Escolar Documentos
Profissional Documentos
Cultura Documentos
Postoperative Phase
Enviado por
reymarhayDescrição original:
Direitos autorais
Formatos disponíveis
Compartilhar este documento
Compartilhar ou incorporar documento
Você considera este documento útil?
Este conteúdo é inapropriado?
Denunciar este documentoDireitos autorais:
Formatos disponíveis
Postoperative Phase
Enviado por
reymarhayDireitos autorais:
Formatos disponíveis
Postoperative Phase
Definition
The postoperative period oI the surgical experience extends Irom the time the client is
transIerred to the recovery room or past-anesthesia care unit (PACU) to the moment he or she is
transported back to the surgical unit, discharged Irom the hospital until the Iollow-up care.
Goals during the Postoperative Period
During the postoperative period, reestablishing the patient`s physiologic balance, pain
management and prevention oI complications should be the Iocus oI the nursing care. To do
these it is crucial that the nurse perIorm careIul assessment and immediate intervention in
assisting the patient to optimal Iunction quickly, saIely and comIortably as possible.
1. aintaining adequate body system Iunctions.
2. Restoring body homeostasis.
3. Pain and discomIort alleviation.
4. Preventing postoperative complications.
5. Promoting adequate discharge planning and health teaching.
Patient Care during Immediate Postoperative Phase: Transferring the Patient
to RR or PACU
Patient Assessment
Special consideration to the patient`s incision site, vascular status and exposure should be
implemented by the nurse when transIerring the patient Irom the operating room to the
postanethesia care unit (PACU) or postanesthesia recovery room (PARR). Every time the patient
is moved, the nurse should Iirst consider the location oI the surgical incision to prevent Iurther
strain on the sutures. II the patient comes out oI the operating room with drainage tubes, position
should be adjusted in order to prevent obstruction on the drains.
1. Assess air exchange status and note patient`s skin color
2. VeriIy patient identity. The nurse must also know the type oI operative procedure
perIormed and the name oI the surgeon responsible Ior the operation.
3. Neurologic status assessment. Level oI consciousness (LOC) assessment and Glasgow
Coma Scale (GCS) are helpIul in determining the neurologic status oI the patient.
4. Cardiovascular status assessment. This is done by determining the patient`s vital signs in
the immediate postoperative period and skin temperature.
5. Operative site examination. Dressings should be checked.
Positioning
oving a patient Irom one position to another may result to serious arterial hypotension.
This occurs when a patient is moved Irom a lithotomy to a horizontal position, Irom a lateral to a
supine position, prone to supine position and even when a patient is transIerred to the stretcher.
Hence, it is very important that patients are moved slowly and careIully during the immediate
postoperative phase.
Promoting Patient Safety
When transIerred to the stretcher, the patient should be covered with blankets and secured
with straps above the knees and elbows. These straps anchor the blankets at the same time
restrain the patient should he or she pass through a stage oI excitement while recovering Irom
anesthesia. To protect the patient Irom Ialls, side rails should be raised.
SaIety checks when transIerring the patient Irom OR to RR:
S Securing restraints Ior I.V. Iluids and blood transIusion.
A Assist the patient to a position appropriate Ior him on her based on the location oI incision
site and presence oI drainage tubes.
F Fall precaution implementation by making sure the side rails are raised and restraints are
secured well.
E Eliminating possible sources oI injuries and accidents when moving the patient Irom the OR
to RR or PACU.
ursing Care for Patient in the PACU or RR
AIRWAY: Maintain a patent airway.
1. eep airway in place until the patient is Iully awake and tries to eject it. The airway is
allowed to remain in place while the client is unconscious to keep the passage open and
prevents the tongue Irom Ialling back. When the tongue Ialls back, airway passage
obstruction will result. Return oI pharyngeal reIlex, noted when the patient regains
consciousness, may cause the patient to gag and vomit when the airway is not removed
when the patient is awake.
2. 2. Suction secretions as needed.
REATHIG: Maintaining adequate respiratory function.
B Bilateral lung auscultation Irequently.
R Rest and place the patient in a lateral position with the neck extended, iI not contraindicated,
and the arm supported with a pillow. This position promotes chest expansion and Iacilitates
breathing and ventilation.
E Encourage the patient to take deep breaths. This aerates the lung Iully and prevents
hypostatic pneumonia.
