Escolar Documentos
Profissional Documentos
Cultura Documentos
4 C0 FCCF9 D 01
Enviado por
Santhosh KumarDescrição original:
Título original
Direitos autorais
Formatos disponíveis
Compartilhar este documento
Compartilhar ou incorporar documento
Você considera este documento útil?
Este conteúdo é inapropriado?
Denunciar este documentoDireitos autorais:
Formatos disponíveis
4 C0 FCCF9 D 01
Enviado por
Santhosh KumarDireitos autorais:
Formatos disponíveis
CONTINUING EDUCATION CREDIT
Pharmacological Management of Sickle Cell Disease
Uche Anadu Ndefo, PharmD, BCPS; Angie Eaton Maxwell, PharmD; Huong Nguyen, PharmD Candidate; and Tochukwu L. Chiobi, PharmD
Educational Objectives
After reviewing this article, readers should be able to: I Define the basic hematological defect in sickle cell disease. I Identify the mechanisms of action and adverse events associated with standard treatment options. I Review the protocol for preventing stroke and infection in patients with sickle cell disease. I Identify treatment options currently under investigation.
Pathogenesis
Sickle cell disease is characterized by a structural abnormality in the beta-globin chain of the hemoglobin molecule within the red blood cells (RBCs). The sickle mutation is a single base change (GAT GTT) in the sixth codon of exon-1 of the betaglobin gene on chromosome 11. This change leads to the synthesis of the beta-globin polypeptide of the hemoglobin molecule. This mutation causes the replacement of the normal glutamic acid with valine acid, thus resulting in the formation of the sickle cell hemoglobin (HbS). This hydrophobic aminoacid substitution causes the hemoglobin to take on a sickle shape when in a deoxygenated state. The ability of these sickled cells to adapt to their surroundings is impaired, especially in the microvasculature. These cells hemolyze prematurely, accounting for the chronic anemia frequently encountered by patients with SCD.5 The paucity of sickled cells in newborns with SCD led to the discovery that fetal hemoglobin (HgF) reduces the severity of SCD by preventing the formation of the hemoglobin S polymer.6 Fever, dehydration, hypoxia, acidosis, stress, and a cold environment may precipitate sickling, although a precursor event is not always identified.7,8 The pathophysiology of SCD is considerably complex, involving abnormalities of hemoglobin, the RBCs membrane, er ythrocyte hydration, the endothelium, vascular tone, inflammatory responses, leukocytes, and coagulation. This forceful combination of factors results in cell interactions, generating hemolysis and microvascular obstruction, ultimately leading to damage of nearly all organ systems.9
Introduction
Sickle cell disease (SCD) is the most common inherited blood disorder in the U.S., affecting about 72,000 Americans. It is also the most common inherited disease among AfricanAmericans and affects approximately one out of every 500 newborns. People of other races are also affected by SCD, with a rate of one of every 1,000 to 1,400 HispanicAmerican births.1 A significant prevalence of the mutation responsible for sickle cell has been reported among other ethnic groups such as those native to Italy, Greece, Turkey, Saudi Arabia, India, Pakistan, Bangladesh, China, and Cyprus.2 In 2004, 83,149 hospitalizations were attributable to SCD in the U.S., at a cost of almost $488 million.3 Episodes of pain, chronic hemolytic anemia, and severe infections are some of the common characteristics of this disease that begin in early childhood.4 Management of SCD is geared toward preventing complications and reducing the number of sickle cell crises.
Risk Factors
Dr. Ndefo and Dr. Maxwell are Assistant Professors of Pharmacy Practice in the College of Pharmacy and Health Sciences at Texas Southern University in Houston, Texas. They are also Drug Information Specialists at Harris County Hospital District in Houston. Huong Nguyen is a pharmacy student at Texas Southern University. Dr. Chiobi is a recent graduate of Texas Southern University.
Two million people worldwide are carriers of or have the sickle cell trait. Carriers are usually asymptomatic and have a low percentage of sickle hemoglobin (HbS). Two parents who are carriers can both pass on the sickle cell trait to their offspring, resulting in SCD. There is a 50% chance with each pregnancy for the child of two sickle cell carriers to be born with the sickle cell trait, and there is a 25% chance for the child to be born with SCD (Figure 1).
Accepted for Continuing Education Credit March 4, 2008.
238 P&T
April 2008 Vol. 33 No. 4
CONTINUING EDUCATION CREDIT
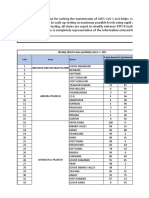
Table 1 Prophylaxis of Complications from Sickle Cell Disease
Complication Streptococcus pneumoniae sepsis Prophylactic Therapy Newborns to 3 years: Penicillin VK, 125 mg orally twice daily 3 to 5 years: Penicillin VK, 250 mg orally twice daily 2 years: 23-valent Streptococcus pneumoniae polysaccharide vaccine (PPV23)
Bone marrow aplasia and megaloblastic erythropoiesis 1 mg folic acid daily Stroke Pain episodes Exchange transfusions Hydroxyurea Initiation of treatment: 1015 mg/kg/day single daily dose for six to eight weeks Monitor: complete blood count every two weeks percent fetal hemoglobin every six to eight weeks serum chemistries every two to four weeks
Diagnosis
Screenings for SCD at birth are now performed in most states in the U.S. The presence of hemoglobin S (HbS) with elevated fetal hemoglobin (HbF) and the absence of hemoglobin A indicate either sickle cell anemia or beta thalassemia. It is imperative that sickle cell anemia be detected early, because preventive care must begin by the time a child is two months of age to improve survival. The diagnosis of SCD is usually confirmed by electrophoresis. The sickle cell trait is also identified in screenings of newborns, who have a much lower percentage of hemoglobin S than other patients with SCD.
Treatment Options
The only cure for SCD is bone marrow transplantation, which usually necessitates a human lymphocyte antigen (HLA)- identical family member donor. There is an 85% diseasefree survival rate, with a 7% transplant-related mortality rate and a 9% graft failure rate.10 Barriers to the widespread use of bone marrow transplantation in patients with SCD include a lack of suitable bone marrow donors and the need to identify patients with an adequate risk-to-benefit ratio. For these reasons, drug therapy for SCD continues to be the primary mode of disease management, focusing on decreasing the complications of this disease (Table 1).
