Escolar Documentos
Profissional Documentos
Cultura Documentos
Hivaidsdm
Enviado por
Jason Ng NgoDescrição original:
Título original
Direitos autorais
Formatos disponíveis
Compartilhar este documento
Compartilhar ou incorporar documento
Você considera este documento útil?
Este conteúdo é inapropriado?
Denunciar este documentoDireitos autorais:
Formatos disponíveis
Hivaidsdm
Enviado por
Jason Ng NgoDireitos autorais:
Formatos disponíveis
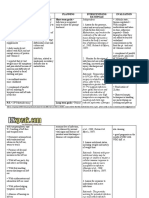
HUMAN IMMUNODEFICIENCY VIRUS (HIV)/ ACQUIRED IMMUNODEFICIENCY SYNDROME (AIDS) Assessment: a.
Malaise, fever, anorexia, weight loss, influenza-like symptoms b. Lymphadenopathy for at least 3 months c. Leukopenia d. Diarrhea e. Fatigue f. Night sweats g. Presence of ooportunistic infections h. Protozoal infections (Pneumocystis jirovecipneumonia, major source of mortality) i. Neoplasms (Kaposis sarcoma, purplish-red lesions of internal organs and skin, B-cell non-Hodgkins lymphoma, cervical cancer) j. Fungal infections (candidiasis, histoplasmosis) k. Viral infections (cytomegalovirus, herpes simplex) l. Bacterial infections Top 8 Issues Facing People with HIV 1. Dealing With a New Diagnosis Find Your Support System It is a fact that living with HIV will change your life. Adjusting to the change will be challenging and won't come over night. It won't be easy, but by seeking out the right support system, the process can be made easier. Once you find out you are positive, take a moment and decide who you feel will be supportive and who won't. You don't need to go through the process alone. Parents, spouses, partners, or families may be good sources of support. Councelors or social workers can also be very helpful in this adjustment time. Don't feel you need to tell everyone about your HIV right away. Only do so when you feel the time is right. 2. Depression 3. Finding the Right Doctor Choose a Doctor that's Right for You Another important step in dealing with your HIV is choosing a doctor to manage your care. While some decide to continue their care with their family physician, experts universally agree that in order to get the best HIV care, you should employ the services of an HIV specialist. 4. Learning About HIV Knowledge is Power - Learn All You Can About HIV The next step in managing this diagnosis, is getting to know the disease. Learn as much as you can about HIV. It is said that knowledge is power. 5. Understanding HIV Medications 6. Adherence to Medication Regimens Some of these tips may help. y To save time, try setting up meds ahead of time using pill boxes. These are available from your health care provider free of charge. y Set the meds up a week ahead of time, saving time each day. y Take the day's box with you to work or when you are out. y Use an alarm on a watch or a timer to tell you when its time for your meds. y If confidentiality is an issue, excuse yourself to the restroom and take your medicines there. y Leave notes around the house where you will be sure to see them; the refrigerator, next to the TV, and the bathroom mirror. y Do trial runs before beginning therapy. Use jelly beans to represent your medications and take them as if they were real antivirals. This will assist you in identifying potential problems in your medication schedule before taking the real thing. 7. Paying the Bills 8. Staying Healthy Staying Healthy One last important step in dealing with your disease is keeping yourself as healthy as possible. While your physicians can help, it is up to you to optimize your health in order to feel good and to live a productive life. Trends:
The best time to start ART is before patients become unwell or develop their first opportunistic infection. The best method to determine when to start treatment is through CD4 testing, which measures the strength of the immune system. The 2010 guidelines promote earlier treatment for all patients, when their CD4 count falls to 350 cells/mm3 or less, regardless of symptoms. The 2010 guidelines propose that countries progressively phase out the use of stavudine as a preferred firstline therapy option and move to lesstoxic alternatives such as zidovudine (AZT) and tenofovir (TDF).
