Escolar Documentos
Profissional Documentos
Cultura Documentos
OB Nursing Ma'Am Pacabis
Enviado por
Argee AlonsabeDireitos autorais
Formatos disponíveis
Compartilhar este documento
Compartilhar ou incorporar documento
Você considera este documento útil?
Este conteúdo é inapropriado?
Denunciar este documentoDireitos autorais:
Formatos disponíveis
OB Nursing Ma'Am Pacabis
Enviado por
Argee AlonsabeDireitos autorais:
Formatos disponíveis
OB 1
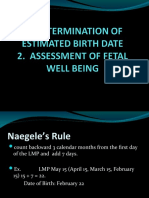
OB Pacabis Pregnancy Days: 260-290 days (Average 280 days!) Weeks: 38-42 weeks (Average 40 weeks) Months: 9 months Lunar: 10 lunar months L and D Puerperium: as early as 6 but not later than 8 weeks
MCN Womens Health Perinatal Nursing fetal and neonatal care
What is the approximate length of a termed fetus? Haeses Rule: Determine the length fetus using lunar months 1-5 lunar months: AOG2 6-10 lunar months: X 5
Stages of Labor Stage 1: Cervical Dilatiion Stage 2: Fetal Expulsion Stage 3: Placental stage 20 hours cut off time for dystocia
Assessment OB Clients: Fetus and Mother! IPPA + Interview Fetal Health Indicators 1. FHR (120-160bpm) 2. Fetal Movement (Starting 20 weeks, grandmultigravida 16-18 weeks); daily fetal movement (10! 1 Every 2 hours!); 20 minutes after meals; danger sign if 3 times in 8 hours! Factors in Labor 1. Power 2. Passage Soft Cervical canal Vagina Hard Pelvis (4 Bones) 2 innominate bone (Ileum biggest, ischium lowermost of the pelvis, pubis anterior), 1 sacrum, 1 coccyx Gynecoid (round) and Anthropoid (Oval) can deliver normally Android (heart shaped) and Platypelloid (flat) abnormal!
OB 2
Inlet shape of the pelvis Diagonal Conjugate can be clinically measured through I/E (11.5cm) OB conjugate most important (narrowest diameter of inlet); cannot be measure, can be estimated by subtracting from the diagonal conjugate (Diagonal conjugate -1.5 to 2cm) = OB conjugate (10cm) complete flexion is important in order for the fetus to pass! Anatomical conjugate 11cm (1cm bigger than OB) Inlet Contraction Mid Pelvis ischial spine Bispinous diameter distance between ischial spines (10cm) ~ most common in CPD Outlet tuberosities 11cm AP Diameter symphysis pubis to the sacrum Transverse Diameter (12.75-13cm)- where fetal head engages
3. Passenger Fetus Attitude Complete Flexion Partial Flexion Partially extended Fully extended 4. Psyche
Presenting Part Vertex Military Brow Face
Presentation Occiput Bregma Brow Chin/Mentum
Position SOB OF MO SMB
Diameter 9.5cm 11cm 13.5cm 9.5cm
Reproductive Process All women must ovulate If no sperm, the woman must also be able to menstruate If there is sperm, the woman must be able to get pregnant o Fertilization phase o Implantation phase
Child Bearing Age 15 years (standard) to 44 (49 years old: Family Planning International ) 45 beginning of menopause: if she has 12 missed cycles, ends at 55 years old
Ideal Reproductive Age 18-35 years old Have its lowest complications if within this range
Ovary Estrogen hormone of being a woman Progesterone hormone of pregnancy Relaxin
OB 3
Fallopian tube Uterus Fundus Corpus Cervix Layers o Endometrium o Myometrium o Perimetrium For gestation and menstruation Isthmus Ampulla (site of fertilization) Infundibulum widest part
Oral Contraceptive Pills DPV Implant (Norplant) Patch Method
Suppresses ovulation by increasing estrogen and progesterone dec FSH and LH; systemic effect, C/I to cardio, liver disorders. Complaints: headache, chest pain, weight gain
Tubal Ligation Permanent (but can recanulate) Prevents fertilization
IUD (CuT380A) Good for 10 years Copper because it kills the sperm Prevents implantation May cause cramps and menorrhagia
Diaphragm Covers cervix Inserted by the woman Does not allow sperm to enter prevents fertilization
Cervical Mucus Method (Billings Method) LAM No ovulation Higher prolactin, lower the progesterone Testing for spinbarkeit characteristics of mucus
*Inc HPL, low Insulin
Ovulation
OB 4
1. 2. 3. 4.
