Escolar Documentos
Profissional Documentos
Cultura Documentos
Rational Antibiotic Therapy
Enviado por
dimcuslongusDescrição original:
Direitos autorais
Formatos disponíveis
Compartilhar este documento
Compartilhar ou incorporar documento
Você considera este documento útil?
Este conteúdo é inapropriado?
Denunciar este documentoDireitos autorais:
Formatos disponíveis
Rational Antibiotic Therapy
Enviado por
dimcuslongusDireitos autorais:
Formatos disponíveis
INFECTION
Rational Antibiotic Therapy
Andrew J H Simpson
Clinical assessment At the initial clinical assessment of an infected patient, the two most important considerations are the type of patient and the likely infecting organism. Several host factors need to be taken into account when selecting a suitable antimicrobial agent. The antibiotic susceptibility patterns for the likely infecting organism will help determine the choice of agent. Host factors Age: some drugs are contraindicated in children, such as the tetracyclines, because they may discolour the teeth. The quinolones are used with caution because of concerns over arthropathy, although they are probably safe. Renal function declines with age and creatinine clearance may be considerably reduced in the elderly, despite apparently normal serum urea and creatinine concentrations. High doses of drugs need to be used with caution. Renal and hepatic function: many drugs are metabolized or excreted via the liver or kidneys. Functional impairment of these organs may therefore substantially alter the pharmacokinetics of a drug. Aminoglycoside and glycopeptide antibiotics need to be used carefully even in mild renal failure. Even the -lactam agents (penicillins and cephalosporins) may cause toxicity (seizures) if used in high doses in renal impairment. The macrolide antibiotics (e.g. erythromycin) and chloramphenicol require cautious administration in liver impairment, as do metronidazole (in severe disease), rifampicin and isoniazid. Pregnancy: all drugs cross the placenta. Penicillins, cephalosporins and macrolides appear to be safe, but for most other agents caution is advisable. Aminoglycosides and tetracyclines should be avoided. Some drugs also enter breast milk, (e.g. trimethoprim, metronidazole and macrolides). Site of the infection: this will help determine the likely aetiology, and will influence the dose and duration of subsequent antibiotic therapy. Antibiotics need to achieve sufficient local concentration at the infected site for effective microbial killing to occur. Abscesses will require drainage if they are to be successfully treated, and necrotic material must be debrided. Presence of prosthetic material: infections related to prosthetic material rarely respond to antibiotic therapy alone and usually require removal of the device. Immune status: some patients will have underlying diseases (e.g. AIDS, haematological malignancies) that influence both the likelihood of an infection and its likely aetiology. Allergy: determination of previous allergic drug reactions, including antimicrobial agents, is an important part of the assessment of any patient. Failure to do so can have catastrophic consequences. Likely infecting agent Clinical assessment may allow a likely source of infection to be identified, and from this assumptions about the probable
Successful chemotherapy must be rational, and rational treatment demands a diagnosis. This may only be provisional, and it may later be proved wrong, but the treatment chosen should be based on some explicit assumption as to the nature of the disease process. This passage, from the second edition of Antibiotic and Chemotherapy by Garrod and OGrady, published in 1968, may be applied to all forms of drug treatment, and to antimicrobial therapy in particular. Antimicrobial drugs are targeted primarily at invading micro-organisms, against which they exhibit selective toxicity. Infection may occur at any site; therefore, therapeutic drugs must be distributed widely at appropriate concentrations. However, antibiotics may be toxic to the patient, may have other adverse effects, and often affect the normal flora of the skin, gut and mucous membranes. This can result in super-infection and, occasionally, drug resistance, which may affect the patient as well as having a wider ecological impact. Antibiotic resistance is becoming an increasingly important issue in many hospitals (e.g. the presence of methicillin-resistant Staphylococcus aureus, or MRSA) and there is no doubt that indiscriminate use of broad-spectrum agents contributes greatly to this problem. Patients who are unlucky enough to acquire an infection while in hospital (and this affects approximately 10% of patients in British institutions) usually require expensive new agents for treatment, and undergo prolonged hospital stays (at additional expense and inconvenience for everybody). All antimicrobial agents therefore require skilled rational prescription, in moderation, rather than ill-considered widespread use. Many institutions now have local antibiotic formularies and antibiotic policies in place, in order to educate prescribers, limit unnecessary use, avoid the development of antibiotic resistance and, importantly, to control costs. Antimicrobial agents are, in general, expensive drugs, and account for a substantial proportion of any hospitals drug budget. The following general principles, guiding choice and use of antimicrobial agents, apply to the treatment of bacterial, fungal, viral and parasitic infections. Use of these agents for prophylaxis of infection is discussed in a separate section.
Andrew J H Simpson is Consultant in Medical Microbiology at the Royal Free Hospital, London, UK. He qualied from Kings College Hospital and trained in microbiology at St Bartholomew's Hospital, London, UK. His research interests include melioidosis and the control of antibiotics in hospitals.