A Assess and periodically evaluate the patient`s orientation to name or command. Cerebral
Iunction alteration is highly suggestive oI impaired oxygen delivery.
T Turn the patient every 1 to 2 hours to Iacilitate breathing and ventilation.
H HumidiIied oxygen administration. During exhalation, heat and moisture are normally lost,
thus oxygen humidiIication is necessary. Aside Irom that, secretion removal is Iacilitated when
kept moist through the moisture oI the inhaled air. Also, dehydrated patients have irritated
respiratory passages thus, it is very important make sure that the inhaled oxygen is humidiIied.
CIRCULATIO: Assess status of circulatory system.
1. Obtain patient`s vital signs as ordered and report any abnormalities.
2. onitor intake and output closely.
3. Recognize early symptoms oI shock or hemorrhage such as cold extremities, decreased
urine output less than 30 ml/hr, slow capillary reIill greater than 3 seconds, dropping
blood pressure, narrowing pulse pressure, tachycardia increased heart rate.
THERMOREGULATIO: Assessing the patient`s thermoregulatory status.
1. Hourly temperature assessment to detect hypothermia or hyperthermia.
2. Report temperature abnormalities to the physician.
3. onitor the patient Ior postanethesia shivering or PAS. This is noted in hypothermic
patients, about 30 to 45 minutes aIter admission to the PACU. PAS represents a heat-gain
mechanism and relates to regaining the thermal balance.
4. Provide a therapeutic environment with proper temperature and humidity. Warm blankets
should be provided when the patient is cold.
LUID VOLUME: Maintaining adequate fluid volume.
1. Assess and evaluate patient`s skin color and turgor, mental status and body temperature.
2. onitor and recognize evidence oI Iluid and electrolyte imbalances such as nausea and
vomiting and body weakness.
3. onitor intake and output closely.
4. Recognize signs oI Iluid imbalances. HYPOVOLEIA: decreased blood pressure,
decreased urine output, increased pulse rate, increased respiration rate, and decreased
central venous pressure (CVP). HYPERVOLEIA: increased blood pressure and CVP,
changes in lung sounds such as presence oI crackles in the base oI both lungs and changes
in heart sounds such as the presence oI S3 gallop.
SAETY: Promoting patient safety.
1. Avoid nerve damage and muscle strain by properly supporting and padding pressure areas.
2. Frequent dressing examination Ior possible constriction.
3. Raise the side rails to prevent the patient Irom Ialling.
4. Protect the extremity where IV Iluids are inserted to prevent possible needle dislodge.
5. ake sure that bed wheels are locked.
COMORT: Promoting patient comfort.
1. Observe and assess behavioral and physiologic maniIestations oI pain.
2. Administer medications Ior pain and document its eIIicacy.
3. Assist the patient to a comIortable position.
SKI ITEGRITY: Minimizing skin impairment.
1. Record the amount and type oI wound drainage.
2. Regularly inspect dressings and reinIorce them iI necessary.
3. Proper wound care as needed.
4. PerIorm hand washing beIore and aIter contact with the patient.
5. Turn the patient to sides every 1 to 2 hours.
6. aintain the patient`s good body alignment.
EVALUATIO in PACU
Patients in PACU are evaluated to determine the client`s discharge Irom the unit. The Iollowing
are the expected outcomes in PACU:
1. Patient breathing easily.
2. Clear lung sounds on auscultation.
3. Stable vital signs.
4. Stable body temperature with minimal chills or shivering.
5. No signs oI Iluid volume imbalance as evidenced by an equal intake and output.
6. Tolerable or minimized pain, as reported by the patient.
7. Intact wound edges without drainage.
. Raised side rails.
9. Appropriate patient position.
10.aintained quiet and therapeutic environment.
Patient Care during Immediate Postoperative Phase: Transferring the Patient
from RR to the Surgical Unit
To determine the patient`s readiness Ior discharge Irom the PACU or RR certain criteria must be
met. The parameters used Ior discharge Irom RR are the Iollowing:
1. Uncompromised cardiopulmonary status
2. Stable vital signs
3. Adequate urine output at least 30 ml/ hour
4. Orientation to time, date and place
5. SatisIactory response to commands
6. inimal pain
7. Absence or controlled nausea and vomiting
. Pulse oximetry readings oI adequate oxygen saturation
9. SatisIactory response to commands
10.ovement oI extremities aIter regional anesthesia
ost hospitals use a scoring system to assess the general condition oI patient in RR or
PACU. Observation and evaluation oI the patient`s physical signs is based on a set oI objective
criteria. The evaluation guide used is a modiIication oI the APGAR scoring system used Ior
newborns. Through this, a more objective assessment oI the patient`s physical condition is
guaranteed while recovering the RR or PACU. The perIect possible score in this modiIied
APGAR scoring system is 10. To be discharge Irom RR or PACU the patient is required to have
at least 7 to points. Patients with score less than 7 must remain in RR or PACU until their
condition improves. Areas oI assessment in PACU or RR evaluation guide are:
1. Respiration ability to breathe deeply and cough.
2. Circulation systolic arterial pressure ~0 oI preanesthetic level
3. Consciousness Level verbally responds to questions or oriented to location
4. Color normal skin color and appearance: pinkish skin and mucus
5. uscle activity moves spontaneously or on command
ursing care during the intermediate postoperative period:
Assessment
1. Respiratory status: airway patency, depth, rate and character oI respirations, nature oI
breath sounds
2. Circulatory Status: vital signs including blood pressure and skin condition
3. Neurologic: level oI responsiveness
4. Drainage: presence oI drainage, need to connect tubes to a speciIic drainage system,
presence and condition oI dressings
5. ComIort: type oI pain and location, nausea and vomiting, position change required
6. Psychologic: nature oI patient`s questions, need Ior rest and sleep, disturbance by noise,
visitors, availability oI call bell or call light
7. SaIety: need Ior side rails, drainage tubes unobstructed, IV Iluid properly inIusing and IV
sites properly splinted
. Equipment: checked Ior proper Iunctioning
Goals and Interventions
P Preventing and/or relieving complications
O Optimal respiratory Iunction
S Support: psychosocial well-being
T Tissue perIusion and cardiovascular status maintenance
O Observing and maintaining adequate Iluid intake
P Promoting adequate nutrition and elimination
A Adequate Iluid and electrolyte balance
R Renal Iunction maintenance
E Encouraging activity and mobility within limits
T Thorough wound care Ior adequate wound healing
I InIection Control
V Vigilant to maniIestations oI anxiety and promoting ways oI relieving it
E Eliminating environmental hazards and promoting client saIety
Você também pode gostar
- Management of Tuberculosis: A guide for clinicians (eBook edition)No EverandManagement of Tuberculosis: A guide for clinicians (eBook edition)Ainda não há avaliações
- Patient ChartDocumento2 páginasPatient ChartHydieAinda não há avaliações
- COMPREHENSIVE NURSING ACHIEVEMENT TEST (RN): Passbooks Study GuideNo EverandCOMPREHENSIVE NURSING ACHIEVEMENT TEST (RN): Passbooks Study GuideAinda não há avaliações
- Naso Orogastric Tube Guideline For The Care of Neonate Child or Young Person RequiringDocumento12 páginasNaso Orogastric Tube Guideline For The Care of Neonate Child or Young Person RequiringmeisygraniaAinda não há avaliações
- Shock Concept MapDocumento2 páginasShock Concept MapElizabeth GarretsonAinda não há avaliações
- NURSING EMERGENCIES. 10 BASED TEST QUESTIONS WITH BIBLIOGRAPHYNo EverandNURSING EMERGENCIES. 10 BASED TEST QUESTIONS WITH BIBLIOGRAPHYAinda não há avaliações
- Maternal and Child Health Nursing: KeepsDocumento32 páginasMaternal and Child Health Nursing: Keepsshenric16Ainda não há avaliações
- Perioperative Nursing ModuleDocumento2 páginasPerioperative Nursing ModulerosanowardAinda não há avaliações
- PRC Form (Minor Operation)Documento1 páginaPRC Form (Minor Operation)mawelAinda não há avaliações
- Geria Lec Portfolio CasiaDocumento9 páginasGeria Lec Portfolio CasiaMarie Ashley CasiaAinda não há avaliações
- Thoracentesis Reflective EssayDocumento2 páginasThoracentesis Reflective EssayAnjae GariandoAinda não há avaliações
- Code Blue in HospitalDocumento7 páginasCode Blue in HospitalJu Lie AnnAinda não há avaliações
- History of Past IllnessDocumento4 páginasHistory of Past IllnessKrisianne Mae Lorenzo FranciscoAinda não há avaliações
- Triage and Priority SettingDocumento10 páginasTriage and Priority SettingekonurcahyaningrumAinda não há avaliações
