Escolar Documentos
Profissional Documentos
Cultura Documentos
Epidemics
Enviado por
Roshan OusephDescrição original:
Direitos autorais
Formatos disponíveis
Compartilhar este documento
Compartilhar ou incorporar documento
Você considera este documento útil?
Este conteúdo é inapropriado?
Denunciar este documentoDireitos autorais:
Formatos disponíveis
Epidemics
Enviado por
Roshan OusephDireitos autorais:
Formatos disponíveis
South Asia Disaster Report 2007
Chapter 11
Epidemics
An Overview
The communicable diseases have been associated with populations displaced by natural disasters. Water-related communicable diseases have been most frequent in South Asian countries. Access to safe water jeopardized by a natural disaster has been causing diarrhoeal disease outbreaks due to contamination of drinking water. An outbreak of diarrhoeal disease after flooding in Bangladesh in 2004 involved more than 17,000 cases; a large (more than 16,000 cases) cholera epidemic in West Bengal in 1998 was attributed to preceding floods, etc.1 The risk of diarrhoeal disease outbreaks following natural disasters has been quite high in South Asian countries. In Muzaffarabad, Pakistan, an outbreak of acute watery diarrhoea occurred in an unplanned, poorly equipped camp of 1,800 persons after the 2005 earthquake. The outbreak involved more than 750 cases, mostly in adults, and was controlled after adequate water and sanitation facilities were provided.2 Hepatitis A and E are also transmitted in association with lack of access to safe water and sanitation. Hepatitis A is endemic in South Asian countries, and most children are exposed and develop immunity at an early age. In Hepatitis Eendemic areas, outbreaks frequently follow heavy rains and floods; the illness is generally mild and self-limited, but for pregnant women casefatality rates can reach 25%3. After the 2005 earthquake in Pakistan, sporadic Hepatitis E cases and clusters were common in areas with poor access to safe water. Over 1,200 cases of acute jaundice, many confirmed as Hepatitis E, occurred among the displaced. Clusters of both Hepatitis A and Hepatitis E were noted after the December 2004 tsunami.4 Leptospirosis is an epidemic-prone zoonotic bacterial disease that can be transmitted by direct contact with contaminated water. Rodents shed large amounts of leptospires in their urine, and transmission occurs through contact of the skin and mucous membranes with water, damp soil or vegetation (such as sugar cane), or mud contaminated with rodent urine. Flooding facilitates spread of the organism because of the proliferation of rodents and proximity. The risk factors for outbreaks after disasters are associated primarily with population displacement. The degree of crowding, access to clean water and sanitation facilities, and the availability of healthcare services all play a role in the spread of communicable diseases and death in the affected population. The most dangerous disease after a disaster event is cholera. It is an intestinal infection generated from the bacterium Vibrio cholerae, spread by contaminated water. It is perhaps the greatest disease threat to survivors of disasters because it progresses rapidly and can kill an individual in less than a day. Vector-borne diseases generally spread after hydro-meteorological disasters. Vector-borne diseases such as malaria normally break out during the flood season. Diseases such as dengue arerelated not only to the flood season but also to meteorological conditions such
119
Epidemics
as rainfall and humidity. However, transmission of vector-borne diseases may happen together with periods of high risk of transmission, human behaviour and availability of the vectors breeding sites. Besides these, typhoid also spreads after disaster events. Typhoid fever is caused by the bacterium Salmonella Typhi generally found in contaminated water.
Incidence of South Asian Epidemics in 2007
The South Asian floods of 2007 triggered many epidemics. Communicable diseases were reported from most of the flood- and cyclone-affected areas. It was more pronounced in 40 districts of Bangladesh, and Bihar and Orissa in India. The outbreak of water-borne diseases after floods was recorded in Bangladesh during the last week of June 2007. Two cases of infectious diseases (Cholera and ARI) were found in Bangladesh.5 As per EMDAT data, from 29 July to 9 October 2007, it was reported that the diarrhoea killed 54 people and affected 236,558 of the population. Within the same period, the viral infection ARI also killed 32 people and affected 48,352 of the population. The statistics of casualties from disaster is depicted in Table 11.1. Further, 302 cases of snake bite, with 116 epidemic-related deaths were also recorded.6
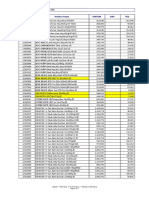
Table 11.1: Casualties from Epidemic 20075 Disease Cholera ARI Country Bangladesh Bangladesh Start 29 Jul 30 Jul End 9 Oct 9 Oct Killed 54 32 Affected 2,36,558 48,352
Bacterial Infectious Diseases Viral Infectious Diseases
Forty districts in Bangladesh were affected with diarrhoea. The most affected district was Jamalpur, where more than 19,000 cases were registered. Dhaka also recorded more than 10,000 cases. The worst affected districts due to epidemics are listed in Figure 11.1.
