Escolar Documentos
Profissional Documentos
Cultura Documentos
Immunohematology
Enviado por
dtimtimanTítulo original
Direitos autorais
Formatos disponíveis
Compartilhar este documento
Compartilhar ou incorporar documento
Você considera este documento útil?
Este conteúdo é inapropriado?
Denunciar este documentoDireitos autorais:
Formatos disponíveis
Immunohematology
Enviado por
dtimtimanDireitos autorais:
Formatos disponíveis
Subject: Clinical Pathology Topic: Immunohematology Lecturer: Dr.
Joan Pascual Rodriguez Date of Lecture: I forgot Transcriptionist: ior Editor: Pages: 10.5
I. IMMUNOHEMATOLOGY the study of immunologic reactions involving all components of blood deals with antigens, antibodies and antigen-antibody reactions
II. APPLICATIONS OF IMMUNOHEMATOLOGY
transfusion of blood and its components diagnosis, prevention and management of immunization associated with pregnancy laboratory resolution of parentage problems
III. DISEASE WHERE BLOOD TRANSFUSION IS NEEDED massive blood loss secondary to severe trauma dengue (where you have active bleeding and thrombocytopenia) patient with severe anemia
IV. DEFINITION OF TERMS Antigen any substance that stimulates production of antibodies (ANTIbody GENerator) Antibody proteins produced by the Reticuloendothelial system in response to antigen stimulation Agglutinogen antigen on the surface of RBC responsible for agglutination Agglutinin antibody that attacks RBC antigens, manifest its activity by clumping of the RBCs Hemolysin antibody that attacks RBC antigens, manifest its activity by lysis of the RBCs Agglutination clumping of RBCs as a result of antibodies binding to the antigenic sites of the adjacent cells Natural Antibodies antibodies that appear without antigenic stimulation, usually these are present during childhood and decreases as we age Acquired/Immune Antibodies antibodies that appear upon introduction of antigen by disease, transfusion, pregnancy and substances chemically related to RBC antigen Complete Antibodies - bivalent antibodies, can agglutinate RBCs Incomplete Antibodies - univalent antibodies, coats RBCs but cannot directly agglutinate them. They require a special enzyme for agglutination to occur Isoantibodies/Alloantibodies antibodies produced against antigen from genetically different individuals coming from the same specie. Auto antibodies - antibodies produced against ones own tissue or self antigens ( as seen in autoimmune diseases) Warm Antibodies o antibodies which react best in vitro at body temp of 37oC o usually IgG o require exposure to foreign antigen before they are produced hence they are also called acquired antibodies o Most are clinically significant except the (ABO blood group which are IgM)
SY 2011-2012
Coats red cells at body temperature and lead to removal by macrophages (extravascular hemolysis) o IgG are small and therefore these antibodies can cross the placenta Cold Antibodies o Antibodies which react best in vitro at 4-10oC or < 25oC o Usually IgM o Exist in humans regardless of whether they have been pregnant or transfused hence they are also called natural antibodies o Most are not clinically significant except for the ABO IgM antibodies o When significant IgM antibodies are very efficient in fixing complement and causes (intravascular hemolysis) o IgM are pentamers composed of 5 subunits of globulin chains therefore they are big and cannot cross the placenta
V. BLOOD GROUP SYSTEM A. ABO blood Group first blood group discovered most significant for transfusion practice ABO compatibility is essential before other pre transfusion test is performed ABO antigens are the only antigens for which reciprocal antibodies exist in serum of normal individuals BIOCHEMISTRY: all of the antigens in the ABO blood group have the same core backbone the PARAGLOBOSIDE composed of (glucose, galactose and N-acetylgalactosamine) o H antigen Precursor to the A and B Made by adding fucose to paragloboside Only after the H antigen is made can the A or B antigens can be added A and B antigens functionally mask the H antigen (the more A and B that is made the less H is present) Type O cells have no A or B antigen so they express the greatest amount of H antigen o A antigen Formed by the addition of N-acetylgalactosamine to the H antigen o B antigen Formed by the addition of galactose to the H antigen
(For people who are visual this is the picture of what is written above)
BLOOD GROUPS o Group A Express A antigen on RBC surface Genotypes AA or AO Have naturally occurring, clinically significant, predominantly IgM with a small amount of IgG antibodies against type B (antibody B) Subgroups A1 (80%) most common form of A antigen A2 (20%) significant because it contains anti A1 antibodies o Group B Express B antigen on their surface Genotypes BB or BO Have naturally occurring, clinically significant, predominantly IgM with a small amount of IgG antibodies against type A antigen (antibody A) o Group O Have neither A nor B antigens on their RBC surface Genotype OO Universal donors have naturally occurring, clinically significant very high titer anti A, anti B and anti AB antibodies the reason why it can only receive blood donors from blood type O maternal anti A and B antibodies are IgG and therefore can cross the placenta to cause hemolytic disease of the newborn Group AB Express A and B antigen on RBC surface Genotypes A1B or A2B remember that A antigen has two subgroups Have no ABO antibodies therefore it is the universal recipient because it can accept blood from all types without the risk of coagulation BLOOD GROUP A B AB O RBC ANTIGEN A B AB O SERUM ANTIBODY B A None A, B and AB