Each ovary will ovulate alternately Starts during menarche (12 years) Release of an egg from menarche to menopause Ovulation occurs 14 days before the next menstruation E.g. April 29-14 = April 15 ~ date of ovulation
Menstruation Brain Hypothalamus GRH FSH and LH APG will release FSH (matures follicles)in the ovary ovary releases estrogen Estrogen develops ducts of breast (breast tenderness); uterus (proliferates endometrium); cervix (Spinbarkeit 8-10cm); Uterus contracts the uterus; proliferative phase! Progesterone relaxes smooth muscles; acts on the breasts Acini cells for BF; thick mucus secretions in the cervix (mucus plug); secretory phase! Implantation phase usually occurs in this phase (Decidua if pregnant) Hormone of ovulation LH Birth 2M Puberty 400K Adults 30K Menopause 0 Ovary Uterus
Menstruation 28 days Duration: 1-9 days (average is 3-5 days) Women One Mature 23 chromosomes X Men Millions Mature/Immature (average 60 days to mature) 23 chromosomes X or Y
Sperm 100M/cc; normal ejaculation is 3-5cc = 300M-500M; should not go <20M/mL=60-100M; if less 20M, low sperm count
Fallopian tube to uterus in 3-4 days; implants in 3-4 days Fertilization to Implantation zygote Implantation to 7 weeks embryo 8 weeks to birth fetus
OB 5
Morulla travelling zygote of the fallopian tube; blastocyst implanting zygote Germ Layer where organs are formed Inner cell mass Amnion and fetus OCM trophoblast (secretes HCG) sustains the pregnancy before the placenta by maintaining the corpus luteum (Effects: N and V, + pregnancy test) Placenta from the decidua basalis; functions at the end of the 12 th weeks! Develops as early as 2 months
4 Weeks heart begins to beath 6-7 Weeks UTZ can show + sign of pregnancy (confirms pregnancy, ages the pregnancy, tells the location of pregnancy) 8 weeks, all major organs are formed 10-12 weeks Doppler can be used for FHR; placental functioning fetal circulation; amniotic fluid develops; fetus voids 12 weeks suck and swallow 12-16 weeks sex can be seen 20 weeks age of viability: FHB, Fetal Movement; Vernix, Lanugo 24 weeks fetal lungs begin to secrete surfactant 32 weeks testes begin to descend 36 weeks presentation is definite (cephalic, breech, shoulder) 38 weeks baby is term
20 weeks 500g Term baby 2500g (5.5lbs) 4000g (4kg) LGA (8.8lbs) Average 3000g (6.6lbs)
Parts of the Placenta 1. 2. Cotyledons Found in the maternal parts Attached to decidua basalis N: 27-30 cotyledons Membrane Fetal side Amnion (clear transparent) and Chorion (thicker, manually removed) components of BOW
Functions of the Placenta Respiratory function fetal circulation (veins carry oxygen)
OB 6
FO DA PDA(Indomethacin) DV No liver and lung circulation Nutritive function Endocrine Excretory Barrier (except viruses)
Amniotic Fluid: 1000mL inc as the baby becomes more mature; decreases once in term; clear with specks of vernix and lanugo pH: alkaline Nitrasine test to differentiate urine from amniotic fluid (blue) Alkaline vagina pruritus
Prenatal Visit 1-7 months monthly 8 q2weeks 9 q week
Integrated Management of Pregnancy and Childbirth Skilled birth attendant at primary level 10-11g of Hb ok (1 tab of Fe) If 7-9g moderately anemic (2tab) <7g severely anemic (2tab) 30-60mg/tablet Folic acid 400mg
Labor Duration increases Freq and Interval decreases FHB Early deceleration normal (HR reduces when contracting) Late deceleration pathologic, uteroplacental insufficiency Variable deceleration cord compression Position Oxygenation 5lpm Refer
OB 7
Leopolds Maneuver LM1 presentation of the fetus presenting part LM2 position of the fetus LM3 confirm LM1 and engagement LM4 Pawlicks grip fetal attitude ROA/LMA 1. 2. 3. 4. 5. 6. 7. 8. Presentation Presenting part Lie Attitude Presenting diameter Measurement of FD FHB Turn Ext Rotation