Hydroxyurea
Hydroxyurea, the only agent that the Food and Drug Administration (FDA) has approved for the management of SCD, is indicated for sickle cell patients who have had at least three painful crises in the previous 12 months. Hydroxyurea prevents the complications of SCD by increasing HbF and total hemoglobin concentrations, by decreasing the adhesion of sickled cells to the endothelium in vitro, and by increasing polymerization time.11 The Multicenter Study of Hydroxyurea in Sickle Cell Anemia (MSH) was a randomized, double-blind, placebocontrolled clinical trial in which adult patients were assigned to receive hydroxyurea and placebo. Treatment with hydroxyurea resulted in a 44% difference in the median annual rate of painful crises: 2.5 crises per year in the hydroxyurea arm vs. 4.5 crises per year in the placebo arm. Because hydroxyurea reduced the frequency of episodes of pain, acute chest syndrome, and the need for blood transfusion, the study was stopped four months early.12 A nine-year follow-up of the participants in this trial showed a 40% reduction in mortality rates for patients taking hydroxyurea.13 In small clinical trials of hydroxyurea in children with SCD, the agent was found to be safe and efficacious, and these effects were sustained in long-term trials.1416
AS
AS
AA
AS
AS
SS
Figure 1 Risk factors. Two parents with the sickle cell trait (AS) have a 25% chance of having a child without the sickle cell trait (AA), a 50% chance of having a child with the sickle cell trait (AS), and a 25% chance of having sickle cell disease (SS). In this inherited condition, both hemoglobin A and S are produced in the red blood cells (more A than S).
Vol. 33 No. 4 April 2008
P&T 239
CONTINUING EDUCATION CREDIT
Table 2 Treatment Options for Complications from Acute Sickle Cell Disease
Complication Pain Mild to moderate Therapy Codeine with acetaminophen or aspirin orally every three to four hours Hydrocodone with acetaminophen orally every three to four hours Morphine sulfate immediate-release (MSIR) IV every two to four hours orally every three to four hours Hydromorphone IV or orally every three to four hours Empirical therapy coverage for: Streptococcus pneumoniae, Salmonella, Haemophilus influenzae, gram-negative enterics Streptococcus pneumoniae, Neisseria meningitides, H. influenzae S. pneumoniae, Legionella, Mycoplasma pneumoniae, respiratory syncytial virus, Chlamydia pneumoniae Salmonella, Staphylococcus aureus, S. pneumoniae Escherichia coli, other gram-negative enterics
Moderate to severe
Infection
Fever without a source (rule out sepsis) Meningitis Chest syndrome Osteomyelitis/septic arthritis Urinary tract infection
IV = intravenously. From National Institutes of Health. The Management of Sickle Cell Disease, 4th ed. revised, June 2002.22
Hydroxyureas potential benefits should be weighed against the risks of bone marrow suppression, which is reversible when the drug is discontinued. Complete blood counts are recommended every four to eight weeks after the hydroxyurea dose is stabilized.
Pain Medications
Pain, which is usually attributed to ischemia from the obstruction of blood vessels by sickled cells, is the most common symptom of SCD. It can be acute or chronic, and it varies among individuals in its frequency and intensity. Pain is the primary cause of hospitalization in patients with SCD, which is why proper management of pain in this population is essential.17 The general approach to the treatment of pain is to identify the causes, which include infection, extreme temperature, and emotional stress. Usually, however, there is not an identifiable cause, and the pain crisis occurs without warning. Milder pain is treated with general nonsteroidal anti-inflammatory drugs (NSAIDs) such as ibuprofen and ketorolac tromethamine (Toradol, Roche) or analgesics like acetaminophen and tramadol (Ultram, PriCara). Severe painful episodes should be treated with parenteral opiates at frequent intervals, not on an as-needed basis. In a study comparing intermittent intravenous (IV) injections and patient-controlled analgesia (PCA), PCA reduced the length of stay and was as efficacious as the injections.18 Acute episodes of pain may also be treated with IV hydration, and milder episodes may be treated with oral hydration regardless of the patients state of hydrationto slow or stop the sickling process, which can be promoted by dehydration.19
After the pain has diminished and has tapered off, an oral analgesic can be given. The opiate drugs that have been studied to treat SCD include morphine, hydromorphone, fentanyl (Duragesic, PriCara), and codeine-related agents.20 Morphine is considered the drug of choice for the treatment of acute sickle cell pain (Table 2), whereas meperidine (Demerol, Sanofi-Synthelabo) should be avoided because of the increased risk of seizures in patients with renal dysfunction, which can occur in patients with SCD.
Infection Prophylaxis
Patients with SCD are at an increased susceptibility to pneumococcal infection primarily because of the development of functional asplenia, which can occur at as early as six months of age.21 In the absence of a functional spleen, the organ can no longer serve its immunological functions of clearing bacteria from the blood and synthesizing antibodies, circumstances that can lead to an increased frequency of infection.22 In the PRophylaxis with Oral Penicillin in children with Sickle Cell Anemia (PROPS) study, when infants received prophylactic penicillin between three months and three years of age, pneumococcal infection rates decreased by 84%.23 PROPS II evaluated the consequences of discontinuing penicillin prophylaxis at five years of age, and there was no difference in the rates of infection in the penicillin arm, compared with the placebo arm (relative risk = 0.5).21 On the basis of the PROPS and PROPS II results, children younger than three years of age should receive 125 mg of penicillin orally twice daily, and children between three and five years of age should receive 250 mg of penicillin orally twice a day. For patients who are allergic to penicillin, erythromycin
240 P&T
April 2008 Vol. 33 No. 4
CONTINUING EDUCATION CREDIT
ethyl succinate (e.g., EryPed, Abbott) 20 mg/kg, divided into two daily doses, can provide adequate prophylaxis.24 Problems with penicillin prophylaxis include compliance, drug cost, patient tolerance, and resistant strains of micro organisms.25 Immunizations in children with SCD should include all regular vaccines, with the addition of the flu vaccine yearly after six months of age; pneumococcal vaccine at two and five years of age; and, possibly, meningococcal vaccine.26 it is proposed that folate in anemia raises hemoglobin levels and helps provide a healthy reticulocyte response,32 the use of folic acid in patients with SCD is not well supported by the primary literature. One prospective, randomized study, published in 1983, found no striking effects of folic acid supplementation in sickle cell anemia on the hematological profile or on growth in children with SCD who received this nutrient.33 In another study that measured folate stores in children with SCD who were not receiving folic acid, folate levels were found to be adequate.34 The National Heart, Lung, and Blood Institute guideline for SCD does recommend folic acid supplementation for patients with sickle cell anemia at the dose of 1 mg/day.21
