Escolar Documentos
Profissional Documentos
Cultura Documentos
Tratamiento Con Acido Retinoico y Antraciclina LLA m3
Enviado por
addygaby910Direitos autorais
Formatos disponíveis
Compartilhar este documento
Compartilhar ou incorporar documento
Você considera este documento útil?
Este conteúdo é inapropriado?
Denunciar este documentoDireitos autorais:
Formatos disponíveis
Tratamiento Con Acido Retinoico y Antraciclina LLA m3
Enviado por
addygaby910Direitos autorais:
Formatos disponíveis
VOLUME
23
NUMBER
30
OCTOBER
20
2005
JOURNAL OF CLINICAL ONCOLOGY
O R I G I N A L
R E P O R T
Treatment With All-Trans Retinoic Acid and Anthracycline Monochemotherapy for Children With Acute Promyelocytic Leukemia: A Multicenter Study by the PETHEMA Group
Juan J. Ortega, Luis Madero, Guillermo Martn, Amparo Verdeguer, Puricacion Garca, Ricardo Parody, Jos Fuster, Antonio Molines, Andrs Novo, Guillermo Debn, Antonia Rodrguez, Eulogio Conde, Javier de la Serna, Mara J. Allegue, Francisco J. Capote, Jos D. Gonzalez, Pascual Bolufer, Marcos Gonzalez, and Miguel A. Sanz
From the Hospital Universitario Materno-Infantil Vall DHebron, Barcelona; Hospital Nino Jesus, Madrid; Hospital Universitario La Fe, Valencia; Hospital Universitario La Fe (Infantil), Valencia; Hospital La Paz (Infantil), Madrid; Hospital Universitario Virgen del Roco, Sevilla; Hospital Universitario Virgen de la Arrixaca (Pediatra), Murcia; Hospital Materno-Infantil de Las Palmas; Hospital Son Dureta, Palma de Mallorca; Hospital Juan Canalejo, La Coruna; Hospital Reina Sofa, Cordoba; Hospital Universitario Marqus de Valdecilla, Santander; Hospital 12 de Octubre, Madrid; Hospital Montecelo, Pontevedra; Hospital Universitario Puerta del Mar, Cadiz; Hospital Insular de Las Palmas; and Hospital Universitario de Salamanca, Spain. Submitted January 24, 2005; accepted June 30, 2005. Presented in part at the 45th Annual Meeting of the American Society of Hematology, San Diego, California, December 3-7, 2003. Authors disclosures of potential conicts of interest are found at the end of this article. Address reprint requests to Miguel A. Sanz, Servicio de Hematologa, Hospital Universitario La Fe, Avenida Campanar 21, 46009 Valencia, Spain; e-mail: msanz@uv.es. 2005 by American Society of Clinical Oncology 0732-183X/05/2330-7632/$20.00 DOI: 10.1200/JCO.2005.01.3359
Purpose To analyze the simultaneous combination of all-trans retinoic acid (ATRA) and anthracycline monochemotherapy for children with acute promyelocytic leukemia (APL). Patients and Methods Since November 1996, 66 children (younger than 18 years) with genetically proven APL received induction therapy with ATRA and idarubicin. Consolidation therapy consisted of three courses of anthracycline monochemotherapy. After November 1999, patients with intermediate and high risk of relapse received consolidation therapy with ATRA and slightly reinforced doses of idarubicin. Maintenance therapy consisted of ATRA and low-dose mercaptopurine and methotrexate. Results Thirty-nine girls (59%) and 27 boys (41%) were included in this study. The WBC count at presentation was more than 10 109/L in 26 patients (39%). Sixty-one children (92%) achieved complete remission (CR). Early deaths from hemorrhage and retinoic acid syndrome occurred in three patients and two patients, respectively. Toxicity was manageable during consolidation and maintenance therapy. No deaths in CR, clinical cardiomyotoxicity, or secondary malignancy occurred. Two patients had molecular persistence at the end of consolidation. Three clinical relapses and two molecular relapses were also observed. Apart from one molecular relapse, all these events occurred among children with hyperleukocytosis. The 5-year cumulative incidence of relapse was 17%, whereas disease-free and overall survival rates were 82% and 87%, respectively. Conclusion A high incidence of hyperleukocytosis in children with APL was conrmed. Besides low toxicity and a high degree of compliance, a risk-adapted therapy combining ATRA and anthracycline monochemotherapy showed an antileukemic efcacy comparable to those previously reported with other chemotherapy combinations in children. J Clin Oncol 23:7632-7640. 2005 by American Society of Clinical Oncology
INTRODUCTION
Acute promyelocytic leukemia (APL) is a rare malignant disorder affecting 4% to 11.5% of children with acute myeloblastic leukemia.1-6 APL in children is characterized by a higher
incidence of hyperleukocytosis (dened as WBC count greater than 10 109/L) than in adults,7,8 which is usually associated with an increased incidence of microgranular morphologic subtype9-11 and PML/RAR isoforms BCR212 and BCR3.7,9-11
7632
Downloaded from jco.ascopubs.org on September 6, 2011. For personal use only. No other uses without permission. Copyright 2005 American Society of Clinical Oncology. All rights reserved.
ATRA and Anthracycline Monochemotherapy for Children With APL
Outcomes for children and adults with APL have dramatically changed since the introduction of all-trans retinoic acid (ATRA) therapy. On the basis of several large multicenter trials,13-20 the current recommendations for treatment of patients with APL include ATRA and anthracycline-based chemotherapy for the induction of remission, anthracyclinebased chemotherapy for consolidation, and ATRA combined with low-dose chemotherapy for maintenance.21 However, as far as we know, only two relatively small pediatric series from the German-Austrian-Swiss group22 and the European APL group,7 as well as the largest pediatric series from the Gruppo Italiano Malattie Ematologiche Maligne dellAdulto (GIMEMA),23 have reported therapeutic results using stateof-the-art approaches. We report here the disease characteristics and therapy outcomes from 66 consecutive children (younger than 18 years) with newly diagnosed PML/RAR -positive APL, who were enrolled in two sequential studies of the PETHEMA Group (Programa de Estudio y Tratamiento de las Hemopatas Malignas).18,20 They were treated with the same strategy and chemotherapy as adult patients, except for a reduction in the ATRA dose from 45 to 25 mg/m2/d in all therapeutic phases.