Reva Rubin Psychologist of Pregnancy
Assessment Data PX Height (<5ft High risk for CPD) Weight high risk for preeclampsia (rapid increase will inc possible preeclampsia) Cephalocaudal Eye conjunctiva (anemia) Teeth infection (streptococcal infection) Neck thyroid Breast nipples (overted, inverted and protruding) Fundic height Primigravida 2 weeks before EDC lightening Vulva any discharge Clear (Mucoidal) Any discoloration pathologic, curd like (fungi), frothy, creamy, greenish (trichomonas), foul, gray (GABS), milky (bacteria) PID ectopic pregnancy and sterility Varicosities Edema Warts Extremities varicosities and edema Lab
OB 8
Health Education Hygiene of Pregnancy Danger Signs Teratogens Infections Chemicals Drugs Smoking (SGA), Alcohol (Mental Retardation, IUGR, facial defects), Caffeine (mother is hyperstimulated) Radiation Exercises Kegels Pelvic Rocking Tailor Sitting Walking Minor Discomforts Varicosities avoid prolonged standing, Leg cramps adequate Ca intake (milk); dorsiflex the foot and massage Constipation high fiber
Nutrition RDA 2200kcal/day; add 300 for pregnant; 500 if lactating Fe: 1 tab CHON: 60-75 grams Ca: 1200mg/day Folic acid: 400-600mcg
Fe: 1g total pregnancy (500mgmother, 300mgfetus and placenta, 200mg blood loss)
Fetal Well Being Fetal Heart Rate UTZ (6-7 weeks) 120-160bpm APGAR 100 and above 2
Daily Fetal Movement
OB 9
28 weeks above Quickening (16 weeks, 20 weeks to majority of women) Kick chart
Non Stress Test Evaluating the FHR vs. Fetal Movement HR inc as the fetus moves HR inc at least 15 beats that will last for 15 seconds If does not accelerate abnormal N: Reactive
Contraction Stress Test FHR vs. UC Decelerations are expected N: Negative
Biophysical Profile FHR F movement F Tone N is fisted hand Respiratory Breathing movements Amniotic Fluid Volume N is 800-1000cc 10 perfect, N is 8-10, <6 Abnormal Done by UTZ
Amniocentesis 1st trimester chromosomal effects 2nd trimester lung maturity o LS Ratio 2:1 higher the lecithin more mature (performed more often in DM mother) DM Mothers Macrosomnia (8lbs above) 37-38 weeks, induct labor, to extract baby at the lowest possible weight (considering the lung maturity) CPD and Fetal Distress most common indication for CS Chorionic Villa Sampling Cordocentesis To evaluate chromosomal aberrations
Congenital Anomaly Scan 20 weeks and above
Labor series of process by which the products of conception are expelled from the uterus
True vs. False Labor Inc duration Regular pains Pain that come from the back and to the front Cervical changes (MAJOR SIGN)
Inc BHC False labor true labor
OB 10
Theory of Labor Estrogen placenta Progesterone placenta; relaxes smooth muscles (withdraws when labor starts) Oxytocin PPG Prostaglandin Decidua (specialized endometrium of pregnancy) Corticosteroid from fetal adrenals; initiates secretion of oxytocin from brain Relaxin placenta
Factors Powers forces that expel products of conceptions Passage hard and soft Passengers each may cause dystocia Fetus size, presentation, gross congenital anomaly (e.g. hydrocephalus) Placenta previa, abruptio, accreta (pregnancies every year! grandmultigravida!) Succenturiata, Circumvallata, Velamentous insertion of cord Amniotic Fluid Poly overdistention (may cause uterine atony) If yellowish chorioamnionitis if there is PROM! BOW transitional to second stage of labor! Membranes (Amnion and Chorion usually left) Cord length is as long as the fetus (50-55cm) Whartons jelly whitish, bluish; if brownish/greenish distress Inspect AVA (if one is absent, congenital anomalies) Cord Loops we can untangle Prolapse of the cord position Position best LOA, a mobile mother!