*** remember that antibodies are found circulating in the blood serum and that antigens are located on RBC surfaces ABO BLOOD GROUP TESTING o Forward Typing/Forward Grouping Also called cell typing Testing antigens on red cells Patients red cells plus commercial sera (anti A and anti B)
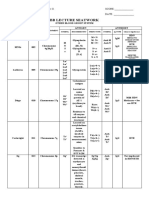
FORWARD TYPING (uses patients RBCs) ABO BLOOD GROUP Anti A Reagent Anti B Reagent AB + + A + B + O ***NOTE: (+) indicates presence of agglutination : Since you are using the red cells you are testing for the Antigens present : The reagents contain the antibodies against the particular antigen present in the RBC : Blood type is determined in the reagent that has agglutination
Reverse Typing also called serum or back typing uses patients serum versus commercial A1 and B cells analyzes patients serum for the presence of Anti A and Anti B antibodies Patients serum plus commercial A and B cells REVERSE TYPING (uses patients serum) A1 Cells B Cells + + + +
ABO BLOOD GROUP AB A B O
***NOTE: since you are using the serum you are looking for the ANTIBODIES present : Example: AB. It is (-) for A and (-) for B, therefore there are no antibodies present in AB : Testing antibodies are not reliable until 6 months of age because newborn serum may contain maternal IgG anti A or anti B which can interfere with the result. COMMON CAUSES OF ABO DISCREPANCIES When the results of the forward and back typing are not compatible, that is ABO discrepancy 1. Abnormal Antigens Person has A2 blood group with anti A1 formation FORWARD TYPING Anti A + Anti B REVERSE TYPING A1 Cells + B cells +
Forward blood type: A ; Reverse blood type: O (+) for B because blood type A has antibodies for B (+) for A1 because there are some people who have A2 blood group with anti A1. Since A1 cells were used, it will react to that causing agglutination To differentiate A1 from A1 you need a special lectin. 2. Acquire B phenotype Seen in group A patients with exposure to gram negative bacteria by way of intestinal obstruction, gram negative sepsis or colon cancer Bacteria removes the N-acetyl group in the A antigen, leaving only the galactosamine. The resultant chains is very much similar to the B antigen, such that the patients express weak B antigens FORWARD TYPING Anti A +++ Anti B + REVERSE TYPING A1 Cells B cells +
Forward typing: AB ; Reverse typing: A (+) for A in forward typing because the patient is blood type A (+) for B in forward typing because they express weak B antigen (+) for B in reverse typing because blood type A has antibodies for B
3. Weak or Missing Antibodies
Common in newborn, elderly, immunosupressed individuals and other conditions that yield hypo/aggamaglobulinemia (decreased or absence of antibodies) REVERSE TYPING A1 Cells B cells -
FORWARD TYPING Anti A + Anti B -
Forward Typing: A or B depends on the antigen present in here we used type A ; Reverse typing: AB due to absence of antibodies Failure to produce antibodies will lead to AB like blood type 4. Non ABO antibodies Ex. Polyagglutinins and multiple myeloma. When present it can cause agglutination of red cells FORWARD TYPING Anti A + Anti B + REVERSE TYPING A1 Cells + B cells +
Forward Typing: A, B, AB or O. in here we just used AB. ; Reverse typing: O Since they cause agglutination of red cells they will type as O on reverse typing (+ for anti A and + for Anti B)
5. Bombay (Oh) Phenotype Patient lack the H gene and therefore cannot make H antigen nor A or B antigen on their red cells (because you need the H antigen as precursor) Forward typing: O (because they do not have A and B antigens) Cause discrepancies on reverse typing o Serum agglutinates A1, B and O cells (A and B antigens mask the H antigen. O cells do not because they dont have A and B antigens). The Bombay phenotype will react to the O cells because they do not have the H antigen, which the O cells have o Confirmatory testing is done using an anti H reagent made from Ulex europaeus plant o Red cells + anti H = NO AGGLUTINATION (there will be no agglutination because theres no H antigen. Even if you have H antibodies there is no antigen to act on. o Have very strong anti A, anti B and anti H and can only receive blood from a Bombay Donor. ** I got confused with the mechanism so I tried to scan wiki. It says that Bombay phenotype doesnt have any antigen (A, B, AB and O) because theres no precursor which is the (H antigen) this is also the antigen of blood type O. Bombays can donate blood to all blood types because phenotypically it is O ( does not have antibody A and antibody B) but cannot accept A, B, AB and O because these set of antigens are not present on the Bombay persons blood and therefore it is not recognized and it will cause an immune reaction. Get it?