PATIENTS AND METHODS Eligibility Patients aged less than 18 years with de novo APL with demonstration of the t(15;17) or PML/RAR rearrangements were included. Other eligibility criteria were (1) normal hepatic and renal functions, (2) no cardiac contraindications for anthracycline chemotherapy, and (3) Eastern Cooperative Oncology Group performance status less than 4. Informed consent from parents or legal guardians was obtained for all children. Institutional review board approval was required. Induction Therapy The induction regimen consisted of oral ATRA (25 mg/m2/ d), divided into two daily doses, which was maintained until complete remission (CR), or for a maximum of 90 days, and idarubicin (12 mg/m2/d) given as an intravenous bolus dose on days 2, 4, 6, and 8. Treatment was started as soon as a diagnosis of APL had been made by cytologic criteria.24,25 For patients in whom the diagnosis was not conrmed by genetic studies, ATRA treatment was withdrawn and alternative chemotherapy was given at the physicians discretion. Consolidation Therapy Between November 1996 and October 1999 (LPA96 study), all patients in CR received three monthly consolidation courses. The rst course consisted of idarubicin (5 mg/m2/d on days 1 to 4), the second of mitoxantrone (10 mg/m2/d on days 1 to 5), and the third of idarubicin (12 mg/m2 on day 1). From November 1999 (LPA99 study), intermediate- and high-risk patients (see Denitions and Study End Points) received ATRA (25 mg/m2/d for 15 days) combined with reinforced singleagent chemotherapy courses.20 To reinforce chemotherapy of
www.jco.org
consolidation, the idarubicin dose in the rst course was increased to 7 mg/m2/d, and idarubicin was administered for two consecutive days instead of one day in the third course. Maintenance Therapy After completion of consolidation, patients who tested negative for PML/RAR (see Laboratory Studies) were started on oral mercaptopurine (50 mg/m2/d), intramuscular methotrexate (15 mg/m2 per week) and oral ATRA (25 mg/m2/d) for 15 days every 3 months. Doses of mercaptopurine and methotrexate were decreased by 50% if the WBC count was less than 3.5 109/L and discontinued if it was less than 2.5 109/L. Maintenance therapy was continued for 2 years. Maintenance therapy was also temporarily reduced or discontinued at the physicians discretion in case of abnormal liver function tests ( 3 the upper limit of normal values). CNS prophylaxis was not given in these studies. Supportive Therapy Coagulopathy, loosely dened by hypobrinogenemia, increased brinogen-brin degradation products, elevated levels of D-dimer, and prolonged prothrombin and thrombin times, was treated with fresh frozen plasma or brinogen. Platelet transfusions were given to maintain a platelet count above 30 109/L until resolution of any signicant sign of coagulopathy. Once the coagulopathy was under control, platelet transfusions were given when the platelet count dropped below 20 109/L or more liberally for patients with infectious or hemorrhagic manifestations. In the LPA99 study, tranexamic acid (100 mg/kg/d) was administered by continuous intravenous infusion until the platelet count was higher than 50 109/L. As prophylaxis for retinoic acid syndrome (RAS), patients in the LPA99 study received prednisone (0.5 mg/kg/d) on days 1 through 15. At the rst signs of suspected RAS, ATRA was temporarily discontinued and patients were given 10 mg of dexamethasone every 12 hours. Laboratory Studies Bone marrow samples were obtained at diagnosis, after induction, after the last cycle of consolidation, and periodically during maintenance and beyond, as reported elsewhere.18 In addition to morphologic evaluation, samples were processed for RNA extraction and reverse transcriptasepolymerase chain reaction (RTPCR) for detecting PML/RAR . RTPCR tests were carried out by 14 different laboratories involved in an external quality control program, which included inter-laboratory exchange of samples, as reported.26,27 If a PCR-positive or doubtful result was reported after consolidation or beyond, a new bone marrow sample was obtained 2 to 4 weeks later and sent to one of two of the reference laboratories. Denitions and Study End Points Response criteria were dened according to the recently revised criteria by Cheson et al.28 According to Frankel et al,29 RAS was dened as denitely present, indeterminate, or denitely absent. Risk of relapse was established at diagnosis according to a predictive model on the basis of patient leukocyte and platelet counts at diagnosis, as reported.30 Low-risk patients had a WBC count equal to or less than 10 109/L and a platelet count more than 40 109/L; intermediate-risk patients had a WBC 10 109/L and a platelet count 40 109/L; and high-risk patients had a WBC count greater than 10 109/L. Statistical Analyses Rates of CR were evaluated using contingency tables. Unadjusted time-to-event analyses were performed using the KaplanMeier method31 and, for comparisons, the log-rank tests.32 The
7633
Downloaded from jco.ascopubs.org on September 6, 2011. For personal use only. No other uses without permission. Copyright 2005 American Society of Clinical Oncology. All rights reserved.
Ortega et al
probability of relapse was also estimated by the cumulative incidence method (marginal probability).33,34 For all estimates in which the event relapse was considered as an end point, hematologic and molecular relapses, as well as molecular persistence, were each considered as uncensored events. The follow-up of the patients was updated on June 30, 2004. All P values reported are two-sided. Multivariate analysis was performed using the Cox proportional hazards model.35 Except for the cumulative incidence method, computations were performed using the 4F, 1L, and 2L programs from the BMDP statistical library (BMDP Statistical Software, Los Angeles, CA).