Stages of Labor First Stage (Cervical Dilatation) Latent 0-3 Mother is very congenial, establish IPR, reinforce teachings given at prenatal (Breathing exercises), mother is receptive at this point
OB 11
Nutrition community setting (food), Hospital (normal nourishment, light CHO diet soups, hot milk) Upright position, mother should be mobile (enhances descent of fetus) Let the mother walk around or comfortable position BOW (+) Active 4-7 Mother feels true pain! 4cm is critical; pain management
Transitional 8-10 Assist mother to take control of situation
Elimination bladder distention may prevent descent Monitor progress of labor check the uterine contraction, cervical dilation (R.A. 9173, mother is in labor, no antenatal bleeding; Suturing suture perineal laceration) Vaginal Exam q4h Primi 1.2cm/h Multi 1.5cm/h (minimum) 2-3cm/h *1cm/1hrD Precipitate Labor labor that lasts 3 hours or less precipitate delivery (grandmultiparities! Oxytocin drips, analgesia) Mother (laceration), Fetus (Brain damage/intracranial hemorrhage); Amniotic fluid embolism (cyanosis, DOB, chest pain, cough give O2 call MD) FHR
st
1 2nd
LR Q30 Q15
HR Q15 Q5
Pain Management Non Pharmacologic - Breathing exercises (breath deeply during contraction; pant and breath transitional ) - Massage effleurage - Hydrotherapy (warm baths, whirlpool) Pharmacologic - Meperidine HCl (Respi Dep) - Nalbuphine (Respi Dep) - Butorphanol (Stradul) - Epidural Anesthesia (Hydrate the patient! S/E is hypotension)
2nd Stage Engagement Primi 2 weeks before EDC; lightening occurs that lightening occurs 2 weeks EDC Multi any time during labor! Descent occurs throughout labor Flexion assumes smallest diameter (SOB smallest diameter)
OB 12
Internal Rotation Crowning Ritgens extends fetal head Extension External Rotation Expulsion
Crowning biggest diameter is in introitus
Active Management of the Third Stage Shortened third stage Preventing bleeding As soon as baby is out, inject Oxytocin contract uterus Calkins sign, thus placental separation
BEMONC Functions: RM, RN, MD primary birth setting (Lying-in, Birthing centers, clinics) Number 1 resource: Blood more than 100mL during placental stage 1 bag of Blood (CEMONC facility)
Patient Median Attendant Mediolateral
Blood transfusion and CS CEMONC (2ndary District Hospital)
Signs of Placental Separation 1. Calkins Sign 2. Gushing of blood 3. Lengthening of cord
Placental Stage Placental Separation 1. Schultz inverted umbrella 2. Duncan Placental Expulsion Brandt Andrews Calkins /Modified Credes Maneuvre
Oxytocics
OB 13
Hormonal oxytocin, pitocin, Syntocinon (dec BP) rhythmic IM, IV Push, IVF IU; 10u/amp; do not exceed 3 liters with 3 amps of hormonal (may not contract!) Herbal methergin, ergotrate, ergonovine maleate (inc BP) sustained action Oral, IM, IV push, never IVF! .2mg never give more than 1 mg (may cause rupture)
4th Stage of Labor: 1-4 hours Vigilance of the mother right after labor Uterus immediately after birth, below the navel, next few hours will rise at the level of navel If above the navel boggy uterus massage/ice dislodge clots Ten days, return to normal uterine size, if subinvolution may be caused by infection Vaginal bleeding Bleeding vaginal pad soaked in 1 hour, heavy bleeding Laceration ice pack in 24 hours, heat after 24 hours First Degree forche, mucosa Second Degree 1st degree + muscles Third Degree 1st, 2nd and anus Fourth Degree 1st, 2nd, 3rd rectum
Vital signs q15min x 4 hours; q30min x 2hours; if stable discharge, take q4h x 24 hour; q8h then discharge Laceration/Episiotomy
Breast RA 7600; EO 51 Gavage/NGT/Dropper/Cup/Human Milk Bank (give within 24 hours, frozen 3-6 months) 3rd to 4th day, post partum, engorgement of breast increase of temperature Uterus Involution; after pains oxytocin (let down reflex hormone) myoepithelial cell of breast (more frequent after pains) Bladder Difficulty of voiding edematous perineum and urethral sphincter Assess distention Bowel 2nd to 3rd days Lochia Emotionality Post partum blues (withdrawal of hormones blues)
