Escolar Documentos
Profissional Documentos
Cultura Documentos
Technique
Enviado por
Bruce Kelly MamarilDescrição original:
Direitos autorais
Formatos disponíveis
Compartilhar este documento
Compartilhar ou incorporar documento
Você considera este documento útil?
Este conteúdo é inapropriado?
Denunciar este documentoDireitos autorais:
Formatos disponíveis
Technique
Enviado por
Bruce Kelly MamarilDireitos autorais:
Formatos disponíveis
Technique
Gastric lavage involves the passage of a tube via the mouth or nose down into the stomach, followed by sequential
administration and removal of small volumes of liquid. The placement of the tube in the stomach must be confirmed
either by air insufflation while listening to the stomach, by pH testing a small amount of aspirated stomach contents,
or x-ray. This is to ensure the tube is not in the lungs. n adults, small amounts of warm water or saline are
administered and via a siphoning action removed again. n children, normal saline is used, as children are more at
risk of developing hyponatremia if lavaged with water. Because of the possibility of vomiting, a suction device is
always on hand in case of pulmonary aspiration of stomach contents. Lavage is repeated until the returning fluid
shows no further gastric contents. f the patient is unconscious or cannot protect their airway then the patient should
be intubated before performing lavage. The person must be put to sleep for a period of time during the operation due
to its high risk of shock and hyponatremia.
[edit]Indications
Gastric lavage is used infrequently in modern poisonings and some authorities have suggested that it not be used
routinely, if ever, in poisoning situations.
[3]
Lavage should only be considered if the amount of poison ingested is
potentially life-threatening and the procedure can be performed within 60 minutes of ingestion.
[4]
[edit]Contraindications
Lavage is contraindicated when patients have a compromised, unprotected airway and in patients at risk of
gastrointestinal hemorrhage or perforation. Relative contraindications include when the poisoning is due to a
corrosive substance (T54.), hydrocarbons (T53.), or for poisons that have an effective antidote.
[edit]AIternatives
An alternative for gastric lavage is the oral administration of activated carbon, a form of carbon with a large surface
area for binding poisons, preventing absorption by the gastrointestinal tract.
[edit]Complications
Many complications have been reported, although it appears serious complications are uncommon. The most
dangerous risk is aspiration pneumonia, which is more likely to occur if hydrocarbons are ingested or in patients
without a protected airway. Other complications
include laryngospasm, hypoxia, bradycardia, epistaxis, hyponatremia, hypochloremia, water intoxication, or
mechanical injury to the stomach.
LAVAGE
a. ntroduction. Gastric lavage is the washing out of the stomach via a nasogastric tube or stomach tube. Lavage is
ordered to wash out the stomach (after ingestion of poison or an overdose of medication, for example) or to control
gastrointestinal bleeding. f the patient does not have a nasogastric tube in place already, the physician will order the
insertion of the appropriate tube. For a stomach wash, the physician will probably order the insertion of an Ewald
stomach tube or a large lumen nasogastric tube. To control gastrointestinal bleeding, a large lumen Levine tube or
Salem sump tube will be inserted. n the event of severe bleeding, as in the case of esophageal varices, a
Sengstaken-Blakemore tube will be inserted. A large lumen tube is preferred, since particles of food or other material
may occlude the lumen of a small tube. The tube must be checked to verify proper placement in the stomach prior to
proceeding with lavage.
b. Equipment. Gather the following equipment and take to the patient's bedside.
(1) Syringes, 2 or more, 50cc catheter tip.
(2) Washbasins, 2 (to collect used solution).
(3) Bath towels.
(4) Chux pads.
(5) Emesis basin.
(6) Paper tissues.
(7) Graduated container for measuring.
(8) Prescribed lavage solution (usually, normal saline solution).
(9) Suction equipment readily available.
c. Preparation. Prior to beginning the procedure, check to be certain that you have prepared everything you will need.