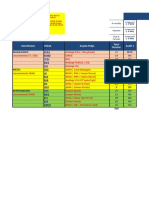
Table 1. Characteristics of Children With APL and Results of Induction Characteristic Overall Age, years 3 4-10 10 Sex Male Female WBC, 109/L 10 10 Hemoglobin, g/dL 10 10 Platelets, 109/L 40 40 FAB subtype Typical Variant Cytogenetics (n 39) t(15;17) t(15;17) other PML/RAR isoform (n BCR1/BCR2 BCR3 Relapse-risk group Low Intermediate High Median Range No. 66 12 2-17 6 20 40 27 39 4.9 0.7-235 40 26 8.5 4.8-12.9 51 15 17 4-143 54 12 54 12 29 10 56) 32 24 7 33 26 57 43 11 50 39 29 22 7 30 24 91 92 100 91 92 82 18 82 18 74 26 50 11 51 10 27 9 93 92 93 86 93 90 67 23 48 13 94 87 61 39 37 24 93 92 9 30 61 41 59 5 18 38 25 36 83 90 95 93 92 % CR 61 % 92
RESULTS
Accrual and Patient Characteristics Between November 1996 and June 2004, 639 consecutive patients with newly diagnosed APL from Spain, the Netherlands, Belgium, Argentina, and the Czech Republic, were included in the PETHEMA LPA96 and LPA99 studies. Sixtyseven of the patients (10.5%) from 35 institutions (see Appendix) were aged less than 18 years. One patient was ineligible for the study because of secondary APL. The main clinical and biologic characteristics of the remaining 66 patients assessable for induction in this series are shown in Table 1. Induction Therapy Of these 66 patients, 61 achieved hematologic CR (92%; 95% CI, 85% to 98%). The remaining ve children died early because of hemorrhage (two pulmonary, one cerebral) and RAS (two children). The low number and variety of causes of failures prevented us from analyzing the prognostic impact of the characteristics at presentation and of prophylactic measures (prednisone and tranexamic acid) in the response rate. Age distribution, response to induction therapy, and causes of failure are shown in Figure 1. RAS was denitely present in three patients (4.5%), two of whom died from it (aged 3 and 6 years). An indeterminate RAS was reported in 10 children (15%). Despite prednisone prophylaxis, the incidence of indeterminate and denitely present retinoic acid syndrome in the LPA99 study was not statistically different to that observed in the LPA96 trial (17% v 28%; P .3). The ATRA therapy was temporarily discontinued in nine children (14%) because of presumed RAS. Therapy recommenced within a median time of 3 days (range, 3 to 12 days). In one additional boy, ATRA was denitively discontinued after 3 days of treatment. The median time of ATRA administration was 35 days (range, 20 to 51 days). Headaches and pseudotumor cerebri were observed in 20 children (30%) and four children (6%), respectively. All these side effects were transient, reversible, and never a cause of death. The ATRA therapy was permanently discontinued on days 21 and 23 in two of the four patients with pseudotumor cerebri. In the remaining two children,
7634
NOTE. There were no signicant differences between the groups. Abbreviations: APL, acute promyelocytic leukemia; CR, complete remission; FAB, French-American-British.
ATRA therapy was temporarily discontinued and resumed without dose reduction after 3 days and 7 days. The median time to attain 1 109 neutrophils/L and the incidence of other signicant nonhematologic toxicities are listed in Table 2. The most prevalent microorganism
Fig 1. Age distribution of the 66 children with acute promyelocytic leukemia, response to induction therapy, and causes of failure. CR, complete remission; RA, retinoic acid.
JOURNAL OF CLINICAL ONCOLOGY
Downloaded from jco.ascopubs.org on September 6, 2011. For personal use only. No other uses without permission. Copyright 2005 American Society of Clinical Oncology. All rights reserved.
ATRA and Anthracycline Monochemotherapy for Children With APL
Table 2. Toxic Effects During Induction and Consolidation Therapy Consolidation Induction No. children with neutropenia/No. Total Days to neutrophils 1 109/L Median Range Fever Clinically documented infection Microbiologically documented infection without bacteremia Microbiologically documented infection with bacteremia Not documented infection Nonhematologic toxicity, grades 3 and 4 (WHO) Hepatic Pulmonary Renal Cardiac Neurologic Dermatologic Diarrhea Oral Both toxicities occurred in the same children in a context of septic shock. 66/66 19 8-39 58 13 7 14 24 2 4 1 4 1 1 3 4 Course 1 31/61 23 1-35 17 4 2 4 7 0 0 0 0 0 0 0 1 Course 2 45/61 24 7-42 39 7 4 7 21 0 1 0 1 0 0 1 4 Course 3 31/60 25 4-55 15 2 3 2 8 0 0 0 0 0 0 0 0
isolated among microbiologically documented infections was coagulase-negative Staphylococcus. No fungal infections were documented. As to cardiac toxicity, three children developed tachycardia, hypotension, and hemodynamic instability, requiring inotropic drugs, two in a context of sepsis and one during severe RAS. Both patients with sepsis had favorable response to treatment and complete resolution of acute cardiotoxicity, while the other child died of RAS with normal echocardiographic evaluation. The fourth child, who had a transient severe bradycardia caused by marked hypokalemia, died of cerebral hemorrhage on day 3. There were no cases of idarubicin induced cardiomyopathy recognized. Consolidation Therapy All patients who achieved CR proceeded to consolidation therapy and all of them, except for one 14-year-old girl who became pregnant after the second consolidation course, received the three consolidation courses as scheduled. Hematologic toxicity was higher during the second course of consolidation. Febrile neutropenia occurred in 17 children and 15 children during the rst and the third course of chemotherapy, respectively; whereas, 39 episodes of febrile neutropenia were observed during the second course. No deaths occurred during consolidation therapy. The median time to attain 1 109 neutrophils/L and the incidence of other signicant nonhematologic toxicities observed in each consolidation course are listed in Table 2. Tests for PML/RAR using RTPCR were carried out on 46 children (75%) at the end of consolidation therapy. The two patients with molecular persistence at this point were among the 20 high-risk patients.
