Escolar Documentos
Profissional Documentos
Cultura Documentos
Warfarin - Drug Information
Enviado por
TestesteDescrição original:
Título original
Direitos autorais
Formatos disponíveis
Compartilhar este documento
Compartilhar ou incorporar documento
Você considera este documento útil?
Este conteúdo é inapropriado?
Denunciar este documentoDireitos autorais:
Formatos disponíveis
Warfarin - Drug Information
Enviado por
TestesteDireitos autorais:
Formatos disponíveis
Warfarin: Drug information
http://www.uptodate.com/contents/warfarin-drug-information...
Official reprint from UpToDate www.uptodate.com 2012 UpToDate
Warfarin: Drug information
Copyright 1978-2012 Lexicomp, Inc. All rights reserved. (For additional information see "Warfarin: Patient drug information" and see "Warfarin: Pediatric drug information")
Special Alerts
Warfarin (Jantoven): Recall Due to Mislabeled Bottle (Update) February 2011 Upsher-Smith Laboratories has initiated a voluntary recall of Jantoven warfarin sodium tablets. The precautionary recall was prompted after a single bottle labeled with 3 mg tablets (tan colored tablets) was found to actually contain the 10 mg strength tablets (white colored tablets). The risk of administering a 10 mg strength tablet in place of the intended 3 mg strength tablet could potentially result in life-threatening hemorrhage. As an additional precautionary measure, Upsher-Smith Laboratories has expanded its previously announced recall to include additional products and lots produced on the same line during a similar period of time. For the most recent information, including the products recalled, please refer to http://www.upsher-smith.com.
ALERT: U.S. Boxed Warning
The FDA-approved labeling includes a boxed warning. See Warnings/Precautions section for a concise summary of this information. For verbatim wording of the boxed warning, consult the product labeling or www.fda.gov.
Brand Names: U.S.
Coumadin; Jantoven Apo-Warfarin; Coumadin; Mylan-Warfarin;
Brand Names: Canada
Novo-Warfarin; Taro-Warfarin
Medication Guide
An FDA-approved patient medication guide, which is available with the product information and at http://www.fda.gov/downloads/Drugs/DrugSafety /ucm088578.pdf, must be dispensed with this medication.
Pharmacologic Category
Antagonist
Anticoagulant, Coumarin Derivative; Vitamin K
Dosing: Adult
Note: Labeling identifies genetic factors which may increase patient sensitivity to warfarin. Specifically, genetic variations in the proteins CYP2C9 and VKORC1, responsible for warfarins primary metabolism and pharmacodynamic activity, respectively, have been identified as predisposing factors associated with decreased dose requirement and increased bleeding risk. Genotyping tests are available, and may provide important guidance on initiation of anticoagulant therapy.
1 de 23
02/01/12 21:28
Warfarin: Drug information
http://www.uptodate.com/contents/warfarin-drug-information...
Prevention/treatment of thrombosis/embolism: I.V. (administer as a slow bolus injection): 2-5 mg/day Oral: Initial dosing must be individualized. Consider the patient (hepatic function, cardiac function, age, nutritional status, concurrent therapy, risk of bleeding) in addition to prior dose response (if available) and the clinical situation. Start 2-5 mg daily for 2 days or 5-10 mg daily for 1-2 days (Ansell, 2008). Adjust dose according to INR results; usual maintenance dose ranges from 2-10 mg daily (individual patients may require loading and maintenance doses outside these general guidelines). Note: Lower starting doses may be required for patients with hepatic impairment, poor nutrition, CHF, elderly, high risk of bleeding, or patients who are debilitated, or those with reduced function genomic variants of the catabolic enzymes CYP2C9 (*2 or *3 alleles) or VKORC1 (-1639 polymorphism); see table. Higher initial doses may be reasonable in selected patients (ie, receiving enzyme-inducing agents and with low risk of bleeding).
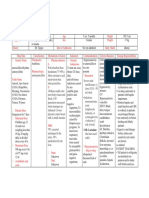
Range1 of Expected Therapeutic Maintenance Dose Based on CYP2C92 and VKORC13 Genotypes VKORC1 *1/*1 GG AG AA 5-7 mg 5-7 mg 3-4 mg *1/*2 5-7 mg 3-4 mg 3-4 mg CYP2C9 *1/*3 3-4 mg 3-4 mg *2/*2 3-4 mg 3-4 mg *2/*3 3-4 mg *3/*3 0.5-2 mg
0.5-2 mg 0.5-2 mg
0.5-2 mg 0.5-2 mg 0.5-2 mg 0.5-2 mg
Note: Must also take into account other patient related factors when determining initial dose (eg, age, body weight, concomitant medications, comorbidities).
1
Ranges derived from multiple published clinical studies. Patients with CYP2C9 *1/*3, *2/*2, *2/*3, and *3/*3 alleles may take up to 4 weeks to achieve maximum INR with a given dose regimen. VKORC1 -1639G>A (rs 9923231) variant is used in this table; other VKORC1 variants may also be important determinants of dose.
Dosing: Pediatric
2 de 23
02/01/12 21:28
Warfarin: Drug information
http://www.uptodate.com/contents/warfarin-drug-information...
(For additional information see "Warfarin: Pediatric drug information") Prevention/treatment of thrombosis: Oral: Infants and Children (unlabeled use): Initial loading dose (if baseline INR is 1-1.3): 0.2 mg/kg (maximum: 10 mg/dose); adjust dose based on INR (reported ranges to maintain INR of 2-3: 0.09-0.33 mg/kg/day). Infants <12 months of age may require doses at or near the high end of this range; consistent anticoagulation may be difficult to maintain in children <5 years of age.
Dosing: Geriatric
Oral: Initial dose 5 mg. Usual maintenance dose: 2-5 mg/day. The elderly tend to require lower dosages to produce a therapeutic level of anticoagulation (due to changes in the pattern of warfarin metabolism).
Dosing: Renal Impairment
No adjustment required, however, patients with renal failure have an increased risk of bleeding complications. Monitor closely.
Dosing: Hepatic Impairment
Monitor effect at usual doses. The response to oral anticoagulants may be markedly enhanced in obstructive jaundice, hepatitis, and cirrhosis. INR should be closely monitored.
Dosage Forms: U.S.
Excipient information presented when available (limited, particularly for generics); consult specific product labeling. Injection, powder for reconstitution, as sodium: Coumadin: 5 mg Tablet, oral, as sodium: 1 mg, 2 mg, 2.5 mg, 3 mg, 4 mg, 5 mg, 6 mg, 7.5 mg, 10 mg Coumadin: 1 mg, 2 mg, 2.5 mg, 3 mg, 4 mg, 5 mg, 6 mg, 7.5 mg [scored] Coumadin: 10 mg [scored; dye free] Jantoven: 1 mg, 2 mg, 2.5 mg, 3 mg, 4 mg, 5 mg, 6 mg, 7.5 mg [scored] Jantoven: 10 mg [scored; dye free]
Generic Equivalent Available: U.S. Administration
Yes: Tablet
Oral: Administer with or without food. Take at the same time each day. I.V.: Administer as a slow bolus injection over 1-2 minutes; avoid all I.M. injections
Compatibility
Stable in D5LR, D51/2NS, D5NS, D5W, D10W, variable stability (consult detailed reference) in LR, NS. Y-site administration: Compatible: Amikacin, ascorbic acid injection, bivalirudin, cefazolin, dopamine, epinephrine, heparin, lidocaine, morphine, nitroglycerin, oxytocin, potassium chloride, ranitidine. Incompatible: Aminophylline, ceftazidime, cimetidine, ciprofloxacin, dobutamine, esmolol, gentamicin, labetalol. Variable (consult detailed reference): Ammonium chloride, ceftriaxone, metronidazole, vancomycin. Compatibility in syringe: Incompatible: Ceftriaxone, heparin.
Use
Prophylaxis and treatment of thromboembolic disorders (eg, venous, pulmonary)
3 de 23
02/01/12 21:28
Warfarin: Drug information
http://www.uptodate.com/contents/warfarin-drug-information...
and embolic complications arising from atrial fibrillation or cardiac valve replacement; adjunct to reduce risk of systemic embolism (eg, recurrent MI, stroke) after myocardial infarction
Use - Unlabeled/Investigational
attacks
Prevention of recurrent transient ischemic
Medication Safety Issues
Sound-alike/look-alike issues: Coumadin may be confused with Avandia, Cardura, Compazine, Kemadrin Jantoven may be confused with Janumet, Januvia High alert medication: The Institute for Safe Medication Practices (ISMP) includes this medication among its list of drugs which have a heightened risk of causing significant patient harm when used in error. 2009 National Patient Safety Goals: The Joint Commission on Accreditation of Healthcare Organizations requires healthcare organizations that provide anticoagulant therapy to have a process in place to reduce the risk of anticoagulant-associated patient harm. Patients receiving anticoagulants should receive individualized care through a defined process that includes standardized ordering, dispensing, administration, monitoring and education. This does not apply to routine short-term use of anticoagulants for prevention of venous thromboembolism when the expectation is that the patients laboratory values will remain within or close to normal values (NPSG.03.05.01).