OB 14
Important: support of significant others Post partum depression Post partum psychosis Manic Skin Chloasma, linea nigra, striae (silvery) Homans Sign Thromboembolic disease Post partum infection any elevation of temperature above 38 degrees that occurs twice within 10 days after birth UTI most common post partum infection
3 Classic Causes of Maternal Death Bleeding HPN Infection Obstructed Labor Unsafe Abortion Drugs Massage Inserting catheter into vulva and probing
Phil MMR 160-162/100000 7-11 daily
Pregnancy
Bleeding Abortion Ectopic H Mole Previa/Abruptio Atony, wounds, placental problems
HPN CHVD PEM Preeclampsia mild PES Preeclampsia severe
Infections TORCH UTI Moriliasis
Others DM, heart disease, multiple gestation, polyhydramnios Preterm labor Dystocia (power, passage, passenger)
Labor and Delivery
Eclampsia Post partum Atony (number 1 killer in 24 hours) Retained Secundings
PROM Frequent Vaginal Exam Wounds Endometritis Wound infections (DM Mothers) Thrombophlebitis Mastitis
Post partum blues psychosis
Pre eclampsia 200 weeks
OB 15
Define Cause Characteristic Signs Management
Abortion termination of pregnancy before the age of viability 1. Spontaneous (Miscarriage) Cervix BOW a. Threatened Closed + Spotting Rest (Physical, Emotional, Sexual) Duvadilan/Duphaston relaxing drugs (non teratogenic) Avoid sex b. Inevitable Open Imminent Abortion c. Incomplete Open d. Habitual Open + 3 or more successive abortions Incompetent cervix cerclage e. Missed Close The fetus has been dead for at least 2 weeks and the mother is not aware; uterus is smaller than AOG; secretion of brownish secretions; Pregnancy Test: (-), no more HCG Mgt: i. Cytotec (misoprostol)/Laminaria/Prostaglandin gel ii. Induce labor (D5LR + 1amp oxytocin) expel the dead fetus; D and C after Causes: o Stress o Infection o Chronic diseases of mother (DM) o Chromosomal effects (non modifiable) 2. Induced a. Therapeutic b. Illegal/Criminal
Ectopic Pregnancy Sharp knifelike abdominal pain radiating to the shoulder Ruptured dull pain in the left or right Surgical Salphingostomy Salphingectomy
Medical Methotrexate pregnancy must not be more than 2 months; fetus should not be longer than 4cm; no heart rate;
H Mole Abnormal zygote
OB 16
Complete More bleeding An empty ovum penetrated by 1 sperm (23 chromosomes) Rapidly enlarging uterus with soft and no FHR
Partial Normal ovum with 23 chromosomes fertilized by 2 sperms (69 chromosomes)
Rapidly enlarging uterus with faint FHR 15-16-18 weeks
May lead to choriocarcinoma No pregnancy for 1 years Monitor for HCG Small doses of Methotrexate 2x (-) HCG, pregnancy is allowed
Você também pode gostar
- Maternity Study GuideDocumento43 páginasMaternity Study Guidepgmanski100% (23)
- Avery's Neonatology PDFDocumento3.845 páginasAvery's Neonatology PDFviaviatan100% (3)
- Fetal Growth Retardation Assessment and Placental InsufficiencyDocumento39 páginasFetal Growth Retardation Assessment and Placental InsufficiencyslyfoxkittyAinda não há avaliações
- OB Study GuideDocumento43 páginasOB Study Guidelilchibaby3161100% (1)
- ATI Maternal Newborn Proctored Study Guide (2018)Documento8 páginasATI Maternal Newborn Proctored Study Guide (2018)Emma Lilly100% (6)
- Perioperative Nursing ConceptDocumento21 páginasPerioperative Nursing ConceptArgee Alonsabe100% (8)
- Curative and Rehabilitative Nursing Care Management of Clients in Acute Biologic CrisisDocumento44 páginasCurative and Rehabilitative Nursing Care Management of Clients in Acute Biologic CrisisArgee AlonsabeAinda não há avaliações
- Acog Practice Bullet In: Neural Tube DefectsDocumento12 páginasAcog Practice Bullet In: Neural Tube DefectsSILVIA GAONAAinda não há avaliações
- MCNP Integrated Concepts NP 2Documento9 páginasMCNP Integrated Concepts NP 2Karen Mae Santiago Alcantara100% (1)
- BFM 800Documento57 páginasBFM 800Sebastian Samolewski100% (1)