Rh BLOOD GROUPS o Complex blood group with > 50 described antigens 1. Nomenclature System a. Fisher Race (English) used by the British Has 5 major antigens (D, C, E, c and e) The one used in the laboratory Chromosome D C e Antigen D C e antibody Anti D Anti C Anti e
Closely linked genes
b. Weiner (American) Has 5 major antigens (Rho, rh, rh, hr,hr)
Chromosome Antigen From a single gene R1 Rh1
Blood Factors Rho rh hr
Antibody Anti Rho anti rh anti hr
2. Rh Antigens lacks corresponding naturally occurring antibodies produce antibodies only after exposure when Rh antibodies are present they are the result of sensitization caused by previous transfusion or pregnancy Fisher Race Weiner D Rho C rh E rh c hr e hr These are the counterparts for the American and British version 3. Rh Antibodies Formation of antibodies may be secondary to transfusion or pregnancy Anti D (Rho), anti C (rh), anti E (rh), anti c (hr), and anti e (hr) have all been known to cause hemolytic transfusion reaction and hemolytic disease of the newborn. Warm reacting, exposure-requiring IgG antibodies that are clinically significant Infants < 4 months usually do not form new antibodies against any incompatible red cell antigens. (immature pa ung immune system nila) 4. Rh Blood Group Testing Testing for D (Rho) antigen is the most common Rh test performed (because it is the most immunogenic) Rh positive also means D positive D antigens are potent immunogens. (Thats why of D negative patients, 80% will develop an anti D when transfused with a single unit of D positive blood). 5. Weak D Phenotype (D) Weakly expressed D antigens that require more sensitive testing to detect it All apparently D negative blood donors must have a weak D test to avoid false classification
When you have determined that a patient has a weak D phenotype, you label them as D positive this is because they still have the antigen its just that the antigen is weak, but the patient can still develop antibodies against the D antigen
OTHER BLOOD GROUPS SYSTEM 1. Kell (K, k, kx) 2. Duffy (Fy) 3. MNSs 4. P 5. Lewis (Le) 6. Lutheran (Lu) o All of these may cause transfusion reactions are hemolytic disease of the newborn. o May interfere with cross matching o For medico legal parenthood problems TRANSFUSION RELATED TESTING o Used to identify clinically significant antigens on red cells o To identify plasma antibodies to red cells o To detect antibodies and complement bound to red cells o IgM and IgG antibodies comprise 80% of the circulating antibodies and are the most significant antibodies for transfusions related testing (because they can cause intra and extravascular hemolysis) o To detect antibodies particularly IgG or complement bound to RBC, anti human globulin reagent (Coombs Reagent ) can be added o Agglutination (clumping) of RBCs is the end result of testing indicating a positive reaction COMMON TEST USED IN IMMUNOHEMATOLOGY o Antiglobulin (Coombs) Test Remains the most important single test in antibody detection Principle: Red Blood Cells sensitized by IgG or complement can be made to agglutinate by adding antihuman globulin 2 Types: 1. Direct Coombs Test (DAT direct antibody test) Detects RBCs that have already been sensitized with IgG Detects in vivo antibody coating (sensitization) of red cells Sample: Patients Red Cells Useful in Detection of hemolytic disease of the newborn ( using infants red cells) Investigation of transfusion reactions Detection of autoimmune hemolytic anemia (AIHA) Detection of red cells sensitization by certain drugs (penicillin, cephalothin, alpha methyldopa)
Patients red cells + Coombs Reagent. If you have antibodies coating the red cells you expect to see agglutination
2. Indirect Coombs Test (IAT indirect antibody test) Detects antibodies to RBC antigens present in the patients serum Detects in vitro red cell sensitization if red cells contain antigen corresponding to serum antibody Sample: Patients Serum Useful in Detection and identification of unexpected antibodies Compatibility testing (cross matching) Red cell antigen phenotyping Investigation of transfusion reactions Detecting Du antigen (weak D phenotype) Procedure Step 1: patients serum (with unknown Ab) + RBC with unknown (Ag) Step 2: product of step 1 + Coombs Reagent