SURGERY
177
2002 The Medicine Publishing Company Ltd
INFECTION
aetiology may be made. Empirical treatment is aimed at these organisms. Clinical assessment can confidently predict a specific microbial aetiology in only a few infectious diseases, such as herpes zoster. More commonly, several possible organisms may be responsible. Community-acquired pneumonia is most commonly caused by Streptococcus pneumoniae, but organisms such as Mycoplasma and Legionella must be considered, particularly in severe disease. Cellulitis is likely to be caused by either S. aureus or Streptococcus pyogenes. Coliforms or enterococci cause the majority of urinary tract infections. Intra-abdominal infections are likely to be polymicrobial. Laboratory investigation Initially, most antibiotic prescribing is empirical. Ideally, the initial clinical assessment of the patient should be supported by laboratory investigations to establish a definitive microbiological diagnosis and to determine the susceptibility of the infection to various drugs, particularly in hospitalized and severely ill patients or when initial treatment is unsuccessful. However, culture and sensitivity results may take several days, so are not of immediate use. Nonetheless, appropriate samples, such as blood cultures, cerebrospinal fluid, pus, urine or sputum, should be taken before beginning chemotherapy, but should not delay treatment unnecessarily. In certain lifethreatening conditions (e.g. meningococcal meningitis) prompt administration of penicillin in the community at the first medical assessment can be life-saving. However, a Gram stain performed on appropriate samples may provide useful information about the likely aetiology and thus guide therapy. Collated susceptibility data also provide valuable epidemiological information on antibiotic resistance trends in the community or in specific hospital environments (e.g. intensive care). Amoxicillin resistance amongst coliforms causing urinary tract infections is common in many areas, to the extent that it can no longer be recommended as a first line empirical agent. The prevalence of MRSA is increasing in many UK hospitals. Multi-resistant Acinetobacter species have been a problem in some burns units for many years and are becoming problematic in other units too. These local patterns of resistance need to be taken into account when prescribing for hospital-acquired infections. Drug resistance is also increasing among non-bacterial pathogens. Candida albicans is showing reduced susceptibility to fluconazole, and intrinsically resistant species (e.g. Candida krusei) have become more common. Other considerations Route of administration Parenteral therapy this is indicated for the seriously ill patient when effective drug concentrations are required rapidly at the site of infection, when oral administration is contraindicated, or for agents that are not absorbed from the gut (e.g. aminoglycosides, glycopeptides). For many infections, patients can be switched to an oral formulation after 4872 hours if there is a satisfactory response. Oral drugs these are absorbed principally from the stomach and proximal small bowel. Absorption of acid-labile agents can be improved by using enteric-coated preparations, which delay drug release until they have passed through the stomach.
Intramuscular administration this is often painful and systemic distribution of drugs is less reliable than with intravenous administration. Topical antimicrobial agents: these are used only for the treatment of superficial skin infections, mucosal candidosis, middle ear and superficial ocular infections. Dosage regimens: the dose of an antibiotic will be influenced by several factors, including the severity of infection, age and weight of the patient. Standard texts such as the British National Formulary or the drug data sheets should be consulted. Encouraging compliance: administering drugs less frequently encourages compliance, particularly for oral agents. Length of treatment: there are few infections for which the duration of treatment has been clearly defined. Duration will vary depending on the site and severity of an infection, the causative organism and the patients response to treatment. Combination therapy A single agent is generally preferred to a multi-drug regimen. It reduces the risks of toxicity and interactions, and reduces the cost and inconvenience of treatment (thus improving compliance). Some antibiotic combinations are potentially antagonistic. However, there are circumstances in which combination therapy is appropriate or essential. Empirical therapy to cover several pathogens: this is a common indication for combination therapy. It applies particularly to acute and potentially life-threatening infections where the range of potential pathogens cannot be defined or covered by a single agent. Severe community-acquired pneumonia is treated with a combination of a -lactam and macrolide (e.g. ceftriaxone and clarithromycin). Brain abscesses are treated with combinations such as ceftriaxone and metronidazole, or benzylpenicillin, chloramphenicol and metronidazole. Treatment of mixed infections: intra-abdominal infections are usually caused by a mixture of aerobic and anaerobic microorganisms (a reflection of the normal gut flora). Combined therapy with a broad-spectrum, Gram-negative agent (e.g. ceftriaxone or an aminoglycoside) and metronidazole (a broad-spectrum anaerobic agent) provides cover against most pathogens. Amoxicillin is often added to provide activity against enterococci. Synergy: some drug combinations are synergistic. streptococcal endocarditis is treated with penicillin and gentamicin, despite gentamicin having no activity against streptococci; the two agents are more effective than penicillin alone. Broadening of antimicrobial activity: several commercially available agents are combinations of an antibiotic and an enzyme inhibitor. The enzyme inhibitor may be active against bacterial enzymes which would destroy the antibiotic, such as -lactamase inhibitors, giving the antimicrobial agent clinically useful activity against organisms which would otherwise be
SURGERY
178
2002 The Medicine Publishing Company Ltd
INFECTION
regarded as resistant. This may allow the avoidance of additional, potentially toxic antibiotics, such as gentamicin. Examples of such combinations include co-amoxiclav (amoxicillin and clavulanic acid) and piperacillin with tazobactam. Some agents contain inhibitors active against human enzymes, to reduce metabolism of the antibiotic (such as cilastatin with imipenem) and extend the half-life. Avoiding drug resistance: by using combinations of antibiotics (e.g. quadruple therapy for tuberculosis) the emergence of drug-resistant strains, produced as a result of DNA mutations, is reduced significantly. Similar considerations have been applied to the management of AIDS patients with highly active anti-retroviral therapy, and are now being applied to the treatment of malaria. Response to treatment It is important to monitor the patients clinical response to antimicrobial therapy (e.g. reduction of fever) and by monitoring blood white cell counts and C-reactive protein concentrations where appropriate. Adverse effects, including antibiotic-related diarrhoea or super-infections, must also be considered. Patients may fail to respond to treatment for many reasons, but this may be due to an organism which is not susceptible to the empirical antimicrobial regimen. Hence, the checking of microbiology culture results and susceptibility tests should not be overlooked. Microbiological information obtained from samples taken at the time of admission may allow the drug regimen to be altered later (e.g. to a single agent). It is also good practice to modify treatment based on culture results when these indicate that a narrower-spectrum agent would be suitable (e.g. switching to benzylpenicillin for meningococcal meningitis rather than continuing with ceftriaxone). A lack of response is often not a failure of antibiotics, but relates instead to the host factors outlined previously. Some older laboratory tests used to monitor treatment, such as the serum bactericidal test, are now largely obsolete. Drug monitoring: determination of serum antibiotic levels, particularly for the aminoglycosides (gentamicin, amikacin and netilmicin) and vancomycin, both to ensure therapeutic levels are being achieved and to minimize toxicity, is vitally important. The exact timing and nature of the samples required for assay varies with both the drug and the dosing regimen used.
Sources of Surgical Infection
Garth Dixon
Prior to the introduction of aseptic technique, sterilisation of surgical equipment and clean operating environment, infections associated with surgery were both commonplace and had disastrous consequences. However, with modern surgical practice, aseptic technique and the development of antimicrobial agents, there has been a great reduction in postoperative infections, but these still remain a significant health care problem. In recent years, the increasingly complex nature of operations (such as organ transplants) and changes in host characteristics, such as an increasingly ageing population, immunosuppressed individuals, together with the emergence of multi-drug resistant organisms, has generated particular challenges for the surgeon, physician and microbiologist alike.