Adverse Reactions Significant
Bleeding is the major adverse effect of warfarin. Hemorrhage may occur at virtually any site. Risk is dependent on multiple variables, including the intensity of anticoagulation and patient susceptibility. Cardiovascular: Angina, chest pain, edema, hemorrhagic shock, hypotension, pallor, syncope, vasculitis Central nervous system: Coma, dizziness, fatigue, fever, headache, lethargy, malaise, pain, stroke Dermatologic: Alopecia, bullous eruptions, dermatitis, rash, pruritus, urticaria Gastrointestinal: Abdominal cramps, abdominal pain, anorexia, diarrhea, flatulence, gastrointestinal bleeding, mouth ulcers, nausea, taste disturbance, vomiting Genitourinary: Hematuria, priapism Hematologic: Agranulocytosis, anemia, leukopenia, retroperitoneal hematoma, unrecognized bleeding sites (eg, colon cancer) may be uncovered by anticoagulation Hepatic: Cholestatic jaundice, hepatic injury, hepatitis, transaminases increased Neuromuscular & skeletal: Joint pain, muscle pain, osteoporosis (potential association with
4 de 23
02/01/12 21:28
Warfarin: Drug information
http://www.uptodate.com/contents/warfarin-drug-information...
long-term use), paralysis, paresthesia, weakness Respiratory: Dyspnea, tracheobronchial calcification Miscellaneous: Anaphylactic reaction, cold intolerance, hypersensitivity/allergic reactions, skin necrosis, gangrene, purple toes syndrome
Contraindications
Hypersensitivity to warfarin or any component of the formulation; hemorrhagic tendencies (eg, patients bleeding from the GI, respiratory, or GU tract; aneurysm; cerebrovascular hemorrhage; following spinal puncture and other diagnostic or therapeutic procedures with potential for significant bleeding; history of bleeding diathesis); recent or potential surgery of the eye or CNS; major regional lumbar block anesthesia or surgery resulting in large, open surfaces; blood dyscrasias; severe uncontrolled or malignant hypertension; pericarditis or pericardial effusion; subacute bacterial endocarditis; history of warfarin-induced necrosis; an unreliable, noncompliant patient; alcoholism; patient who has a history of falls or is a significant fall risk; unsupervised senile or psychotic patient; eclampsia/pre-eclampsia, threatened abortion, pregnancy
Warnings/Precautions
Boxed warnings: Bleeding: See Concerns related to adverse effects below. Special handling: Hazardous agent: Use appropriate precautions for handling and disposal. Concerns related to adverse effects: Anaphylaxis/hypersensitivity: May cause hypersensitivity reactions, anaphylaxis; use with caution in patients with anaphylactic disorders. including
Bleeding: [U.S. Boxed Warning]: May cause major or fatal bleeding. Risk factors for bleeding include high intensity anticoagulation (INR >4), age (65 years), variable INRs, history of GI bleeding, hypertension, cerebrovascular disease, serious heart disease, anemia, severe diabetes, malignancy, trauma, renal insufficiency, polycythemia vera, vasculitis, open wound, history of PUD, indwelling catheters, menstruating and postpartum women, drug-drug interactions, long duration of therapy, or known genetic deficiency in CYP2C9 activity. Patient must be instructed to report bleeding, accidents, or falls as well as any new or discontinued medications, herbal or alternative products used, or significant changes in smoking or dietary habits. Unrecognized bleeding sites (eg, colon cancer) may be uncovered by anticoagulation. Skin necrosis/gangrene: Necrosis or gangrene of the skin and other tissue can occur (rarely, <0.1%) due to paradoxical local thrombosis; onset is usually within the first few days of therapy and is frequently localized to the limbs, breast, or penis. The risk of this effect is increased in patients with protein C or S deficiency. Purple toe syndrome, due to cholesterol microembolization, has been rarely described with coumarin-type anticoagulants. Typically, this occurs after several weeks of therapy, and may present as a dark, purplish, mottled discoloration of the plantar and lateral surfaces. Other manifestations of cholesterol microembolization
5 de 23
02/01/12 21:28
Warfarin: Drug information
http://www.uptodate.com/contents/warfarin-drug-information...
may include rash; livedo reticularis; gangrene; abrupt and intense pain in lower extremities; abdominal, flank, or back pain; hematuria, renal insufficiency; hypertension; cerebral ischemia; spinal cord infarction; or other symptoms of vascular compromise. Disease-related concerns: Dietary insufficiency: Use with caution insufficiencies (vitamin K deficiency). in patients with prolonged dietary
Heparin-induced thrombocytopenia: Use with caution in patients with heparininduced thrombocytopenia and DVT; limb ischemia, necrosis, and gangrene have occurred when warfarin was started or continued after heparin was stopped. Warfarin monotherapy is contraindicated in the initial treatment of active HIT; warfarin initially inhibits the synthesis of protein C, potentially accelerating the underlying active thrombotic process. Hepatic impairment: Reduced liver function, regardless of etiology, may impair synthesis of coagulation factors leading to increased warfarin sensitivity. Infection: Use with caution in patients with acute infection or active TB or any disruption of normal GI flora; antibiotics and fever may alter response to warfarin. Renal impairment: Use with caution in patients with moderate-to-severe renal impairment. Thyroid disease: Use with caution in patients with thyroid disease. Special populations: Elderly: The elderly may be more sensitive to anticoagulant therapy. Ovulating women: May be at risk of developing ovarian hemorrhage at the time of ovulation. Patients with genomic variants in CYP2C9 and/or VKORC1: Presence of the CYP2C9*2 or *3 allele and/or polymorphism of the vitamin K oxidoreductase (VKORC1) gene may increase the risk of bleeding. The *2 allele is reported to occur with a frequency of 4% to 11% in African-Americans and Caucasians, respectively, while the *3 allele frequencies are 2% to 7% respectively. Other variant 2C9 alleles (eg, *5, *6, *9, and *11) are also associated with reduced metabolic activity and thus may increase risk of bleeding, but are much less common. Lower doses may be required in these patients; genetic testing may help determine appropriate dosing. Pediatrics: Safety and efficacy have not been established in children; monitor closely. Other warnings/precautions: Patient selection: Use care in the selection of patients appropriate for this treatment; ensure patient cooperation especially from the alcoholic, illicit drug user, demented, or psychotic patient; ability to comply with routine laboratory monitoring is essential.
Metabolism/Transport Effects Drug Interactions
6 de 23
Substrate of CYP1A2 (minor), 2C9 (major), 2C19 (minor), 3A4 (minor); Inhibits CYP2C9 (moderate), 2C19 (weak)
02/01/12 21:28
Warfarin: Drug information
http://www.uptodate.com/contents/warfarin-drug-information...
(For additional information: Launch Lexi-Interact Drug Interactions Program ) Acetaminophen: May enhance the anticoagulant effect of Vitamin K Antagonists. Most likely with daily acetaminophen doses >1.3 g for >1 week. Risk C: Monitor therapy Allopurinol: May enhance the anticoagulant effect of Vitamin K Antagonists. Risk D: Consider therapy modification Aminoglutethimide: May increase the metabolism of Vitamin K Antagonists. Risk D: Consider therapy modification Amiodarone: May enhance the anticoagulant effect of Vitamin K Antagonists. Risk D: Consider therapy modification Androgens: May enhance the anticoagulant effect of Vitamin K Antagonists. Risk D: Consider therapy modification Anticoagulants: May enhance the anticoagulant effect of other Anticoagulants. Risk C: Monitor therapy Antineoplastic Agents: May enhance the anticoagulant effect of Vitamin K Antagonists. Antineoplastic Agents may diminish the anticoagulant effect of Vitamin K Antagonists. Exceptions: Alitretinoin; Altretamine; Aminoglutethimide; Anastrozole; Asparaginase; AzaCITIDine; Bleomycin; Capecitabine; CARBOplatin; Carmustine; Chlorambucil; CISplatin; Cladribine; Cytarabine; Cytarabine (Liposomal); Dacarbazine; DACTINomycin; DAUNOrubicin Citrate (Liposomal); DAUNOrubicin Hydrochloride; Denileukin Diftitox; DOCEtaxel; DOXOrubicin (Liposomal); Epirubicin; Estramustine; Etoposide Phosphate; Exemestane; Fludarabine; Goserelin; Hydroxyurea; IDArubicin; Irinotecan; Letrozole; Leuprolide; Lomustine; Mechlorethamine; Megestrol; MitoMYcin; MitoXANtrone; Nilutamide; PACLitaxel; Pegaspargase; Pentostatin; Polyestradiol; Porfimer; RiTUXimab; Streptozocin; Tamoxifen; Temozolomide; Teniposide; Thioguanine; Thiotepa; Topotecan; Toremifene; Tretinoin (Systemic); Valrubicin; VinBLAStine; Vinorelbine. Risk C: Monitor therapy Antiplatelet Agents: May enhance the anticoagulant effect of Anticoagulants. Risk C: Monitor therapy Antithyroid Agents: May diminish the anticoagulant effect of Vitamin K Antagonists. Risk D: Consider therapy modification Aprepitant: May decrease the serum concentration of Warfarin. Risk C: Monitor therapy Atazanavir: May increase the serum concentration of Warfarin. Risk C: Monitor therapy AzaTHIOprine: May diminish the anticoagulant effect of Vitamin K Antagonists. Risk C: Monitor therapy Barbiturates: May increase the metabolism of Vitamin K Antagonists. Risk D: Consider therapy modification Bicalutamide: May increase the serum concentration of Vitamin K Antagonists. Specifically, free concentrations of the vitamin K antagonists may be increased. Risk C: Monitor therapy Bile Acid Sequestrants: May decrease the absorption of Vitamin K Antagonists. Risk C:
7 de 23
02/01/12 21:28
Warfarin: Drug information
http://www.uptodate.com/contents/warfarin-drug-information...
