Escolar Documentos
Profissional Documentos
Cultura Documentos
Cakcium 1
Enviado por
Hilal Mohamed NorDescrição original:
Direitos autorais
Formatos disponíveis
Compartilhar este documento
Compartilhar ou incorporar documento
Você considera este documento útil?
Este conteúdo é inapropriado?
Denunciar este documentoDireitos autorais:
Formatos disponíveis
Cakcium 1
Enviado por
Hilal Mohamed NorDireitos autorais:
Formatos disponíveis
Hypocalcemia refers to a diminished calcium level, below 8.5 mg/dL, in the bloodstream.
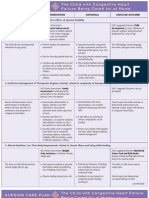
Calcium is vital to the body for the formation of bones and teeth, blood coagulation, nerve impulse transmission, cell permeability, and normal muscle contraction. Although nearly all of the bodys calcium is found in the bones, three forms of calcium exist in the serum: free or ionized calcium, calcium bound to protein, and calcium complexed with citrate or other organic ions. Ionized calcium is reabsorbed into bone, absorbed from the gastrointestinal mucosa, and excreted in urine and feces as regulated by the parathyroid glands. Parathyroid hormone (PTH) is necessary for calcium absorption and normal serum calcium levels. Hypocalcemia is a more common clinical problem than hypercalcemia and may occur as frequently as 15% to 50% in acutely and critically ill patients. When calcium levels drop, neuromuscular excitability occurs in smooth, skeletal, and cardiac muscle, thus causing the muscles to twitch. The result can lead to cardiac dysrhythmias. Hypocalcemia can also cause increased capillary permeability, pathological fractures, and decreased blood coagulation. Most severe cases result in tetany (condition of prolonged, painful spasms of the voluntary muscles of the fingers and toes (carpopedal spasm) as well as the facial muscles), which if left untreated, leads to carpopedal and laryngeal spasm, seizures, and respiratory arrest. The most frequent cause of hypocalcemia is a low albumin level, but if serum ionized (free) calcium is normal, then no disorder of calcium metabolism is present and no treatment is needed. Causes of low ionized calcium, which is needed for enzymatic reactions and neuromuscular function, include renal failure, hypoparathyroidism, severe hypomagnesemia, hypermagnesemia, and acute pancreatitis. It is also associated with thyroidectomy and radical neck dissection when there is postoperative ischemia to the parathyroids. Low serum calcium levels can also occur after small bowel resection, partial gastrectomy with gastrojejunostomy, and Crohns disease. Severe diarrhea or laxative abuse may also cause hypocalcemia; when intestinal surfaces are lost, less calcium is absorbed. A transient low calcium level can result from massive administration of citrated blood. Some drugs that can result in hypocalcemia include loop diuretics, phenytoin, phosphates, caffeine, alcohol, antimicrobials (pentamidine, ketoconazole, aminoglycosides), antineoplastic agents (cisplatin, cytosine arabinoside), and corticosteroids. Nursing care plan assessment and physical examination Ask about a prior diagnosis of hypoparathyroidism, pancreatic insufficiency, or hypomagnesemia. Elicit a history of severe infections or burns. Ask if the patient has been under treatment for acidosis, which might lead to alkalosis. Determine if the patient has an inadequate intake of calcium, vitamin D, or both. Investigate causes of vitamin D or magnesium deficiency, such as a gastrointestinal disease that is associated with malabsorption, poor diet, gastrectomy, intestinal resection or bypass, or hepatobiliary disease. Ask about medication use that is associated with disordered calcium metabolism, such as phenytoin or plicamycin. Inquire about anxiety, irritability, twitching around the mouth, laryngospasm, or convulsions, all central nervous system signs and symptoms of hypocalcemia. Establish a history of tingling or numbness in the fingers (paresthesia), tetany or painful tonic muscle spasms, abdominal cramps, muscle cramps, or spasmodic contractions. Ask the patient about gastrointestinal symptoms such as diarrhea. Assess airway, breathing, and circulation (ABCs). Hypocalcemia can lead to laryngospasm, dyspnea, and heart failure. Auscultate for heart sounds. The patient may have dysrhythmias, especially heart block and ventricular fibrillation. Tetany, increased neural excitability, accounts for the majority of signs and symptoms of hypocalcemia. Check for Trousseaus sign (development of carpal spasm when a blood pressure cuff is inflated above systolic pressure for 3 minutes) and Chvosteks sign (twitching