In step 1: if the serum contains antibodies against antigens on the red cells, the antibodies will adhere to the antigen on the red cell. In step 2: when you add the Coombs Reagent, if there are antibodies attached to the antigens on the red cells, there will also be agglutinations
RBC Typing 1. Forward Typing 2. Reverse Typing 3. D antigen Cross Matching Absence of agglutination or hemolysis is essential to the safety of blood transfusion You do cross matching to check if your sample are compatible Uses To detect antibodies to the donor or recipient To detect ABO typing discrepancies Types: 1. Major Cross match Tests patients (recipients) serum + donor cells Detects antibodies in the patients serum that may destroy transfused donor RBCs Functions to determine the ABO compatibility of the donor cells Concept is like the indirect Coombs test 2. Minor Cross match Uses recipients red cells + donor serum Detects antibodies in the donor serum which may react with antigen in the recipient No longer requires as part of the cross match procedure Concept is like the directs Coombs test
3 phases when performing a cross match 1. Immediate Spin in saline at room temperature Patients serum + RBC will be mixed and centrifuged
Examine for hemolysis (red supernatant) or agglutination If there is agglutination, then it is positive on immediate spin phase 2. Incubation at 37oC with enhancement medium Patients Serum + donor RBC + enhancing medium (ex. Low ionic strength solution LISS, polyethylene glycol PEG or albumin) Incubate at 37oC and centrifuge Examine for hemolysis (red supernatant) or agglutination 3. Antiglobulin Phase after washing incubated cells with saline o After 37oC reading, wash RBCs with saline o Add AHG (Coombs Reagent) mix then centrifuge o Examine for hemolysis or agglutination *** NOTE: all 3 phases must be negative for hemolysis if there is no hemolysis in all 3 phases then youre ready for transfusion Effects of Temperature on Antibodies IgM antibodies are usually cold antibodies and are often detected in the immediate spin phase of testing ( so if you have + immediate spin phase, the antibodies are most likely IgM or cold antibodies) IgG antibodies usually react at 37oC and are referred as warm antibodies and are often detected in the antihuman globulin phase of testing ( so if you have a + result on that phase the antibodies are most likely IgG or Warm antibodies)
Antibody Screening Used to demonstrate unexpected antibodies in the serum of the recipient that may destroy donor RBCs that were thought to be compatible on the basis of the Rh and ABO typing Has replaced minor cross matching ** minsan kahit same blood type there is still reaction so dont give blood. Pre Transfusion/ Compatibility Testing You are testing the blood unit from the donor, if it is compatible with the recipients blood 1. Review recipients blood bank history a. Check for ABO discrepancies or crossmatching problems that have been demonstrated in previous transfusion 2. ABO and Rh typing of recipient and donor a. Should be compatible 3. Antibody screening of recipient and donor serum 4. Major crossmatching
HEMOLYTIC DISEASE OF THE NEWBORN o Also referred to as erythroblastosis fetalis or fetal hydrops o Occurs when the mother is alloimmunized to antigens found on the RBC of the fetus o End result: destruction of fetal RBCs by mothers IgG antibodies A. HDN due to Rh incompatibility o Set up: Rh (-)mother and Rh (+) baby o Once Rh (-) person is exposed to Rh (+) blood he will develop reaction after 2-4 weeks o Mother develops antibody against the Rh (+) blood coming from the baby o First baby is not affected: HDN occurs during subsequent pregnancies (because Rh antibodies are exposure requiring) o May be prevented by giving anti Rh to Rh (-) mothers in the ante natal (28weeks) and immediate postnatal period (within 72 hours after delivery) to neutralize the Rh antigens transfused into the mother