Monitor therapy Boceprevir: May decrease the serum concentration of Warfarin. Boceprevir may increase the serum concentration of Warfarin. Risk C: Monitor therapy Bosentan: May increase the metabolism of Vitamin K Antagonists. Risk C: Monitor therapy Capecitabine: May increase the serum concentration of Vitamin K Antagonists. Risk D: Consider therapy modification CarBAMazepine: May decrease the serum concentration of Vitamin K Antagonists. Risk D: Consider therapy modification Cephalosporins: May enhance the anticoagulant effect of Vitamin K Antagonists. Exceptions: Cefaclor; Cefadroxil; Cefdinir; Cefditoren; Cefepime; Cefixime; Cefotaxime; Cefpodoxime; Cefprozil; Ceftaroline Fosamil; CefTAZidime; Ceftibuten; Cefuroxime; Cephalexin. Risk C: Monitor therapy Chloral Hydrate: May increase the serum concentration of Vitamin K Antagonists. Risk C: Monitor therapy Chloramphenicol: May enhance the anticoagulant effect of Vitamin K Antagonists. Chloramphenicol may increase the serum concentration of Vitamin K Antagonists. Risk C: Monitor therapy Cimetidine: May enhance the anticoagulant effect of Vitamin K Antagonists. Risk D: Consider therapy modification Clopidogrel: May enhance the anticoagulant effect of Warfarin. Risk D: Consider therapy modification Coenzyme Q-10: May diminish the anticoagulant effect of Vitamin K Antagonists. Risk C: Monitor therapy Collagenase (Systemic): Anticoagulants may enhance the adverse/toxic effect of Collagenase (Systemic). Specifically, the risk of injection site bruising and/or bleeding may be increased. Risk C: Monitor therapy Contraceptives (Estrogens): May diminish the anticoagulant effect of Vitamin K Antagonists. In contrast, enhanced anticoagulant effects have also been noted with some products. Risk D: Consider therapy modification Contraceptives (Progestins): May diminish the anticoagulant effect of Vitamin K Antagonists. In contrast, enhanced anticoagulant effects have also been noted with some products. Management: When possible, concomitant hormonal contraceptives and coumarin derivatives should be avoided in order to eliminate the risk of thromboembolic disorders. Consider using an alternative, nonhormonal contraceptive. Risk D: Consider therapy modification Corticosteroids (Systemic): May enhance the anticoagulant effect of Warfarin. Risk C: Monitor therapy Cranberry: May enhance the anticoagulant effect of Vitamin K Antagonists. Risk C: Monitor therapy CYP2C9 Inducers (Highly Effective): May increase the metabolism of CYP2C9 Substrates (High risk). Risk C: Monitor therapy
8 de 23
02/01/12 21:28
Warfarin: Drug information
http://www.uptodate.com/contents/warfarin-drug-information...
CYP2C9 Inhibitors (Moderate): May decrease the metabolism of CYP2C9 Substrates (High risk). Risk C: Monitor therapy CYP2C9 Inhibitors (Strong): May decrease the metabolism of CYP2C9 Substrates (High risk). Risk D: Consider therapy modification Cyproterone: May decrease the serum concentration of CYP1A2 Substrates. Risk C: Monitor therapy Darunavir: May decrease the serum concentration of Warfarin. Risk C: Monitor therapy Deferasirox: Anticoagulants may enhance the adverse/toxic effect of Deferasirox. Specifically, the risk for GI ulceration/irritation or GI bleeding may be increased. Risk C: Monitor therapy Desvenlafaxine: May enhance the adverse/toxic effect of Vitamin K Antagonists. Specifically, the risk for bleeding may be increased. Risk C: Monitor therapy Dexmethylphenidate: May increase the serum concentration of Vitamin K Antagonists. Risk C: Monitor therapy Dicloxacillin: May diminish the anticoagulant effect of Vitamin K Antagonists. Risk C: Monitor therapy Disulfiram: May increase the serum concentration of Vitamin K Antagonists. Risk C: Monitor therapy Dronedarone: May increase the serum concentration of Vitamin K Antagonists. Risk C: Monitor therapy Drotrecogin Alfa: Vitamin K Antagonists may enhance the adverse/toxic effect of Drotrecogin Alfa. Bleeding may occur. Management: Weigh potential benefits of drotrecogin against increased bleeding risk in patients who have received oral anticoagulants within 1 week or have INR 3 or greater. Monitor for bleeding and immediately stop infusion if clinically important bleeding occurs. Risk D: Consider therapy modification Efavirenz: May decrease the serum concentration of Vitamin K Antagonists. Efavirenz may increase the serum concentration of Vitamin K Antagonists. Risk C: Monitor therapy Erythromycin (Ophthalmic): May increase the serum concentration of Vitamin K Antagonists. Risk C: Monitor therapy Esomeprazole: May increase the serum concentration of Vitamin K Antagonists. Risk C: Monitor therapy Ethacrynic Acid: May increase the serum concentration of Vitamin K Antagonists. Risk C: Monitor therapy Ethotoin: May enhance the anticoagulant effect of Vitamin K Antagonists. Vitamin K Antagonists may increase the serum concentration of Ethotoin. Management: Anticoagulant dose adjustment will likely be necessary when ethotoin is initiated or discontinued. Monitor patients extra closely (INR and signs/symptoms of bleeding) when using this combination. Risk D: Consider therapy modification Etoposide: May enhance the anticoagulant effect of Vitamin K Antagonists. Risk C: Monitor therapy
9 de 23
02/01/12 21:28
Warfarin: Drug information
http://www.uptodate.com/contents/warfarin-drug-information...
Exenatide: May enhance the anticoagulant effect of Vitamin K Antagonists. Risk C: Monitor therapy Fenofibrate: May enhance the anticoagulant effect of Warfarin. Fenofibrate may increase the serum concentration of Warfarin. Risk D: Consider therapy modification Fenofibric Acid: May enhance the anticoagulant effect of Warfarin. Fenofibric Acid may increase the serum concentration of Warfarin. Risk D: Consider therapy modification Fenugreek: May enhance the anticoagulant effect of Vitamin K Antagonists. Risk C: Monitor therapy Fibric Acid Derivatives: May enhance the anticoagulant effect of Vitamin K Antagonists. Risk D: Consider therapy modification Fluconazole: May increase the serum concentration of Vitamin K Antagonists. Risk D: Consider therapy modification Fluorouracil: May increase the serum concentration of Vitamin K Antagonists. Risk D: Consider therapy modification Fluorouracil (Systemic): May increase the serum concentration of Vitamin K Antagonists. Risk D: Consider therapy modification Fluorouracil (Topical): May increase the serum concentration of Vitamin K Antagonists. Risk C: Monitor therapy Fosamprenavir: May increase the serum concentration of Warfarin. Risk C: Monitor therapy Fosaprepitant: May decrease the serum concentration of Warfarin. The active metabolite aprepitant is likely responsible for this effect. Risk C: Monitor therapy Fosphenytoin: May enhance the anticoagulant effect of Vitamin K Antagonists. Vitamin K Antagonists may increase the serum concentration of Fosphenytoin. Management: Anticoagulant dose adjustment will likely be necessary when phenytoin is initiated or discontinued. Monitor patients extra closely (INR and signs/symptoms of bleeding) when using this combination. Risk D: Consider therapy modification Gefitinib: May enhance the anticoagulant effect of Vitamin K Antagonists. Risk C: Monitor therapy Ginkgo Biloba: May enhance the adverse/toxic effect of Vitamin K Antagonists. Management: Consider avoiding the use of this combination of agents. Monitor for signs and symptoms of bleeding if vitamin K antagonists and Ginkgo biloba are used concomitantly. Risk D: Consider therapy modification Ginseng (American): May decrease the serum concentration of Warfarin. Risk C: Monitor therapy Glucagon: May enhance the anticoagulant effect of Vitamin K Antagonists. Risk C: Monitor therapy Glutethimide: May increase the metabolism of Vitamin K Antagonists. Risk D: Consider therapy modification Green Tea: May enhance the adverse/toxic effect of Vitamin K Antagonists. Particularly, the risk of bleeding may be increased due to possible antiplatelet effects of green tea.
10 de 23
02/01/12 21:28
Warfarin: Drug information
http://www.uptodate.com/contents/warfarin-drug-information...