Stroke Prevention
The prevalence of stroke in patients with SCD was reported to be 11% before routine screening with transcranial Doppler ultrasonography (TCD) and monthly transfusions for primary stroke prevention in children at risk. Not all children with SCD are at equal risk for stroke; Doppler ultrasound should be performed to assess the patients blood flow velocity, because high blood flow velocity has been correlated with a subsequent stroke in children with SCD.27 In a randomized study of children with SCD, patients who had abnormal results (time-averaged mean blood flow exceeding 200 cm/second) received standard-of-care or transfusions with a target hemoglobin S concentration of less than 30%. The study was terminated early, because there was a 92% difference in cerebrovascular accidents (CVAs) between the standard-ofcare group and the transfusion group.27 It is still not known when, if ever, it is optimal to discontinue prophylactic transfusions in patients with abnormal TCD results. The Optimal Primary Stroke Prevention in Sickle Cell Anemia (STOP 2) Trial Investigators randomly assigned children who were receiving prophylactic transfusions to either stop receiving them after 30 months or to continue with them. The endpoints evaluated were abnormal TCD findings or stroke; neither event occurred in the arm that continued transfusion therapy. The arm that discontinued therapy had 14 abnormal TCD results and two strokes within 4.5 2.6 months of stopping transfusions.28 Children with abnormal TCD outcomes had a hydroxyurea-related decrease in TCD flow velocity from 216 14 to 173 31 cm/second, suggesting the possible benefit of switching to hydroxyurea for stroke prevention.29 With regular transfusions comes the burden of iron overload; until recently in the U.S., this condition was treated only with deferoxamine (Desferal, Novartis), which was administered by subcutaneous or IV infusion. A new once-daily oral chelator, deferasirox (Exjade, Novartis), when compared with deferoxamine in patients with SCD and iron overload, was found to be safe and effective in these patients.30 At the time of this writing, a study evaluating the role of aspirin in the stroke prophylaxis in children was recruiting participants.31
Pulmonary Hypertension
Some studies have suggested that pulmonary hypertension (PHTN) is common in patients with sickle cell anemia. A prospective study of sickle cell anemia reported a 31% prevalence of PHTN in children 10 years of age and older.35 There is emerging evidence on the treatment of traditional PHTN with prostanoids such as epoprostenol (Flolan, GlaxoSmithKline) and phosphodiesterase-5 inhibitors such as sildenafil citrate (Revatio, Pfizer). The FDA approved sildenafil for the treatment of PHTN in 2005. A study conducted at the Howard University Center for Sickle Cell Disease tested PHTN reversibility by giving prostacyclin infusions to eight patients with PHTN during cardiac catheterization.36 Pulmonar y pressures were significantly reduced in six of the eight patients who received the infusions. An open-label, uncontrolled pilot trial of 12 patients with SCD and PHTN found that sildenafil improved exercise capacity and PHTN.37
Priapism
Priapism, possibly resulting from decreased blood flow to the corpus cavernosum, is a known problem in men with SCD.38 Usually precipitated by sexual activity, priapism has a prevalence of between 6% and 38% in SCD patients.39 There are two kinds of priapism: (1) stuttering, defined as repeated short episodes, with each episode lasting for between 30 minutes and three hours, and (2) prolonged, defined as episodes lasting for more than three hours. Acute episodes of priapism lasting for more than two hours should be treated in the emergency department. Penile aspiration, followed by irrigation of the corpus cavernosum with a sympathomimetic agent, should be initiated if detumescence does not occur an hour after the patients arrival. Oral terbutaline (Brethine, aaiPharma) and pseudoephedrine (e.g., Sudafed, Pfizer) have demonstrated efficacy in the treatment of priapism.40
Folic Acid and Anemia
In patients with SCD, the RBC count is lower than normal because sickled cells usually die after 10 to 20 days, in contrast to 120 days for normal RBCs. Because of high cell turnover, folate stores are often depleted. Folic acid replenishes the depleted folate stores necessary for erythropoiesis. Folic acid supplementation is well established in the treatment of chronic hemolytic anemia. Although
Investigational Treatment Options
Niprisan
As a phytopharmaceutical derived from a plant in its original state, Niprisan was developed by the Nigerian National Institute for Pharmaceutical Research and Development. This anti-sickling agent was granted orphan drug status by the FDA in 2003 under the name Hemoxin, made by Xechem International. Its anti-sickling properties are attributed to its
Vol. 33 No. 4 April 2008
P&T 241
CONTINUING EDUCATION CREDIT
ability to prolong or delay the time to polymerization of deoxyHb S.41 A phase 2, double-blind, placebo-controlled, six-month randomized crossover trial revealed that the frequency of sickle cell pain crisis in the Niprisan arm was significantly reduced.42 A phase 3 clinical trial is under way, and an investigational New Drug Application (NDA) is being prepared by Xechem for submission to the FDA.
Nitric Oxide
in daily narcotic usage. Overall, the oral administration of
L-glutamine has shown a consistent and significant increase in
red blood cell NADH and was well tolerated by the patients with no adverse effects.50
Magnesium
Nitric oxide (NO), a potent vasodilator thought to be deficient in patients with SCD, has been suggested as a therapeutic option.43 Its proposed mechanism of action is its ability to limit the sickling of RBCs by preventing them from sticking to vessel walls or by dilating peripheral blood vessels.44 Studies by Head et al. suggested that NO increases the hemoglobin oxygen affinity in homozygous HbS (SS) erythrocytes either when RBCs are exposed to NO in vitro or during NO inhalation in low concentrations in vivo.45 It is not clear how low concentrations of NO enhance oxygen affinity of erythrocytes in SCD, compared with normal erythrocytes, but research suggests that NO modifies HbS, thereby reducing polymerization and increasing oxygen affinity in sickled RBCs.
L-Arginine
De Franceschi et al. suggested that a possible therapeutic strategy for SCD was based on reducing the cellular concentration of sickle cell hemoglobin (HbS) by preventing erythrocyte dehydration.51 The major determinant of sickle cell dehydration is the potassium chloride transporter, which is inhibited by increasing the erythrocyte magnesium content. Oral administration of magnesium showed considerable increases in sickle erythrocyte magnesium and potassium content and reductions in the number of dense sickle erythrocytes. In addition, the erythrocyte potassium chloride co-transport was reduced significantly, and the absolute reticulocyte count and the number of immature reticulocytes were greatly reduced. The authors concluded that oral magnesium reduced the number of dense erythrocytes and improved the erythrocyte membrane transport abnormalities of patients with SCD, thus reducing erythrocyte dehydration. Transient diarrhea was the only significant side effect and was noted in one of 10 patients in the study.