facial muscles when the facial nerve is tapped anterior to the ear). Inspect the patients skin to see if it is dry, coarse, or scaly, which are signs of hypocalcemia. Note any exacerbation of eczema or psoriasis along with hair loss or brittle nails. Check for dental abnormalities. Inspect the patients eyes for cataracts of the cortical portion of the lens, which may develop within a year after the onset of hypocalcemia. Severe hypocalcemia may produce mental changes. Assess for depression, impaired memory, and confusion. As the condition continues, delirium and hallucinations may be present. In severe cases of hypocalcemia, psychosis or dementia may develop. Electrolyte disturbances that affect a patients personality often increase the patients and familys anxiety. Assess the patients and familys coping mechanisms. Nursing care plan primary nursing diagnosis: Risk for ineffective airway clearance related to laryngospasm. Nursing care plan intervention and treatment plan If the patient has an airway obstruction, endotracheal intubation and mechanical ventilation may be needed to manage laryngospasm. Hypocalcemia is treated pharmacologically. Acute hypocalcemia with tetany is a medical emergency that requires parenteral calcium supplements. Be aware of factors related to the administration of calcium replacement. A too-rapid infusion rate can lead to bradycardia and cardiac arrest; therefore, place patients who are receiving a continuous calcium infusion on a cardiac monitor, and place the infusion on a controlled infusion device. The infusion rate should be adjusted to avoid recurrent symptomatic hypocalcemia and to maintain serum calcium levels between 8 and 9 mg/dL. Monitor the patients serum calcium levels every 12 to 24 hours, and immediately report a calcium deficit less than 8.5 mg/dL. When giving calcium supplements, frequently check pH levels because an alkaline state (pH 7.45) inhibits calcium ionization and decreases the free calcium available for physiological reactions. Chronic hypocalcemia can be treated in part by a high dietary intake of calcium. If the deficiency is caused by hypoparathyroidism, however, teach the patient to avoid foods high in phosphate. Vitamin D supplements are prescribed to facilitate gastrointestinal calcium absorption. If the patient has an altered mental status, institute the appropriate safety measures. Provide a quiet, stress-free environment for patients with tetany. Institute seizure precautions for patients with severe hypocalcemia. If tetany is a possibility, maintain an oral or a nasal airway and intubation equipment at the bedside. Initiate patient teaching to prevent future episodes of hypocalcemia. Nursing care plan discharge and home health care guidelines Instruct the patient about foods rich in calcium, vitamin D, and protein. Emphasize the effect of drugs on serum calcium levels. High intakes of alcohol and caffeine decrease calcium absorption, as does moderate cigarette smoking. Patients with a tendency to develop renal calculi should be told to consult their physician before increasing their calcium intake. When hypocalcemia is caused by hypoparathyroidism, milk and milk products are omitted from the patients diet to decrease phosphorus intake. Be sure the patient understands any calcium supplements prescribed, including dosages, route, action, and side effects. Advise the patient that calcium may cause constipation, and review methods to maintain bowel elimination. Hypercalcemia may develop as a consequence of the treatment for hypocalcemia. Teach the patient the signs and symptoms of increased serum calcium levels and the need to call the physician if they develop.