Green Tea may diminish the anticoagulant effect of Vitamin K Antagonists. Risk C: Monitor therapy Griseofulvin: May decrease the serum concentration of Vitamin K Antagonists. Risk C: Monitor therapy Herbs (Anticoagulant/Antiplatelet Properties) (eg, Alfalfa, Anise, Bilberry): May enhance the adverse/toxic effect of Anticoagulants. Bleeding may occur. Risk D: Consider therapy modification HMG-CoA Reductase Inhibitors: May enhance the anticoagulant effect of Vitamin K Antagonists. Exceptions: Atorvastatin. Risk C: Monitor therapy Ifosfamide: May enhance the anticoagulant effect of Vitamin K Antagonists. Risk C: Monitor therapy Imatinib: May enhance the anticoagulant effect of Warfarin. Imatinib may decrease the metabolism of Warfarin. Risk D: Consider therapy modification Itraconazole: May increase the serum concentration of Vitamin K Antagonists. Risk C: Monitor therapy Ivermectin: May enhance the anticoagulant effect of Vitamin K Antagonists. Risk C: Monitor therapy Ketoconazole: May increase the serum concentration of Vitamin K Antagonists. Risk C: Monitor therapy Ketoconazole (Systemic): May increase the serum concentration of Vitamin K Antagonists. Risk C: Monitor therapy Lansoprazole: May increase the serum concentration of Vitamin K Antagonists. Risk C: Monitor therapy Leflunomide: May enhance the anticoagulant effect of Vitamin K Antagonists. Risk C: Monitor therapy Lopinavir: May decrease the serum concentration of Warfarin. Risk C: Monitor therapy Macrolide Antibiotics: May increase the serum concentration of Vitamin K Antagonists. Exceptions: Fidaxomicin (Systemic); Spiramycin. Risk C: Monitor therapy Mercaptopurine: May diminish the anticoagulant effect of Vitamin K Antagonists. Risk C: Monitor therapy Methylphenidate: May increase the serum concentration of Vitamin K Antagonists. Risk C: Monitor therapy MetroNIDAZOLE: May increase the serum concentration of Vitamin K Antagonists. Management: Consider alternatives to concomitant therapy with these agents. Monitor for increased INR/bleeding risk if metronidazole is initiated/dose increased, or decreased effects if metronidazole is discontinued/dose decreased. Risk D: Consider therapy modification MetroNIDAZOLE (Systemic): May decrease the metabolism of Vitamin K Antagonists. Risk D: Consider therapy modification Miconazole (Oral): May increase the serum concentration of Warfarin. Risk C: Monitor
11 de 23
02/01/12 21:28
Warfarin: Drug information
http://www.uptodate.com/contents/warfarin-drug-information...
therapy Miconazole (Topical): May increase the serum concentration of Vitamin K Antagonists. Risk D: Consider therapy modification Milnacipran: May enhance the adverse/toxic effect of Vitamin K Antagonists. Specifically, the risk for bleeding may be increased. Risk C: Monitor therapy Mirtazapine: May enhance the anticoagulant effect of Warfarin. Risk C: Monitor therapy Nafcillin: May diminish the anticoagulant effect of Vitamin K Antagonists. Risk D: Consider therapy modification Nelfinavir: May decrease the serum concentration of Warfarin. Nelfinavir may increase the serum concentration of Warfarin. Risk C: Monitor therapy Neomycin: May enhance the anticoagulant effect of Vitamin K Antagonists. Risk C: Monitor therapy NSAID (COX-2 Inhibitor): May enhance the anticoagulant effect of Vitamin K Antagonists. Risk C: Monitor therapy NSAID (Nonselective): May enhance the anticoagulant effect of Vitamin K Antagonists. Risk D: Consider therapy modification Omega-3-Acid Ethyl Esters: May enhance the anticoagulant effect of Warfarin. Risk C: Monitor therapy Omeprazole: May increase the serum concentration of Vitamin K Antagonists. Risk C: Monitor therapy Orlistat: May enhance the anticoagulant effect of Warfarin. Risk C: Monitor therapy Peginterferon Alfa-2b: May decrease the serum concentration of CYP2C9 Substrates (High risk). Risk C: Monitor therapy Pentosan Polysulfate Sodium: May enhance the anticoagulant effect of Anticoagulants. Risk C: Monitor therapy Pentoxifylline: May enhance the anticoagulant effect of Vitamin K Antagonists. Risk C: Monitor therapy Phenytoin: May enhance the anticoagulant effect of Vitamin K Antagonists. Vitamin K Antagonists may increase the serum concentration of Phenytoin. Management: Anticoagulant dose adjustment will likely be necessary when phenytoin is initiated or discontinued. Monitor patients extra closely (INR and signs/symptoms of bleeding) when using this combination. Risk D: Consider therapy modification Phytonadione: May diminish the anticoagulant effect of Vitamin K Antagonists. Risk D: Consider therapy modification Posaconazole: May increase the serum concentration of Vitamin K Antagonists. Risk C: Monitor therapy Propafenone: May increase the serum concentration of Vitamin K Antagonists. Risk C: Monitor therapy Propoxyphene: May enhance the anticoagulant effect of Vitamin K Antagonists. Risk C: Monitor therapy
12 de 23
02/01/12 21:28
Warfarin: Drug information
http://www.uptodate.com/contents/warfarin-drug-information...
Prostacyclin Analogues: May enhance the adverse/toxic effect of Anticoagulants. Specifically, the antiplatelet effects of these agents may lead to an increased risk of bleeding with the combination. Risk C: Monitor therapy QuiNIDine: May enhance the anticoagulant effect of Vitamin K Antagonists. Note that the INR/PT might be unchanged in the face of increased bleeding. Risk C: Monitor therapy QuiNINE: May enhance the anticoagulant effect of Vitamin K Antagonists. Risk C: Monitor therapy Quinolone Antibiotics: May enhance the anticoagulant effect of Vitamin K Antagonists. Risk C: Monitor therapy Ranitidine: May increase the serum concentration of Warfarin. Risk C: Monitor therapy Rifamycin Derivatives: May increase the metabolism of Vitamin K Antagonists. Risk C: Monitor therapy Ritonavir: May decrease the serum concentration of Warfarin. Risk C: Monitor therapy Rivaroxaban: Anticoagulants may enhance the anticoagulant effect of Rivaroxaban. Risk X: Avoid combination RomiDEPsin: May enhance the therapeutic effect of Warfarin. Risk C: Monitor therapy Salicylates: May enhance the anticoagulant effect of Vitamin K Antagonists. Exceptions: Salsalate. Risk D: Consider therapy modification Salicylates: May enhance the anticoagulant effect of Anticoagulants. Risk C: Monitor therapy Saquinavir: May increase the serum concentration of Warfarin. Risk C: Monitor therapy Selective Serotonin Reuptake Inhibitors: May enhance the anticoagulant effect of Vitamin K Antagonists. Risk C: Monitor therapy Sitaxentan: May increase the serum concentration of Warfarin. Risk D: Consider therapy modification SORAfenib: May enhance the anticoagulant effect of Warfarin. SORAfenib may increase the serum concentration of Warfarin. Management: Warfarin dose adjustment will likely be necessary. Increase frequency of INR monitoring during sorafenib therapy (particularly when starting or stopping therapy), and increase monitoring for signs and symptoms of bleeding. Risk D: Consider therapy modification St Johns Wort: May increase the metabolism of Vitamin K Antagonists. Risk D: Consider therapy modification Sucralfate: May diminish the anticoagulant effect of Vitamin K Antagonists. Sucralfate may decrease the serum concentration of Vitamin K Antagonists. Specifically, sucralfate may decrease the absorption of Vitamin K Antagonists. Management: Administer vitamin K antagonists at least 2 hours before or at least 6 hours after sucralfate. Risk D: Consider therapy modification Sulfinpyrazone [Off Market]: May decrease the metabolism of Vitamin K Antagonists. Sulfinpyrazone [Off Market] may decrease the protein binding of Vitamin K Antagonists. Risk D: Consider therapy modification
13 de 23
02/01/12 21:28
Warfarin: Drug information
http://www.uptodate.com/contents/warfarin-drug-information...
Sulfonamide Derivatives: May enhance the anticoagulant effect of Vitamin K Antagonists. Risk D: Consider therapy modification Tamoxifen: May increase the serum concentration of Vitamin K Antagonists. Risk X: Avoid combination Telaprevir: May decrease the serum concentration of Warfarin. Telaprevir may increase the serum concentration of Warfarin. Risk C: Monitor therapy Tetracycline Derivatives: May enhance the anticoagulant effect of Vitamin K Antagonists. Risk C: Monitor therapy Thrombolytic Agents: May enhance the anticoagulant effect of Anticoagulants. Risk C: Monitor therapy Thyroid Products: May enhance the anticoagulant effect of Vitamin K Antagonists. Risk D: Consider therapy modification Tigecycline: May increase the serum concentration of Warfarin. Risk C: Monitor therapy Tocilizumab: May decrease the serum concentration of CYP3A4 Substrates. Risk C: Monitor therapy Tolterodine: May enhance the anticoagulant effect of Warfarin. Risk C: Monitor therapy Toremifene: May enhance the anticoagulant effect of Vitamin K Antagonists. Risk C: Monitor therapy Torsemide: May increase the serum concentration of Warfarin. Risk C: Monitor therapy TraMADol: May enhance the anticoagulant effect of Vitamin K Antagonists. Risk C: Monitor therapy Tricyclic Antidepressants: May enhance the anticoagulant effect of Vitamin K Antagonists. Risk C: Monitor therapy Venlafaxine: May enhance the adverse/toxic effect of Vitamin K Antagonists. Specifically, the risk for bleeding may be increased. Risk C: Monitor therapy Vitamin E: May enhance the anticoagulant effect of Vitamin K Antagonists. Risk C: Monitor therapy Voriconazole: May increase the serum concentration of Vitamin K Antagonists. Risk C: Monitor therapy Vorinostat: May enhance the anticoagulant effect of Vitamin K Antagonists. Risk C: Monitor therapy Zafirlukast: May increase the serum concentration of Vitamin K Antagonists. Risk C: Monitor therapy Zileuton: May increase the serum concentration of Warfarin. Risk C: Monitor therapy
Ethanol/Nutrition/Herb Interactions
Ethanol: Avoid ethanol. Acute ethanol ingestion (binge drinking) decreases the metabolism of warfarin and increases PT/INR. Chronic daily ethanol use increases the metabolism of warfarin and decreases PT/INR.