The amino acid L-arginine is a required substrate for nitric acid synthesis by endothelial cells, platelets, and other cells. In addition to having a deficiency of NO, adults with SCD sometimes have significantly diminished arginine levels. This arginine deficiency may be the cause of PHTN in sickle cell patients; therefore, the infusion of L-arginine has been shown to reduce vascular resistance and improve blood oxygenation in infants with PHTN.46 In one study, L-arginine supplementation improved pulmonary artery pressures and hemodynamics in primary and secondary hypertension within one week of therapy. Overall, arginine was well tolerated with minimal adverse effects.47
L-Glutamine
L-Glutamine is a precursor for nicotinamide adenine dinucleotide (NAD), which is deficient in patients with sickle cell anemia. A deficiency of glutamine may result in the possibility of skeletal muscle wasting, immunosuppression, and impaired wound healing.48 It is suggested that the deficiency in glutamine is a result of the rate of active transport of glutamate (a by-product of glutamine) in sickled RBCs. Oral L-glutamine therapy can be beneficial in patients with sickle cell anemia by increasing the activity of NAD synthesis, thus countering the oxidant-dependent pathophysiology of sickled RBCs.49 In a four-week study of seven patients with sickle cell anemia who were 19 to 60 years of age, Niihara and colleagues found that given 30 g of oral L-glutamine for four weeks brought about a significant increase in NADH (the reduced form of NAD) and NAD redox potential (the ratio of NADH to NAD+ plus NADH). These participants also experienced an overall improvement in energy, accompanied by an increased activity level and various degrees of decreases in chronic pain. Of the seven patients who participated in the study, six reported a decrease
Conclusion
Although bone marrow transplantation can cure SCD, it is an impractical solution for most Third World countries, which have a high disease burden. Even in the U.S., bone marrow transplantation is limited by the availability of donors. Pharmacological therapies are effective at reducing complications of SCD and are safe and easily administered, and they continue to prolong the life expectancy of patients.
References
1. American Stroke Association. Sickle cell disease. Available at www.strokeassociation.org/presenter.jhtml?identifier=3034962. Accessed August 10, 2007. 2. Nietert PJ, Silverstein MD, Abboud MR. Sickle cell anemia: Epidemiology and cost of illness. Pharmacoeconomics 2002;20:357 366. 3. Steiner C, Miller J. Sickle cell disease patients in U.S. hospitals, 2004. Healthcare Cost and Utilization Project (HCUP) Statistical Brief No. 21, December 2006. Rockville, Md: Agency for Healthcare Research and Quality. Available at: www.hcup-us.ahrq.gov/ reports/statbriefs/sb21.pdf. Accessed 2/24/2008. 4. Anemia, sickle cell. National Library of Medicine. Available at: www.ncbi.nlm.nih.gov/books/bv.fcgi?call=bv.View.ShowSection &rid=gnd.section.98. Accessed October 8, 2007. 5. Sickle cell anemia. ACP PIER & AHFS DI Essentials, 2007. American College of Physicians (Philadelphia, Pa.), Physicians Information and Education Resource and American Hospital Formulary Service, Drug Information. Available at: http:/online.statref. com/titles/title infopage.aspx?titleid=92. Accessed December 14, 2007. 6. A brief history of sickle cell disease. Harvard University Information Center for Sickle Cell and Thalassemic Disorders. Available at: http://sickle.bwh.harvard.edu/scd_history.html. Accessed December 17, 2007. 7. Fosdal MB, Alexandrov AW. Events of hospitalization among children with sickle cell disease. J Pediatr Nurs 2007; 22:342346. 8. Driscoll CM. Sickle cell disease. Pediatr Rev 2007;28:259267.
242 P&T
April 2008 Vol. 33 No. 4
CONTINUING EDUCATION CREDIT
9. Raphael RI, Vichinsky EP. Pathophysiology and treatment of sickle cell disease. Clin Adv Hematol Oncol 2005;3:492505. 10. Iannone R, Ohene-Frempong K, Fuchs EJ, et al. Bone marrow transplantation for sickle cell anemia: Progress and prospects. Pediatr Blood Cancer 2005;44:436440. 11. Bunn HF. Pathogenesis and treatment of sickle cell disease. N Engl J Med 1997;337:762769. 12. Charache S, Terrin ML, Moore RD, et al. Effect of hydroxyurea on the frequency of painful crises in sickle cell anemia. N Engl J Med 1995;332:13171322. 13. Steinberg MH, Barton F, Castro O, et al. Effect of hydroxyurea on morbidity and mortality in adult sickle cell anemia: Risks and benefits up to 9 years of treatment. JAMA 2003;289:16451651. 14. Ferster A, Vermylen C, Cornu G, et al. Hydroxyurea for treatment of severe sickle cell anemia: A pediatric clinical trial. Blood 1996;88(6):19601964. 15. Kinner TR, Helms RW, OBranski EE, et al., Pediatric Hydroxyurea Group. Safety of hydroxyurea in children with sickle cell anemia: Results of the HUGKIDS study, a phase I/II trial. Blood 1999;94(5):15501554. 16. Zimmerman SA, Schultz WH, Davis JS, et al. Sustained long-term hematologic efficacy of hydroxyurea at maximum tolerated dose in children with sickle cell disease. Blood 2004;103(6):20392045. 17. Marlowe KF, Chicella MF. Treatment of sickle cell pain. Pharmacotherapy 2002;22(4):484491. 18. Gonzalez ER, Bahal N, Hansen LA, et al. Intermittent injection vs. patient-controlled analgesia for sickle cell crisis pain: Comparison in patients in the emergency department. Arch Intern Med 1991;151(7):13731378. 19. Okomo U, Meremikwu MM. Fluid replacement therapy for acute episodes of pain in people with sickle cell disease (Cochrane Review). In: The Cochrane Library. Issue 2, 2007. Article No. CD005406. 20. Steinberg MH. Management of sickle cell disease. N Engl J Med 1999;340:10211029. 21. Falletta JM, Woods GM, Verter JI, et al. Discontinuing penicillin prophylaxis in children with sickle cell anemia. J Pediatr 1995; 127:685690. 22. The Management of Sickle Cell Disease, 4th ed. revised, June 2002. National Institutes of Health/National Heart, Lung, and Blood Institute, Division of Blood Diseases and Resources, NIH Pub No. 02-2117. 23. Gatson MH, Verter JI, Woods G, et al. Prophylaxis with oral penicillin in children with sickle cell anemia: A randomized trial. N Engl J Med 1986;314:15931599. 