- Operating RoomDocumento13 páginasOperating RoomrichardAinda não há avaliações
- P2 Long Exam A 15 Block 3 Funda Lecture PDFDocumento25 páginasP2 Long Exam A 15 Block 3 Funda Lecture PDFryllerylle05Ainda não há avaliações
- Hygiene (NCLEX) Flashcards - QuizletDocumento5 páginasHygiene (NCLEX) Flashcards - QuizletA.Ainda não há avaliações
- NCPDocumento2 páginasNCPMelissa David100% (1)
- IntussusceptionDocumento1 páginaIntussusceptionJune DumdumayaAinda não há avaliações
- CIP-NCM-121-Disaster Nursing-TuesdaysDocumento3 páginasCIP-NCM-121-Disaster Nursing-TuesdaysKhen QuiringAinda não há avaliações
- Nursing Interventions CHFDocumento3 páginasNursing Interventions CHFbanyenye25100% (1)
- Communicable DiseaseDocumento3 páginasCommunicable Diseasemiss RNAinda não há avaliações
- 51 100Documento18 páginas51 100Jaessa Feliciano100% (1)
- Pediatric Nursing Edison O Dangkeo RNDocumento59 páginasPediatric Nursing Edison O Dangkeo RNshenric16100% (1)
- Aseptic TecniqueDocumento40 páginasAseptic TecniquepsyconnectAinda não há avaliações
- Journal in Medical WardDocumento4 páginasJournal in Medical WardApol PenAinda não há avaliações
- PnclexDocumento3 páginasPnclexPaul Michael BaguhinAinda não há avaliações
- Multiple Choice Test QuestionsDocumento6 páginasMultiple Choice Test QuestionsNicole MaeAinda não há avaliações
- ImciDocumento3 páginasImciJohn Benzon0% (1)
- Wound Healing and Wound CareDocumento15 páginasWound Healing and Wound CareNinaAinda não há avaliações
- Neumans Systems ModelDocumento4 páginasNeumans Systems Modelapi-482732223Ainda não há avaliações
- NCP For UDHDocumento3 páginasNCP For UDHTomohiro HorieAinda não há avaliações
- Case Study Medical WardDocumento4 páginasCase Study Medical WardFrancis Antonio Llenaresas QuijanoAinda não há avaliações
- Final Teaching PlanDocumento2 páginasFinal Teaching Planapi-352581650Ainda não há avaliações
- MeaslesDocumento32 páginasMeaslesYum C100% (2)
- ANEMIADocumento48 páginasANEMIAjomcy0% (2)
- Health AssessmentDocumento51 páginasHealth AssessmentJared Dela cruzAinda não há avaliações
- Post Op Case Studies StudentsDocumento19 páginasPost Op Case Studies StudentsRenie SerranoAinda não há avaliações
- Wound Essentials 2 The Treatment of Pressure Ulcers From Grade 1 To Grade 4Documento5 páginasWound Essentials 2 The Treatment of Pressure Ulcers From Grade 1 To Grade 4archanaAinda não há avaliações
- Administering Pulse OxDocumento2 páginasAdministering Pulse OxjepoiAinda não há avaliações
- At LTC N Theories Models 1Documento35 páginasAt LTC N Theories Models 1Darin BransonAinda não há avaliações
- Foreigh Body Airway Obstruction Management July 2019Documento1 páginaForeigh Body Airway Obstruction Management July 2019Feliros S. SanciangcoAinda não há avaliações
- Bedside TeachingDocumento23 páginasBedside TeachingBella HannaAinda não há avaliações
- MCN Test DrillsDocumento20 páginasMCN Test DrillsFamily PlanningAinda não há avaliações
- Practice Summary Paper For PortfolioDocumento9 páginasPractice Summary Paper For Portfolioapi-290938460Ainda não há avaliações
- A. Setting Up B. Inserting IV Utilizing The Dummy Arm C. Changing An IV Solution D. Discontinuing An IV InfusionDocumento7 páginasA. Setting Up B. Inserting IV Utilizing The Dummy Arm C. Changing An IV Solution D. Discontinuing An IV InfusionJerika Shane MañosoAinda não há avaliações
- Management of Patients With Neurologic Infections, Autoimmune Disorders & NeuropathiesDocumento92 páginasManagement of Patients With Neurologic Infections, Autoimmune Disorders & NeuropathiesejarnmdAinda não há avaliações
- NCP (Burn)Documento2 páginasNCP (Burn)Maricel R. ManabatAinda não há avaliações