14 de 23
02/01/12 21:28
Warfarin: Drug information
http://www.uptodate.com/contents/warfarin-drug-information...
Food: The anticoagulant effects of warfarin may be decreased if taken with foods rich in vitamin K. Vitamin E may increase warfarin effect. Cranberry juice may increase warfarin effect. Herb/Nutraceutical: Cranberry, fenugreek, ginkgo biloba, glucosamine, may enhance bleeding or increase warfarin's effect. Ginseng (American), coenzyme Q10, and St Johns wort may decrease warfarin levels and effects. Avoid alfalfa, anise, bilberry, bladderwrack, bromelain, cat's claw, celery, chamomile, coleus, cordyceps, dong quai, evening primrose oil, fenugreek, feverfew, garlic, ginger, ginkgo biloba, ginseng (American), ginseng (Panax), ginseng (Siberian), grapeseed, green tea, guggul, horse chestnut seed, horseradish, licorice, omega-3-acids, prickly ash, red clover, reishi, SAMe (s-adenosylmethionine), sweet clover, turmeric, and white willow (all have additional antiplatelet activity).
Pregnancy Risk Factor Pregnancy Implications
X (show table)
Warfarin crosses the placenta; concentrations in the fetal plasma are similar to maternal values. Teratogenic effects have been reported following first trimester exposure and may include coumarin embryopathy (nasal hypoplasia and/or stippled epiphyses; limb hypoplasia may also be present). Adverse events to the fetus have also been observed following second and third trimester exposure and may include CNS abnormalities (including ventral midline dysplasia, dorsal midline dysplasia). Use is contraindicated during pregnancy (or in women of reproductive potential), threatened abortion, eclampsia, or preeclampsia. Frequent pregnancy tests are recommended for women who are planning to become pregnant and adjusted dose heparin or low molecular weight heparin should be substituted as soon as pregnancy is confirmed. In pregnant women with high-risk mechanical heart valves, the benefits of warfarin therapy should be discussed with the risks of available treatments; when possible avoid warfarin use during the first trimester and close to delivery.
Lactation
pending)
Does not enter breast milk (AAP rates compatible; AAP 2001 update
Breast-Feeding Considerations
Breast-feeding women may be treated with warfarin. Based on limited data, warfarin does not pass into breast milk; however, prolonged PT may occur in some infants (product labeling). Women who are breast-feeding should be carefully monitored to avoid excessive anticoagulation. ACCP guidelines recommend continuation of warfarin in lactating women who wish to breast-feed their infants (Bates, 2008). Warfarin was not detected in breast milk in 2 reports of warfarin exposure during breast-feeding in 9 infants. Evaluation of coagulation tests and vitamin K status of breast-feeding infant is considered prudent (product labeling).
Dietary Considerations
Foods high in vitamin K (eg, beef liver, pork liver, green tea, and leafy green vegetables) inhibit anticoagulant effect. Do not change dietary habits once stabilized on warfarin therapy. A balanced diet with a consistent intake of vitamin K is essential. Avoid large amounts of alfalfa, asparagus, broccoli, Brussels sprouts, cabbage, cauliflower, green teas, kale, lettuce, spinach, turnip greens, and watercress; decreased efficacy of warfarin. It is recommended that the diet contain a CONSISTENT vitamin K content of 70-140 mcg/day. Check with healthcare provider before changing diet.
Pricing: U.S. (www.drugstore.com)
15 de 23
02/01/12 21:28
Warfarin: Drug information
http://www.uptodate.com/contents/warfarin-drug-information...
Tablets (Coumadin) 1 mg (30): $46.99 2 mg (30): $50.99 2.5 mg (30): $52.99 3 mg (30): $55.99 4 mg (30): $54.99 5 mg (30): $53.99 6 mg (30): $56.99 7.5 mg (30): $58.99 10 mg (30): $62.99 Tablets (Jantoven) 2 mg (30): $17.99 4 mg (30): $17.99 5 mg (30): $17.99 Tablets (Warfarin Sodium) 1 mg (30): $13.99 2 mg (30): $14.99 2.5 mg (30): $14.99 3 mg (30): $15.99 4 mg (30): $14.99 5 mg (30): $13.99 7.5 mg (30): $23.99 10 mg (30): $24.99
Monitoring Parameters Reference Range
Prothrombin time, hematocrit, INR; consider genotyping of CYP2C9 and VKORC1 prior to initiation of therapy, if available
INR = patient prothrombin time/mean normal prothrombin time ISI = international sensitivity index INR should be increased by 2-3.5 times depending upon indication. An INR >4 does not generally add additional therapeutic benefit and is associated with increased risk of bleeding. Note: To prevent gastrointestinal bleeding events in patients receiving the combination of warfarin, aspirin, and clopidogrel, an INR of 2-2.5 is recommended unless condition requires a higher INR target (eg, certain mechanical heart valves) (Bhatt, 2008).
16 de 23
02/01/12 21:28
Warfarin: Drug information
http://www.uptodate.com/contents/warfarin-drug-information...
Adult Target INR Ranges Based Upon Indication Targeted INR Targeted INR Range
Indication
Cardiac Acute myocardial infarction (high risk)1,2,3 Atrial fibrillation or atrial flutter Valvular Bileaflet or Medtronic Hall tilting disk mechanical aortic valve in normal sinus rhythm and normal LA size Bileaflet or tilting disk mechanical mitral valve Caged ball or caged disk mechanical valve 2.5 2.5 2-3 2-3
2.5
2-3
3 3
2.5-3.5 2.5-3.5 2.5-3.5
Mechanical prosthetic valve with systemic embolism despite adequate anticoagulation4
3 or 3.5
or 3-4
Mechanical valve and risk factors for thromboembolism (eg, AF, MI5, LA enlargement, hypercoagulable state, low EF) or history of atherosclerotic vascular disease6 Bioprosthetic mitral valve7 Bioprosthetic mitral or aortic valve with prior history of systemic embolism7 Bioprosthetic mitral or aortic valve with evidence of LA thrombus at surgery8 Bioprosthetic mitral or aortic valve with risk factors for thromboembolism (eg, AF, hypercoagulable state or low EF)
9
2.5-3.5
2.5
2-3
2.5
2-3
2.5
2-3
2.5
2-3
17 de 23
02/01/12 21:28
Warfarin: Drug information
http://www.uptodate.com/contents/warfarin-drug-information...
Indication
Targeted INR
Targeted INR Range 3.5-4.5 3-4
Prosthetic mitral valve thrombosis (resolved)3 Prosthetic aortic valve thrombosis (resolved)3 Rheumatic mitral valve disease and normal sinus rhythm (LA diameter >5.5 cm), AF, previous systemic embolism, or LA thrombus Thromboembolism Treatment Venous thromboembolism10,11 Thromboprophylaxis Chronic thromboembolic pulmonary hypertension (CTPH) Idiopathic pulmonary artery hypertension (IPAH)12 Lupus inhibitor (no other risk factors) Lupus inhibitor and recurrent thromboembolism Major trauma patients with impaired mobility undergoing rehabilitation Spinal cord injury (acute) undergoing rehabilitation Total hip or knee replacement (elective) or hip fracture surgery13 Other Indications Cerebral venous sinus thrombosis14 Ischemic stroke due to AF
1
4 3.5
2.5
2-3
2.5
2-3
2.5
2-3
2 2.5 3
1.5-2.5 2-3 2.5-3.5
2.5
2-3
2.5
2-3
2.5
2-3
2.5 2.5
2-3 2-3
High-risk includes large anterior MI, significant heart failure,
18 de 23
02/01/12 21:28
Warfarin: Drug information
http://www.uptodate.com/contents/warfarin-drug-information...
Indication
Targeted INR
Targeted INR Range
intracardiac thrombus, atrial fibrillation, history of thromboembolism.
2
Maintain anticoagulation for 3 months. Combine with aspirin 81 mg/day. Combine with aspirin 81 mg/day, if not previously receiving, and/or if previous target INR was 2.5, then new target INR should be 3 (2.5-3.5). If previous target INR was 3, then new target INR should be 3.5 (3-4). MI refers to anterior-apical ST-segment elevation myocardial infarction. Combine with aspirin 81 mg/day unless patient is at high risk of bleeding (eg, history of GI bleed, age >80 years). Maintain anticoagulation for 3 months after valve insertion then switch to aspirin 81 mg/day if no other indications for warfarin exist or clinically reassess need for warfarin in patients with prior history of systemic embolism. Maintain anticoagulation with warfarin until thrombus resolution. If patient has history of atherosclerotic vascular disease, combine with aspirin 81 mg/day unless patient is at high risk of bleeding (eg, history of GI bleed, age >80 years). Treat for 3 months in patients with VTE due to transient reversible risk factor. Treat for a minimum of 3 months in patients with unprovoked VTE and evaluate for long term therapy. Other risk groups (eg, cancer) may require >3 months of therapy. In patients with unprovoked VTE who prefer less frequent INR monitoring, low-intensity therapy (INR range: 1.5-1.9) with less frequent monitoring is recommended over stopping treatment. Recommendation from the ACCF/AHA 2009 Expert Consensus Document on Pulmonary Hypertension (McLaughlin, 2009) Continue for at least 10 days and up to 35 days after surgery.