www.jco.org
Maintenance Therapy All patients proceeded to maintenance therapy. Cytopenias, especially neutropenia, and slight abnormalities in liver function tests were commonly observed in this phase, often requiring dose reduction of 6-mercaptopurine (25 children) or temporary discontinuation (4 children) of chemotherapy. No refusals to injections of methotrexate were reported during maintenance therapy. No deaths in remission occurred during maintenance therapy. Outcomes In addition to two children with molecular persistence at the end of consolidation, three children had clinical relapses at 5 months, 32 months, and 48 months, and two had molecular relapses at 12 months and 16 months from the achievement of CR. The remaining patients are in continuous CR from 4 months to 89 months (median, 38 months). All clinical relapses occurred in high-risk patients and two relapses were in the CNS. Because of the small number of children with low risk of relapse (n 7), they were analyzed together with the intermediate risk group (ie, patients with WBC counts less than 10 109/L were compared with those with more than 10 109/L). The characteristics and outcomes of patients who had molecular persistence and molecular or clinical relapses are shown in Table 3. Among the 15 patients who were not tested by RT-PCR at the end of consolidation therapy, one high-risk patient from the LPA96 trial relapsed at 4 months. Cumulative Incidence of Relapse With a median follow-up of 39 months (range, 6 months to 90 months) for all surviving patients, the 5-year cumulative incidence of relapse (CIR) was 17% (Fig 2A),
7635
Downloaded from jco.ascopubs.org on September 6, 2011. For personal use only. No other uses without permission. Copyright 2005 American Society of Clinical Oncology. All rights reserved.
Ortega et al
Table 3. Characteristics and Follow-Up of Children With Molecular Persistence, Molecular Relapse, or Clinical Relapse Type of Event Molecular persistence LPA96 LPA99 Molecular relapse LPA99 LPA99 Clinical relapse LPA96 LPA96 LPA99 16 6 13 Male Female Male 26.7 13.6 20.5 23 8 72 High High High Bone marrow AIDA HD/Ara-C and CNS CNS MTZ HD/Ara-C IT CHT Bone marrow MTZ HD/Ara-C 3 PBSCT Death (d3 of CHT) CR, alive and well CR, alive and well 17 16 Female Male 0.7 39.2 44 17 Low High Bone marrow MTZ HD/Ara-C 3 PBSCT Bone marrow ATRA 3 Allo SCT Death (d 7 post-SCT) CR, alive and well 2 8 Male Male 11 115 12 57 High High Bone marrow MTZ HD/Ara-C 3 UCBT 3 CR3 Relapse Bone marrow MTZ HD/Ara-C 3 PBSCT 3 Relapse 3 AlloSCT Death CR, alive and well Study Age, Years Sex WBC ( 109/L) Platelets ( 109/L) Risk Group Site of Relapse Subsequent Treatments Current Status
Abbreviations: MTZ, mitoxantrone; HD/Ara-C, high-dose Ara-C; UCBT, umbilical cord blood transplantation; CR, complete remission; PBSCT, peripheral blood stem-cell transplantation; AlloSCT, allogeneic stem-cell transplantation; SCT, stem-cell transplantation; CHT, chemotherapy. CNS hemorrhage at presentation. Not tested for molecular status at the end of consolidation.
being 25% and 11% for patients in the LPA96 and LPA99 studies, respectively (P .3). The CIR rate for low- and intermediate-risk groups when analyzed together was 3.5%, whereas for the high-risk group it was 31% (P .01; Fig 2B). Disease-Free and Overall Survival The 5-year estimate of disease-free survival (DFS) was 82% 14% (Fig 3). For children in the LPA96 study,
the DFS was 75% 25%, whereas in the LPA99 study, it was 89% 12% (P .3). The DFS rates for lowand intermediate-risk groups together and for the highrisk group were 96% 7% and 68% 24%, respectively (P .01). The probability of remaining alive after 5 years was 87% 9% (Fig 4). For children in the LPA96 study, the overall survival was 71% 24%, whereas in the LPA99 study, it was 91% 8% (P .06). The overall survival rates for low- and intermediate-risk groups together and for the high-risk group were 88% 12% and 83% 12%, respectively (P .6).
DISCUSSION
This study conrms a high incidence of hyperleukocytosis at presentation in children with APL. A risk-adapted strategy based on the combination of a reduced dose of ATRA (25 mg/m2/d) with anthracycline monochemotherapy for
Fig 2. Cumulative incidence of relapse from the time of complete remission among all 61 children (A) and according to presenting WBC counts (B).
Fig 3. Kaplan-Meier product-limit estimate of disease-free survival.
7636
JOURNAL OF CLINICAL ONCOLOGY
Downloaded from jco.ascopubs.org on September 6, 2011. For personal use only. No other uses without permission. Copyright 2005 American Society of Clinical Oncology. All rights reserved.