o o
On first exposure the mother develops antibodies against the Rh + blood of the baby On subsequent exposure since the mom already has the antibodies it will react to the babys Rh + blood cells causing hemolysis. This will destroy the fetal RBCs HEMOLYSIS
ANEMIA
HEMOGLOBIN DEGRADATION
EXTRAMEDULLARY
HYPOXIC INJURY TO LIVER AND HEART
INCREASE BILIRUBIN
HEPATOSPLENOMEGALY
HYDROPS (Anasarca of baby)
JAUNDICE KERNICTERUS (Deposition in tissue) (Deposition in Brain)
10
PHYSIOLOGY OF HDN o If hemolysis is not prevented it will lead to anemia and hemoglobin degradation o There is extramedullary hematopoiesis, so there will be an increase in RBC production in organs like the spleen and liver aside from the bone marrow, resulting to hepatosplenomegaly o Due to hypoxic injury to the liver, there will be decreased albumin. Since albumin controls oncotic pressure it will result to hydrops or generalized edema o There will also be increase in bilirubin , primarily conjugated, due to the breakdown of hemoglobin leading to the pathological condition of jaundice and kernicterus o Since bilirubin can cross the blood brain barrier it can be deposited in the brain causing kernicterus Factors affecting maternal response to Rh + fetal RBCs: o Concurrent ABO incompatibility o Dose of immunizing antigen o Isotype of antibody (IgM vs IgG) B: HDN DUE TO ABO INCOMPATIBILITY o Set up : type O mother + type A or B baby o ABO incompatibility occurs in 20-25% of pregnancies o Hemolytic disease occurs only in 10% o Treatment warranted in 1 out of 200 cases o Most anti A and anti B are IgM (do not cross the placenta so you dont have massive destruction of your fetal RBCs o A and B antigens are poorly expressed in neonatal RBCs
11
Você também pode gostar
- Microbiology (Bacteriolog) Lab - Practicals 1Documento4 páginasMicrobiology (Bacteriolog) Lab - Practicals 1Junno Turiano95% (20)
- Blood Bank Review 2019 PDFDocumento613 páginasBlood Bank Review 2019 PDFCuddles Pingoy100% (1)
- Chapter 25 - Extrinsic Defects Leading To Increased Erythrocyte Destruction - Immune Causes Final DraftDocumento2 páginasChapter 25 - Extrinsic Defects Leading To Increased Erythrocyte Destruction - Immune Causes Final DraftNathaniel SimAinda não há avaliações
- MUST To KNOW in HistopathologyDocumento34 páginasMUST To KNOW in HistopathologyRuiz Arenas Agacita89% (9)
- 3 ABO Discrepancies Other ProblemsDocumento65 páginas3 ABO Discrepancies Other ProblemsRuel Maddawin100% (2)
- Reviewer - Immunohematology - Part 1Documento16 páginasReviewer - Immunohematology - Part 1Joshua TrinidadAinda não há avaliações
- Modern Blood Banking & Transfusion Practices Ed6 Harmening-235-257Documento23 páginasModern Blood Banking & Transfusion Practices Ed6 Harmening-235-257ivanlchAinda não há avaliações
- ABO DiscrepanicesDocumento12 páginasABO DiscrepanicesGlenn PerezAinda não há avaliações
- Blood Bank Case StudyDocumento17 páginasBlood Bank Case StudyMelissa Harding33% (3)
- Forward and ReverseDocumento11 páginasForward and ReversecyrhenmieAinda não há avaliações
- MLT Blood Bank Exam 3 FullDocumento2 páginasMLT Blood Bank Exam 3 Fullkasdf gre bbtAinda não há avaliações
- Immunohematology Trans by KTRC (Wala Ito Sa Book)Documento21 páginasImmunohematology Trans by KTRC (Wala Ito Sa Book)Angelo ErispeAinda não há avaliações
- Plant Patho Lab Exer 2 Study QuestionsDocumento2 páginasPlant Patho Lab Exer 2 Study QuestionsJoni Gabriel Cruzata100% (3)
- ABO Blood Group SystemDocumento26 páginasABO Blood Group SystemFahimAinda não há avaliações
- 68th AACC Annual Scientific Meeting Abstract eBookNo Everand68th AACC Annual Scientific Meeting Abstract eBookAinda não há avaliações
- Essentials of ABO -Rh Grouping and Compatibility Testing: Theoretical Aspects and Practical ApplicationNo EverandEssentials of ABO -Rh Grouping and Compatibility Testing: Theoretical Aspects and Practical ApplicationNota: 5 de 5 estrelas5/5 (1)