Surgical site infections
Denitions Surgical site infections (SSIs) not only have an attributable mortality, but also place an enormous burden on health care systems in terms of increased length of stay, use of antibiotics, re-operations or cancelled operations. SSIs are classified as either superficial, deep incisional or organ/space (Figure 1). Numerous studies have attempted to identify which patient or operative characteristics may be associated with an increased risk of postoperative infections, including SSIs. A risk factor refers specifically to a variable or characteristic that has a significant independent association with the development of SSI after a specific operation. This may allow identification of susceptible individuals and strategies for preventing such infections. These can usually be identified only after extensive epidemiological studies using multivariate analyses. There are three broad categories of variables that have been used as reliable predicators of SSI risk: (1) those that estimate the intrinsic degree of microbial contamination of a surgical site, (2) those that measure the duration of the operation, and (3) those that serve as markers for host susceptibility. The most widely accepted scheme for estimating the intrinsic degree of microbial contamination of surgical sites was first developed in 1964, and was modified by the Center for Disease Control in USA in 1982 (Figure 2). However, stratifying risk of SSI according to wound class alone is not recommended. The National Nosocomial
FURTHER READING British National Formulary (BNF): Latest edition. Moellering R C, Jr. Principles of Anti-infective Therapy. In: Mandell G L, Bennett J E, Dolin R, eds. Mandell, Douglas, and Bennetts Principles and Practice of Infectious Diseases. 5th edition. Philadelphia: Churchill Livingstone, 2000: 22335. OGrady F W, Lambert H P, Finch R G, Greenwood D, eds. Antibiotic and Chemotherapy: Anti-infective agents and their use in therapy. 7th edition. Edinburgh: Churchill Livingstone, 1997.
Garth Dixon is Specialist Registrar in Medical Microbiology at the Royal Free Hospital, London, UK. He qualied from Bristol University and trained in paediatric medicine at St Thomas Hospital and Guys Hospital in London, UK. He studied for his thesis on meningococcal disease at the Institute of Child Health at Great Ormond Street Hospital, UK, prior to starting training in microbiology. His main research interests are host inammatory responses in severe bacterial sepsis.
SURGERY
179
2002 The Medicine Publishing Company Ltd
INFECTION
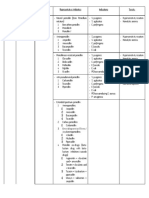
Criteria for denition of SSI
Supercial incisional SSI Infection occurs within 30 days of operation and involves only skin or subcutaneous tissues and at least one of the following: Purulent discharge from the wound Organisms obtained from aseptically obtained culture of uid or tissue Signs of infection: pain or tenderness, localised swelling, redness or heat and supercial lesion is deliberately opened by surgeon unless incision is culture-negative Clinical diagnosis of supercial SSI by attending doctor Deep incisional SSI Infection occurs within 30 days of operation if no implant is left in place or within 1 year. If implant is in place and the infection appears to be related to the operation and at least one of the following: Purulent discharge from the deep incision, but not from the organ or space component of the site A deep incision spontaneously dehisces or is deliberately opened by a surgeon when the patient has at least one of the following signs or symptoms: fever (> 38 C), localised pain, tenderness, unless site is culture-negative An abscess or other evidence of infection involving the deep incision is found by direct examination, during re-operation, or by histopathological or radiological examination Diagnosis of a deep incisional SSI by surgeon or attending physician NB: An infection that involves both supercial and deep incision sites should be reported as a deep SSI. An organ/space SSI that drains through the incision site should be reported as a deep incision SSI Organ/Space SSI Infection occurs within 30 days of operation if no implant is left in place or within 1 year. If implant is in place and the infection appears to be related to the operation and infection involves any part of the anatomy (e.g. organs or spaces), other than the incision, which was opened or manipulated during the operation, and at least one of the following: Purulent discharge from a drain that is placed through a stab wound into the organ/space Organisms isolated from an aseptically obtained culture or tissue in the organ/space An abscess or other evidence of infection involving the organ/ space that is found on direct examination, during re-operation, or by histopathological or radiological examination Diagnosis of an organ/space SSI by surgeon or attending physician 1 2
Surgical wound classication
Clean/Class I An uninfected operative wound in which no inammation is encountered and the respiratory, alimentary, genital, or uninfected urinary tract is not entered. In addition, clean wounds are primarily closed and, if necessary, drained with closed drainage. Operative incisional wounds that follow blunt trauma should be included in this category An operative wound in which the respiratory, alimentary, genital or urinary tracts are entered under controlled conditions and without unusual contamination. Specically, operations involving the biliary tract, appendix, vagina, and oropharynx are included in this category, provided no evidence of infection or major break in technique is encountered Open, fresh, accidental wounds. In addition, operations with major breaks in sterile technique (e.g. open cardiac massage) or gross spillage from the gastrointestinal tract, and incisions in which acute, nonpurulent inammation is encountered are included in this category Old traumatic wounds with retained devitalised tissue and those that involve existing clinical infection or perforated viscera. This denition suggests that the organisms causing postoperative infection were present in the operative eld before the operation
Cleancontaminated/ Class II
Contaminated/ Class III
Dirty-infected/ Class IV
index scores will be developed that are procedure-specific. However, there is extensive published data on associations with SSIs using univariate analysis. Other operative and patient characteristics that have been associated with the increased risk of developing SSIs are listed in Figure 4. Epidemiology The recent English Nosocomial Infection National Surveillance Scheme (NINSS) reported that the overall incidence of SSIs was 4.3% of all surgical operations, of which 25% were serious deep or organ/space infections. According to category of surgical procedure, limb amputation and large bowel surgery most frequently lead to infection. In the USA, SSIs are the third most common nosocomial infection in hospitalized patients. Also, 2.6% of all operations reported an SSI, of which two-thirds were confined to the incision site, but the remaining one-third involved deep organ or space infections. When surgical patients with nosocomial SSI died, 77% were related to the infection and most had serious infections involving deep organ spaces accessed during the operation. The 1999 Incidence des infections du site opratoire (INCISO) surveillance from France found that, over a three-year period in 38,973 surgical patients, 3.4%
