuro CelDocumento3 páginasCross Edit Neuro CelMihaela MtnAinda não há avaliações
- Future diagnosis and management of celiac diseaseDocumento9 páginasFuture diagnosis and management of celiac diseaseمودة المنعميAinda não há avaliações
- NCGS or WIS - J Pediatr 2015Documento7 páginasNCGS or WIS - J Pediatr 2015Fernando Clemente YagoAinda não há avaliações
- Epidemiology, Pathogenesis, and Clinical Manifestations of Celiac Disease in Adults - UpToDateDocumento41 páginasEpidemiology, Pathogenesis, and Clinical Manifestations of Celiac Disease in Adults - UpToDatealinetibes1Ainda não há avaliações
- Celiac Disease Paper 1Documento21 páginasCeliac Disease Paper 1M SalmanAinda não há avaliações
- Case Questions and Case StudyDocumento15 páginasCase Questions and Case Studyapi-240616135Ainda não há avaliações
- Inflammatorybowel Disease: Anne Walsh,, John Mabee,, Kashyap TrivediDocumento18 páginasInflammatorybowel Disease: Anne Walsh,, John Mabee,, Kashyap Trivediangeldavid26Ainda não há avaliações
- 147 Galleys 1591 3 10 20230712Documento12 páginas147 Galleys 1591 3 10 20230712Amir KhanAinda não há avaliações
- Effect of Gluten-Free Diet On Gut MicrobiotaDocumento23 páginasEffect of Gluten-Free Diet On Gut Microbiotaandressa yabikuAinda não há avaliações
- Brottveit 2013Documento9 páginasBrottveit 2013posclinicaarquivoAinda não há avaliações
- Rcuh PDFDocumento27 páginasRcuh PDFicoanamareAinda não há avaliações
- The Molecular Investigation of Celiac DiseaseDocumento7 páginasThe Molecular Investigation of Celiac DiseasesserggiosAinda não há avaliações
- Summary of Andrew J. Wakefield's Waging War On The Autistic ChildNo EverandSummary of Andrew J. Wakefield's Waging War On The Autistic ChildAinda não há avaliações
- Fped 06 00350Documento19 páginasFped 06 00350Jake DagupanAinda não há avaliações
- Gluten Related Disorders Celiac Disease Wheat Allergy and Nonceliac Gluten SensitivityDocumento17 páginasGluten Related Disorders Celiac Disease Wheat Allergy and Nonceliac Gluten SensitivityAngélica MuñozAinda não há avaliações
- Case StudyDocumento12 páginasCase Studyapi-242211536100% (1)
- Nutrition's Role in Celiac Disease DevelopmentDocumento4 páginasNutrition's Role in Celiac Disease DevelopmentKajee GrantAinda não há avaliações
- Are Viruses Causing Celiac DiseaseDocumento5 páginasAre Viruses Causing Celiac DiseaseFrancisco Lopez LopeAinda não há avaliações
- Pharmaceutical Sciences: Celiac Disease: From Pathophysiology To TreatmentDocumento4 páginasPharmaceutical Sciences: Celiac Disease: From Pathophysiology To TreatmentiajpsAinda não há avaliações
- Autoimmune Disorders Associated To Type 1Documento10 páginasAutoimmune Disorders Associated To Type 1Ina SimacheAinda não há avaliações
- Celiac Disease New Approaches To Therapy: A ReviewDocumento14 páginasCeliac Disease New Approaches To Therapy: A ReviewCeliacDesiAinda não há avaliações
- El Chammas2011Documento7 páginasEl Chammas2011lalala lalalalAinda não há avaliações
- Celiac DiseaseDocumento25 páginasCeliac DiseaseMateen ShukriAinda não há avaliações
- The Link Between The Clinical Features o PDFDocumento2 páginasThe Link Between The Clinical Features o PDFwulanAinda não há avaliações
- Gluten IntoleranceDocumento8 páginasGluten IntoleranceSanda Maria CretoiuAinda não há avaliações
- Zacharyhuntresearchpaper CeliacdiseaseDocumento9 páginasZacharyhuntresearchpaper Celiacdiseaseapi-328409633Ainda não há avaliações
- 2008 Wieser de CititDocumento13 páginas2008 Wieser de CititElisabeta StamateAinda não há avaliações
- Boala CelacaDocumento6 páginasBoala Celacacroitoru tatianaAinda não há avaliações