- Pre Transfusion TestingDocumento57 páginasPre Transfusion TestingDominic Bernardo100% (4)
- C1 IH Lab L3 ABO Forward Reverse Typing Manual and Gel MethodDocumento8 páginasC1 IH Lab L3 ABO Forward Reverse Typing Manual and Gel MethodDIVINA KYLE YGOAinda não há avaliações
- Immunohematology Handouts UpdatedDocumento15 páginasImmunohematology Handouts UpdateddmclmllAinda não há avaliações
- Immunoserology: Medical Technology Assessment Progam 1 Discussed By: Mr. Mark MendrosDocumento8 páginasImmunoserology: Medical Technology Assessment Progam 1 Discussed By: Mr. Mark MendrosLea Juan100% (1)
- Blood Banking - Component PreparationDocumento34 páginasBlood Banking - Component PreparationLentoOt EksDiiAinda não há avaliações
- Blood Bank Harmening Chapter 10Documento14 páginasBlood Bank Harmening Chapter 10ichummy19100% (3)
- Blood Bank Guy Blood GroupsDocumento19 páginasBlood Bank Guy Blood GroupsJessica TuAinda não há avaliações
- Antibody IdentificationDocumento27 páginasAntibody Identificationhamaada100% (1)
- Flashcards in Abo Blood GroupDocumento10 páginasFlashcards in Abo Blood GroupVincent ReyesAinda não há avaliações
- Histopathology: Ann Fatima G. Quindao, RMT, LPT, MPHDocumento108 páginasHistopathology: Ann Fatima G. Quindao, RMT, LPT, MPHMarry Grace CiaAinda não há avaliações
- Other Blood Group System AssignmentDocumento5 páginasOther Blood Group System AssignmentMary ChristelleAinda não há avaliações
- Blood BankingDocumento118 páginasBlood BankingRay Jr Jr100% (2)
- MLT Blood Bank Exam 4 FullDocumento3 páginasMLT Blood Bank Exam 4 Fullkasdf gre bbtAinda não há avaliações
- ABO Discrepancy Assignment Spring 2021Documento5 páginasABO Discrepancy Assignment Spring 2021Ciarra AsuncionAinda não há avaliações
- Resolution of Abo DiscrepanciesDocumento4 páginasResolution of Abo DiscrepanciesPatrick MabugatAinda não há avaliações
- Blood BankDocumento32 páginasBlood Bankpikachu100% (1)
- RH Typing ReagentsDocumento2 páginasRH Typing ReagentsMelanie Tomita100% (1)
- Mtap - Immunohema Transfusion MedicineDocumento9 páginasMtap - Immunohema Transfusion MedicineMoira Pauline LibroraniaAinda não há avaliações
- MTAP ISBB - Sir JJ (Merged)Documento9 páginasMTAP ISBB - Sir JJ (Merged)Nathan DrakeAinda não há avaliações
- Immunohematology/ Blood BankingDocumento2 páginasImmunohematology/ Blood BankingSophia AmpatuanAinda não há avaliações
- Blood Banking: RH Blood Group SystemDocumento2 páginasBlood Banking: RH Blood Group SystemRomie Solacito100% (1)
- ImmunohematologyDocumento4 páginasImmunohematologyosama1381971Ainda não há avaliações
- Blood Banking Course BookDocumento2 páginasBlood Banking Course BookShukr Wesman BlbasAinda não há avaliações
- Blood Banking ReviewDocumento442 páginasBlood Banking ReviewMayra Flor100% (2)
- Blood BankingDocumento8 páginasBlood Bankingadagay100% (1)
- Recalls Ascp (Exam) - 2021 - 240103 - 185452Documento16 páginasRecalls Ascp (Exam) - 2021 - 240103 - 185452gaber 230100% (2)
- Study Stack - MLT Table ReviewDocumento3 páginasStudy Stack - MLT Table Review장주연Ainda não há avaliações
- Clinical Microscopy ExamDocumento3 páginasClinical Microscopy ExamKarla GiorlaAinda não há avaliações
- Gel TechnologyDocumento2 páginasGel TechnologyJai Carungay100% (1)
- Coombs TestDocumento15 páginasCoombs TestFatema AminAinda não há avaliações
- Immunohematology-Unit 1 Exam: Please Provide The Correct AnswerDocumento11 páginasImmunohematology-Unit 1 Exam: Please Provide The Correct AnswerchavelAinda não há avaliações
- Antibody IdentificationDocumento74 páginasAntibody IdentificationNilver Zenteno100% (3)
- MUST To KNOW in Blood Banking 1Documento19 páginasMUST To KNOW in Blood Banking 1Aya Virtucio100% (1)
- Immunology and Serology TestsDocumento2 páginasImmunology and Serology TestsPearlregine Cianne MirandaAinda não há avaliações
- Immunohematology Review ASCLSGA 2015 PDFDocumento49 páginasImmunohematology Review ASCLSGA 2015 PDFSheanalene CastroAinda não há avaliações
- CLINICAL CHEMISTRY - Specimen CollectionDocumento4 páginasCLINICAL CHEMISTRY - Specimen CollectionthedarkwingAinda não há avaliações