- Admitting Patient: When Admitting A Patient What Are The Basic Procedures?Documento4 páginasAdmitting Patient: When Admitting A Patient What Are The Basic Procedures?diah ayuAinda não há avaliações
- Learning PlanDocumento5 páginasLearning PlansameenaesmailAinda não há avaliações
- Nurs 641 Case Study PresentationDocumento12 páginasNurs 641 Case Study Presentationapi-251235373Ainda não há avaliações
- Glasgow Coma ScaleDocumento13 páginasGlasgow Coma ScaleDanna Christine Gumboc PaguntalanAinda não há avaliações
- Case StudyDocumento9 páginasCase StudyPalwasha KhanAinda não há avaliações
- SOFA (Sequential Organ Failure Assessment) and PELOD (Pediatric LogisticDocumento5 páginasSOFA (Sequential Organ Failure Assessment) and PELOD (Pediatric LogisticvidyahamzahAinda não há avaliações
- SpectorDocumento6 páginasSpectorAmiLia CandrasariAinda não há avaliações
- Cystic HygromaDocumento2 páginasCystic HygromaAmal AlahmariAinda não há avaliações
- NURSES NOTES With CaseDocumento4 páginasNURSES NOTES With CaseGrape JuiceAinda não há avaliações
- Wound CareDocumento4 páginasWound CareChrisTine M. MoralesAinda não há avaliações
- NCM 114 Gerontology - WeeK 1Documento38 páginasNCM 114 Gerontology - WeeK 1Jmarie Brillantes Popioco0% (1)
- The Icd - 10 DictionaryDocumento10 páginasThe Icd - 10 DictionarySeraphin MulambaAinda não há avaliações
- Haemodialysis Access UKDocumento19 páginasHaemodialysis Access UKmadimadi11Ainda não há avaliações
- (JURNAL, Eng) A Retrospective Cohort Review of Prescribing in Hospitalised Patients With Heart Failure Using Beers Criteria and STOPP RecommendationsDocumento7 páginas(JURNAL, Eng) A Retrospective Cohort Review of Prescribing in Hospitalised Patients With Heart Failure Using Beers Criteria and STOPP RecommendationsAurellia Annisa WulandariAinda não há avaliações
- Stress WorkshopDocumento14 páginasStress Workshopapi-297796125Ainda não há avaliações
- Neonataljaundice 140128015601 Phpapp02Documento39 páginasNeonataljaundice 140128015601 Phpapp02Tina TalmadgeAinda não há avaliações
- Euthanasia and DNRDocumento44 páginasEuthanasia and DNRAtinder SranAinda não há avaliações
- M. Pharm Review NAPLEX38Documento1 páginaM. Pharm Review NAPLEX38JUSASBAinda não há avaliações
- Musni Theo Roi Ncm116a - DS MedwardDocumento2 páginasMusni Theo Roi Ncm116a - DS Medwardjovert davidAinda não há avaliações
- RetinoblastomaDocumento24 páginasRetinoblastomaMiguel Carlos Navarro Tacderan100% (1)
- Case-Presentation OTITIS MEDIADocumento22 páginasCase-Presentation OTITIS MEDIAJean nicole GaribayAinda não há avaliações
- Guidelines On Cleaning and Disinfection in GI Endoscopy: E.S.G.E. GuidelinesDocumento7 páginasGuidelines On Cleaning and Disinfection in GI Endoscopy: E.S.G.E. GuidelinesSailu KatragaddaAinda não há avaliações
- Stroke 2Documento8 páginasStroke 2Jarmy BjAinda não há avaliações
- Post Doc Proposal PDFDocumento9 páginasPost Doc Proposal PDFMaqsood RehmanAinda não há avaliações
- Module 01 - Introduction To Laboratory ManagementDocumento7 páginasModule 01 - Introduction To Laboratory ManagementBea Reen BurgosAinda não há avaliações
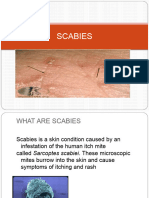
- ScabiesDocumento14 páginasScabiessyemiAinda não há avaliações
- Neonatal and Obstetric Risk Assessment (NORA) Pregnancy Cohort Study in SingaporeDocumento7 páginasNeonatal and Obstetric Risk Assessment (NORA) Pregnancy Cohort Study in SingaporePremier PublishersAinda não há avaliações
- Esophageal Cancer PDFDocumento16 páginasEsophageal Cancer PDFAJ AYAinda não há avaliações
- First Aid Book PDFDocumento47 páginasFirst Aid Book PDFHannan AliAinda não há avaliações