Infections Surveillance (NNIS) risk index is one accepted operation-specific score that can be applied to prospectively collected surveillance data (Figure 3). However, this method has problems, as it may not adequately discriminate SSI risk for all types of operations. It is likely that modified NNIS risk
SURGERY
180
2002 The Medicine Publishing Company Ltd
INFECTION
The NNIS risk index for SSI ASA score of 3, 4 or 5 An operation classied as contaminated or dirty An operation with the duration of surgery greater than T hours, where T is approximately the 75th percentile of duration of surgery
American Society of Anaesthesiologists (ASA) preoperative assessment score Normally healthy person Patient with mild systemic disease Patient with severe disease that is not incapacitating Patient with incapacitating systemic disease that is a constant threat to life Moribund patient who is not expected to survive for 24 hours with or without an operation
NB: Each of the risk factors described above contributes one point to the risk index, ranging from 0 (none of the risk factors present) to 3 (all of the risk factors present)
Sources of microbial infection Factors that may inuence risk of post-surgical infections
Patient Age Nutrition Diabetes mellitus Smoking Obesity Co-existent infections at a remote body site Colonization with particular micro-organisms Immunosuppression Length of preoperative stay Blood transfusion Anaemia Malignancy Operation Category of surgical procedure (large intestine and limb amputation high risk) Skin asepsis Preoperative shaving Preoperative skin preparation Duration of procedure Antimicrobial prophylaxis Operating room ventilation Inadequate sterilization of instruments Foreign material in surgical site Surgical drains Surgical technique Poor haemostasis Failure to obliterate a dead space Duration of surgical scrub Tissue trauma 4
Endogenous sources Since most surgical infections are derived from the patients own normal flora, an appreciation of the nature of human normal flora is critical (Figure 5). All micro-organisms have pathogenic potential, and whether they cause infection or not is dependent on numerous factors. Surgery, by its very nature, causes a breech in both physical and immunological barriers, which can be rapidly exploited by micro-organisms. Contamination of the surgical site appears to be a necessary precursor to developing an SSI. This has been conceptualized according to the formula: Dose of bacterial contamination virulence = Risk of SSI Resistance of patient The risk of SSIs increases markedly when contamination of tissue is > 105 micro-organisms per gram of tissue. However, the dose required may be much less when a foreign body is involved (such as sutures) and even fewer in the case of prosthetic implants. Microbial factors The degree of damage induced by particular micro-organisms is dependent on a number of virulence factors that facilitate attachment and invasion of host tissues, induce tissue damage or evade the host immune and inflammatory responses. Staphylococcus aureus (S. aureus) in particular stands out as the most common agent responsible for SSIs in all the large scale UK, European and US studies. S. aureus produces numerous potent enzymes (such as hyaluronidase and lipases) which can degrade connective tissue. It can also produce toxins that are directly cytotoxic, whilst others may have superantigen activity (e.g. toxic shock syndrome toxin-1). Staphylococci in particular bind well to subepithelial tissues by connecting to extracellular membrane molecules (such as fibronectin), which may explain why they have a propensity to colonize and infect wounds. In addition, staphylococci produce extracellular matrix polysaccharide which renders them resistant to the activity of phagocytes and antibiotics. These can rapidly form a biofilm on intravascular devices, intracerebral shunts and prosthetic devices. Bacteria at the base of the biofilm become quiescent and therefore not susceptible to the effects of cell-wall-active antibiotics such as -lactams and glycopeptides. -haemolytic
patients acquired a SSI, of which 568 died. Furthermore, there may be some under-reporting of hospital-acquired SSIs (and other infections) in patients who develop symptoms after discharge from hospital. For this reason, it is essential that primary health care surveillance systems should include nosocomial infection surveillance schemes.
SURGERY
181
2002 The Medicine Publishing Company Ltd
INFECTION
Normal body ora
Anatomical site Head and neck Skin Nasal cavity Oral cavity and nasopharynx Thorax (including axilla) Oesophagus, stomach, jejunum Large intestine Female genital tract Skin of lower limbs and groin 5 Flora Staphylococci (aureus and coagulase-negative), streptococci, propionobacter, corynebacteria Staphylococci (including aureus) Staphylococci, streptococci (including pneumococci), Neisseria species, haemophilus, corynebacteria, anaerobes Staphylococci (aureus and coagulase-negative) Nasopharynx ora, Gram-negative rods, including Enterobacteriaeciae occasionally, lactobacilli when fasting Aerobic Gram-negative rods, mainly Enterobacteriaciae, enterococci, anaerobes-bacteroides, Clostridium, yeasts Large bowel ora, staphylococci (including aureus), streptococci (including -haemolytic group B) lactobacilli, corynebacteria Staphylococci (aureus and coagulase-negative), occasionally large bowel ora in groin area
streptococci (especially Lancefield group A, but also C and G) can cause devastating SSIs, including cellulitis and necrotizing deep tissue infections. Group A streptococci produce a plethora of enzymes and toxins (including streptokinase, DNA-se, hyaluronidase and streptolysin) all of which can produce tissue damage. They also produce potent exotoxins that have specific inflammatory effects and can be associated with toxic shock syndrome. Clostridium species are capable of producing gas gangrene, mostly by direct inoculation of organisms or spores into wounds, and were frequent causes of infections in wounds acquired outdoors (e.g. military conflict, sports or farming). However, they can occasionally cause postoperative infections, especially in operations involving the perineum or gallbladder and can also infect implants. Clostridium perfringens in particular is highly toxic, and can produce a number of toxins which can cause haemolysis and tissue necrosis, in addition to gas formation. Gram-negative bacteria, such as members of Enterobacteriaceae (such as E. coli, Klebsiella and Proteus), possess lipopolysaccharide, which can trigger a cascade of inflammatory responses, including cytokine release, procoagualant activity and endothelial dysfunction that, in addition to other virulence factors, can result in multi-organ dysfunction syndrome with a high mortality. Although the distribution of different types of organisms causing SSIs have not changed dramatically over the last decade, there have been some notable trends. As Figure 6 shows, the incidence of Candida albicans has increased, which may reflect greater numbers of debilitated and immunocompromised patients, and the use of broad-spectrum antibiotics. However, it is the continued increase in the prevalence of multi-drug resistant strains which is most striking. This is particularly true in the case of S. aureus, since more than half the S. aureus isolates causing SSIs are methicillin-resistant (MRSA). Although there may be some difference in virulence between strains, MRSA has the same pathogenic potential as methicillin-sensitive S. aureus. However, it can be much more difficult and costly to treat. The same also applies to the extended -lactamase Gram-negative Enterobacteriaceae (such as E. coli, Enterobacter and Klebsiella species).