24. What is sickle cell anemia? National Heart, Lung, and Blood Institute (NHLBI). Available at: www.nhlbi.nih.gov/health/dci/ Diseases/Sca/SCA_WhatIs.html. Accessed August 10, 2007. 25. Pai VB, Nahata MC. Duration of penicillin prophylaxis in sickle cell anemia: Issues and controversies. Pharmacotherapy 2000; 20(1):110117. 26. Centers for Disease Control and Prevention (DCDC). Sickle cell disease: Five tips to help prevent infection. Available at: www. cdc.gov/ncbddd/sicklecell/tips_prevent.htm. Accessed October 16, 2007. 27. Adams RJ, McKie VC, Hsu L et al. Prevention of a first stroke by transfusions in children with sickle cell anemia and abnormal results on transcranial Doppler ultrasonography. N Engl J Med 1998;339:511. 28. The Optimizing Primary Stroke Prevention in Sickle Cell Anemia (STOP 2) Trial Investigators. Discontinuing prophylactic transfusions used to prevent stroke in sickle cell disease. N Engl J Med 2005;353:27692778. 29. Zimmerman SA, Schultz WH, Burgett S, et al. Hydroxyurea therapy lowers transcranial Doppler flow velocities in children with sickle cell anemia. Blood 2007;110:10431047. 30. Vichinsky E, Onyekwere O, Porter J, et al. A randomised comparison of deferasirox versus deferoxamine for the treatment of transfusional iron overload in sickle cell disease. Br J Haematol 2007;136(3):501508. 31. Lerner NB. Aspirin prophylaxis in sickle cell disease. Trial No. NCT00178464. Available at: http://clinicaltrials.gov/ct/show/ NCT00178464?order=1. Accessed September 5, 2007. 32. Stuart MJ, Nagel RL. Sickle cell disease. Lancet 2004;364(9442): 13431360. 33. Rabb LM, Grandison Y, Mason K, et al. A trial of folate supplementation in children with homozygous sickle cell disease. Br J Haematol 1983;54:589594. 34. Rodriguez-Cortez HM, Griener JC, Hyland K, et al. Plasma homocysteine levels and folate status in children with sickle cell anemia. J Pediatr Hematol Oncol 1999;21:219223. 35. Nelson SC, Adade BB, McDonough EA, et al. High prevalence of pulmonary hypertension in children with sickle cell disease. J Pediatr Hematol Oncol 2007;29:334337. 36. Castro O, Hoque M, Brown MD. Pulmonary hypertension in sickle cell disease: Cardiac catheterization results and survival. Blood 2003;101:12571261. 37. Machado RF, Martyr S, Kato GJ et al. Sildenafil therapy in patients with sickle-cell disease and pulmonary hypertension. Br J Haematol 2005;130:445453. 38. Adeyoju AB, Olujohunbge ABK, Morris J, et al. Priapism in sicklecell disease: Incidence, risk factors and complications. An international multicentre study. BJU Int 2002;90(9):898902. 39. Fowler JE, Koshy M, Strub M, et al. Priapism associated with the sickle cell hemoglobinopathies: Prevalence, natural history and sequelae. J Urol 1991;145(1):6568. 40. Pryor J, Akkus E, Alter G, et al. Priapism. J Sex Med 2004;1(1): 116120. 41. Iyamu EW, Turner EA, Asakura T. In vitro effects of niprisan (Nix0699): A naturally occurring, potent antisickling agent. Br J Haematol 2002;118(1):337343. 42. Wambebe C, Khamofu H, Momoh JA, et al. Double-blind, placebocontrolled, randomized cross-over clinical trial of niprisan in patients with sickle cell disorder. Phytomedicine 2001;8(4):252 261. 43. Stuart MJ, Nagel RL. Sickle-cell disease. Lancet 2004;364:1343 1360. 44. Christensen D. Nitric oxide may help treat sickle cell anemia. Science News 2000;157(5):7881. 45. Head CA, Brugnara C, Martinez-Ruiz R, et al. Low concentrations of nitric oxide increase oxygen affinity of sickle erythrocytes in vitro and in vivo. J Clin Invest 1997;100(5):11931198. 46. Waugh WH, Daeschner CW, Files BA, et al. Evidence that L-arginine is a key amino acid in sickle cell anemia: A preliminary report. Nutr Res 1999;19(4):501518. 47. Morris CR, Morris SM, Hagar W, et al. Arginine therapy: A new treatment for pulmonary hypertension in sickle cell disease? Am J Respir Crit Care Med 2003;168:6369. 48. Williams R, Olivi S, Li CS, et al. Oral glutamine supplementation decreases resting energy expenditure in children and adolescents with sickle cell anemia. J Pediatr Hematol Oncol 2004;26(10): 619625. 49. Niihara Y, Zerez CR, Akiyama DS, et al. Increased red cell glutamine availability in sickle cell anemia: Demonstration of increased active transport, affinity, and increased glutamate level in intact red cells. J Lab Clin Med 1997;130(1):8390. 50. Niihara Y, Zerez CR, Akiyama DS, et al. Oral L-glutamine therapy for sickle cell anemia: I. Subjective clinical improvement and favorable change in red cell NAD redox potential. Am J Hematol 1998;58:117121. 51. De Franceschi L, Bachir D, Galacteros F, et al. Oral magnesium supplements reduce erythrocyte dehydration in patients with sickle cell disease. J Clin Invest 1997;100(7):18471852. I
Conflict of Interest (COI) Statement
The authors have no relationships to disclose. The article contains a discussion of off-label use. The content of this article has been reviewed under Jeffersons COI policy.
Vol. 33 No. 4 April 2008
P&T 243
CONTINUING EDUCATION CREDIT
Continuing Education Questions for Physicians and Pharmacists
P&T 2008;33(4):238243 ACPE Program # 079-000-08-016-H01-P Expiration Date: April 30, 2009 TOPIC: Pharmacological Management of Sickle Cell Disease
CME Accreditation
This activity has been planned and implemented in accordance with the Essential Areas and Policies of the Accreditation Council for Continuing Medical Education (ACCME) through the joint sponsorship of Jefferson Medical College and MediMedia USA, Inc. Jefferson Medical College of Thomas Jefferson University, as a member of the Consortium for Academic Continuing Medical Education, is accredited by the Accreditation Council for Continuing Medical Education to sponsor continuing medical education for physicians. All faculty/authors participating in continuing medical education activities sponsored by Jefferson Medical College are expected to disclose to the activity audience any real or apparent conflict(s) of interest related to the content of their article(s). Full disclosure of these relationships appears on the last page of the article.