(1) n most gastric lavage procedures, the physician's order will be to lavage "until clear." This means that the lavage
procedure will be repeated until the stomach contents that are returned are clear, that is, nothing returned except the
irrigating solution itself. This requires that you be prepared with at least 6 liters of solution. You may not need to use it
all, but you should have it available at the bedside.
(2) f the lavage procedure is being done to control gastrointestinal bleeding, the order will probably be "ice lavage."
Chilling the solution with ice will promote constriction of the blood vessels, thereby helping to control bleeding. Again,
you will need to have quite a bit of iced solution on hand and ready for use.
(3) Position of the patient for lavage will depend upon the patient's tolerance and the physician's preference. Lavage
may be done with the patient sitting or lying. Placing the patient on his left side with the HOB elevated 15 degrees will
allow the tip of the tube to lie in the greater curvature of the stomach.
d. Lavage Technique. There are two basic techniques used in performing gastric lavage. The technique used
depends upon the reason for the procedure and the physician's preference. Check the doctor's orders to see which
method is specified. f the physician does not specify the technique, consult with the professional nurse. The two
techniques used are as follow.
(1) Solution is instilled and aspirated 50cc at a time, using a catheter tip syringe. The procedure is repeated until the
stomach contents return clear, the entire amount of prescribed solution has been used, or otherwise directed.
(2) Solution is slowly poured into the tube through a funnel, allowing the solution to enter the stomach by gravity. Up
to 500cc of solution may be instilled at a time, depending upon the size and tolerance of the patient. The tube is then
lowered below the level of the patient, allowing the solution to drain out of the stomach by gravity. When using this
technique to lavage, it is imperative that the patient be assessed carefully for abdominal distension. Repeat the
procedure until the stomach contents return clear, the entire amount of solution has been used, or otherwise directed.
e. Procedure.
(1) Assemble the necessary equipment.
(2) dentify the patient and explain what is to be done.
(3) Position the patient and place an emesis basin and paper tissues within reach.
(4) Drape the patient with towels or paper chux to absorb any drainage.
(5) Verify tube placement by aspirating stomach contents.
(6) Place the stomach contents in a labeled specimen container for examination by the physician and/or laboratory
analysis.
(7) nstill lavage solution, using one of the techniques described above.
(8) Remove the lavage solution, using one of the techniques described above, as appropriate to the method of
administration.
(9) Continue to lavage until stomach contents return clear, the prescribed amount of solution has been used, or as
otherwise directed.
(10) Continually observe the patient for cyanosis, increased respiration’s, gagging, and attempts to vomit. f
the patient vomits, support his chin in hyperextension to keep the airway open and prevent aspiration.
(11) When lavage is completed, clamp the tube if it is to remain in place.
(12) f the tube is to be removed, clamp or pinch off the tube and withdraw it quickly and smoothly. Place it in a basin
or chux.
(13) Remove all used equipment from the bedside.
(14) Measure the total lavage return. Estimate the amount of stomach contents by subtracting the known amount of
solution used from the total. Record on the &O worksheet.
(15) Discard lavage solution.
(16) Dispose of equipment in accordance with local SOP.
(17) Record the procedure in the patient's Nursing Notes. Note the following information.
(a) Type and amount of lavage solution used.
(b) Appearance, odor, color, and amount of gastric return.
(c) Patient's tolerance to procedure.
(d) Disposition of specimens.