Figure 11.1: Diarrhoea-affected five districts (Bangladesh), X-axis: Cases, Y-axis: Districts6
120
South Asia Disaster Report 2007
Among the Indian States, Orissa was the worst affected. The different waves of floods during the continuous rain in July-August 2007 led the outbreak of cholera in Orissa (districts of Koraput, Rayagada, Dasmantpur and Kalahandi). More than 100 people were killed by this disease. 7 The hardest hit victims were the people from indigenous or tribal communities. The UNDP situation report during August 2007 reported 184 people killed by flood epidemic. The death casualty in Orissa is depicted in Table 11.2. The death figures as on 31st August 2007 are presented in Figure 11.2
Table 11.2: Death from flood epidemic, 2007, Orissa Affected Districts Rayagada Kahalanadi Koraput Dasmantpur Laximipur Nandapur Kundra Mathalput Deaths 64 17 52 35 9 2 2 3 Figure 11.2: People killed by flood epidemic disease (OrissaIndia), X-axis: Cases, Y-axis: Districts8
The outbreak, which started in mid-July, continued for almost two months and reached its peak during the last week of August 2007. The epidemic curve is shown in Figure 11.3. The outbreak was considered to be the result of poor sanitation and water contamination in the flood-affected areas.
Figure11.3: Epidemic curve of the acute severe diarrhoeal diseases outbreak in Orissa:
July-September 20079
121
Epidemics
Response
The Directorate General of Health Services (DGHS) of Bangladesh organized 3,528 medical teams to work in the forty flood-affected districts and provided emergency medical services to the flood victims to recover from the health problems. The team provided emergency drugs for combating health impacts of floods at all levels and provided service in treatment of all types of flood-related patients at all levels. The WHO-EHA Program provided emergency health kits such as cholera kits, malaria kits, etc. to the health sector for post-flood health management. UNICEF Bangladesh provided 10 mobile water treatment plants for different areas. Government of India and the concerned State Governments responded to the health emergency needs in floodaffected areas. To control the disease in Orissa, a coordination meeting of members representing the UN agencies was held on 27th August 2007 and a technical team was created to support the three most affected districts.
State-Level Measures to contain the spread of Cholera in Orissa
A team was deputed by Government of India to take stock of the health situation in the three affected districts. The National Institute of Communicable Diseases (NICD) apprised the Government of Orissa (GoO) about the health situation and also shared their recommendations to restrict further spread of cholera. The NICD appreciated Govt. of Orissa (GoOs), measures, which included setting up diarrhoea treatment centres; mobilization of doctors and nurses; deployment of Mobile Health teams; organisation of mobility support for getting patients from affected villages to CHC/PHC; adequate drug flow to affected areas; mobilization of sick patients to treatment centres by PRI and ICDS and multi-sectoral involvement for managing the crisis (ICDS, RWSS, PRI, Administration). Recommendations by NICD include: The medicine for treatment is Doxycycline and Tetracycline. They did not recommend Chloramphenicol immediately. They also discouraged the use of other antibiotics, like ciprofloxacin, gentamycin and amikacin at PHC level. They recommended initial quick rehydration and quick switchover to ORS once the patient was ready to eat and dehydration was corrected to restrict over-use of IV fluids; chemoprophylaxis with Tetracycline across the village is discouraged but chemprophylaxis with Tetracycline was recommended for contact cases to be continue. They did not recommendcholera vaccination or mass use of chemoprophylaxis, and restricted trace activities and travel. Further, the NICD requested Government of Orissa to ensure appropriate treatment of soaked lines and disinfection of clothes before washing them in river water or tap water, putting up of pre-fabricated toilets, and management of overcrowding in wards of hospitals to improve the sanitary conditions at PHC/CHC; the District administration are installing Sintex tanks at diarrhoea treatment centres for safe water supply. The plan should also ensure that affected villages are also covered.
Source: UNDP, India, Situation Report, 31 August 2007
122
South Asia Disaster Report 2007
UNICEF continues its support in flood-stricken Bangladesh
15 August 2007 One month after floods devastated Bangladesh, the United Nations Childrens Fund (UNICEF) continues to provide food, safe drinking water, sanitation facilities and shelter to those affected by the monsoon rains. UNICEF has also deployed 10 mobile water treatment plants for communities needing safe water in concert with the countrys Department of Public Health and Engineering. The agency said in its latest update, released yesterday, that deaths resulting from diarrhoea have been avoided to date despite 15,000 reported cases thanks to the availability of oral rehydration salts to treat dehydration. It is critical to recognize that in this situation the children and women, especially children of female-headed households, are the most affected, said UNICEFs Representative in Bangladesh Louis-Georges Arsenault.Our assessments of the situation confirm that there are some very specific needs such as for special nutrients for children, pregnant and lactating women, which must continue to be addressed. So far, UNICEF and the UN World Food Programme (WFP) have distributed 90 tons of high-protein biscuits in Bangladesh and plan to deliver another 24 tons this week, UN spokesperson Michele Montas told reporters in New York yesterday. An estimated 45 million people across India, Nepal, Bangladesh and Pakistan have been affected by the flooding, with many of them forced to leave their homes. At least 2,200 people have been killed. The UNs Office for the Coordination of Humanitarian Affairs (OCHA) announced that it is increasing its support of South Asian governments as they respond to the flooding, including by drawing from the Central Emergency Response Fund (CERF).