- DRP Registration Form V9.1 (PCNE Classification) : (ATC Code(s) )Documento4 páginasDRP Registration Form V9.1 (PCNE Classification) : (ATC Code(s) )briandiniAinda não há avaliações
- Stroke Mimics: Clinical and Radiological Evaluation: Poster No.: Congress: Type: Authors: KeywordsDocumento20 páginasStroke Mimics: Clinical and Radiological Evaluation: Poster No.: Congress: Type: Authors: KeywordsOrlin ZlatarskiAinda não há avaliações
- Vadim SentchoukDocumento42 páginasVadim SentchoukAnil KapuAinda não há avaliações
- Effects of Mouthpiece Use On Airway Openings and Lactate LevelsDocumento6 páginasEffects of Mouthpiece Use On Airway Openings and Lactate LevelsFábio LopesAinda não há avaliações
- Nursing Theory FlorenceDocumento19 páginasNursing Theory FlorencesrinivasanaAinda não há avaliações
- Florida Physician Database - Areas Includes Gainesville, Orlando and JacksonvilleDocumento20 páginasFlorida Physician Database - Areas Includes Gainesville, Orlando and JacksonvilleBhuvana RajendranAinda não há avaliações
- The Bioarcheology of Health Crisis. Infectious Disease in The PastDocumento23 páginasThe Bioarcheology of Health Crisis. Infectious Disease in The PastJosé OrtízAinda não há avaliações
- The REMAP-CAP InvestigatorsDocumento32 páginasThe REMAP-CAP InvestigatorsAaron Nureña JaraAinda não há avaliações
- EDITED - G9 - IPT of FRANCISCO & MACABABBADDocumento17 páginasEDITED - G9 - IPT of FRANCISCO & MACABABBADCHAROLF CARANGUIANAinda não há avaliações
- J of Ultrasound Medicine 2022 Demi New International GuidelinesDocumento36 páginasJ of Ultrasound Medicine 2022 Demi New International Guidelineslilo serranoAinda não há avaliações
- Chikungunya Fever - WHO FactSheetDocumento2 páginasChikungunya Fever - WHO FactSheetDr.SagindarAinda não há avaliações
- MSK CasesDocumento331 páginasMSK CasesRadio Resident100% (6)
- Love Life: How to Raise Your Standards, Find Your Person, and Live Happily (No Matter What)No EverandLove Life: How to Raise Your Standards, Find Your Person, and Live Happily (No Matter What)Nota: 3 de 5 estrelas3/5 (1)
- ADHD is Awesome: A Guide to (Mostly) Thriving with ADHDNo EverandADHD is Awesome: A Guide to (Mostly) Thriving with ADHDNota: 5 de 5 estrelas5/5 (2)
- The Age of Magical Overthinking: Notes on Modern IrrationalityNo EverandThe Age of Magical Overthinking: Notes on Modern IrrationalityNota: 4 de 5 estrelas4/5 (29)
- LIT: Life Ignition Tools: Use Nature's Playbook to Energize Your Brain, Spark Ideas, and Ignite ActionNo EverandLIT: Life Ignition Tools: Use Nature's Playbook to Energize Your Brain, Spark Ideas, and Ignite ActionNota: 4 de 5 estrelas4/5 (404)
- By the Time You Read This: The Space between Cheslie's Smile and Mental Illness—Her Story in Her Own WordsNo EverandBy the Time You Read This: The Space between Cheslie's Smile and Mental Illness—Her Story in Her Own WordsAinda não há avaliações
- Summary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedNo EverandSummary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedNota: 5 de 5 estrelas5/5 (81)
- Think This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BeNo EverandThink This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BeNota: 2 de 5 estrelas2/5 (1)
- Mindset by Carol S. Dweck - Book Summary: The New Psychology of SuccessNo EverandMindset by Carol S. Dweck - Book Summary: The New Psychology of SuccessNota: 4.5 de 5 estrelas4.5/5 (328)
- The Obesity Code: Unlocking the Secrets of Weight LossNo EverandThe Obesity Code: Unlocking the Secrets of Weight LossNota: 4 de 5 estrelas4/5 (6)