ATRA and Anthracycline Monochemotherapy for Children With APL
Fig 4. Kaplan-Meier product-limit estimate of overall survival.
induction and consolidation, followed by ATRA and lowdose methotrexate and mercaptopurine for maintenance therapy, produced high antileukemic efcacy, moderate toxicity, and a high degree of compliance. Information about therapeutic results with state-ofthe-art treatments in children with APL (ie, with combinations of ATRA and anthracycline-based chemotherapy) is still scarce. To our knowledge, only three series, of 22, 31, and 110 children from the German-Austrian-Swiss,22 European APL,7 and GIMEMA groups, respectively, have reported therapeutic results using such approaches. The main characteristics and therapeutic results of those studies and of the present one are summarized in Table 4. It should be noted that the three largest studies show a relatively high proportion of children with hyperleukocytosis at presentation, ranging from 35% to 48%. This is clearly higher than in adults, in whom it is usually around 20% to 25%. However, other characteristics that have been reported with increased incidence in children, such as the microgranular M3 variant9 11 and the PML/RAR isoforms BCR3,7,9 11 were found not to be consistently increased in the GIMEMA and PETHEMA studies, when compared with adults. In fact, the incidences of 18% and 43% of microgranular M3 variant and of the BCR3 isoform, respectively, in the present pediatric series do not differ from the 19% and 44% previously reported for the whole series of patients included in both LPA96 and LPA99 studies of the PETHEMA group.20 The predominance of girls in the series of children reported by de Bottom et al.7 was also seen in our study, but not in the largest one reported by the GIMEMA group. In our opinion, this nding should be interpreted cautiously because we have found an erratic distribution of male and female patients in the two studies carried out by the PETHEMA group, with a signicantly higher proportion of women in the LPA99 study than in the LPA96.20 It should be noted that the median age ranged widely, from a low of 7.2 years in the German-Austrian-Swiss study22 to a high of 15 years in the European APL study.7 Regardwww.jco.org
ing the low incidence of additional chromosomal abnormalities reported in other small pediatric series,2,7 this nding was not conrmed here, in which the proportion of children with additional chromosomal abnormalities did not differ from that reported in the PETHEMA studies for adult patients.36 All patients in our study, as in the GIMEMA study, were genetically proven APL, unlike the German-Austrian-Swiss and the European APL studies, in which genetic diagnosis was not conrmed in 14% of patients and 10% of patients, respectively. Most pediatric series treated with the simultaneous combination of ATRA and anthracycline-containing chemotherapy have consistently reported remission rates above 90% (ranging from 92% to 97%), and all of them conrm the virtual absence of leukemia resistance using state-of-the-art treatments. Sample sizes, eligibility criteria, and some aforementioned differences in characteristics with potential impact on responses to therapy canat least partially explain these apparently different results, which in fact are not statistically signicant. The apparently lower incidence of pseudotumor cerebri and headache, together with the excellent therapy results obtained with ATRA at 25 mg/m2/d, when compared with the administration of ATRA at 45 mg/m2/d, suggest that 25 mg/m2 could be the recommended dose, at least for children. Nevertheless, this issue should be denitively settled in a randomized study. The variability in the reported incidence of ATRA syndrome, ranging from 7.5% in the GIMEMA study to 20% in our study, is probably because of the denition criteria used. In fact, if only denitely present RAS is considered, GIMEMA and PETHEMA studies, both using the same AIDA regimen for induction therapy, reported a similar low rate of RAS. It is noteworthy that this severe complication and pulmonary or CNS hemorrhages were the only causes of death during induction therapy in the present series. The comparison of postremission outcomes shows no clear differences between the four series. It is important to highlight that no deaths in remission, severe clinical cardiomyopathy, or secondary malignancies were reported in these series, except for two children who developed therapy-related myelodysplasia in the GIMEMA-AIEOP study.23 As in the Italian study, the functional evaluation of late asymptomatic cardiomyopathy is ongoing. On the other hand, a possible association has been suggested between the use of ATRA and an increased incidence of CNS involvement. However, the low CNS relapse rate observed in the present series does not support this hypothesis. This is in line with a large study of the GIMEMA comparing the incidence of CNS relapse in patients treated with or without ATRA that failed to demonstrate this correlation.37
7637
Downloaded from jco.ascopubs.org on September 6, 2011. For personal use only. No other uses without permission. Copyright 2005 American Society of Clinical Oncology. All rights reserved.
Ortega et al
Table 4. Four Series of Children With Newly Diagnosed APL Treated With Combinations of ATRA and Anthracycline-Based Chemotherapy Characteristic Author Year Group No. of children/patients registered % Study period Genetic diagnosis, % Male sex, % Median age, years 3 3-10 11-17 Median WBC 109/L WBC 10 109/L, % Median platelet 109/L Microgranular variant, % Cytogenetics, % t(15;17) t(15;17) other PML/RAR isoform, % BCR1/BCR2 BCR3 ATRA dose, mg/m2/d Median time of ATRA, days Cumulative dose of anthracycline, mg/m2 CR rate, % ATRA toxicity, % RAS Denitely present Indeterminate Pseudotumor cerebri Headache Postremission outcome Median follow-up, months Molecular persistence, % Deaths in CR 5-year EFS, % 95% CI 5-year OS, % 95% CI 5-year DFS, % 95% CI 5-year CIR, % 95% CI Time from diagnosis to relapse, months Late side effects Secondary malignancy Myocardiotoxicity Mann et al22 2001 German-Austrian-Swiss 22/NA Since 1994 86 50 7.2 13 41 45 5.3 23 21.5 13 NA NA NA NA 25 NA DNR 60, IDR 24, ADR 120 95 14 Study Data De Botton et al7 2004 European APL 31/576 5% Apr. 93/Oct. 98 90 29 15 16 6.5 77.5 6.5 48 22 32 79 11 62.5 37.5 45 NA DNR 495 97 13 Testi et al23 2005 GIMEMA 124/983 13% Jan. 93/Jun. 00 100 50 11.6 NA NA NA 3.95 34.5 20 11 NA NA 62 37 25 NA IDR 80, MTZ 50 96 7.5 2 6 9 13 79 3 0 76 65 to 85 89 83 to 95 78 68 to 88 NA Ortega et al Present study PETHEMA 66/639 10% Nov. 96/Jul. 04 100 41 12 11 30 59 4.9 39 17 18 74 26 57 43 25 35 IDR 80/100, MTZ 50 92 20 3 10 6 30 39 3 0 77 63 to 91 87 79 to 96 82 68 to 96 17 5-48
5 27 34 NA 0 76 87 NA NA 14-30
16 39 67 NA 0 71 62 to 80 90 80 to 100
27 9 to 45 4-36
No No
No No
2 No
No No
Abbreviations: APL, acute promyelocytic leukemia; ATRA, all-trans retinoic acid; GIMEMA, Gruppo Italiano Malattie Ematologiche Maligne dellAdulto group; PETHEMA, Programa de Estudio y Tratamiento de las Hemopatas Malignas group; NA, not available; DNR, daunorubicin; IDR, idarubicin; ADR, Adriamycin; MTZ, mitoxantrone; CR, complete remission; RAS, retinoic acid syndrome; EFS, event-free survival; OS, overall survival; DFS, disease-free survival; CIR, cumulative incidence of relapse. Eight children did not receive simultaneous ATRA plus chemotherapy for induction therapy because they were assigned to ATRA3 chemotherapy in a randomized study. Seven children received 45 mg. At the end of consolidation. Two children developed therapy-related myelodysplasia.