- Transfusion TherapyDocumento14 páginasTransfusion TherapyCMLAinda não há avaliações
- Hematology 2Documento89 páginasHematology 2Marie Llanes100% (1)
- ABO Blood Group System RH Blood Group SystemDocumento2 páginasABO Blood Group System RH Blood Group SystemDannie Desaca100% (1)
- Group 6 - Immunohematology - Blood BankingDocumento8 páginasGroup 6 - Immunohematology - Blood Bankingjulo_05Ainda não há avaliações
- ABO Blood Group SystemDocumento117 páginasABO Blood Group SystemShemiza BalmacoonAinda não há avaliações
- COMPLETE BLOOD COUNT Lecture GuideDocumento9 páginasCOMPLETE BLOOD COUNT Lecture GuideKaycee Gretz LorescaAinda não há avaliações
- Blood Bank QuizDocumento13 páginasBlood Bank Quizdimalawang.af100% (1)
- Immunohematology NotesDocumento1 páginaImmunohematology NotesAlyanna BaldoquinAinda não há avaliações
- Blood Banking: Donor ScreeningDocumento16 páginasBlood Banking: Donor ScreeningNikka Ong100% (2)
- Agglutination, Complement, Neutralization, and Inhibition: Methods in Immunology and Immunochemistry, Vol. 4No EverandAgglutination, Complement, Neutralization, and Inhibition: Methods in Immunology and Immunochemistry, Vol. 4Ainda não há avaliações
- Approach To Patients With Motor and Sensory Disorder 3-2012Documento7 páginasApproach To Patients With Motor and Sensory Disorder 3-2012dtimtimanAinda não há avaliações
- Factors That Affect LaborDocumento9 páginasFactors That Affect LabordtimtimanAinda não há avaliações
- Eating, Elimination and Impulse Control DisordersDocumento4 páginasEating, Elimination and Impulse Control DisordersdtimtimanAinda não há avaliações
- Basic Approaches in Clinical Practice Guideline DevelopmentDocumento11 páginasBasic Approaches in Clinical Practice Guideline DevelopmentdtimtimanAinda não há avaliações
- Behavior by Dra PacificoDocumento6 páginasBehavior by Dra PacificodtimtimanAinda não há avaliações
- Affective Disorders and SuicideDocumento5 páginasAffective Disorders and SuicidedtimtimanAinda não há avaliações
- Addendum To Epidemic Investigation 2 NotesDocumento2 páginasAddendum To Epidemic Investigation 2 NotesAna Cristina MontillanoAinda não há avaliações
- Epidemic Investigation 2Documento3 páginasEpidemic Investigation 2Ana Cristina MontillanoAinda não há avaliações
- Endocrine HistologyDocumento21 páginasEndocrine HistologydtimtimanAinda não há avaliações
- Answer Key Pedia 1st Evals 2011-2012Documento1 páginaAnswer Key Pedia 1st Evals 2011-2012dtimtimanAinda não há avaliações
- Pediatrics Evals 1, SY 11-12Documento4 páginasPediatrics Evals 1, SY 11-12dtimtimanAinda não há avaliações
- 2012-01-MEDICINE-Cardinal Manifestation of Renal DiseaseDocumento15 páginas2012-01-MEDICINE-Cardinal Manifestation of Renal Diseasedtimtiman100% (1)
- Food Poisoning TableDocumento1 páginaFood Poisoning TabledtimtimanAinda não há avaliações
- Bacteria Associated With GIT 3 FOOD POISONINGDocumento5 páginasBacteria Associated With GIT 3 FOOD POISONINGdtimtimanAinda não há avaliações
- Dyspnea and HypoxiaDocumento9 páginasDyspnea and Hypoxiadtimtiman100% (3)
- Skills in CV1Documento7 páginasSkills in CV1dtimtimanAinda não há avaliações
- 2011 11 PHARMA GIT Anti Diarrhea and Pro KineticDocumento5 páginas2011 11 PHARMA GIT Anti Diarrhea and Pro KineticdtimtimanAinda não há avaliações
- Intestinal Parasitism: ProtozoansDocumento10 páginasIntestinal Parasitism: ProtozoansdtimtimanAinda não há avaliações
- 2011-11-PHARMA-GIT-antidiarrhea and Prokinetic-TableDocumento3 páginas2011-11-PHARMA-GIT-antidiarrhea and Prokinetic-TabledtimtimanAinda não há avaliações
- 2011-11-PATHO-Dses of Small and Large IntestineDocumento9 páginas2011-11-PATHO-Dses of Small and Large IntestinedtimtimanAinda não há avaliações
- Commed Research Design1Documento6 páginasCommed Research Design1Hedley ChuaAinda não há avaliações
- Macrolides Ketolides Chloram Oxazolinodines StreptogamisDocumento6 páginasMacrolides Ketolides Chloram Oxazolinodines StreptogamisdtimtimanAinda não há avaliações