10
11
12
13
19 de 23
02/01/12 21:28
Warfarin: Drug information
http://www.uptodate.com/contents/warfarin-drug-information...
Indication
Targeted INR
Targeted INR Range
14
Continue for up to 12 months.
Warfarin levels are not used for monitoring degree of anticoagulation. They may be useful if a patient with unexplained coagulopathy is using the drug surreptitiously or if it is unclear whether clinical resistance is due to true drug resistance or lack of drug intake. Normal prothrombin time (PT): 10.9-12.9 seconds. Healthy premature newborns have prolonged coagulation test screening results (eg, PT, aPTT, TT) which return to normal adult values at approximately 6 months of age. Healthy prematures, however, do not develop spontaneous hemorrhage or thrombotic complications because of a balance between procoagulants and inhibitors.
International Brand Names
Aldocumar (ES); Befarin (TH); Circuvit (AR); Cofarin (TW); Coumadan (AR); Coumadin (AE, AU, BF, BH, BJ, CI, CN, CY, DE, EC, EG, ET, GH, GM, GN, IL, IQ, IR, IT, JO, KE, KP, KW, LB, LR, LY, MA, ML, MR, MU, MW, MX, NE, NG, NZ, OM, PE, PH, PK, PY, QA, SA, SC, SD, SL, SN, SY, TN, TR, TZ, UG, VE, YE, ZM, ZW); Coumadine (FR); Dagonal (UY); Fargem (TH); Lawarin (CZ); Lennon-Warfarin (ZA); Mafarin (TW); Maforan (TH); Marevan (AU, BE, BR, DK, EE, FI, GB, IE, LU, NO, NZ, SG); Marfarin (HN); Marivarin (HR); Orfarin (MY, TH, TW); Panwarfin (GR); Simarc-2 (ID); Tedicumar (ES); Tufam (TH); UniWarfin (IN); Varfine (PT); Waran (SE); Warfar (CO, KP); Warfil 5 (DO); Warfin (PL); Warik (PH); Zydarin (TH); Zyfarin (PH)
Mechanism of Action
Hepatic synthesis of coagulation factors II, VII, IX, and X, as well as proteins C and S, requires the presence of vitamin K. These clotting factors are biologically activated by the addition of carboxyl groups to key glutamic acid residues within the proteins structure. In the process, active vitamin K is oxidatively converted to an inactive form, which is then subsequently reactivated by vitamin K epoxide reductase complex 1 (VKORC1). Warfarin competitively inhibits the subunit 1 of the multi-unit VKOR complex, thus depleting functional vitamin K reserves and hence reduces synthesis of active clotting factors.
Pharmacodynamics/Kinetics
Onset of action: Anticoagulation: Oral: 24-72 hours Peak effect: Full therapeutic effect: 5-7 days; INR may increase in 36-72 hours Duration: 2-5 days Absorption: Oral: Rapid, complete Distribution: 0.14 L/kg Protein binding: 99% Metabolism: Hepatic, primarily via CYP2C9; minor pathways include CYP2C8, 2C18, 2C19, 1A2, and 3A4
20 de 23
02/01/12 21:28
Warfarin: Drug information
http://www.uptodate.com/contents/warfarin-drug-information...
Genomic variants: Approximately 37% reduced clearance of S-warfarin in patients heterozygous for 2C9 (*1/*2 or *1/*3), and ~70% reduced in patients homozygous for reduced function alleles (*2/*2, *2/*3, or *3/*3) Half-life elimination: 20-60 hours; Mean: 40 hours; highly variable among individuals Time to peak, plasma: Oral: ~4 hours Excretion: Urine (92%, primarily as metabolites) Use of UpToDate is subject to the Subscription and License Agreement. REFERENCES 1. Albers GW, Amarenco P, Easton JD, et al, Antithrombotic and Thrombolytic Therapy for Ischemic
Stroke: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines (8th Edition), Chest, 2008, 133(6 Suppl):630-69. [PubMed 18574275]
2. American Academy of Pediatrics Committee on Drugs. The Transfer of Drugs and Other Chemicals
Into Human Milk, Pediatrics, 2001, 108(3):776-89. [PubMed 11533352]
3. Anand SS, Yusuf S, Pogue J, et al, Long-Term Oral Anticoagulant Therapy in Patients With Unstable
Angina or Suspected Non-Q-Wave Myocardial Infarction: Organization to Assess Strategies for Ischemic Syndromes (OASIS) Pilot Study Results, Circulation, 1998, 98(11):1064-70. [PubMed 9736592]
4. Ansell J, Hirsh J, Hylek E, et al, The Pharmacology and Management of the Vitamin K Antagonists:
American College of Chest Physicians Evidence-Based Clinical Practice Guidelines (8th Edition), Chest, 2008, 133(6 Suppl):160-98. [PubMed 18574265]
5. Antman EM, Anbe SC, Alpert JS, et al, ACC/AHA Guidelines for the Management of Patients With
ST-Elevation Myocardial Infarction - Executive Summary: A Report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Writing Committee to Revise the 1999 Guidelines for the Management of Patients With Acute Myocardial Infarction), Circulation, 2004, 110(5):588-636. [PubMed 15289388]
6. Arepally GM and Ortel TL, Heparin-Induced Thrombocytopenia, N Engl J Med, 2006, 355
(8):809-17. [PubMed 16928996]
7. Bates SM, Greer IA, Pabinger I, et al, Venous Thromboembolism, Thrombophilia, Antithrombotic
Therapy, and Pregnancy: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines (8th Edition), Chest, 2008, 133(6 Suppl):844-86. [PubMed 18574280]
8. Bhatt DL, Scheiman J, Abraham NS, et al, ACCF/ACG/AHA 2008 Expert Consensus Document on
Reducing the Gastrointestinal Risk of Antiplatelet Therapy and NSAID Use. A Report of the American College of Cardiology Foundation Task Force on Clinical Expert Consensus Documents, J Am Coll Cardiol, 2008, 52(18):1502-17. [PubMed 19017521]
9. Broderick J, Connolly S, Feldmann E, et al, "Guidelines for the Management of Spontaneous
Intracerebral Hemorrhage in Adults: 2007 Update: A Guideline From the American Heart Association/American Stroke Association Stroke Council, High Blood Pressure Research Council, and the Quality of Care and Outcomes in Research Interdisciplinary Working Group," Stroke, 2007, 38(6):2001-23. [PubMed 17478736]
10. Carabello PJ, Heit JA, Atkinson EJ, et al, Long-Term Use of Oral Anticoagulants and the Risk of
Fracture, Arch Intern Med, 1999, 159(15):1750-6. [PubMed 10448778]
11. Chimowitz MI, Lynn MJ, Howlett-Smith H, et al, "Comparison of Warfarin and Aspirin for Symptomatic
Intracranial Arterial Stenosis," N Engl J Med, 2005, 352(13):1305-16. [PubMed 15800226]
12. Dager WE and White RH, Pharmacotherapy of Heparin-Induced Thrombocytopenia, Expert Opin
Pharmacother, 2003, 4(6):919-40. [PubMed 12783589]
13. Dager WE, King JF, Regalia RC, et al, Reversal of Elevated International Normalized Ratios and
Bleeding With Low-Dose Recombinant Activated Factor VII in Patients Receiving Warfarin, Pharmacotherapy, 2006, 26(8):1091-8. [PubMed 16863486]
14. Douketis JD, Berger PB, Dunn AS, et al, The Perioperative Management of Antithrombotic Therapy:
21 de 23
02/01/12 21:28
Warfarin: Drug information
http://www.uptodate.com/contents/warfarin-drug-information...