- Birth Asphyxia and Cerebral Palsy: Understanding the PathophysiologyDocumento16 páginasBirth Asphyxia and Cerebral Palsy: Understanding the PathophysiologySebastián Silva SotoAinda não há avaliações
- AntepartalDocumento43 páginasAntepartalxing414Ainda não há avaliações
- 4 ProcessDocumento12 páginas4 ProcessTel EscorialAinda não há avaliações
- Walang Kwentang NotesDocumento107 páginasWalang Kwentang NotesAnonymousTargetAinda não há avaliações
- Midterm FetalDocumento4 páginasMidterm FetalRizalyn Padua ReyAinda não há avaliações
- LaborDocumento45 páginasLaborDakayu Amin LugitAinda não há avaliações
- Ante Natal Care: by Naveen Sharma J.N - Medical College Belgaum, IndiaDocumento37 páginasAnte Natal Care: by Naveen Sharma J.N - Medical College Belgaum, IndiaNaveen SharmaAinda não há avaliações
- Revised OB Handout Part 1 MAY 2023 PNLE RefresherDocumento15 páginasRevised OB Handout Part 1 MAY 2023 PNLE RefresherMatelyn OargaAinda não há avaliações
- Clinical Activities: A. Pre - ConsultationDocumento13 páginasClinical Activities: A. Pre - ConsultationerykafadsAinda não há avaliações
- Intrapartum QuizletDocumento15 páginasIntrapartum Quizletanon_616227840100% (3)
- LaborDocumento25 páginasLaborSameera DahamAinda não há avaliações
- Primary ObstetricsDocumento62 páginasPrimary ObstetricsGill Bulanan - PeñaAinda não há avaliações
- Normal LaborDocumento33 páginasNormal Laboreric100% (1)
- OB RNSG 2208 Mid-term OutlineDocumento23 páginasOB RNSG 2208 Mid-term OutlineAnnissaLarnardAinda não há avaliações
- Obgyn Revalida Review 2022 RcsDocumento248 páginasObgyn Revalida Review 2022 RcsSophia SaquilayanAinda não há avaliações
- Maternal and Child Health IDocumento772 páginasMaternal and Child Health Ikarendelarosa06100% (6)
- C. Care and Management of Intrapartum WomanDocumento86 páginasC. Care and Management of Intrapartum WomanKeziah TampusAinda não há avaliações
- NCM 107 - MATERNAL & CHILD HEALTH NURSING 1st SEMESTER MIDTERM REVIEWERDocumento4 páginasNCM 107 - MATERNAL & CHILD HEALTH NURSING 1st SEMESTER MIDTERM REVIEWERskoolrkiveAinda não há avaliações
- Maternity Nursing TermsDocumento7 páginasMaternity Nursing TermsBernardMarkMateoAinda não há avaliações
- Ob Ati StudyDocumento22 páginasOb Ati Studylpirman0580% (5)
- MCN Lec Reviewer FinalsDocumento7 páginasMCN Lec Reviewer Finalszyyw.abello.uiAinda não há avaliações
- Ultrasound: Assessment of Fetal Well-BeingDocumento11 páginasUltrasound: Assessment of Fetal Well-Beingsafira ainunAinda não há avaliações
- ASSESSMENT OF FETAL GROWTH AND DEVELOPMENTDocumento84 páginasASSESSMENT OF FETAL GROWTH AND DEVELOPMENTAlessandra Franchesca CortezAinda não há avaliações
- Labor & DeliveryDocumento14 páginasLabor & DeliveryNiña Eleana FranciscoAinda não há avaliações
- MidtermsDocumento12 páginasMidtermsMarga PalomaAinda não há avaliações
- Care of Mother and Adolescent Well Client RLE Skills Lab ReviewerGonzalesDocumento22 páginasCare of Mother and Adolescent Well Client RLE Skills Lab ReviewerGonzalesKarl LintanAinda não há avaliações
- Human Fetal Period-A General SurveyDocumento42 páginasHuman Fetal Period-A General Surveyg_muhammadusmanAinda não há avaliações
- Institute of Nursing Intrapartum Care Handouts: Labor and Delivery Theories of Labor OnsetDocumento7 páginasInstitute of Nursing Intrapartum Care Handouts: Labor and Delivery Theories of Labor OnsetTimi BCAinda não há avaliações
- Assessment of Fetal Well BeingDocumento29 páginasAssessment of Fetal Well Beingmalaika khanAinda não há avaliações
- Perub Fisik Saat KehamilanDocumento66 páginasPerub Fisik Saat KehamilanrismaAinda não há avaliações
- ObstetricsDocumento6 páginasObstetricsanonymousAinda não há avaliações
- First 6 Weeks Pregnancy Hormones Physiological ChangesDocumento4 páginasFirst 6 Weeks Pregnancy Hormones Physiological ChangesRojales FrancisAinda não há avaliações
- Assessment of Fetal WellbeingDocumento177 páginasAssessment of Fetal Wellbeingvrutipatel100% (1)