- 2011-08-PATHO-WBC Disorder 01 and 02Documento30 páginas2011-08-PATHO-WBC Disorder 01 and 02dtimtimanAinda não há avaliações
- CP Blood CoagulationDocumento14 páginasCP Blood CoagulationdtimtimanAinda não há avaliações
- Project Proposal AttachmentDocumento2 páginasProject Proposal AttachmentdtimtimanAinda não há avaliações
- Commed Research Design 2Documento6 páginasCommed Research Design 2ninjaningAinda não há avaliações
- Site MapDocumento2 páginasSite MapdtimtimanAinda não há avaliações
- Flow of Events and BudgetDocumento4 páginasFlow of Events and BudgetdtimtimanAinda não há avaliações
- Orphanage Project ProposalDocumento3 páginasOrphanage Project ProposaldtimtimanAinda não há avaliações
- Chest and Lungs 1Documento6 páginasChest and Lungs 1dtimtimanAinda não há avaliações
- Blood Grouping Catalog 2022Documento8 páginasBlood Grouping Catalog 2022Nas simaAinda não há avaliações
- BookDocumento248 páginasBookMostafa GabrAinda não há avaliações
- Cotton Diseases Handout EnglishDocumento6 páginasCotton Diseases Handout Englishusama_yasinAinda não há avaliações
- DeGowin's Diagnostic Examination (8th Ed)Documento306 páginasDeGowin's Diagnostic Examination (8th Ed)Farah Syazana100% (1)
- The Ore Exam1191Documento17 páginasThe Ore Exam1191hard02Ainda não há avaliações
- PDD BSC MLS 2022 Cohort 2023013Documento177 páginasPDD BSC MLS 2022 Cohort 2023013yoyowong512Ainda não há avaliações
- Blood Case 6Documento12 páginasBlood Case 6إنعام الحفيانAinda não há avaliações
- Medicolegal DeathDocumento13 páginasMedicolegal DeathWASIF ISMAILAinda não há avaliações
- Death PathologyDocumento80 páginasDeath PathologyAlex GasnasAinda não há avaliações
- Dermatopathology For The Surgical Pathologist A Pattern-Based Approach To The Diagnosis of Inflammatory Skin Disorders Part IDocumento21 páginasDermatopathology For The Surgical Pathologist A Pattern-Based Approach To The Diagnosis of Inflammatory Skin Disorders Part IkarigargiuloAinda não há avaliações
- 01introduction To PathologyDocumento71 páginas01introduction To PathologyAishwarya PanchalAinda não há avaliações
- Wa0012Documento1 páginaWa0012Nice BennyAinda não há avaliações
- Adenocarcinoma Article 2021Documento7 páginasAdenocarcinoma Article 2021Bapai MallikAinda não há avaliações
- CCEB Exam Content July 2013Documento24 páginasCCEB Exam Content July 2013StarLink1Ainda não há avaliações
- PG Deemed CollegesDocumento53 páginasPG Deemed CollegesAvi KhannaAinda não há avaliações
- Practical Medical MicrobiologyDocumento12 páginasPractical Medical MicrobiologyAli RazaAinda não há avaliações
- CHC Jawa Hub: Jawa, Rewa, Madhya Pradesh Rewa Madhya Pradesh - 486223 Phone No.Documento2 páginasCHC Jawa Hub: Jawa, Rewa, Madhya Pradesh Rewa Madhya Pradesh - 486223 Phone No.MAHESH GAUTAMAinda não há avaliações
- Host-Pathogen Interaction PDFDocumento11 páginasHost-Pathogen Interaction PDFSafira Najwa ElzamAinda não há avaliações
- 1514456610Syllabus-CMS and EDDocumento5 páginas1514456610Syllabus-CMS and EDUnderstanding HomoeopathyAinda não há avaliações
- Job Descriptions Roles and ResponsibilitiesDocumento7 páginasJob Descriptions Roles and ResponsibilitiesASHOK KUMAR LENKAAinda não há avaliações
- Kavita Sahay Blood GroupDocumento1 páginaKavita Sahay Blood GroupKrishna GowdaAinda não há avaliações
- C1 IH Lab L3 ABO Forward Reverse Typing Manual and Gel MethodDocumento8 páginasC1 IH Lab L3 ABO Forward Reverse Typing Manual and Gel MethodDIVINA KYLE YGOAinda não há avaliações
- Microscope History - Pre-Achromatic MicroscopesDocumento3 páginasMicroscope History - Pre-Achromatic MicroscopesArturoAinda não há avaliações
- Introduction To Medical MicrobiologyDocumento60 páginasIntroduction To Medical Microbiologytummalapalli venkateswara rao100% (1)
- Jurnal Parotis2Documento5 páginasJurnal Parotis2AstridApriliaSimanjuntakAinda não há avaliações
- 2021 Hawaii Physician Workforce AssessmentDocumento44 páginas2021 Hawaii Physician Workforce AssessmentHPR NewsAinda não há avaliações
- NOTES HospitalDocumento21 páginasNOTES HospitalMahendar SankhalaAinda não há avaliações