Continuing Medical Education Credit
This CME activity is designed to assist physicians and other health care professionals who are P&T committee members in making formulary decisions. Its goal is to increase participants ability to recognize and treat important medical problems. Jefferson Medical College designates this continuing medical education activity for a maximum of one Category 1 credit toward the Physicians Recognition Award (PRA) of the American Medical Association. Each physician should claim only those credits that he/she actually spent in the educational activity. This credit is available for the period of one year from the date of publication. Although forms will be processed when received, certificates for CME credits will be issued every six months, in February and August. Interim requests for certificates can be made by contacting the Jefferson Office of Continuing Medical Education at (215) 955-6992 or by going online to http://jeffline.tju.edu/jeffcme/.
Continuing Pharmacy Education Credit
The Department of Health Policy, Thomas Jefferson University Hospital, is approved by the Accreditation Council for Pharmacy Education (ACPE) as a provider of continuing pharmacy education and complies with the Criteria for Quality for continuing pharmacy education programming. This program (079-000-08-016-H01-P) is acceptable for 1.0 hour of continuing education credit (0.1 CEUs) in states that recognize ACPE-approved providers. Statements of Credit indicating hours/CEUs will be mailed within six to eight weeks to participants who completed this activity and submitted a completed evaluation with payment.
How to Apply for CE Credit
1. Each CE article is prefaced by learning objectives for participants to use to determine whether the article relates to their individual learning needs. 2. Read the article carefully, paying particular attention to the tables and other illustrative materials. 3. Complete the questions and fill in the answers on the evaluation form on the next page. 4. Complete the CE Registration and Evaluation Form. Type or print your full name and address in the space provided, and evaluate the activity as requested. In order for the form to be processed, all information must be complete and legible. 5. Payment of $10 per exam is required for processing and maintenance of records. Make checks payable to P&T. This processing fee is non-refundable. 6. Send the completed form, answer sheet, and $10 payment to: Department of Health Policy Thomas Jefferson University Attn: Continuing Education Credit 1015 Walnut Street, Suite 115 Philadelphia, PA 19107 7. Be sure to mail the Registration, Evaluation Form, and $10 payment within one year of the date of publication. After that date, this article will no longer be designated for credit and forms cannot be processed.
244 P&T
April 2008 Vol. 33 No. 4
CONTINUING EDUCATION CREDIT
Continuing Education Questions for Physicians and Pharmacists
TOPIC: Pharmacological Management of Sickle Cell Disease ACPE Program # 079-000-08-016-H01-P
CE Evaluation: Select the one best answer to each of the following questions, and record your response on the examination answer sheet. Complete the additional requested information. Forward the answer sheet, with appropriate payment, to the Department of Health Policy, Thomas Jefferson University Hospital, at the address indicated. A certificate of completion will be mailed within six to eight weeks of receipt of your exam/payment. (A minimum test score of 70% is required.)
Multiple Choice
Select the one correct answer.
1. Sickle cell disease is an inherited blood disorder that: a. affects one of every 1,000 to 1,400 African-American births. b. involves episodes of pain, chronic hemolytic anemia, and severe infections. c. is not a commonly inherited blood disorder in the U.S. d. causes complications only in adulthood. The pathogenesis of sickle cell disease does not include: a. sickling of red blood cells when deoxygenated. b. premature hemolysis of red blood cells. c. obstruction of microvasculature resulting from sickling. d. a change in the alpha-globin polypeptide of the hemoglobin molecule. Bone marrow transplantation is the only cure for sickle cell disease, but it is not a common procedure because of: a. mortality rates exceeding 30%. b. a lack of suitable donors. c. graft failure rates below 50%. d. disease-free survival rates below 30%. Management of sickle cell disease with hydroxyurea: a. may result in reversible bone marrow suppression. b. may be indicated for patients who have had at least three pain crises in the previous three months. c. may prevent complications of sickle cell disease by decreasing polymerization time. d. does not require monitoring complete blood counts. According to the authors, which of the following should be avoided in patients with pain and impaired renal function? a. morphine b. codeine c. hydromorphone d. meperidine
6.
According to authors, the following statements about infection in patients with sickle cell disease are true except: a. Prophylaxis of infection may be discontinued after five years of age. b. Prophylaxis with penicillin is a problem. c. Erythromycin ethyl succinate is not adequate for prophylaxis. d. Functional asplenia can occur as early as six months of age. Iron overload is a complication of the regularly needed transfusions for the treatment of anemia in patients with sickle cell disease. Which of the following medications was found to be safe and effective compared with deferoxamine in the treatment of iron overload? a. folic acid b. vitamin B12 c. deferasirox d. none of the above A deficiency of glutamine, a consequence of sickle cell anemia, may result in the possibility of: a. skeletal muscle wasting. b. immunosuppression. c. improved wound healing. d. all of the above Folic acid is well supported in the primary literature for use in sickle cell disease. a. True b. False
7.
2.
3.
8.
4.
9.
5.