7638
JOURNAL OF CLINICAL ONCOLOGY
Downloaded from jco.ascopubs.org on September 6, 2011. For personal use only. No other uses without permission. Copyright 2005 American Society of Clinical Oncology. All rights reserved.
ATRA and Anthracycline Monochemotherapy for Children With APL
The 3.5% CIR at 5 years among patients with WBC counts of less than 10 109/L (ie, children in the low- and intermediate-risk groups, together accounting for twothirds of all patients) suggest that there is probably room for reducing chemotherapy in the future for this setting. Riskadapted strategies focusing on children with WBC counts greater than 10 109/L at presentation are warranted, and this high-risk group of children with APL should, therefore, be the major subject of future clinical trials.
Acknowledgment We thank Luis Benlloch for data collection and management. Appendix The Appendix is included in the full-text version of this article, available online at www.JCO.org. It is not included in the PDF (via Adobe Acrobat Reader) version. Authors Disclosures of Potential Conicts of Interest The authors indicated no potential conicts of interest.
21. Tallman MS, Nabhan CH, Feusner JH, et al: Acute promyelocytic leukemia: Evolving therapeutic strategies. Blood 99:759-767, 2002 22. Mann G, Reinhardt D, Ritter J, et al: Treatment with all-trans retinoic acid in acute promyelocytic leukemia reduces early deaths in children. Ann Hematol 80:417-422, 2001 23. Testi AM, Biondi A, Lo-Coco F, et al: GIMEMA-AIEOP AIDA protocol for the treatment of newly diagnosed acute promyelocytic leukemia (APL) in children. Blood 106:447-453, 2005 24. Bennett JM, Catovsky D, Daniel MT, et al: Proposals for the classication of the acute leukemias. Br J Haematol 33:451-461, 1976 25. Bennett JM, Catovsky D, Daniel MT, et al: A variant form of hypergranular promyelocytic leukemia (M3). Ann Intern Med 92:280-288, 1980 26. Bolufer P, Barragan E, Sanz MA, et al: Preliminary experience in external quality control of RT-PCR PML/RAR detection in promyelocytic leukemia. Leukemia 12:2024-2028, 1998 27. Bolufer P, Lo Coco F, Grimwade D, et al: Variability in the levels of PML-RAR fusion transcripts detected by laboratories participating in an external quality control program using several reverse transcription polymerase chain reaction protocols. Haematologica 86:570-576, 2001 28. Cheson BD, Bennett JM, Kopecky K, et al: Revised recommendations of the International Working Group for Diagnosis, Standardization of Response Criteria, Treatment Outcomes, and Reporting Standards for Therapeutic Trials in Acute Myeloid Leukemia. J Clin Oncol 21:46424649, 2003 29. Frankel SR, Eardley A, Heller G, et al: All-trans retinoic acid for acute promyelocytic leukemia. Results of the New York Study. Ann Intern Med 120:278-286, 1994 30. Sanz MA, Lo Coco F, Martn G, et al: Denition of relapse risk and role of nonanthracycline drugs for consolidation in patients with acute promyelocytic leukemia: A joint study of the PETHEMA and GIMEMA cooperative groups. Blood 96:1247-1253, 2000 31. Kaplan EL, Meier P: Nonparametric estimations from incomplete observations. J Am Stat Assoc 53:457-481, 1958 32. Mantel N: Evaluation of survival data and two new rank order statistics arising in its consideration. Cancer Chemother Rep 50:163-170, 1966
REFERENCES
1. Creutzig U, Zimmermann M, Ritter J, et al: Denition of a standard-risk group in children with AML. Br J Haematol 104:630-639, 1999 2. Raimondi S, Chang MN, Ravindranath Y, et al: Chromosomal abnormalities in 478 children with acute myeloid leukemia: Clinical characteristics and treatment outcome in a Cooperative Pediatric Oncology Group Study-POG8821. Blood 94:3707-3716, 1999 3. OBrien TA, Rissell SJ, Vowels MR, et al: Results of consecutive trials for children with acute myeloid leukemia from the Australian and New Zealand Childrens Cancer Study Group. Blood 100:2708-2716, 2002 4. Perel Y, Auvrignon A, Leblanc T, et al: Impact of addition of maintenance therapy to intensive induction acute myeloblastic chemotherapy for childhood acute myeloblastic leukemia: Results of a prospective randomized trial, LAME 89/91. J Clin Oncol 20:2774-2782, 2002 5. Stevens RF, Hann JM, Wheatly K, et al: Marked improvements in outcome with chemotherapy alone in pediatric acute myeloid leukemia: Results of the United Kingdom Medical Research Councils 10th AML trial. Br J Haematol 101:130-140, 1998 6. Woods WG, Kobrinsky N, Buckley JD, et al: Timed-sequential