When lL ls lmporLanL Lo remove or dlluLe
gasLrlc conLenLs rapldlygasLrlc lavagelrrlgaLlon or washlng ouL of Lhe sLomach
may be lndlcaLed ln acuLe polsonlng or
lngesLlon of a causLlc subsLance a largebore 30 Lo 36 lrench nasogasLrlc Lube
ls lnserLed and lavage performed When
gasLrlc hemorrhage occurs lavage may
be used Lo remove blood from Lhe Cl
LracL 8ecause Lhe Cl LracL ls noL sLerlle
clean Lechnlque ls approprlaLe for use
alLhough Lhe soluLlon used wlll generally be sLerlle
% CbLaln basellne assessmenL lncludlng vlLal slgns abdomlnal lnspecLlon
glrLh and bowel sounds lL ls lmporLanL Lo have assessmenL daLa documenLed prlor Lo lnsLlLuLlng Lhe
procedure for comparlson
% Lxplaln Lhe procedure answerlng
quesLlons and clarlfylng percepLlons
lnsLrucL Lo reporL any paln dlfflculLy
breaLhlng or oLher problems durlng
Lhe procedure A cllenL who ls able Lo
undersLand and cooperaLe wlLh Lhe
procedure wlll LoleraLe lavage beLLer
1he cllenL may be aware of sympLoms
of compllcaLlons such as perforaLlon or
Lube dlsplacemenL before Lhey are evldenL Lo Lhe nurse
% lace ln semllowler's or lowler's poslLlon lf unable Lo LoleraLe elevaLlon
of Lhe head of Lhe bed because of hypoLenslon place ln lefL sldelylng poslLlon LlevaLlng of Lhe head of
Lhe bed
or sldelylng poslLlon wlll mlnlmlze Lhe
rlsk of asplraLlon
% lnserL a nasogasLrlc Lube lf one ls noL
already ln place verlfy Lube placemenL by asplraLlng gasLrlc conLenLs
and LesL pP of asplraLe roper placemenL ls vlLal Lo prevenL asplraLlon or
overdlsLenLlon of Lhe small bowel wlLh
lrrlgaLlng soluLlon
CLCSLu S?S1LM l88lCA1lCn
% Wearlng clean gloves connecL bag
or boLLle of normal sallne lrrlgaLlng
soluLlon Lo nasogasLrlc Lube uslng a
? connecLor ALLach dralnage or sucLlon Lube Lo oLher arm of connecLor
(llgure 1 ) LmpLy Lhe sLomach
clamp draln Lube or Lurn off sucLlon
and allow 30 Lo 200 mL of soluLlon
Lo run lnLo sLomach by gravlLy SLop
soluLlon and allow Lo draln or sucLlon
ouL 8epeaL unLll ordered amounL
has been used or deslred resulLs are
obLalned for example no furLher
cloLs and soluLlon reLurns clear or
llghL plnk Measure Lhe amounL of
dralnage subLracLlng Lhe amounL of
lrrlganL lnsLllled Lo obLaln gasLrlc
ouLpuL 1he closed sysLem mlnlmlzes
Lhe rlsk of conLacL wlLh body flulds for
Lhe nurse Measurlng gasLrlc ouLpuL ls
lmporLanL ln monlLorlng fluld balance
ln1L8Ml11Ln1 CLn S?S1LM
% Wearlng clean gloves and oLher personal proLecLlve equlpmenL as necessary (gown and face
proLecLlon)
empLy Lhe sLomach uslng sucLlon or a
30mL caLheLerLlp syrlnge Measure
and dlscard Lhe asplraLe uslng Lhe syrlngedraw up approxlmaLely 30 mL of
lrrlgaLlon soluLlon and lnsLlll lL uslng
genLle pressure AsplraLe Lhe nasogasLrlc Lube and dlscard Lhe soluLlon lnLo
a measurlng conLalner ConLlnue Lhls
procedure unLll Lhe deslred amounL of
lrrlganL or deslred resulLs have been
obLalned Manual lrrlgaLlon wlLh a
caLheLerLlp syrlnge may be more effecLlve ln removlng cloLs from Lhe sLomach
and nasogasLrlc Lube
% ConLlnue Lo monlLor vlLal slgns (lncludlng LemperaLure) Lolerance of
Lhe procedure and oLher assessmenL
daLa1he cllenL may be unsLable and requlre conLlnuous reevaluaLlon CasLrlc
lavage may cause hypoLhermla Lherefore monlLor LemperaLure and lndlcaLlons of hypoLhermla such as
leLhargy
and changes ln cardlac raLe and
rhyLhm
% lf Lhe asplraLe has noL cleared Lo llghL
plnk or plnkLlnged afLer 20 Lo 30 mlnuLes of lavage or lf Lhe cllenL ls unable