American College of Chest Physicians Evidence-Based Clinical Practice Guidelines (8th Edition), Chest, 2008, 133(6 Suppl):299-339. [PubMed 18574269]
15. Eagle KA, Guyton RA, Davidoff R, et al, ACC/AHA 2004 Guideline Update for Coronary Artery Bypass
Graft Surgery: A Report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Committee to Update the 1999 Guidelines for Coronary Artery Bypass Graft Surgery), Circulation, 2004, 110(14):e340-437. [PubMed 15466654]
16. Effect of Long-Term Oral Anticoagulant Treatment on Mortality and Cardiovascular Morbidity After
Myocardial Infarction. Anticoagulants in the Secondary Prevention of Events in Coronary Thrombosis (ASPECT) Research Group, Lancet, 1994, 343(8896):499-503. [PubMed 7906757]
17. Furie KL, Kasner SE, Adams RJ, et al, Guidelines for the Prevention of Stroke in Patients With Stroke
or Transient Ischemic Attack: A Guideline for Healthcare Professionals from the American Heart Association/American Stroke Association, Stroke, 2011,42(1):227-76 [PubMed 20966421]
18. Fuster V, Ryden LE, Cannom DS, et al, ACC/AHA/ESC 2006 Guidelines for the Management of
Patients With Atrial Fibrillation-Executive Summary. A Report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines and the European Society of Cardiology Committee for Practice Guidelines (Writing Committee to Revise the 2001 Guidelines for the Management of Patients With Atrial Fibrillation). Developed in Collaboration With the European Heart Rhythm Association and the Heart Rhythm Society, J Am Coll Cardiol, 2006, 48(4):854-906. [PubMed 16904574 ]
19. Gage BF, Birman-Deych E, Radford MJ, et al, Risk of Osteoporotic Fracture in Elderly Patients Taking
Warfarin. Results From the National Registry of Atrial Fibrillation 2, Arch Intern Med, 2006, 166(2):241-6. [PubMed 16432096]
20. Geerts WH, Bergqvist D, Pineo GF, et al, Prevention of Venous Thromboembolism: American College
of Chest Physicians Evidence-Based Clinical Practice Guidelines (8th Edition), Chest, 2008, 133(6 Suppl):381-453. [PubMed 18574271]
21. GrandMaison A, Charest AF, and Geerts WH, Anticoagulant Use in Patients With Chronic Renal
Impairment, Am J Cardiovasc Drugs, 2005, 5(5):291-305. [PubMed 16156685]
22. Hirsh J, Guyatt G, Albers GW, et al, Executive Summary: American College of Chest Physicians
Evidence-Based Clinical Practice Guidelines (8th Edition), Chest, 2008, 133(6 Suppl):71-109. [PubMed 18574259]
23. Jaff MR, McMurtry MS, Archer SL, et al, Management of Massive and Submassive Pulmonary
Embolism, Iliofemoral Deep Vein Thrombosis, and Chronic Thromboembolic Pulmonary Hypertension: A Scientific Statement from the American Heart Association, Circulation, 2011, 123(16):1788-830. [PubMed 21422387]
24. Jamal SA, Browner WS, Bauer DC, et al, Warfarin Use and Risk for Osteoporosis in Elderly Women.
Study of Osteoporotic Fractures Research Group, Ann Intern Med, 1998, 128(10):829-32. [PubMed 9599195]
25. Kearon C, Kahn SR, Agnelli G, et al, Antithrombotic Therapy for Venous Thromboembolic Disease:
American College of Chest Physicians Evidence-Based Clinical Practice Guidelines (8th Edition), Chest, 2008, 133(6 Suppl):454-545. [PubMed 18574272]
26. Kovacs MJ, Rodger M, Anderson DR, et al, Comparison of 10-mg and 5-mg Warfarin Initiation
Nomograms Together With Low-Molecular-Weight Heparin for Outpatient Treatment of Acute Venous Thromboembolism. A Randomized, Double-Blind, Controlled Trial, Ann Intern Med, 2003, 138(9):714-9. [PubMed 12729425]
27. Lindenfeld J, Albert NM, Boehmer JP, et al, HFSA 2010 Comprehensive Heart Failure Practice
Guideline, J Card Fail, 2010, 16(6):e1-194. [PubMed 20610207]
28. McLaughlin VV, Archer SL, Badesch DB, et al, ACCF/AHA 2009 Expert Consensus Document on
Pulmonary Hypertension. A Report of the American College of Cardiology Foundation Task Force on Expert Consensus Documents and the American Heart Association, Circulation, 2009, 119(16):2250-94. [PubMed 19332472]
29. McMahan DA, Smith DM, Carey MA, et al, Risk of Major Hemorrhage for Outpatients Treated With
Warfarin, J Gen Intern Med, 1998, 13(5):311-6. [PubMed 9613886]
30. Randomised Double-Blind Trial of Fixed Low-Dose Warfarin With Aspirin After Myocardial Infarction.
Coumadin Aspirin Reinfarction Study (CARS) Investigators, Lancet, 1997, 350(9075):389-96. [PubMed 9259652]
31. Sacco RL, Adams R, Albers G, et al, Guidelines for Prevention of Stroke in Patients With Ischemic
Stroke or Transient Ischemic Attack: A Statement for Healthcare Professionals From the American
22 de 23
02/01/12 21:28
Warfarin: Drug information
http://www.uptodate.com/contents/warfarin-drug-information...
Heart Association/American Stroke Association Council on Stroke: Co-Sponsored by the Council on Cardiovascular Radiology and Intervention: The American Academy of Neurology Affirms the Value of this Guideline, Stroke, 2006, 37(2):577-617. [PubMed 16432246]
32. Salem DN, OGara PT, Madias C, et al, Valvular and Structural Heart Disease: American College of
Chest Physicians Evidence-Based Clinical Practice Guidelines (8th Edition), Chest, 2008, 133(6 Suppl):593-629. [PubMed 18574274]
33. Singer DE, Albers GW, Dalen JE, et al, Antithrombotic Therapy in Atrial Fibrillation: American College
of Chest Physicians Evidence-Based Clinical Practice Guidelines (8th Edition), Chest, 2008, 133(6 Suppl):546-92. [PubMed 18574273]
34. Smith P, Arnesen H, and Holme I, The Effect of Warfarin on Mortality and Reinfarction After
Myocardial Infarction, N Engl J Med, 1990, 323(3):147-52. [PubMed 2194126]
35. Smythe MA, Warkentin TE, Stephens JL, et al, Venous Limb Gangrene During Overlapping Therapy
With Warfarin and a Direct Thrombin Inhibitor for Immune Heparin-Induced Thrombocytopenia, Am J Hematol, 2002, 71(1):50-2. [PubMed 12221676]
36. Suvarna R, Pirmohamed M, and Henderson L, Possible Interaction Between Warfarin and Cranberry
Juice, BMJ, 2003, 327(7429):1454. [PubMed 14684645]
37. Wann SL, Curtis AB, January CT, et al, 2011 ACCF/AHA/HRS Focused Update on the Management of
Patients With Atrial Fibrillation (Updating the 2006 Guideline): A Report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines, Circulation, 2011, 123 (1):104-23. [PubMed 21173346]
2012 UpToDate, Inc. All rights reserved. | Subscription and License Agreement [ecapp0604p.utd.com-187.78.250.62-AE4CAE0D6B-6.14-178237201] Licensed to: UpToDate Individual Web - Lucas R. Diniz | Support Tag:
23 de 23
02/01/12 21:28
Você também pode gostar
- Warfarin Guide: Uses, Dosing, Interactions & MonitoringDocumento4 páginasWarfarin Guide: Uses, Dosing, Interactions & MonitoringekramAinda não há avaliações
- Case Study IDocumento2 páginasCase Study IJoAnne Saba100% (2)
- LOSARTANDocumento3 páginasLOSARTANReinell GoAinda não há avaliações
- NifedipineDocumento3 páginasNifedipineNovi YulianaAinda não há avaliações
- Zolpidem TartrateDocumento2 páginasZolpidem TartrateAndrea Huecas TriaAinda não há avaliações
- AmiodaroneDocumento2 páginasAmiodaroneanindiawAinda não há avaliações
- P 398Documento1 páginaP 398Arup Ratan PaulAinda não há avaliações
- CoversylDocumento3 páginasCoversylianecunarAinda não há avaliações
- Verapamil HCLDocumento3 páginasVerapamil HCLMae Ann Bueno CastillonAinda não há avaliações
- Darbepoetin AlfaDocumento3 páginasDarbepoetin Alfaapi-3797941Ainda não há avaliações
- Drug Study - IbuprofenDocumento3 páginasDrug Study - IbuprofenThalia UyAinda não há avaliações
- DrugStudy - CamaristaColeenMaeC (BSN III-G) (Prednisone)Documento2 páginasDrugStudy - CamaristaColeenMaeC (BSN III-G) (Prednisone)Coleen Mae CamaristaAinda não há avaliações
- Paracetamol Biogesic Analgesic AntipyreticDocumento8 páginasParacetamol Biogesic Analgesic AntipyreticGian Era100% (1)
- D50WDocumento1 páginaD50WElizalde Husband100% (1)
- COPD Drug Study: Ipratropium Bromide and Albuterol SulfateDocumento9 páginasCOPD Drug Study: Ipratropium Bromide and Albuterol SulfateShane Arroyo100% (1)
- Drug Study - AmlodipineDocumento1 páginaDrug Study - AmlodipineDanielle Marie SamblacenoAinda não há avaliações
- 005LEU11EDocumento4 páginas005LEU11ELiaWahyuniAinda não há avaliações
- Drug Study - CefradoxilDocumento13 páginasDrug Study - CefradoxilJohara G'naid0% (1)
- DS (Calcium + Vit. D)Documento6 páginasDS (Calcium + Vit. D)Mary April MendezAinda não há avaliações