Distribution of pathogens isolated from SSIs, NNIS, 198696
Percentage isolates 198689 199096 (N=16,727) (N=17,671) Pathogen Staphylococcus aureus Coagulase-negative staphylococci Enterococus species Escherichia coli Pseudomonas aeruginosa Enterobacter species Proteus mirabilis Klebsiella pneumoniae Streptococcal species Candida albicans Group D streptococci (e.g. milleri) Other Gram-positive aerobes Bacteroides fragilis 17 12 13 10 8 8 4 3 3 2 20 14 12 8 8 7 3 3 3 3 2 2 2
Pathogens representing less than 2% not included. Source: Mangram A J, Horan T C, Pearson M L, Silver L C, Jarvis W R. Guideline for prevention of surgical site infection, 1999. Hospital Infection Control Practices Advisory Committee. Infect Control Hosp Epidemiol 1999; 20: 25078.
The establishment of a commensal relationship between the host and microbial world is both complex and still poorly understood. However, this relationship is constantly changing and dynamic. Patients can be rapidly colonized with organisms from the hospital environment, which is important since colonization is in most cases a prerequisite for invasive disease. Microbial surveillance systems are thus essential to monitoring trends in particular hospitals, wards and specialties. The site of operation is also important when considering the likely pathogens associated with an SSI. Thus, when the skin is incised, deeper tissue is exposed to micro-organisms (e.g.
SURGERY
182
2002 The Medicine Publishing Company Ltd
INFECTION
staphylococci). However, if the incision is near the groin or perineum, then contamination can be with faecal flora (e.g. anaerobes and enterococci). If intestinal viscera are opened, then Gram-negative coliforms, enterococci and anaerobes are more likely to be pathogens. In addition to these direct mechanisms, seeding of the operation site from a distant site source in the patient has been reported, and this is particularly important in prostheses and implants. Exogenous sources There have been outbreaks of MRSA infections directly attributable to a single surgeon, but other health care workers (HCW) can be responsible, especially where hand hygiene practice is poor. Some cross-infection may be airborne, as has occurred with some HCW who have been colonised rectally, vaginally, or on the skin with group A streptococci, causing outbreaks of SSI. Operating room air can be a source, either from particulate matter harbouring bacteria, or spores or skin cells from personnel. This is very important in ultra-clean surgery (such as implantation of prostheses) where only very small numbers of organisms are required to cause infections, often with devastating consequences and need for prosthesis removal and revision. Similarly, infection may be acquired from inadequately sterilized tools, instruments and materials. Some of the more unusual examples include contaminated dressings, gel used for ultrasound examination, and even contaminated disinfection solutions. Many of these can include organisms able to live in the environment, such as Pseudomonas, Klebsiella, S. aureus and Acinetobacter species. When pathogens have been isolated, formal epidemiological and microbiological investigations are required to investigate the source. This may entail environmental testing of wards, floors, curtains, water sources, including sinks and tap water. Recent concerns about the potential for acquiring new variant CJD acquired intraoperatively has lead to a change in procedures, such as providing disposal instrumentation for patients having certain operations (e.g. tonsillectomy). Host factors associated with an increased risk of SSIs Diabetes Diabetics appear to be susceptible to a number of postoperative infections, including SSIs. Whether diabetes is independently associated with an increased incidence of SSIs has been difficult to assess because of the large number of confounding variables. There is evidence that diabetes mellitus (even previously undiagnosed) increases patients risk of SSI after cardiothoracic surgery. Steroids Patients who have received steroids, especially long-term, and other immunosupressive agents may be at risk of developing SSIs, but the evidence is contradictory. Malnutrition and preoperative feeding It is widely believed that protein calorie malnutrition can be associated with an increased incidence of postoperative infections and impaired wound healing. Epidemiological studies and multivariate analyses have failed to show a consistent link between protein calorie malnutrition and increase in the risk of
SSIs following surgery. Moreover, there has been no consistent benefit shown in administration of total parenteral feeding preoperatively in reducing SSIs. However, given that nutritional support (both pre- and postoperatively) may ameliorate the numerous other metabolic complications associated with major elective surgery in the severely malnourished, there may be scope to assess SSIs risk and other postoperative infective complications in randomized trials. Nasal S. aureus colonization S. aureus is carried in up to 30% of normal healthy people, and is one of the most common causes of intravascular device infections. Preoperative nasal carriage with this organism is associated with an increased risk of SSIs. It is the single most powerful independent risk factor for SSI following cardiothoracic and orthopaedic implant surgery. What is unclear is whether eradication of nasal carriage significantly alters this risk. One study suggested that preoperative application of mupirocin to the nose of patients regardless of carrier status reduced the risk of SSIs after cardiothoracic surgery. However, these rates were compared to historical controls. A recent, randomized, double-blind, placebo-controlled trial was conducted to determine whether intranasal treatment with mupirocin reduced the rate of S. aureus infections at surgical sites and prevented other nosocomial infections. This study concluded that prophylactic intranasal application of mupirocin did not significantly reduce the rate of S. aureus surgical-site infections overall, but did significantly decrease the rate of all nosocomial S. aureus infections among the patients who were S. aureus carriers. Age and gender In developed nations, increasing life expectancies have meant that larger numbers of elderly patients are undergoing surgical procedures. Evidence suggests that infection in the elderly (particularly in the > 70 years age bracket) is associated with a high mortality. There is no significant difference in overall mortality from infection after surgery between the sexes. Interestingly, in one large study, mortality from nosocomial pneumonia was significantly higher in women rather than men, even after adjusting for co-morbidity. Host inammatory and immune responses Surgery, depending on the extent and nature of the procedure, can have profound effects on host immune and inflammatory responses. This can affect neutrophil function, endothelial and complement activation, and induce a procoagulant state. There have been great advances in the understanding of the pathophysiological mechanisms underlying host response to infection, inflammation and injury. For example, cardiopulmonary bypass can induce a state of immunological anergy or unresponsiveness, which may have profound effects on subsequent inflammatory and immune processes. Moreover, it seems that some of the inflammatory consequences of major surgery may be mediated by host-derived molecules such as heat shock proteins (HSPs) released as a result of cellular damage. Fascinatingly, it may be that the same host receptors that recognize and respond to microbial danger signals, such as lipopolysaccharide (or endotoxin), may also respond to HSPs.