Lo LoleraLe Lhe procedure noLlfy Lhe
physlclan Medlcal or surglcal lnLervenLlon may be necessary Lo sLop hemorrhage ln some lnsLances
% Cn compleLlon of lavage provlde
mouLh and nares care ConLlnue Lo
monlLor vlLal slgns abdomlnal sLaLus
and oLher assessmenL daLa
% uocumenL Lhe procedure lncludlng
Lhe amounL and Lype of lrrlganL used
gasLrlc ouLpuL characLer and amounL
and Lhe cllenL's condlLlon and Lolerance of Lhe procedure
hLLp//slmplemedblogspoLcom/2009/01/gasLrlclavagehLml
Você também pode gostar
- The Yellow House: A Memoir (2019 National Book Award Winner)No EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Nota: 4 de 5 estrelas4/5 (98)
- Tx. COVID 19 en UCIDocumento6 páginasTx. COVID 19 en UCIVictor Augusto Ávila HernándezAinda não há avaliações
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeNo EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeNota: 4 de 5 estrelas4/5 (5795)
- Ghid de Resuscitare Dupa Chirurgia Cardiaca EACTS 2009Documento24 páginasGhid de Resuscitare Dupa Chirurgia Cardiaca EACTS 2009Raluca L100% (1)
- Surgical Reconstruction of Interdental Papilla Using Subepithelialconnective Tissue Graft by Microsurgical Technique A Clinical ST 2376 032X 1000229Documento6 páginasSurgical Reconstruction of Interdental Papilla Using Subepithelialconnective Tissue Graft by Microsurgical Technique A Clinical ST 2376 032X 1000229neighAinda não há avaliações
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureNo EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureNota: 4.5 de 5 estrelas4.5/5 (474)
- The Language of AnatomyDocumento7 páginasThe Language of AnatomyLinziJaeOnelAinda não há avaliações
- 03 Anaesthesia Machine PDFDocumento0 página03 Anaesthesia Machine PDFjuniorebindaAinda não há avaliações
- What To Do About Extracranial and Intracranial Stenosis: Home About Issues Categories Back Issues Case Reports ContactDocumento13 páginasWhat To Do About Extracranial and Intracranial Stenosis: Home About Issues Categories Back Issues Case Reports ContactpramitaListyAinda não há avaliações
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryNo EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryNota: 3.5 de 5 estrelas3.5/5 (231)
- Foundation Module Embrology and Gernal Anatomy MCQ by DR of 2027 28Documento53 páginasFoundation Module Embrology and Gernal Anatomy MCQ by DR of 2027 28Xandws -IOS tips and trick and gamingAinda não há avaliações
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceNo EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceNota: 4 de 5 estrelas4/5 (895)
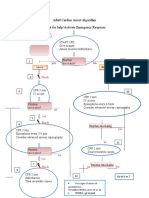
- Adult Cardiac Arrest Algorithm Shout For Help/activate Emergency ResponseDocumento1 páginaAdult Cardiac Arrest Algorithm Shout For Help/activate Emergency ResponseICU RSBMAinda não há avaliações
- Never Split the Difference: Negotiating As If Your Life Depended On ItNo EverandNever Split the Difference: Negotiating As If Your Life Depended On ItNota: 4.5 de 5 estrelas4.5/5 (838)
- Rhinoplasty With Barbed Threads: CosmeticDocumento12 páginasRhinoplasty With Barbed Threads: CosmeticRaphaela TravassosAinda não há avaliações
- The Little Book of Hygge: Danish Secrets to Happy LivingNo EverandThe Little Book of Hygge: Danish Secrets to Happy LivingNota: 3.5 de 5 estrelas3.5/5 (400)
- Catalogo Dtek NylonDocumento25 páginasCatalogo Dtek NylonAna UmañaAinda não há avaliações