- The Body Keeps the Score by Bessel Van der Kolk, M.D. - Book Summary: Brain, Mind, and Body in the Healing of TraumaNo EverandThe Body Keeps the Score by Bessel Van der Kolk, M.D. - Book Summary: Brain, Mind, and Body in the Healing of TraumaNota: 4.5 de 5 estrelas4.5/5 (266)
- Summary: Outlive: The Science and Art of Longevity by Peter Attia MD, With Bill Gifford: Key Takeaways, Summary & AnalysisNo EverandSummary: Outlive: The Science and Art of Longevity by Peter Attia MD, With Bill Gifford: Key Takeaways, Summary & AnalysisNota: 4.5 de 5 estrelas4.5/5 (42)
- The Ritual Effect: From Habit to Ritual, Harness the Surprising Power of Everyday ActionsNo EverandThe Ritual Effect: From Habit to Ritual, Harness the Surprising Power of Everyday ActionsNota: 3.5 de 5 estrelas3.5/5 (3)
- Raising Mentally Strong Kids: How to Combine the Power of Neuroscience with Love and Logic to Grow Confident, Kind, Responsible, and Resilient Children and Young AdultsNo EverandRaising Mentally Strong Kids: How to Combine the Power of Neuroscience with Love and Logic to Grow Confident, Kind, Responsible, and Resilient Children and Young AdultsNota: 5 de 5 estrelas5/5 (1)
- The Courage Habit: How to Accept Your Fears, Release the Past, and Live Your Courageous LifeNo EverandThe Courage Habit: How to Accept Your Fears, Release the Past, and Live Your Courageous LifeNota: 4.5 de 5 estrelas4.5/5 (253)
- Dark Psychology & Manipulation: Discover How To Analyze People and Master Human Behaviour Using Emotional Influence Techniques, Body Language Secrets, Covert NLP, Speed Reading, and Hypnosis.No EverandDark Psychology & Manipulation: Discover How To Analyze People and Master Human Behaviour Using Emotional Influence Techniques, Body Language Secrets, Covert NLP, Speed Reading, and Hypnosis.Nota: 4.5 de 5 estrelas4.5/5 (110)
- Why We Die: The New Science of Aging and the Quest for ImmortalityNo EverandWhy We Die: The New Science of Aging and the Quest for ImmortalityNota: 4 de 5 estrelas4/5 (5)
- Outlive: The Science and Art of Longevity by Peter Attia: Key Takeaways, Summary & AnalysisNo EverandOutlive: The Science and Art of Longevity by Peter Attia: Key Takeaways, Summary & AnalysisNota: 4 de 5 estrelas4/5 (1)
- Cult, A Love Story: Ten Years Inside a Canadian Cult and the Subsequent Long Road of RecoveryNo EverandCult, A Love Story: Ten Years Inside a Canadian Cult and the Subsequent Long Road of RecoveryNota: 4 de 5 estrelas4/5 (45)
- Raising Good Humans: A Mindful Guide to Breaking the Cycle of Reactive Parenting and Raising Kind, Confident KidsNo EverandRaising Good Humans: A Mindful Guide to Breaking the Cycle of Reactive Parenting and Raising Kind, Confident KidsNota: 4.5 de 5 estrelas4.5/5 (170)
- Summary: Thinking, Fast and Slow: by Daniel Kahneman: Key Takeaways, Summary & Analysis IncludedNo EverandSummary: Thinking, Fast and Slow: by Daniel Kahneman: Key Takeaways, Summary & Analysis IncludedNota: 4 de 5 estrelas4/5 (61)
- Manipulation: The Ultimate Guide To Influence People with Persuasion, Mind Control and NLP With Highly Effective Manipulation TechniquesNo EverandManipulation: The Ultimate Guide To Influence People with Persuasion, Mind Control and NLP With Highly Effective Manipulation TechniquesNota: 4.5 de 5 estrelas4.5/5 (1412)
- How to ADHD: The Ultimate Guide and Strategies for Productivity and Well-BeingNo EverandHow to ADHD: The Ultimate Guide and Strategies for Productivity and Well-BeingNota: 1 de 5 estrelas1/5 (1)
- The Marshmallow Test: Mastering Self-ControlNo EverandThe Marshmallow Test: Mastering Self-ControlNota: 4.5 de 5 estrelas4.5/5 (59)