Você também pode gostar
- MCM Who Academy Guide FinalDocumento88 páginasMCM Who Academy Guide FinalHilal Mohamed NorAinda não há avaliações
- Module 1 Peri-Pre-Operative Patient CareDocumento25 páginasModule 1 Peri-Pre-Operative Patient CareHilal Mohamed NorAinda não há avaliações
- WHO scales up trauma response in SomaliaDocumento3 páginasWHO scales up trauma response in SomaliaHilal Mohamed NorAinda não há avaliações
- Hospital Employees Improve Basic Life Support Skills and Confidence With A Personal Resuscitation Manikin and A 24-Min Video InstructionDocumento1 páginaHospital Employees Improve Basic Life Support Skills and Confidence With A Personal Resuscitation Manikin and A 24-Min Video InstructionHilal Mohamed NorAinda não há avaliações
- The Human Brain: An Introduction to Neuroanatomy and Brain FunctionDocumento10 páginasThe Human Brain: An Introduction to Neuroanatomy and Brain FunctionHilal Mohamed NorAinda não há avaliações
- Adult vital signs monitoring chartDocumento2 páginasAdult vital signs monitoring chartHilal Mohamed NorAinda não há avaliações
- Adult Basic Life Support (BLS) Awareness and Knowledge Among Medical and Dental Interns Completing Internship From Deemed University PDFDocumento8 páginasAdult Basic Life Support (BLS) Awareness and Knowledge Among Medical and Dental Interns Completing Internship From Deemed University PDFHilal Mohamed NorAinda não há avaliações
- Reducing Nurses' Stress - A Randomized Controlled Trial of A Web-BasedDocumento8 páginasReducing Nurses' Stress - A Randomized Controlled Trial of A Web-BasedHilal Mohamed Nor0% (1)
- Emergency Department Triage RevisitedDocumento8 páginasEmergency Department Triage RevisitedHilal Mohamed NorAinda não há avaliações
- SOM HealthcareseekingbehaviourReport 10-WEB PDFDocumento52 páginasSOM HealthcareseekingbehaviourReport 10-WEB PDFHilal Mohamed Nor100% (1)
- Job Stress Management in Nurses PDFDocumento6 páginasJob Stress Management in Nurses PDFHilal Mohamed NorAinda não há avaliações
- Child - Heart at HomeDocumento2 páginasChild - Heart at HomeHilal Mohamed NorAinda não há avaliações
- Effect of Triage TrainingDocumento3 páginasEffect of Triage TrainingHilal Mohamed NorAinda não há avaliações
- Disorders of Calcium and Phosphate MetabolismDocumento20 páginasDisorders of Calcium and Phosphate MetabolismHilal Mohamed NorAinda não há avaliações
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeNo EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeNota: 4 de 5 estrelas4/5 (5784)
- The Little Book of Hygge: Danish Secrets to Happy LivingNo EverandThe Little Book of Hygge: Danish Secrets to Happy LivingNota: 3.5 de 5 estrelas3.5/5 (399)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceNo EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceNota: 4 de 5 estrelas4/5 (890)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureNo EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureNota: 4.5 de 5 estrelas4.5/5 (474)
- The Yellow House: A Memoir (2019 National Book Award Winner)No EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Nota: 4 de 5 estrelas4/5 (98)
- Team of Rivals: The Political Genius of Abraham LincolnNo EverandTeam of Rivals: The Political Genius of Abraham LincolnNota: 4.5 de 5 estrelas4.5/5 (234)
- Never Split the Difference: Negotiating As If Your Life Depended On ItNo EverandNever Split the Difference: Negotiating As If Your Life Depended On ItNota: 4.5 de 5 estrelas4.5/5 (838)
- The Emperor of All Maladies: A Biography of CancerNo EverandThe Emperor of All Maladies: A Biography of CancerNota: 4.5 de 5 estrelas4.5/5 (271)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryNo EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryNota: 3.5 de 5 estrelas3.5/5 (231)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaNo EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaNota: 4.5 de 5 estrelas4.5/5 (265)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersNo EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersNota: 4.5 de 5 estrelas4.5/5 (344)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyNo EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyNota: 3.5 de 5 estrelas3.5/5 (2219)