induction therapy improves post-remission outcome in acute myeloid leukemia: A report from the Childrens Cancer Group. Blood 87:4979-4989, 1996 7. de Botton S, Coiteux V, Chevret S, et al: Outcome of childhood acute promyelocytic leukemia with all-trans-retinoic acid and chemotherapy. J Clin Oncol 22:1404-1412, 2004 8. Sanz MA, Vellenga E, Rayon C: All-trans retinoic acid and anthracycline monochemotherapy for the treatment of elderly patients with acute promyelocytic leukemia. Blood 104:34903493, 2004 9. Guglielmi C, Martelli MP, Diviero D, et al: Immunophenotype of adult and childhood acute promyelocytic leukemia: Correlation with morphology, type of PML gene breakpoint and clinical outcomeA cooperative Italian study on 196 cases. Br J Haematol 102:1035-1041, 1998 10. Rovelli A, Biondi A, Cantu-Rajnoldi A, et al: Microgranular variant of acute promyelocytic leukemia in children. J Clin Oncol 10:1413-1418, 1992
11. Biondi A, Rovelli A, Cantu-Rajnoldi A, et al: Acute promyelocytic leukemia in children: Experience of the Italian Pediatric Hematology and Oncology Group (AIEOP). Leukemia 8:12641268, 1994 12. Kane JR, Head DR, Balazs L, et al: Molecular analysis of the PML/RAR alpha chimeric gene in pediatric acute promyelocytic leukemia. Leukemia 10:1296-1302, 1996 13. Mandelli F, Diverio D, Avvisati G, et al: Molecular remission in PML/RAR -positive acute promyelocytic leukemia by combined alltrans retinoic acid and idarubicin (AIDA) therapy. Blood 90:1014-1021, 1997 14. Tallman MS, Andersen JW, Schiffer CA, et al: All-trans retinoic acid in acute promyelocytic leukemia. N Engl J Med 337:1021-1028, 1997 15. Asou N, Adachi K, Tamura J, et al: Analysis of prognostic factors in newly diagnosed acute promyelocytic leukemia treated with all-trans retinoic acid and chemotherapy. J Clin Oncol 16:78-85, 1998 16. Burnett AK, Grimwade D, Solomon E, et al: On behalf of the MRC Adult Leukemia Working Party: Presenting white blood cell count and kinetics of molecular remission predict prognosis in acute promyelocytic leukemia treated with all-trans retinoic acid: Result of the randomized MRC trial. Blood 93:4131-4143, 1999 17. Fenaux P, Chastang C, Sanz MA, et al: A randomized comparison of ATRA followed by chemotherapy and ATRA plus chemotherapy, and the role of maintenance therapy in newly diagnosed acute promyelocytic leukemia. Blood 94:1192-1200, 1999 18. Sanz MA, Martn G, Rayon C, et al: A modied AIDA protocol with anthracycline-based consolidation results in high antileukemic efcacy and reduced toxicity in newly diagnosed PML/RAR -positive acute promyelocytic leukemia. PETHEMA Group. Blood 94:30153021, 1999 19. Lengfelder E, Reichert A, Schoch C, et al: Double induction strategy including high dose cytarabine in combination with all-trans retinoic acid: Effects in patients with newly diagnosed acute promyelocytic leukemia. German AML Cooperative Group. Leukemia 14:13621370, 2000 20. Sanz MA, Martn G, Gonzalez M, et al: Risk-adapted treatment of acute promyelocytic leukemia with all-trans retinoic acid and anthracycline monochemotherapy: A multicenter study by the PETHEMA Group. Blood 103:1237-1243, 2004
www.jco.org
7639
Downloaded from jco.ascopubs.org on September 6, 2011. For personal use only. No other uses without permission. Copyright 2005 American Society of Clinical Oncology. All rights reserved.
Ortega et al
33. Gray RJ: A class of K-sample test for comparing the cumulative incidence of a competing risk. Ann Stat 16:1141-1154, 1988 34. Pepe MS, Mori M: Kaplan-Meier, marginal or conditional probability curves in summarizing competing risks failure time data? Stat Med 12:737-751, 1993
35. Cox DR: Regression models and life tables (with discussion). J R Stat Soc B 34:187-220, 1972 36. Cervera J, Martin G, Hernandez JM, et al: Additional chromosome abnormalities have no prognostic value in acute promyelocytic leukemia patients treated with simultaneous ATRA and anthracycline-based chemotherapy: An up-
date of the APL96 and APL99 PETHEMA. Blood 104(suppl 1):557 (abstr 2019) 37. Specchia G, Lo Coco F, Vignetti M, et al: Extramedullary involvement at relapse in acute promyelocytic leukemia patients treated or not with ATRA. A report by the GIMEMA Group. J Clin Oncol 19:4023-4028, 2001
7640
JOURNAL OF CLINICAL ONCOLOGY
Downloaded from jco.ascopubs.org on September 6, 2011. For personal use only. No other uses without permission. Copyright 2005 American Society of Clinical Oncology. All rights reserved.