Source: UN news Centre, 2007
Bangladesh
Figure 11.4: Villagers rescuing mother and children at Shirajgunj
Figure 11.5: Distributing clean water to community, 2007, Photo source: UNICEF
123
Epidemics
Orissa - India
Figure 11.6: A bridge damaged in floods near Gudhikhal village of Balasore District in Orissa Photo source: Times of India
Figure 11.7: Drinking water supply in Orissa, 2007 Photo source: Ramakrishna Mission, Belgharia
Figure 11.8: Clean and safe water distribution in Orissa Photo source: Times of India
Figure 11.9: Food relief in Orissa, 2007, Photo source: Ramakrishna Mission, Belgharia
REFERENCES
Please give full names of journals 1. Sur D. Severe cholera outbreak following floods in a northern district of West Bengal. Indian Journal of Medicine Res. 2000; 112:17882. 2. World Health Organization. Acute water diarrhoea outbreak. Weekly Morbidity and Mortality Report. 2005;1:6. [cited 2006 Aug10]. Available from h t t p : / / w w w. w h o. i n t / h a c / c r i s e s / i n t e r n a t i o n a l / p a k i s t a n _ e a r t h q u a k e / s i t r e p / FINAL_WMMR_Pakistan_1_December_06122005.pdf
124
South Asia Disaster Report 2007
3.
Aggarwal R., Krawczynski K. Hepatitis E: an overview and recent advances in clinical and laboratory research. J Gastroenterol Hepatol.2000;15:920. World Health Organization. Epidemic-prone disease surveillance and response after the tsunami in Aceh Province, Indonesia. Wkly Epidemiol Rec. 2005;80:1604. CRED Data, www.emdat.be WHO Situational Report, 2007, Bangladesh. UNICEF update, 25 September 2007. Situational report, UNDP India, 2007. www.searo.who.int/LinkFiles/CDS_CDS-Newsletter-Vol4issue4.pdf
4.
5. 6. 7. 8. 9.
10. UNDP, India, Situation Report, 31 August 2007. 11. UN news Centre, 2007. 12 . UNDP Situation report, August 2007.
*****
125
Você também pode gostar
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)No EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Nota: 4.5 de 5 estrelas4.5/5 (121)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryNo EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryNota: 3.5 de 5 estrelas3.5/5 (231)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaNo EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaNota: 4.5 de 5 estrelas4.5/5 (266)
- Never Split the Difference: Negotiating As If Your Life Depended On ItNo EverandNever Split the Difference: Negotiating As If Your Life Depended On ItNota: 4.5 de 5 estrelas4.5/5 (838)
- The Emperor of All Maladies: A Biography of CancerNo EverandThe Emperor of All Maladies: A Biography of CancerNota: 4.5 de 5 estrelas4.5/5 (271)
- The Little Book of Hygge: Danish Secrets to Happy LivingNo EverandThe Little Book of Hygge: Danish Secrets to Happy LivingNota: 3.5 de 5 estrelas3.5/5 (400)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeNo EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeNota: 4 de 5 estrelas4/5 (5794)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyNo EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyNota: 3.5 de 5 estrelas3.5/5 (2259)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreNo EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreNota: 4 de 5 estrelas4/5 (1090)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersNo EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersNota: 4.5 de 5 estrelas4.5/5 (345)
- Team of Rivals: The Political Genius of Abraham LincolnNo EverandTeam of Rivals: The Political Genius of Abraham LincolnNota: 4.5 de 5 estrelas4.5/5 (234)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceNo EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceNota: 4 de 5 estrelas4/5 (895)
- The Unwinding: An Inner History of the New AmericaNo EverandThe Unwinding: An Inner History of the New AmericaNota: 4 de 5 estrelas4/5 (45)
- Skeletal SystemDocumento29 páginasSkeletal SystemCrii XiaAinda não há avaliações
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureNo EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureNota: 4.5 de 5 estrelas4.5/5 (474)
- 54 Sex AffirmationsDocumento2 páginas54 Sex AffirmationsR.u. KhanAinda não há avaliações