- Drug Analysis: Malaise, Fatigue, Dizziness, Tremors, AtaxiaDocumento2 páginasDrug Analysis: Malaise, Fatigue, Dizziness, Tremors, AtaxiaFerdinand Sherwin MorataAinda não há avaliações
- Drug Study Emergency DrugsDocumento6 páginasDrug Study Emergency DrugsJhessa Curie PitaganAinda não há avaliações
- ValsartanDocumento3 páginasValsartanapi-3797941100% (1)
- PrednisoneDocumento3 páginasPrednisoneMaja DeraAinda não há avaliações
- Nifedipine and Prednisone Drug StudyDocumento5 páginasNifedipine and Prednisone Drug StudyAllyne GavinoAinda não há avaliações
- OB Drug StudyDocumento12 páginasOB Drug StudyCj AttoAinda não há avaliações
- Sal But AmolDocumento2 páginasSal But AmolCalimlim KimAinda não há avaliações
- Drug Analysis CefoxitinDocumento2 páginasDrug Analysis CefoxitinNika LoAinda não há avaliações
- AzithromycinDocumento3 páginasAzithromycinapi-3797941100% (2)
- MotiliumDocumento5 páginasMotiliumAkram KhanAinda não há avaliações
- DRUG NAME: Hydroxyurea: Synonym (S) : Common Trade Name (S) : ClassificationDocumento7 páginasDRUG NAME: Hydroxyurea: Synonym (S) : Common Trade Name (S) : ClassificationDewinta AbutAinda não há avaliações
- Xarelto PDFDocumento33 páginasXarelto PDFNovita Dewi LestariAinda não há avaliações
- AMARYL 1mg, 2mg, 3mg, 4mg: 1 Indications and UsageDocumento16 páginasAMARYL 1mg, 2mg, 3mg, 4mg: 1 Indications and Usageddandan_2Ainda não há avaliações
- AcyclovirDocumento20 páginasAcyclovirBrian Enrile Dorado0% (1)
- Drug StudyDocumento2 páginasDrug StudyJanina Patricia BuddleAinda não há avaliações
- Drug StudyDocumento21 páginasDrug StudyShyla Garnace JavillonarAinda não há avaliações
- Esomeprazole MagnesiumDocumento3 páginasEsomeprazole Magnesiumapi-3797941100% (1)
- Drug Study...Documento5 páginasDrug Study...Ezra Dizon ManzanoAinda não há avaliações
- FluconazoleDocumento3 páginasFluconazoleMary Kate ClarosAinda não há avaliações
- DRUG CLASSIFICATION AND ACTIONDocumento8 páginasDRUG CLASSIFICATION AND ACTIONtintinAinda não há avaliações
- The Format of This Leaflet Was Determined by The Ministry of Health and Its Content Was Checked and Approved by It On February 2016Documento10 páginasThe Format of This Leaflet Was Determined by The Ministry of Health and Its Content Was Checked and Approved by It On February 2016ddandan_2Ainda não há avaliações
- Levofloxacin: A Potent Fluoroquinolone AntibioticDocumento2 páginasLevofloxacin: A Potent Fluoroquinolone AntibioticEliza Rahardja100% (1)
- Enalapril MaleateDocumento3 páginasEnalapril MaleatelichunghkAinda não há avaliações
- Drug MetronidazoleDocumento1 páginaDrug MetronidazoleSrkocherAinda não há avaliações
- Drug Name Mechanism of Action Administration Indication Contraindication Adverse Effects Nursing ResponsibilitiesDocumento1 páginaDrug Name Mechanism of Action Administration Indication Contraindication Adverse Effects Nursing ResponsibilitiesIvan Liquiran AvenadoAinda não há avaliações
- Ertapenem (Invanz)Documento1 páginaErtapenem (Invanz)Adrianne BazoAinda não há avaliações
- AminophyllineDocumento6 páginasAminophyllineapi-3797941100% (1)
- Drug study cilostazol intermittent claudicationDocumento2 páginasDrug study cilostazol intermittent claudicationart_mutantAinda não há avaliações
- Drug StudyDocumento3 páginasDrug Studyanon_11638632Ainda não há avaliações
- Drug Study Catapres. Losartan, Nootropil Cefuroxime, ArcoxiaDocumento2 páginasDrug Study Catapres. Losartan, Nootropil Cefuroxime, Arcoxiajoy_monterubioAinda não há avaliações
- COPD Treatment Spiriva Handihaler Drug StudyDocumento1 páginaCOPD Treatment Spiriva Handihaler Drug Studylivewithoutgoals0% (1)
- Azithromycin, Cefixime, Paracetamol Drug StudyDocumento4 páginasAzithromycin, Cefixime, Paracetamol Drug StudyAzizah VillaminAinda não há avaliações
- SpironolactoneDocumento2 páginasSpironolactoneNinoska Garcia-Ortiz100% (1)
- AmloDocumento1 páginaAmloamy navajaAinda não há avaliações
- Arfarin: Arget UdienceDocumento4 páginasArfarin: Arget UdienceMano cempakaAinda não há avaliações
- Loading Doses Primary CareDocumento3 páginasLoading Doses Primary CareGalih AsaAinda não há avaliações
- Vitamin K Antagonists: American College of Pharmacology and Management of TheDocumento41 páginasVitamin K Antagonists: American College of Pharmacology and Management of TheCatalina VallejoAinda não há avaliações
- Ajovy - Fremanezumab - Drug Information - UpToDateDocumento6 páginasAjovy - Fremanezumab - Drug Information - UpToDateDiana PhamAinda não há avaliações
- Chest Guidelines - WarfarinDocumento41 páginasChest Guidelines - Warfarinkedaw100% (1)
- Summary of Product Characteristics: PosologyDocumento9 páginasSummary of Product Characteristics: Posologyddandan_2Ainda não há avaliações
- Name of The Medicinal Product: Prescribing Information Coumadin TabletsDocumento13 páginasName of The Medicinal Product: Prescribing Information Coumadin Tabletsddandan_2Ainda não há avaliações
- Seminar Paper - DrugsDocumento3 páginasSeminar Paper - Drugst.barcaAinda não há avaliações
- Essential Roles of Hospital PharmacistsDocumento92 páginasEssential Roles of Hospital PharmacistsabdrhmanAinda não há avaliações
- Lesson Plan Fonn S.1Documento10 páginasLesson Plan Fonn S.1Sandeep MeenaAinda não há avaliações
- Bioeq Rev-Oxcarbazepine TabsDocumento55 páginasBioeq Rev-Oxcarbazepine TabsJagdish ChanderAinda não há avaliações
- PSA MedsCheck GuidelinesDocumento18 páginasPSA MedsCheck GuidelinesRobbie WilliamsAinda não há avaliações
- Pharmacy & Therapeutics (P&T) Journal-February 2016Documento53 páginasPharmacy & Therapeutics (P&T) Journal-February 2016Mohamed OmerAinda não há avaliações
- Sandoseacidplanet Com Product ActavisDocumento5 páginasSandoseacidplanet Com Product ActavisSandoseacidplanetAinda não há avaliações
- Μ. Bs Eb‡Qi Bvg †Jl‡Ki Bvg Cyivzb B¤^I Eb‡Qi Lð Eb Msl¨V G~J¨ MöæcDocumento121 páginasΜ. Bs Eb‡Qi Bvg †Jl‡Ki Bvg Cyivzb B¤^I Eb‡Qi Lð Eb Msl¨V G~J¨ MöæcErshad RoufAinda não há avaliações
- Compounding (I)Documento90 páginasCompounding (I)Tantri RaraAinda não há avaliações
- Rishum 1 262421216 2Documento1 páginaRishum 1 262421216 2HellcroZAinda não há avaliações
- Forensic Pharmacy (Pakistan)Documento30 páginasForensic Pharmacy (Pakistan)areeba100% (1)
- Pharma Pass Medicin 2020Documento654 páginasPharma Pass Medicin 2020VikrantAinda não há avaliações
- Public Law 110-85 110th Congress An ActDocumento156 páginasPublic Law 110-85 110th Congress An ActJames LindonAinda não há avaliações
- List of PMPF products with validity from September 1st, 2021Documento94 páginasList of PMPF products with validity from September 1st, 2021Gabriel SilvaAinda não há avaliações
- Pharmaceutical AnalysisDocumento73 páginasPharmaceutical AnalysisChristinaAinda não há avaliações
- Working PaperDocumento24 páginasWorking PaperMaryrose Gabrentina TerreAinda não há avaliações
- Lipid Lowering AgentsDocumento2 páginasLipid Lowering Agentsapi-623203696Ainda não há avaliações
- Prescription AuditDocumento23 páginasPrescription Auditkanchan waghmareAinda não há avaliações
- 1 s2.0 S0014488621001849 MainDocumento14 páginas1 s2.0 S0014488621001849 MainGregory AssonitisAinda não há avaliações
- Malaria Prevention 1Documento3 páginasMalaria Prevention 1Anastasia Caesarani KristelAinda não há avaliações
- NFC Codes 2013cusu 0313Documento64 páginasNFC Codes 2013cusu 0313vaibhavAinda não há avaliações
- Drug Study Amoxicillin PDFDocumento4 páginasDrug Study Amoxicillin PDFMc SantosAinda não há avaliações
- BActidolDocumento2 páginasBActidolianecunar100% (3)
- Daftar Obat Alkes Trolley EmergencyDocumento15 páginasDaftar Obat Alkes Trolley EmergencyPRIHATINAinda não há avaliações
- Antihistamine On ChildrenDocumento10 páginasAntihistamine On ChildrenOpl OplAinda não há avaliações
- Philippine Pharmacists AssociationDocumento4 páginasPhilippine Pharmacists AssociationAbby LumanglasAinda não há avaliações
- Orientation To Pharmacy 2014 - Part 1Documento26 páginasOrientation To Pharmacy 2014 - Part 1Khairi Mustafa Salem100% (1)
- Amlodipine - C20H25ClN2O5 - PubChem PDFDocumento72 páginasAmlodipine - C20H25ClN2O5 - PubChem PDFDavid HCAinda não há avaliações
- Aniracetam ReviewDocumento20 páginasAniracetam ReviewCarina MirnaAinda não há avaliações
- Brad Hinton CVDocumento6 páginasBrad Hinton CVapi-486072801Ainda não há avaliações