- Fmu Trainging ModuleDocumento23 páginasFmu Trainging ModulesamAinda não há avaliações
- Celiac Disease: Mobin Ur RehmanDocumento46 páginasCeliac Disease: Mobin Ur RehmanMobin Ur Rehman KhanAinda não há avaliações
- Celiac DiseaseDocumento37 páginasCeliac DiseaseTaj lamajed100% (1)
- Celiac Disease Research Paper OutlineDocumento7 páginasCeliac Disease Research Paper Outlinefvgcaatd100% (1)
- Celiac Disease With Balanced TranslocationDocumento3 páginasCeliac Disease With Balanced TranslocationAdvanced Research PublicationsAinda não há avaliações
- GWAS Data Analysis of Type 1 Diabetes Using Pathway and Network ApproachesDocumento38 páginasGWAS Data Analysis of Type 1 Diabetes Using Pathway and Network ApproachesathayafebAinda não há avaliações
- Review Article: Streptozotocin-Induced Diabetes Models: Pathophysiological Mechanisms and Fetal OutcomesDocumento12 páginasReview Article: Streptozotocin-Induced Diabetes Models: Pathophysiological Mechanisms and Fetal OutcomesMayra PereiraAinda não há avaliações
- REVISADO Murch2016 - Article - RecentAdvancesInCeliacDiseaseDocumento8 páginasREVISADO Murch2016 - Article - RecentAdvancesInCeliacDiseaseCamilo ReyesAinda não há avaliações
- Epidemiology, Pathogenesis, and Clinical Manifestations of Celiac Disease in Children - UpToDateDocumento26 páginasEpidemiology, Pathogenesis, and Clinical Manifestations of Celiac Disease in Children - UpToDatejandagashvili2007Ainda não há avaliações
- Complementary and Alternative Medical Lab Testing Part 12: NeurologyNo EverandComplementary and Alternative Medical Lab Testing Part 12: NeurologyAinda não há avaliações
- Celiac Disease in Children: A Review of The LiteratureDocumento20 páginasCeliac Disease in Children: A Review of The LiteraturefaithAinda não há avaliações
- Challenges in Differential Diagnosis of Coeliac DiDocumento10 páginasChallenges in Differential Diagnosis of Coeliac DiNäjlãå SlnAinda não há avaliações
- Celiac DiseaseDocumento8 páginasCeliac DiseaseKristine KaneichiAinda não há avaliações
- Frontiers in Celiac Disease (Pediatric and Adolescent Medicine, Vol. 12)Documento231 páginasFrontiers in Celiac Disease (Pediatric and Adolescent Medicine, Vol. 12)Lina LynaAinda não há avaliações
- Novel Immune Response To Gluten in Individuals WithDocumento15 páginasNovel Immune Response To Gluten in Individuals WithMartha DiazAinda não há avaliações
- Immunology of Type 1 DiabetesDocumento14 páginasImmunology of Type 1 DiabetesKPRI Bina WaluyaAinda não há avaliações
- Kejang Hiperglikemi PDFDocumento10 páginasKejang Hiperglikemi PDFNishfullaili Nurun NisaAinda não há avaliações
- Chronic Constipation in A 7-Year-Old Boy: Judy-April Oparaji, MD, RDN, CSP, Theresa Heifert, MDDocumento5 páginasChronic Constipation in A 7-Year-Old Boy: Judy-April Oparaji, MD, RDN, CSP, Theresa Heifert, MDbella friscaamaliaAinda não há avaliações
- Epigenetic Alterations Related To Gestational Diabetes MellitusDocumento15 páginasEpigenetic Alterations Related To Gestational Diabetes MellitusEdgar GustavoAinda não há avaliações
- Non-Classical Celiac Disease: Often MissedDocumento11 páginasNon-Classical Celiac Disease: Often MissedMounira MHAinda não há avaliações
- Safety and Health at Work: Kyung-Taek RimDocumento8 páginasSafety and Health at Work: Kyung-Taek RimAkbarAinda não há avaliações
- Bishop Score of PregnancyDocumento13 páginasBishop Score of PregnancydrvijeypsgAinda não há avaliações
- Antepartum HemorrhageDocumento3 páginasAntepartum Hemorrhagenur1146Ainda não há avaliações