10. In the treatment of dehydration in sickle cell disease, oral magnesium showed considerable: a. decreases in sickle erythrocyte magnesium. b. increases in sickle erythrocyte potassium content. c. increases in the number of dense sickle erythrocytes. d. none of the above
Vol. 33 No. 4 April 2008
P&T 245
CE Registration and Evaluation Form
Date of publication: April 2008 Title: Pharmacological Management of Sickle Cell Disease Authors: Uche Anadu Ndefo, PharmD, BCPS; Angie Eaton Maxwell, PharmD; Huong Nguyen, PharmD Candidate; and Tochukwu L. Chiobi, PharmD Submission deadline: April 30, 2009 ACPE Program # 079-000-08-016-H01-P
Pharmacy and Therapeutics
A Peer-Reviewed Journal for Managed Care and Hospital Formulary Management
Registration
Name: ____________________________________________________________ Degree: ____________________________________ Street address: ______________________________________________ Last 4 Digits of Social Security No. (Web ID): __________ City: ___________________________________ State: _________ Zip:__________ Telephone: _____________________________ E-mail Address: _______________________________________ Check one: I Physician I Pharmacist I Other Time needed to complete this CE activity in hours: I 0.5 hr I 1 hr I 1.5 hr I 2 hr I Other _________________________
Certification: I attest to having completed this CE activity. ___________________________________________________________ Signature (required) Date _______________
Answer Sheet
Please fill in the box next to the letter corresponding to the correct answer
1. a I 2. a I 3. a I 4. a I 5. a I
b I b I b I b I b I
c I c I c I c I c I
d I d I d I d I d I
6. a I 7. a I 8. a I 9. a I 10. a I
b I b I b I b I b I
c I c I c I c I c I
d I d I d I d I d I
Evaluation
Rate the extent to which: 1. Objectives of this activity were met 2. You were satisfied with the overall quality of this activity 3. Content was relevant to your practice needs 4. Participation in this activity changed your knowledge/attitudes 5. You will make a change in your practice as a result of participation in this activity 6. This activity presented scientifically rigorous, unbiased, and balanced information 7. Individual presentations were free of commercial bias 8. Adequate time was available for Q&A I I I I I I I I I I I I I I I Very High I I I I I I High I I I I I I Moderate I I I I I I Low I I I I I I Very Low I I I I I I
9. Which ONE of the following best describes the impact of this activity on your performance: I This program will not change my behavior because my current practice is consistent with what was taught. I This activity will not change my behavior because I do not agree with the information presented. I I need more information before I can change my practice behavior. I I will immediately implement the information into my practice. 10. Will you take any of the following actions as a result of participating in this educational activity (check all that apply) I Discuss new information with other professionals I Discuss with industry representative(s) I Other ____________________________________ I Consult the literature I Participate in another educational activity I None
Send the completed form and $10 payment (make checks payable to P&T) to: Department of Health Policy, Thomas Jefferson University, Attn: Continuing Education Credit, 1015 Walnut Street, Suite 115, Philadelphia, PA 19107.
246 P&T
April 2008 Vol. 33 No. 4
Você também pode gostar
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeNo EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeNota: 4 de 5 estrelas4/5 (5794)
- The Little Book of Hygge: Danish Secrets to Happy LivingNo EverandThe Little Book of Hygge: Danish Secrets to Happy LivingNota: 3.5 de 5 estrelas3.5/5 (399)
- Cmri 2021 NMC New RulesDocumento4 páginasCmri 2021 NMC New RulesSanthosh KumarAinda não há avaliações
- HS RegistryDocumento1 páginaHS RegistrySanthosh KumarAinda não há avaliações
- Dengue Feve1Documento10 páginasDengue Feve1Santhosh KumarAinda não há avaliações
- E HealthDocumento10 páginasE HealthSanthosh KumarAinda não há avaliações
- StarDocumento1 páginaStarSanthosh KumarAinda não há avaliações
- Approved List For NOCDocumento10 páginasApproved List For NOCSanthosh KumarAinda não há avaliações
- Return Form - 692429350311221Documento6 páginasReturn Form - 692429350311221Santhosh KumarAinda não há avaliações
- Infant Radiant WarmerDocumento10 páginasInfant Radiant WarmerSanthosh KumarAinda não há avaliações
- Oxygen Hood - HTTP - WWW - Niceneotech.com - BlogDocumento13 páginasOxygen Hood - HTTP - WWW - Niceneotech.com - BlogSanthosh KumarAinda não há avaliações
- List of Health Service Offices in KeralaDocumento16 páginasList of Health Service Offices in KeralaSanthosh KumarAinda não há avaliações
- Bool BehaviouralDocumento94 páginasBool BehaviouralSanthosh KumarAinda não há avaliações
- COVID19 District Wise Positivity Analysis 29 Jan 2022Documento28 páginasCOVID19 District Wise Positivity Analysis 29 Jan 2022Santhosh KumarAinda não há avaliações
- Intravenous Fluid Therapy in Children and Young People in Hospital PDF 1837340295109 PDFDocumento35 páginasIntravenous Fluid Therapy in Children and Young People in Hospital PDF 1837340295109 PDFFidel BareaAinda não há avaliações
- Application for PostDocumento3 páginasApplication for PostSanthosh KumarAinda não há avaliações
- Nephrotic SyndromeDocumento6 páginasNephrotic SyndromeSanthosh KumarAinda não há avaliações
- Nephrotic SyndromeDocumento6 páginasNephrotic SyndromeSanthosh KumarAinda não há avaliações
- CHICAGODocumento2 páginasCHICAGOSanthosh KumarAinda não há avaliações
- WWW - Medicalppt.: For More Free Medical Powerpoint Presentations Visit WebsiteDocumento15 páginasWWW - Medicalppt.: For More Free Medical Powerpoint Presentations Visit WebsiteJoko Sutrisno,S.Kep,Ns.M.KesAinda não há avaliações
- Doctor On Duty Health Services KeralaDocumento2 páginasDoctor On Duty Health Services KeralaSanthosh Kumar0% (1)
- Floor 2500 Cam 4650 Rain 1190 4760 To Gaurds 5000 Seat 5821 22731 7000Documento5 páginasFloor 2500 Cam 4650 Rain 1190 4760 To Gaurds 5000 Seat 5821 22731 7000Santhosh KumarAinda não há avaliações
- March 2017: ST Current Month Cumilative Total Year Total ST TotalDocumento2 páginasMarch 2017: ST Current Month Cumilative Total Year Total ST TotalSanthosh KumarAinda não há avaliações
- Fao Hunger MapDocumento1 páginaFao Hunger Mapfercho120Ainda não há avaliações
- Multisystem Inflammatory Syndrome in Children (MIS-C) Interim GuidanceDocumento7 páginasMultisystem Inflammatory Syndrome in Children (MIS-C) Interim GuidanceSanthosh KumarAinda não há avaliações
- Report of District Cancer Care Unit: Particulars Up To TotalDocumento1 páginaReport of District Cancer Care Unit: Particulars Up To TotalSanthosh KumarAinda não há avaliações