SURGERY
183
2002 The Medicine Publishing Company Ltd
INFECTION
Further knowledge of this process may lead to new therapies that can modulate inflammatory responses as a result of surgery or trauma. Other evidence suggests that certain polymorphisms in genes critical to regulating immune and inflammatory responses may contribute to an increased susceptibility to nosocomial or postoperative infections, or severity of infection once established. In the future, patients may be identified preoperatively as having a particular risk for infection or the development of multi-organ dysfunction syndrome. Operative factors The quality of the surgical environment is of paramount importance in reducing the risk of SSIs. Outbreaks of SSIs caused by highly virulent bacteria (such as -haemolytic group A streptococcus and MRSA) from colonizing operative personnel have occurred. Microbial contamination can come from dust, skin squames, respiratory droplets and other airborne particulate matter (e.g. lint, spores). The microbial burden is directly related to the number of personnel moving about the operation room, hence traffic must be kept to a minimum. Operating rooms should be kept at positive pressure with respect to adjacent rooms, so that air movement moves from clean to less clean. Airflow must be effectively monitored, and any failure reported and immediately investigated. It has been shown that the use of both ultraclean air and antimicrobial prophylaxis can reduce the risk of deep SSIs following orthopaedic implant surgery. In all cases, there should be a minimum of 20 air changes per hour, of which 20% should be fresh, and relative humidity between 30 and 60%, with temperature between 18 and 24o C. Microbial air sampling (sometimes called slit sampling, depending on the method used) should be carried out, especially in order to commission a theatre after cleaning, building, renovation, or filter changes. The surfaces of the operating environment are rarely implicated as sources of SSIs. However, they should be made of a material that is both non-porous and easy to clean. Preoperative stay Whilst the length of preoperative stay is often suggested to increase the risk of nosocomial infection, this is confounded by factors such as severity of illness, and other pre-existing medical conditions that may require investigation and treatment. Multivariate analyses of a large cohort of patients with SSIs found the length of preoperative stay to be an independent risk factor for developing a SSI. Where possible, patients should be admitted the night before or even on the day of the procedure. Increasing use of day case operations, and less invasive techniques that reduce operation time and surgical insult, will reduce the overall length of stay in hospital. Length of operation The duration of operation is a likely risk factor for acquiring a SSI, and is included in both NNIS and study of the efficacy of nosocomial infection control (SENIC) risk stratification scores. However, it is difficult to disaggregate this risk from other co-morbid variables, such as disease severity, poor surgical technique or inadequate haemostasis, that may contribute to the longer duration of operation. However, unnecessary delays must be prevented. There is evidence that hypothermia (which
is more likely to occur during long operations) can increase the risk of SSI, and that body warming can reduce this risk. Co-existent infections at a remote body site Such infections definitely increase the risk of post-surgical infections. These may range from SSIs to urinary tract infections and respiratory tract infections. In the emergency situation, it may not be possible to delay operation. In elective surgery this may be necessary whilst treatment occurs.
Non-SSI post-surgical infection
Bacteraemia, including intravascular device infections Hospital-acquired bacteraemia (HAB) is a significant cause of mortality and morbidity world-wide. The National Surveillance of Hospital-Acquired Bacteraemia in English Hospitals showed that HAB occurred in 3.6 patients/1000 admissions or 0.6 bacteraemias per 1000 patient days. Six specialties accounted for 72% of all bacteraemia, the highest being general ICU (9.6 HAB/1000 patients days, including surgical patients). The figures for general surgery are 0.8 HAB/1000 patient days and 1.1 HAB/1000 patient days for cardiothoracic surgery. Two-thirds of all HAB had a source known to be associated with an intravascular device (usually central venous line). Half the isolates were staphylococci, of which 24% were S. aureus, and half were MRSA. Detailed guidelines now exist for the management and prevention of intravascular catheter-related infections. Strategies designed to reduce the risk of these infections have shown to be positive, based on the multiple approach prevention strategy, and the clarification of techniques on insertion and maintenance of central vascular devices. The importance of basic hand hygiene and aseptic technique in both the insertion and care of intravenous catheters is paramount. Pneumonia Lower respiratory tract infection is common post-surgery. Nosocomial pneumonia occurs 48 hours after admission to hospital and occurs in up to 1% of all patients. It is common on the ICU and surgical high-dependency units (SHDUs), particularly in ventilated patients, and accounts for about 40% of surgical intensive care infections; it is an independent risk factor for death on the intensive therapy unit (ITU). Ventilatorassociated pneumonia (VAP) is a complication of intubation and mechanical ventilation. Early-onset VAP occurs in the first 72 hours and is likely to be caused by community-acquired upper respiratory tract organisms such as Streptococcus pneumoniae, Moraxella catarrhalis and Haemophilus influenzae. Late onset VAP (> 72 hours) is associated with aerobic Gram-negative bacteria such as Pseudomonas, Acinetobacter, E. coli and Klebsiella species. In addition, S. aureus is an important cause of both early- and late-onset VAP. The incidence of VAP and nosocomial pneumonia with multi-drug resistant bacteria (including aminoglycoside-resistant and extended -lactamase producing Enterobactericiae and MRSA) has been steadily increasing over the last 20 years. It seems that the essential steps are colonisation of the patient with potentially pathogenic bacteria, followed by aspiration of gastric and oropharyngeal contents. Severely ill and ventilated
SURGERY
184
2002 The Medicine Publishing Company Ltd
INFECTION