- NCM 106 Pharmacology: St. Thomas Aquinas: Prayer Before StudyDocumento29 páginasNCM 106 Pharmacology: St. Thomas Aquinas: Prayer Before StudyNurse HoomanAinda não há avaliações
- Japan Metabo LawDocumento16 páginasJapan Metabo LawReginAinda não há avaliações
- CAz Clinic Poliserozita UMFDocumento16 páginasCAz Clinic Poliserozita UMFMariaIoanaCoroiuAinda não há avaliações
- Mens Health Philippines 2013Documento2 páginasMens Health Philippines 2013Kallyx Kiel ManjiroAinda não há avaliações
- Department of Genetics: Covid-19 RT PCRDocumento1 páginaDepartment of Genetics: Covid-19 RT PCRAshwin ShajiAinda não há avaliações
- WHO 2019 nCoV Vaccination Microplanning 2021.1 EngDocumento81 páginasWHO 2019 nCoV Vaccination Microplanning 2021.1 Engdr.tabitaAinda não há avaliações
- RockerDocumento2 páginasRockerwan hseAinda não há avaliações
- Clinical Practice Guidelines for Hepatitis B Virus (HBV) ManagementDocumento48 páginasClinical Practice Guidelines for Hepatitis B Virus (HBV) ManagementAqila MumtazAinda não há avaliações
- Sf2 - 2022 - Grade 1 - RoseDocumento3 páginasSf2 - 2022 - Grade 1 - RoseNorlds TacukenAinda não há avaliações
- Legal and Ethical Issues in NursingDocumento53 páginasLegal and Ethical Issues in Nursingkrishnasree100% (2)
- Motivation Letter - EmboDocumento1 páginaMotivation Letter - EmboFebby NurdiyaAinda não há avaliações
- Telaah Jurnal KGDDocumento17 páginasTelaah Jurnal KGDriska eka fatma HasibuanAinda não há avaliações
- Penggunaan Polyethylene Fiber-Reinforced Composite Resin Sebagai Short Post Dan Inti Pada Gigi Anterior Sulung Dengan Karies Yang Luas Laporan KasusDocumento14 páginasPenggunaan Polyethylene Fiber-Reinforced Composite Resin Sebagai Short Post Dan Inti Pada Gigi Anterior Sulung Dengan Karies Yang Luas Laporan Kasusfebriani serojaAinda não há avaliações
- CPG Management of Dementia (2nd Edition)Documento162 páginasCPG Management of Dementia (2nd Edition)umiraihana1Ainda não há avaliações
- Introduction of Family MedicineDocumento52 páginasIntroduction of Family MedicineAyi Abdul BasithAinda não há avaliações
- Contingency Plan For Covid 19Documento27 páginasContingency Plan For Covid 19Oteee17Ainda não há avaliações
- GMDSS Exam Schedule For Year 2022Documento7 páginasGMDSS Exam Schedule For Year 2022Mani ThapaAinda não há avaliações
- NHS Pan London Follicular Lymphoma 2018Documento18 páginasNHS Pan London Follicular Lymphoma 2018Syed Touseef AhmedAinda não há avaliações
- Medsurg RoleDocumento12 páginasMedsurg RoleRUby JanabanAinda não há avaliações
- Advantage and DisadvantageDocumento5 páginasAdvantage and Disadvantageحسين يوسفAinda não há avaliações
- 1.maternal and Child Health NursingDocumento33 páginas1.maternal and Child Health NursingBhie Bhie100% (1)
- Professional Football Club Registration & Consent Form: Personal Information - Child / Young PersonDocumento2 páginasProfessional Football Club Registration & Consent Form: Personal Information - Child / Young PersonanilAinda não há avaliações
- Resume William S Tokasz December 2015 For BuffstateDocumento2 páginasResume William S Tokasz December 2015 For Buffstateapi-301347959Ainda não há avaliações
- INI-CET Corrigendum No.23-2020. & Sponsorship Certificate PDFDocumento2 páginasINI-CET Corrigendum No.23-2020. & Sponsorship Certificate PDFpriyathileepan-1Ainda não há avaliações
- Fundamentals FM PDFDocumento10 páginasFundamentals FM PDFabdo elbahrawyAinda não há avaliações
- 5 dfgs34 24dDocumento2 páginas5 dfgs34 24dKenneth SyAinda não há avaliações
- Daily UrduDocumento4 páginasDaily UrduFurqanAftabAinda não há avaliações