- March 2017: ST Current Month Cumilative Total Year Total ST TotalDocumento2 páginasMarch 2017: ST Current Month Cumilative Total Year Total ST TotalSanthosh KumarAinda não há avaliações
- E2020040279 FullDocumento25 páginasE2020040279 FullSanthosh KumarAinda não há avaliações
- Report of District Cancer Care Unit: Particulars Up To TotalDocumento1 páginaReport of District Cancer Care Unit: Particulars Up To TotalSanthosh KumarAinda não há avaliações
- March 2017: ST Current Month Cumilative Total Year Total ST TotalDocumento2 páginasMarch 2017: ST Current Month Cumilative Total Year Total ST TotalSanthosh KumarAinda não há avaliações
- GO (P) No 07-2016-Fin Dated 20.01.16 With Index PDFDocumento359 páginasGO (P) No 07-2016-Fin Dated 20.01.16 With Index PDFvpzfarisAinda não há avaliações
- E2020040279 FullDocumento25 páginasE2020040279 FullSanthosh KumarAinda não há avaliações
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryNo EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryNota: 3.5 de 5 estrelas3.5/5 (231)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceNo EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceNota: 4 de 5 estrelas4/5 (894)
- The Yellow House: A Memoir (2019 National Book Award Winner)No EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Nota: 4 de 5 estrelas4/5 (98)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureNo EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureNota: 4.5 de 5 estrelas4.5/5 (474)
- Never Split the Difference: Negotiating As If Your Life Depended On ItNo EverandNever Split the Difference: Negotiating As If Your Life Depended On ItNota: 4.5 de 5 estrelas4.5/5 (838)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaNo EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaNota: 4.5 de 5 estrelas4.5/5 (265)
- The Emperor of All Maladies: A Biography of CancerNo EverandThe Emperor of All Maladies: A Biography of CancerNota: 4.5 de 5 estrelas4.5/5 (271)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersNo EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersNota: 4.5 de 5 estrelas4.5/5 (344)
- Team of Rivals: The Political Genius of Abraham LincolnNo EverandTeam of Rivals: The Political Genius of Abraham LincolnNota: 4.5 de 5 estrelas4.5/5 (234)
- The Unwinding: An Inner History of the New AmericaNo EverandThe Unwinding: An Inner History of the New AmericaNota: 4 de 5 estrelas4/5 (45)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyNo EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyNota: 3.5 de 5 estrelas3.5/5 (2219)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreNo EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreNota: 4 de 5 estrelas4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)No EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Nota: 4.5 de 5 estrelas4.5/5 (119)
- Thesis On Education System of PakistanDocumento5 páginasThesis On Education System of Pakistaniouliakingbellevue100% (2)
- Division of Las Pinas Golden Acres National High School: I. ObjectivesDocumento2 páginasDivision of Las Pinas Golden Acres National High School: I. ObjectivesARVEE DAVE GIPA100% (1)
- Music 8 SLM Q1 Module - 2Documento23 páginasMusic 8 SLM Q1 Module - 2Glydel Mae Villamora - SaragenaAinda não há avaliações
- SpinozaDocumento310 páginasSpinozaRamy Al-Gamal100% (4)
- Readiness For Enhanced Knowledge HealthDocumento2 páginasReadiness For Enhanced Knowledge HealthSenyorita KHaye92% (12)
- REVIEW OF RELATED LITERATURE - Docx JasminDocumento6 páginasREVIEW OF RELATED LITERATURE - Docx JasminRay Jefferson ValdonAinda não há avaliações
- Sec Young Fathers Flyer - JuneDocumento1 páginaSec Young Fathers Flyer - JuneMarcus AttheCenter FlenaughAinda não há avaliações
- Newsletter 1982 460Documento12 páginasNewsletter 1982 460api-241041476Ainda não há avaliações
- RA 1425 Significance and ValuesDocumento4 páginasRA 1425 Significance and ValuesRed MonteroAinda não há avaliações
- Architectural Design 3 - Lecture 0 - Welcome OrientationDocumento15 páginasArchitectural Design 3 - Lecture 0 - Welcome OrientationBrigitte ParagasAinda não há avaliações
- Frei Universitat PDFDocumento167 páginasFrei Universitat PDFalnaturamilkaAinda não há avaliações
- Math 7 Q4 Module 1Documento12 páginasMath 7 Q4 Module 1Joseph Agustin50% (4)
- AICB Compliance DPSDocumento7 páginasAICB Compliance DPSAravind Hades0% (1)
- Alexander Rosenberg - Philosophy of Social ScienceDocumento15 páginasAlexander Rosenberg - Philosophy of Social Sciencegabay123Ainda não há avaliações
- Guidelines For The USC Vol CorpsDocumento3 páginasGuidelines For The USC Vol CorpsAngeli GuadalupeAinda não há avaliações
- Effect of Romantic Relationship On Undergraduate Students' Academic Performance: A Case Study of Islamic University in UgandaDocumento9 páginasEffect of Romantic Relationship On Undergraduate Students' Academic Performance: A Case Study of Islamic University in UgandaJohn Miller CaliaoAinda não há avaliações
- Systems Archetypes II TRSA02EDocumento31 páginasSystems Archetypes II TRSA02EMariani Sinaga100% (1)
- Universe in Nutshell Hawking ReviewDocumento3 páginasUniverse in Nutshell Hawking ReviewVladica Barjaktarovic100% (1)
- Sustainable Sweden: VästeråsDocumento17 páginasSustainable Sweden: VästeråsFoundation for Indian Scientific Heritage FISHAinda não há avaliações
- Guidelines For Demonstration Teaching General GuidelinesDocumento2 páginasGuidelines For Demonstration Teaching General GuidelinesAmor Rosario EspinaAinda não há avaliações
- Architects DONEDocumento10 páginasArchitects DONEAyu Amrish Gupta0% (1)
- Correction and Repair in Language TeachingDocumento3 páginasCorrection and Repair in Language TeachingAwg Zainal AbidinAinda não há avaliações
- Cambridge Assessment International Education: This Document Consists of 7 Printed PagesDocumento7 páginasCambridge Assessment International Education: This Document Consists of 7 Printed Pagestaqi razaAinda não há avaliações
- Module On Contemporary Philippine ArtsDocumento7 páginasModule On Contemporary Philippine ArtsJohn Wowa MalayaAinda não há avaliações
- La Comunicación Médico - PacienteDocumento8 páginasLa Comunicación Médico - PacienteHugo SanchezAinda não há avaliações
- TM Develop & Update Tour Ind Knowledge 310812Documento82 páginasTM Develop & Update Tour Ind Knowledge 310812Phttii phttii100% (1)
- Drama Games For Acting ClassesDocumento12 páginasDrama Games For Acting ClassesAnirban Banik75% (4)
- Developing Interprofessional Competencies in Professional PsychologyDocumento32 páginasDeveloping Interprofessional Competencies in Professional PsychologyCharleneKronstedtAinda não há avaliações
- Media LiteracyDocumento16 páginasMedia LiteracyRLM100% (2)
- Frame CorrectionDocumento32 páginasFrame CorrectionsahayaAinda não há avaliações