patients have decreased gastric acidity and impairment of oral clearance mechanisms, which leads to increased bacterial colonization of stomach, oropharynx and proximal small intestine. However, recent evidence suggests that the crucial site of colonization (with respect to the risk of VAP) is the oropharynx itself, rather than the stomach. Microbiological monitoring of oropharyngeal flora in ventilated patients is an important guide to the identity of likely pathogens, and their antimicrobial sensitivities, associated with VAP. Recent work has emphasized that in patients with VAP, bronchoscopy, followed by lavage or protected specimen brushings and quantitative microbiological counts, has been shown to improve outcome and reduce unnecessary antibiotic usage. However, these invasive practices are not in widespread use on ITUs or SHDUs. Further studies, evaluating the use of quantitative cultures from endotracheal aspirates, which are simpler, less invasive and cheaper, would seem prudent. In addition, a number of preventive strategies aimed at reducing incidence of VAP, such as subglottic aspiration, use of antiseptic (e.g. chlorhexidine) oropharyngeal decontamination, and treating patients in a semi-recumbent position, require further evaluation by largescale prospective studies. The role of antibiotic prophylaxis in preventing lower respiratory tract infections in ventilated patients remains controversial, with some studies showing a reduction of mortality in ICU (including surgical patients). It may be that certain groups of patients who are most prone to early-onset VAP (such as head injury) may benefit from a short course of systemic antibiotic prophylaxis. The prolonged use of systemic broad-spectrum antimicrobials in an attempt to reduce the risk of VAP (or any other nosocomial infection) is rarely justified (except in special circumstances, such as profound immunosuppression) and also will select for fungi, such as Candida and multi-drug resistant bacteria. Surgical patients not on ITU are also at risk of nosocomial pneumonia, either because of intubation and ventilation in surgery, or previous stay on ITU/SHDU, or other pre-existing pathology, such as chronic obstructive pulmonary disease, being elderly, and immunosuppression. The identity of the likely pathogens must take into account the length of stay in hospital, recent colonization of micro-organisms (such as multi-drug resistant bacteria). Surgical patients are also prone to airborne and fomite transmissible respiratory tract viruses such as influenza and respiratory syncytial virus. Clues to these may include seasonality, clinical features such as coryza, or chest x-ray suggestive changes, illness in HCWs and relatives. In these cases, rapid diagnosis can be achieved by immunofluorescence techniques from nasopharyngeal aspirates. Although treatment options for established disease is limited, they are important to recognize, since they will be a cross infection hazard and certain groups of patients may benefit from anti-viral prophylaxis. UTIs UTIs are responsible for 30% of all nosocomial infections, and are associated with urethral catheterization in the majority of cases. Up to 30% of catheterized patients develop bacteruria, and up to 6% of these develop UTI. The risk of developing UTI increases by 5% per day of catheterization. One to four per cent of patients with a UTI progress to bacteraemia, of which 1330% will die. A significant minority of patients have no
classical UTI symptoms and may be asymptomatic. The most prevalent causative organisms are E. coli, Enterococcus species, Candida albicans, Klebsiella and Pseudomonas aeruginosa. Adherence to recently published guidelines on the prevention of nosocomial UTIs is likely to reduce the high rates of such infections. Removal of short-term urinary catheters (as soon as possible) is the most effective way of reducing the incidence of nosocomial UTIs. In large-scale studies, there were significant numbers of cases where urinary catheterization was not indicated in the first instance or was prolonged unnecessarily. Alternative methods to urethral catheterization, such as external collection devices, and a suprapubic device where long-term catheterization is envisaged, should be considered. Good aseptic technique during insertion and maintenance of catheters is essential. The most common error in urinary catheter management has been found to be opening of the closed drainage system. Poor hand hygiene, inadequate training, supervision and adherence to sterile technique is a particular problem in care of short-term urethral catheters. Cross-infection with multi-drug resistant bacteria is a potential hazard in catheterized patients where poor practice occurs. Again, routine use of antimicrobials to treat colonized catheters is likely to be either ineffective or even harmful. Removal of catheter and use of directed antimicrobial cover during re-insertion is warranted.
Conclusions
Prevention of nosocomial infections is not only highly desirable for patients, but is now seen as a major political priority. Guidelines and protocols for basic infection control practice (such as basic handwashing) and written protocols for the safe insertion and maintenance of devices such as intravascular catheters, should be widely available and adhered to. Close liaison between the surgical team and microbiologists, infection control team, ward managers and nursing staff is essential to proper functioning of high quality surgical service. There should also be a co-ordinated, multidisciplinary approach where accountability is clearly defined, and performance is regularly monitored, such as partaking in regional and national SSI surveillance schemes.
FURTHER READING Koeman M, van der Ven A J, Ramsay G, Hoepelman I M, Bonten M J. Ventilator-associated pneumonia: recent issues on pathogenesis, prevention and diagnosis. J Hosp Infect 2001; 49: 15562. Mangram A J, Horan T C, Pearson M L, Silver L C, Jarvis W R. Guideline for prevention of surgical site infection, 1999. Hospital Infection Control Practices Advisory Committee. Infect Control Hosp Epidemiol 1999; 20: 25078. Mermel L A, Farr B M, Sherertz R J et al. Guidelines for the management of intravascular catheter-related infections. Clin Infect Dis 2001; 32: 124972. Panknin H T, Althaus P. Guidelines for preventing infections associated with the insertion and maintenance of short-term indwelling urethral catheters in acute care. J Hosp Infect 2001; 49: 1467.