- Assem Draz: Neurological DisordersDocumento26 páginasAssem Draz: Neurological DisordersxuexueAinda não há avaliações
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersNo EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersNota: 4.5 de 5 estrelas4.5/5 (345)
- Surgery For Endocrinological Diseases and Malformations in ChildhoodDocumento155 páginasSurgery For Endocrinological Diseases and Malformations in ChildhoodBeng DinAinda não há avaliações
- Final Physical ExaminationDocumento3 páginasFinal Physical Examinationapi-620159117Ainda não há avaliações
- The Unwinding: An Inner History of the New AmericaNo EverandThe Unwinding: An Inner History of the New AmericaNota: 4 de 5 estrelas4/5 (45)
- EZ-IO Insertion Proximal Humerus - in DepthDocumento36 páginasEZ-IO Insertion Proximal Humerus - in Depthwps013100% (1)
- Team of Rivals: The Political Genius of Abraham LincolnNo EverandTeam of Rivals: The Political Genius of Abraham LincolnNota: 4.5 de 5 estrelas4.5/5 (234)
- Basic Life Support: Elements of The Survey The SceneDocumento5 páginasBasic Life Support: Elements of The Survey The SceneMarrianne MortaAinda não há avaliações
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyNo EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyNota: 3.5 de 5 estrelas3.5/5 (2259)
- Gastro EndosDocumento263 páginasGastro EndosJay Seetohul50% (2)
- How I Bypassed My Bypass-SurgeryDocumento4 páginasHow I Bypassed My Bypass-Surgeryharinag49Ainda não há avaliações
- Ix - (Revised) Med Cert ValidationDocumento5 páginasIx - (Revised) Med Cert ValidationAlvin Xtian NucumAinda não há avaliações
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaNo EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaNota: 4.5 de 5 estrelas4.5/5 (266)
- Performing Different Types of BiopsiesDocumento5 páginasPerforming Different Types of BiopsiesTALHA AKRAMAinda não há avaliações
- The Emperor of All Maladies: A Biography of CancerNo EverandThe Emperor of All Maladies: A Biography of CancerNota: 4.5 de 5 estrelas4.5/5 (271)
- Worksheets - Isbar 3 StrokeDocumento3 páginasWorksheets - Isbar 3 Strokeapi-673621869Ainda não há avaliações
- Sdfa Sdfasdk JFLKSDF Asdfasdf Sdaf AsdfDocumento19 páginasSdfa Sdfasdk JFLKSDF Asdfasdf Sdaf AsdfFaris BariqiAinda não há avaliações
- Emergency Profile ManagementDocumento13 páginasEmergency Profile ManagementCristian PazAinda não há avaliações
- Anal GlandsDocumento7 páginasAnal GlandsSuraj_Subedi100% (2)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreNo EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreNota: 4 de 5 estrelas4/5 (1090)
- VaricoceleDocumento10 páginasVaricoceleDenny SetyadiAinda não há avaliações
- Rsi Currency Practical 3 1Documento2 páginasRsi Currency Practical 3 1Cristian CoronelAinda não há avaliações
- Https Emedicine - MedscapeDocumento14 páginasHttps Emedicine - MedscapeNanaAinda não há avaliações
- Lung Cancer Case Study 4Documento36 páginasLung Cancer Case Study 4mulanAinda não há avaliações
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)No EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Nota: 4.5 de 5 estrelas4.5/5 (121)
- Shoulder CodeDocumento2 páginasShoulder CodeNasfikurAinda não há avaliações
- AngiotechDocumento48 páginasAngiotechWei LiangAinda não há avaliações
- Guide To Dental Treatment BandsDocumento2 páginasGuide To Dental Treatment BandsVikram Kapur100% (1)