- The Unwinding: An Inner History of the New AmericaNo EverandThe Unwinding: An Inner History of the New AmericaNota: 4 de 5 estrelas4/5 (45)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreNo EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreNota: 4 de 5 estrelas4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)No EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Nota: 4.5 de 5 estrelas4.5/5 (119)
- Sarns Modular Perfusion System 8000: A Flexible, Dependable, and Cost-Efficient Modular Blood Pumping SystemDocumento4 páginasSarns Modular Perfusion System 8000: A Flexible, Dependable, and Cost-Efficient Modular Blood Pumping SystemAdvancemicronics MedicalsystemsAinda não há avaliações
- Chapter 1 The Foundations of BiochemistryDocumento5 páginasChapter 1 The Foundations of BiochemistryghurapAinda não há avaliações
- 11.transportation in Plants & AnimalsDocumento51 páginas11.transportation in Plants & AnimalsReshma ModhiaAinda não há avaliações
- Binocular Anomalies - GriffinDocumento595 páginasBinocular Anomalies - GriffinAdolph Grey75% (4)
- Journey Through DigestionDocumento4 páginasJourney Through DigestionJoy JonesAinda não há avaliações
- Assessment of HearingDocumento51 páginasAssessment of HearingSwetha PasupuletiAinda não há avaliações
- Newborn Hypothermia and Hyperthermia (Final Copy)Documento30 páginasNewborn Hypothermia and Hyperthermia (Final Copy)Shizuka Marycris Amane67% (3)
- University of Phoenix Anatomy and Physiology Week 2 QuizDocumento2 páginasUniversity of Phoenix Anatomy and Physiology Week 2 QuizSophia FHSAinda não há avaliações
- Histology Guide: Tissues, Epithelial Types & FunctionsDocumento40 páginasHistology Guide: Tissues, Epithelial Types & FunctionsStevenRafaelGarciaManingasAinda não há avaliações
- Ppe4 Reflection AssignmentDocumento11 páginasPpe4 Reflection Assignmentapi-318846856100% (1)
- The Quest For Consciousness A Neurobiological ApproachDocumento435 páginasThe Quest For Consciousness A Neurobiological ApproachMaria Karystinou94% (18)
- Delprato and MidgleyDocumento14 páginasDelprato and MidgleyAna LucaAinda não há avaliações
- X - Problem Prioritization and NCPDocumento5 páginasX - Problem Prioritization and NCPMartin Lєtmaku Espina100% (2)
- Inductions To LearnDocumento7 páginasInductions To LearnMichael HobbsAinda não há avaliações
- MedulloblastomaDocumento2 páginasMedulloblastomaMohammadAwitAinda não há avaliações
- Bac ToxinDocumento9 páginasBac ToxinJawairia KhawarAinda não há avaliações
- A Presentation On Pantothenic Acid or b5Documento28 páginasA Presentation On Pantothenic Acid or b5jainsaketAinda não há avaliações
- Analgesia AvesDocumento16 páginasAnalgesia AvesJESSICA ZAPATAAinda não há avaliações
- Aqa Byb1 W QP Jun07Documento12 páginasAqa Byb1 W QP Jun07李超然Ainda não há avaliações
- Basic PhysiologyDocumento58 páginasBasic PhysiologyVidit JoshiAinda não há avaliações
- Herbesser 90 SR and 180 SR capsules for hypertension and anginaDocumento2 páginasHerbesser 90 SR and 180 SR capsules for hypertension and anginaAqleedasAinda não há avaliações
- Physical ExaminationDocumento117 páginasPhysical Examinationsasmita nayakAinda não há avaliações
- Principle of The Method Quality Control: Alkaline PicrateDocumento1 páginaPrinciple of The Method Quality Control: Alkaline PicrateRisqon Anjahiranda Adiputra100% (1)
- Fluid Volume DeficitDocumento2 páginasFluid Volume DeficitpeternohibiAinda não há avaliações
- Parasitology Lect. (4) : Preparation of Solutions For Wet MountDocumento5 páginasParasitology Lect. (4) : Preparation of Solutions For Wet MountAbdul hadiAinda não há avaliações
- DR Anu Arasu How Trauma Affects Your HormonesDocumento14 páginasDR Anu Arasu How Trauma Affects Your HormonesShalu SaharanAinda não há avaliações
- Nursing Care Plan AmoebiasisDocumento2 páginasNursing Care Plan Amoebiasisderic97% (35)
- Endocrine Physiology Lecture 2Documento9 páginasEndocrine Physiology Lecture 2Tofunmi Kunle-KunbiAinda não há avaliações
- Medial Longitudinal FasciculusDocumento5 páginasMedial Longitudinal FasciculussakuraleeshaoranAinda não há avaliações
- GATE Life Science Syllabus 2020 - GATE XL Chapters & TopicsDocumento11 páginasGATE Life Science Syllabus 2020 - GATE XL Chapters & TopicsSaiful IslamAinda não há avaliações