- Pregnancy Diagnosis: Peng Xuebing, M.D. Dept of Obs/Gyn Beijing Fu Xing Hospital Capital Medical UniversityDocumento48 páginasPregnancy Diagnosis: Peng Xuebing, M.D. Dept of Obs/Gyn Beijing Fu Xing Hospital Capital Medical UniversityAhmed TarigAinda não há avaliações
- Diagnosing PregnancyDocumento44 páginasDiagnosing PregnancyJisha SinghAinda não há avaliações
- CHAPTER 8 LABOR and DELIVERYDocumento85 páginasCHAPTER 8 LABOR and DELIVERYBardiaga JmayAinda não há avaliações
- 3amali S9Documento34 páginas3amali S9Arsh KaiwanAinda não há avaliações
- Dec2012nletips MCHN 121021230343 Phpapp01 PDFDocumento7 páginasDec2012nletips MCHN 121021230343 Phpapp01 PDFJessamine Rochelle Reyes EsbertoAinda não há avaliações
- OB Exam 2Documento14 páginasOB Exam 2Katie GermanAinda não há avaliações
- Pregnancy Confirmation and ChangesDocumento37 páginasPregnancy Confirmation and Changesana aurea aquino de leonAinda não há avaliações
- Understanding the Partograph for Monitoring LaborDocumento14 páginasUnderstanding the Partograph for Monitoring Labornaomie manaliliAinda não há avaliações
- OBGYN Student Study GuideDocumento39 páginasOBGYN Student Study GuideGoffo13100% (4)
- History TakingDocumento26 páginasHistory TakingShauie CayabyabAinda não há avaliações
- Assessment of Fetal G&DDocumento75 páginasAssessment of Fetal G&DHillary Praise AquinoAinda não há avaliações
- Prenatal: Prepared byDocumento94 páginasPrenatal: Prepared byHelenAinda não há avaliações
- Lecturio 3041Documento17 páginasLecturio 3041Pranjali WeladiAinda não há avaliações
- Pregnancy DiagnosisDocumento28 páginasPregnancy Diagnosisamit vishenAinda não há avaliações
- MCN 1stweekDocumento4 páginasMCN 1stweekCrystal MaidenAinda não há avaliações
- RACE Annotated ObsDocumento35 páginasRACE Annotated ObsIsmath JahangirAinda não há avaliações
- Final MCNDocumento3 páginasFinal MCNKyla R. PinedaAinda não há avaliações
- Perkembangan Fetus Dr. Richardi., SP - OGDocumento43 páginasPerkembangan Fetus Dr. Richardi., SP - OGAray Al-AfiqahAinda não há avaliações
- What Goes On Inside Pregnant Mommy's Tummy? Big Ideas Explained Simply - Science Book for Elementary School | Children's Science Education booksNo EverandWhat Goes On Inside Pregnant Mommy's Tummy? Big Ideas Explained Simply - Science Book for Elementary School | Children's Science Education booksAinda não há avaliações
- How To Have an Easy and Safe Pregnancy and Bring Forth a Healthy Baby: A Pregnancy Book for First Time Moms for a Successful and Healthy Journey through Pregnancy, Childbirth and NewbornNo EverandHow To Have an Easy and Safe Pregnancy and Bring Forth a Healthy Baby: A Pregnancy Book for First Time Moms for a Successful and Healthy Journey through Pregnancy, Childbirth and NewbornAinda não há avaliações
- Mommy and Baby: Everything about pregnancy, birth and baby sleep!No EverandMommy and Baby: Everything about pregnancy, birth and baby sleep!Ainda não há avaliações
- Nursingbulletin Laws Affecting The Practice of NursingDocumento4 páginasNursingbulletin Laws Affecting The Practice of Nursingseigelystic100% (43)
- HAAD Antidote ListDocumento2 páginasHAAD Antidote Listashazainniz100% (5)
- Professional AdjustmentDocumento22 páginasProfessional AdjustmentArgee Alonsabe100% (1)
- Pedia NotesDocumento47 páginasPedia NotesArgee AlonsabeAinda não há avaliações
- Types of HypersensitivityDocumento1 páginaTypes of HypersensitivityArgee AlonsabeAinda não há avaliações
- Ortho LectureDocumento35 páginasOrtho LectureArgee AlonsabeAinda não há avaliações
- Respi NotesDocumento34 páginasRespi NotesArgee Alonsabe100% (1)
- EKG Self Study GuideDocumento40 páginasEKG Self Study GuideArgee AlonsabeAinda não há avaliações
- Ra 9173Documento12 páginasRa 9173Argee AlonsabeAinda não há avaliações
- NCM of Clients With Reproductive DisordersDocumento24 páginasNCM of Clients With Reproductive DisordersArgee AlonsabeAinda não há avaliações
- Nursing JurisprudenceDocumento1 páginaNursing JurisprudenceArgee AlonsabeAinda não há avaliações
- NCM HemaDocumento13 páginasNCM HemaArgee AlonsabeAinda não há avaliações