- The Yellow House: A Memoir (2019 National Book Award Winner)No EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Nota: 4 de 5 estrelas4/5 (98)
- Capillarys Immunotyping NorestrictionDocumento24 páginasCapillarys Immunotyping Norestrictionabbhyasa5206100% (2)
- How The Immune System WorksDocumento13 páginasHow The Immune System Worksnishant nagyan100% (2)
- Case Study On SchizophreniaDocumento21 páginasCase Study On SchizophreniaAdrian Mallar100% (1)
- Exploratory Latin AnimalsDocumento15 páginasExploratory Latin AnimalsKari Kristine Hoskins BarreraAinda não há avaliações
- Science of Being - 27 Lessons (19-27) - Eugene FersenDocumento257 páginasScience of Being - 27 Lessons (19-27) - Eugene FersenOneness100% (2)
- Single Complete Denture FinalDocumento15 páginasSingle Complete Denture FinalVikas AggarwalAinda não há avaliações
- Violet Winspear The Awakening of AliceDocumento197 páginasViolet Winspear The Awakening of AliceSaumya Bhasin80% (5)
- Aries Kitten: Head & BodyDocumento4 páginasAries Kitten: Head & BodySelena KAinda não há avaliações
- No Quarter 05Documento100 páginasNo Quarter 05guilherme100% (1)
- Tortle VariantsDocumento4 páginasTortle VariantsCarter RobinsonAinda não há avaliações
- Presentation 1Documento10 páginasPresentation 1Roshan OusephAinda não há avaliações
- Control of Sedimentation in ReservoirsDocumento43 páginasControl of Sedimentation in ReservoirsDev AnandAinda não há avaliações
- 48 Killed As Indonesian Volcano Erupts AgainDocumento3 páginas48 Killed As Indonesian Volcano Erupts AgainRoshan OusephAinda não há avaliações
- Infectious Disease: EMS Professions Temple CollegeDocumento133 páginasInfectious Disease: EMS Professions Temple CollegeRoshan OusephAinda não há avaliações
- Biological HazardDocumento15 páginasBiological HazardRoshan Ouseph100% (1)
- Sample Paper 1 ENGLISHDocumento22 páginasSample Paper 1 ENGLISHDhawan ChoudharyAinda não há avaliações
- Binding Capacity of Bull Spermatozoa ToDocumento180 páginasBinding Capacity of Bull Spermatozoa ToczumoffenAinda não há avaliações
- Abraham Blessing Cluster 988Documento102 páginasAbraham Blessing Cluster 988Becky ChiloveAinda não há avaliações
- Navarro College Dining MenuDocumento2 páginasNavarro College Dining MenuNavarro CollegeAinda não há avaliações
- Treatment and Management of Lumpy Skin Disease in Cow: A Case ReportDocumento2 páginasTreatment and Management of Lumpy Skin Disease in Cow: A Case ReportjabidurAinda não há avaliações
- RFTPS2CULTDocumento7 páginasRFTPS2CULTAna Vaquer MontoroAinda não há avaliações
- Harga Baru Nestle OkeDocumento8 páginasHarga Baru Nestle OkeFitri 'cwett' WijayantiAinda não há avaliações
- The White Ship - Chingiz AitmatovDocumento92 páginasThe White Ship - Chingiz AitmatovYêu Văn Học100% (5)
- Connective TissueDocumento21 páginasConnective TissueCalvin Lin Jia RongAinda não há avaliações
- Estrogenic Activity of Alcoholic Extract of Lemon Seeds (Citrus Limonum) On Immature Albino RatsDocumento5 páginasEstrogenic Activity of Alcoholic Extract of Lemon Seeds (Citrus Limonum) On Immature Albino RatsKocyd Dyck OkooAinda não há avaliações
- Euthanasia: Methods of Euthanasia Case Study - Euthanasia ReferencesDocumento11 páginasEuthanasia: Methods of Euthanasia Case Study - Euthanasia ReferencesManoj KarkiAinda não há avaliações
- Sample Test Paper: Le Feuv Egùke VadDocumento17 páginasSample Test Paper: Le Feuv Egùke VadFarhanAinda não há avaliações
- Macros HunterDocumento5 páginasMacros HunterikenconstructAinda não há avaliações
- English 2 Periodical Test Quarter 4Documento5 páginasEnglish 2 Periodical Test Quarter 4April CelebradosAinda não há avaliações
- Multiple Choices and Key AnswersDocumento8 páginasMultiple Choices and Key AnswersSrimurtiniDw'yuAinda não há avaliações
- 1 Eye of Horus and Count Like An Egyptian 2Documento6 páginas1 Eye of Horus and Count Like An Egyptian 2yin yinAinda não há avaliações
- Formato Examen BimestralDocumento4 páginasFormato Examen BimestraldestendAinda não há avaliações
- Materi Reading 2Documento10 páginasMateri Reading 2Putri DinantiAinda não há avaliações