Você também pode gostar
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeNo EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeNota: 4 de 5 estrelas4/5 (5794)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreNo EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreNota: 4 de 5 estrelas4/5 (1090)
- Never Split the Difference: Negotiating As If Your Life Depended On ItNo EverandNever Split the Difference: Negotiating As If Your Life Depended On ItNota: 4.5 de 5 estrelas4.5/5 (838)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceNo EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceNota: 4 de 5 estrelas4/5 (895)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersNo EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersNota: 4.5 de 5 estrelas4.5/5 (345)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureNo EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureNota: 4.5 de 5 estrelas4.5/5 (474)
- The Emperor of All Maladies: A Biography of CancerNo EverandThe Emperor of All Maladies: A Biography of CancerNota: 4.5 de 5 estrelas4.5/5 (271)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)No EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Nota: 4.5 de 5 estrelas4.5/5 (121)
- The Little Book of Hygge: Danish Secrets to Happy LivingNo EverandThe Little Book of Hygge: Danish Secrets to Happy LivingNota: 3.5 de 5 estrelas3.5/5 (400)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyNo EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyNota: 3.5 de 5 estrelas3.5/5 (2259)
- The Yellow House: A Memoir (2019 National Book Award Winner)No EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Nota: 4 de 5 estrelas4/5 (98)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaNo EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaNota: 4.5 de 5 estrelas4.5/5 (266)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryNo EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryNota: 3.5 de 5 estrelas3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnNo EverandTeam of Rivals: The Political Genius of Abraham LincolnNota: 4.5 de 5 estrelas4.5/5 (234)
- The Unwinding: An Inner History of the New AmericaNo EverandThe Unwinding: An Inner History of the New AmericaNota: 4 de 5 estrelas4/5 (45)
- Acupuncture & Dentistry: News 67 October 2001Documento1 páginaAcupuncture & Dentistry: News 67 October 2001anlme7899Ainda não há avaliações
- Breast Self-Examination: Knowledge and Practice Among Nurses in United Arab EmiratesDocumento4 páginasBreast Self-Examination: Knowledge and Practice Among Nurses in United Arab EmiratesMuhammad AlfianAinda não há avaliações
- Lumbar StenosisDocumento104 páginasLumbar StenosismohamedwhateverAinda não há avaliações
- Insomnia and CanabisDocumento10 páginasInsomnia and CanabisEbetWasuwayAinda não há avaliações
- Spondylolisthesis PDFDocumento121 páginasSpondylolisthesis PDFishak_alsophAinda não há avaliações
- Auriculotherapy For Pain Management: A Systematic Review and Meta-Analysis of Randomized Controlled TrialsDocumento12 páginasAuriculotherapy For Pain Management: A Systematic Review and Meta-Analysis of Randomized Controlled TrialsSol Instituto TerapêuticoAinda não há avaliações
- Clayton Jensen, Pharmd Candidate 2018 Dabigatran Versus Warfarin in Patients With Mechanical Heart ValvesDocumento2 páginasClayton Jensen, Pharmd Candidate 2018 Dabigatran Versus Warfarin in Patients With Mechanical Heart ValvesClayton JensenAinda não há avaliações
- Drug and Therapeutics Committee: Session 4. Assessing and Managing Medicine SafetyDocumento40 páginasDrug and Therapeutics Committee: Session 4. Assessing and Managing Medicine SafetyPratyAinda não há avaliações
- Gemcitabine Vs BCGDocumento8 páginasGemcitabine Vs BCGmulkikimulAinda não há avaliações
- The Association of Blood Pressure and Primary Open-Angle Glaucoma: A Meta-AnalysisDocumento23 páginasThe Association of Blood Pressure and Primary Open-Angle Glaucoma: A Meta-AnalysisSarah Martinauli HarahapAinda não há avaliações
- Guideline On Bioavailability and BioequivalanceDocumento26 páginasGuideline On Bioavailability and BioequivalanceGima Amezia SariAinda não há avaliações
- Obat TaxolDocumento53 páginasObat TaxolerdynAinda não há avaliações
- RCT LectureDocumento64 páginasRCT LectureAKNTAI002Ainda não há avaliações
- LIPUS TRUST StudyDocumento7 páginasLIPUS TRUST StudymedtechyAinda não há avaliações
- Analytical StudiesDocumento23 páginasAnalytical StudiesnavneetbadeshaAinda não há avaliações
- JCutanAesthetSurg104186-3056457 082924Documento9 páginasJCutanAesthetSurg104186-3056457 082924Elaine MedeirosAinda não há avaliações
- Jurnal - Rhinitis AlergiDocumento8 páginasJurnal - Rhinitis AlergiRezky PutriAinda não há avaliações
- Program Level 1 4 ContactsDocumento7 páginasProgram Level 1 4 ContactsiamarrhinneAinda não há avaliações
- NIDCR Clinical TrialDocumento67 páginasNIDCR Clinical TrialEnrique TrvjilloAinda não há avaliações
- Acp-56 Snars1 - Scoring - v2Documento1.063 páginasAcp-56 Snars1 - Scoring - v2Luluk Panacita100% (2)
- List of Pharmaceutical Manufacturer in BangladeshDocumento11 páginasList of Pharmaceutical Manufacturer in Bangladeshsujal0211100% (1)
- Bmjophth 2017 000109Documento8 páginasBmjophth 2017 000109Faris LahmadiAinda não há avaliações
- DAIDS GuidelinesDocumento112 páginasDAIDS GuidelinesMike SanchezAinda não há avaliações
- Chapter - Iii Aims and ObjectiveDocumento4 páginasChapter - Iii Aims and ObjectiveHakeem Farhan TariqiAinda não há avaliações
- Navitas BABE BrochureDocumento4 páginasNavitas BABE BrochureDurai rajAinda não há avaliações
- 9-A System Model of Oral Glucose AbsorptionDocumento7 páginas9-A System Model of Oral Glucose AbsorptionVitorDiegoAinda não há avaliações
- Pink Esthetic ScoreDocumento6 páginasPink Esthetic ScoreEstefania Beltran TatesAinda não há avaliações
- NEJ 1995 Activador Del PlaminogenoDocumento7 páginasNEJ 1995 Activador Del PlaminogenomrschihuahuaAinda não há avaliações
- Oos-Out of SpecificationDocumento12 páginasOos-Out of Specificationasit_m50% (2)
- NevroblastomprotokollDocumento217 páginasNevroblastomprotokollsfghhhAinda não há avaliações