- NCM of Clients With Endocrine DisordersDocumento24 páginasNCM of Clients With Endocrine DisordersArgee Alonsabe100% (1)
- Maternal and Child Nursing From Tina CompleteDocumento51 páginasMaternal and Child Nursing From Tina CompleteArgee AlonsabeAinda não há avaliações
- NCM 202 GitDocumento24 páginasNCM 202 GitArgee AlonsabeAinda não há avaliações
- NCM CDDocumento25 páginasNCM CDArgee AlonsabeAinda não há avaliações
- Immunologic and Inflammatory NotesDocumento26 páginasImmunologic and Inflammatory NotesArgee AlonsabeAinda não há avaliações
- L and MDocumento26 páginasL and MArgee AlonsabeAinda não há avaliações
- Fluids and ElectrolytesDocumento27 páginasFluids and ElectrolytesArgee AlonsabeAinda não há avaliações
- Curative and Rehabilitative NCM of Client With Neurologic DisordersDocumento41 páginasCurative and Rehabilitative NCM of Client With Neurologic DisordersArgee AlonsabeAinda não há avaliações
- CardioDocumento24 páginasCardioArgee AlonsabeAinda não há avaliações
- Nursing Care Plan Placenta PreviaDocumento2 páginasNursing Care Plan Placenta PreviaApril Ann HortilanoAinda não há avaliações
- Chapter 10 Physiological Psychological Changes in PregnancyDocumento48 páginasChapter 10 Physiological Psychological Changes in PregnancyJeremiah Paul Gotia Humiwat100% (2)
- How Pandemics SpreadDocumento7 páginasHow Pandemics SpreadTấn NguyễnAinda não há avaliações
- Module 2 Physical and Motor Development of Children and AdolescentDocumento13 páginasModule 2 Physical and Motor Development of Children and Adolescentjaz bazAinda não há avaliações
- Antepartum Fetal EvaluationDocumento26 páginasAntepartum Fetal EvaluationNadiah F. HamkaAinda não há avaliações
- 4BI1 1BR Que 20201107Documento24 páginas4BI1 1BR Que 20201107Adeeba iqbal100% (5)
- ABNORMAL UTERINE BLEEDING EVALUATIONDocumento41 páginasABNORMAL UTERINE BLEEDING EVALUATIONShriyansh Chahar0% (1)
- Maternity Q&ADocumento30 páginasMaternity Q&AYasin JamalAinda não há avaliações
- Research Article For Soft ComputingDocumento19 páginasResearch Article For Soft ComputingManikandanAinda não há avaliações
- Hilaria Sas 8Documento3 páginasHilaria Sas 8Christy Mae Batucan HilariaAinda não há avaliações
- Management of Dystocia Due To Fetal Anasarca With Ascites and Hydrocephalus in A Cow: A Case ReportDocumento5 páginasManagement of Dystocia Due To Fetal Anasarca With Ascites and Hydrocephalus in A Cow: A Case ReportIndian Journal of Veterinary and Animal Sciences RAinda não há avaliações
- Uterine AnomaliesDocumento24 páginasUterine AnomaliesAnaAinda não há avaliações
- Fetal Circulation (For MBBS)Documento50 páginasFetal Circulation (For MBBS)Tashif100% (1)
- BAHASA INGGRIS LITERASI MENGURANGI RISIKO KEHAMILANDocumento6 páginasBAHASA INGGRIS LITERASI MENGURANGI RISIKO KEHAMILANHelmyHaikalAinda não há avaliações
- CS Case PresentationDocumento16 páginasCS Case PresentationjisooAinda não há avaliações
- Dystocia in Sheep and GoatsDocumento12 páginasDystocia in Sheep and GoatsgnpobsAinda não há avaliações
- UntitledDocumento18 páginasUntitledstuffednurseAinda não há avaliações
- Anatomy and Physiology of Breech PresentationDocumento2 páginasAnatomy and Physiology of Breech Presentationeskempertus0% (2)
- A Review of The Literature On The Effects of Acetaminophen On Pregnancy OutcomeDocumento13 páginasA Review of The Literature On The Effects of Acetaminophen On Pregnancy OutcomeJack AndreasAinda não há avaliações
- GYNECOLOGICALNURSINGDocumento4 páginasGYNECOLOGICALNURSINGSheana TmplAinda não há avaliações
- 1Documento25 páginas1Harvey Cj NarvasaAinda não há avaliações
- Drug in PregnancyDocumento5 páginasDrug in PregnancyjokosudibyoAinda não há avaliações
- Atlas of The Newborn Rudolf S Vol.1Documento167 páginasAtlas of The Newborn Rudolf S Vol.1Gabriel Burachi PeruchiAinda não há avaliações
- Mid 3 QuizletDocumento3 páginasMid 3 Quizletkristel ludangcoAinda não há avaliações
- Practice Test 2 MCNDocumento8 páginasPractice Test 2 MCNIriel Nadonga50% (2)