SURGERY
185
2002 The Medicine Publishing Company Ltd
Você também pode gostar
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryNo EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryNota: 3.5 de 5 estrelas3.5/5 (231)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)No EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Nota: 4.5 de 5 estrelas4.5/5 (119)
- Never Split the Difference: Negotiating As If Your Life Depended On ItNo EverandNever Split the Difference: Negotiating As If Your Life Depended On ItNota: 4.5 de 5 estrelas4.5/5 (838)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaNo EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaNota: 4.5 de 5 estrelas4.5/5 (265)
- The Little Book of Hygge: Danish Secrets to Happy LivingNo EverandThe Little Book of Hygge: Danish Secrets to Happy LivingNota: 3.5 de 5 estrelas3.5/5 (399)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyNo EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyNota: 3.5 de 5 estrelas3.5/5 (2219)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeNo EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeNota: 4 de 5 estrelas4/5 (5794)
- Team of Rivals: The Political Genius of Abraham LincolnNo EverandTeam of Rivals: The Political Genius of Abraham LincolnNota: 4.5 de 5 estrelas4.5/5 (234)
- The Emperor of All Maladies: A Biography of CancerNo EverandThe Emperor of All Maladies: A Biography of CancerNota: 4.5 de 5 estrelas4.5/5 (271)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreNo EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreNota: 4 de 5 estrelas4/5 (1090)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersNo EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersNota: 4.5 de 5 estrelas4.5/5 (344)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceNo EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceNota: 4 de 5 estrelas4/5 (890)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureNo EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureNota: 4.5 de 5 estrelas4.5/5 (474)
- The Unwinding: An Inner History of the New AmericaNo EverandThe Unwinding: An Inner History of the New AmericaNota: 4 de 5 estrelas4/5 (45)
- The Yellow House: A Memoir (2019 National Book Award Winner)No EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Nota: 4 de 5 estrelas4/5 (98)
- Drug CardsDocumento187 páginasDrug Cardsintaaf82% (33)
- Tufts Pharmacology ReviewDocumento46 páginasTufts Pharmacology Reviewtesh_sachdeva100% (3)
- Farmakologi AntibiotikDocumento80 páginasFarmakologi AntibiotikTheodoric Cahyo PangestuAinda não há avaliações
- A Case Study On PnuemoniaDocumento23 páginasA Case Study On Pnuemoniaxyzert88% (8)
- Concepts of Bypass Protein Feeding in RuminantsDocumento57 páginasConcepts of Bypass Protein Feeding in Ruminantswiwiih doangAinda não há avaliações
- Drug Profile of Penicillin: 1. Product DescriptionDocumento18 páginasDrug Profile of Penicillin: 1. Product DescriptionIrfan HaiderAinda não há avaliações
- Isolation and Characterization of Bacteria Associated With Silkworm Gut Under Antibiotic-Treated Larval FeedingDocumento7 páginasIsolation and Characterization of Bacteria Associated With Silkworm Gut Under Antibiotic-Treated Larval FeedingRobert Pereira dos SantosAinda não há avaliações
- ChemotherapyDocumento253 páginasChemotherapyalmskein100% (1)
- English - II FinalDocumento31 páginasEnglish - II FinalNaeem Akhtar0% (1)
- Micro 1 - Antibiotics TableDocumento4 páginasMicro 1 - Antibiotics TableVenice RamosAinda não há avaliações
- Antibiotic Resistance - A Growing Global Health IssueDocumento6 páginasAntibiotic Resistance - A Growing Global Health IssueBramaAinda não há avaliações
- Pharmacy Training Book Topic GuideDocumento355 páginasPharmacy Training Book Topic GuideHaneen HaneenAinda não há avaliações
- Ielts Test 1 PDFDocumento23 páginasIelts Test 1 PDFBoűmřãh FōüĀdAinda não há avaliações
- Anti-Infective PPDocumento30 páginasAnti-Infective PPHlaSoe WinAinda não há avaliações
- Nursing Care Plan for Clear Airway GoalDocumento9 páginasNursing Care Plan for Clear Airway GoalSkyerexAinda não há avaliações
- Pharmaceutical Chemistry Answer Key-PINK PACOPDocumento54 páginasPharmaceutical Chemistry Answer Key-PINK PACOPArk Olfato ParojinogAinda não há avaliações
- VPT 411: Veterinary Chemotherapy (2+0) : Syllabus TheoryDocumento192 páginasVPT 411: Veterinary Chemotherapy (2+0) : Syllabus TheoryDr Ashwini ShuklaAinda não há avaliações
- 22 - Disease Biology PDFDocumento28 páginas22 - Disease Biology PDFashutosh samalAinda não há avaliações
- Adverse Reaction Case Report on Amoxicillin AllergyDocumento4 páginasAdverse Reaction Case Report on Amoxicillin Allergylia primasariAinda não há avaliações
- Dhanasekaran, Dharumadurai PanneErselvam, A. Thajuddin, Nooruddin Antimicrobials Synthetic and Natural CompoundsDocumento532 páginasDhanasekaran, Dharumadurai PanneErselvam, A. Thajuddin, Nooruddin Antimicrobials Synthetic and Natural CompoundsKima MadAinda não há avaliações
- Penicillin Allergy GuidanceDocumento9 páginasPenicillin Allergy Guidancerob burrAinda não há avaliações
- Wesleyan: College of Nursing and Allied Medical SciencesDocumento2 páginasWesleyan: College of Nursing and Allied Medical SciencesShane Aileen AngelesAinda não há avaliações
- Pharmacology Assignment 2Documento3 páginasPharmacology Assignment 2Shamantha Santhana KrishnanAinda não há avaliações
- Cephalosphorins 3rd Gen 4rt GenDocumento24 páginasCephalosphorins 3rd Gen 4rt GenshaitabliganAinda não há avaliações
- Cephalosporins: A Brief Overview of Their Chemistry, Mechanism of Action, and ClassificationDocumento34 páginasCephalosporins: A Brief Overview of Their Chemistry, Mechanism of Action, and ClassificationTasnim sarairehAinda não há avaliações
- Chemistry ProjectDocumento11 páginasChemistry ProjectRhythm's PathakAinda não há avaliações
- DifcoBBLManual 2ndedDocumento700 páginasDifcoBBLManual 2ndedEl CapitanAinda não há avaliações
- Sas Hes032 7Documento7 páginasSas Hes032 7Jose Melmar Autida AutenticoAinda não há avaliações
- Sample: The Redesigned SAT & PSAT Course BookDocumento14 páginasSample: The Redesigned SAT & PSAT Course BookBenjamin ButtonAinda não há avaliações
- MCB 419 Updated NoteDocumento37 páginasMCB 419 Updated NotetripsAinda não há avaliações