Management: Underlying condition 1. Treatments are available for the underlying immunodeficiency. 2. HIV vaccines studies are showing initial promise as a treatment to prolong life in those already infected with HIV. 3. Treatment is available for some opportunistic infections and other diseases associated with AIDS. Although individual response to treatment can be variable, treatment of opportunistic infections may suppress the disease for months or for the life of the patient. 4. Management requires the expertise of many specialties: infectious disease, pulmonary medicine, gastroenterology, neurology, obstetrics and gynecology, dentistry, surgery, psychiatry, nursing, nutrition, and social work. Specific Treatment 1. Antiretroviral therapy (ART) consist of medications that belongs to three different classifications because they act to prevent HIV replication at three different points along the replication process. The standard for ART is to take a minimum of three different drugs that come from at least two different drug classifications. 2. Highly active antiretroviral therapy (HAART) refers to any medication regimen that can be expected to decrease the viral load to non- detectable. 3. Classes of antiretroviral drugs: a. Nucleoside reverse transcriptase inhibitors (NRTIs) such as zidovudine (AZT), didanosine (ddI), stavudine (d4T) b. Non-nucleoside reverse transcriptase inhibitors (NNRTIs) such as nevirapine (Viramune), efavirenz (Sustiva) c. Protease inhibitors (PIs) such as indinavir (Crixivan), ritonavir (Norvir), and saquinavir (Fortovase) 4. Goals of antiviral therapy: a. Prolong life and improve quality of life b. Reduce viral load to as low as possible for as long as possible c. Increase the CD4 count 5. Indications for antiviral therapy: a. Acute retroviral syndrome or less than 6 months since seroconversion b. HIV symptoms such as oral thrush c. No HIV symptoms but has a CD4 count of 500/mm3 or less and/or a viral load greater than 20,000. Prevention therapies 1. Opportunistic infections a. P. carinii pneumonia (PCP) prophylaxis is started when the CD4 count is less than 200 and the most effective medication is sulfamethoxazole/trimethoprim (Bactrim); others are dapsone, atovaquone (Mepron), and aerosolized pentamidine. b. M avium complex prophylaxis is started when the CD4 count is less than 50; medications used are azithromycin (Zithromax) and clarithromycin (Biaxin) 2. Vaccinations a. Tubercolosis- all patients should be screened every year with a PPD b. Pneumococcal pneumonia- all patients should receive pneumovax every 5 to 6 years c. Influenza- patients with a CD4 greater than 200 should recieve a flu vaccine each fall Supportive Care 1. Treatment of reversible illness 2. Nutritional support 3. Palliation of pain 4. Dental management 5. Evaluation and management of psychological and social aspects of AIDS 6. Treatment to relieve symptoms (cough, diarrhea) 7. Antidepressant drugs; psychiatric interventions Nursing Interventions Reducing Fear 1. Maintain nonjudgmental attitude and nonprejudicial approach. 2. Anticipate that the patient may pass through a series of stages: initial crisis, transitional stage, acceptance state, and preparation for death 3. Allow patient to use denial as a protective mechanism- gives some control over when and how patient will control mortality a. Expect some displaced anger; avoid being personally affronted by patient's anger b. Allow patient to acknowledge reality of the situation without false reassurance 4. Help patient set realistic goals and expectations 5. Offer counseling services, especially when AIDS is initially diagnosed and as patients enters terminal phase of illness
6. Help patient identify and strengthen personal resources and services such as positive coping skills, relaxation techniques, strong support network, and optimistic outlook. 7. Encourage patient to join a support group- helpful in defusing stressful issues and in developing strategies to cope with the disease Preventing infection 1. Have a high index of suspicion for infection even when clinical manifestations are subtle or absentopportunistic infections may be reactivated at any time during the course of the disease 2. Follow universal precaution for all patients 3. Administer prescribed pharmacologic agents; some infections are not treatable with currently available regimens 4. Administer and teach patient/family good skin care- a break in skin is a source of secondary infection; use position changes, emollient lotions, special pads and beds, and attend to hydration and nutrition. Improving Nutritional Status 1. Monitor nutritional status by weighing, recording dietary intake and calorie count, taking anthropometric measurements, and evaluating serum albumin, blood urea nitrogen, protein, and transferrin levels. 2. Monitor for sore throat that progress to dysphagia or odynophagia (pain on swallowing) or persistent heartburnsuggestive of esophageal candidiasis 3. Consult with dietitian to develop strategies for nutritional supplements to maintain strength, comfort, and level of functioning 4. Include patient in making nutrition care 5. For patients with oral/esophageal pain from Candida esophagitis, herpetic esophagitis, endotracheal Kaposi's sarcoma: a. Administer prescribed antifungal therapy b. Avoid highly seasoned or acidic foods c. Offer fluids and blenderized foods to minimize chewing and ease swallowing d. Suggest nutrition-dense supplements such as instant breakfast drinks or protein-fortified juices for home care 8. Discourage excessive alcohol intake- has immunosuppressive effect 9. Encourage small, frequent meals because these may make best use of limited absorptive capacity Relieving Oral Discomfort 1. Ask about persistent sore throat, dysphagia, and heartburn- these sypmtoms are suggestive of oral/esophageal candidiasis 2. Examine mouth for oral candidiasis and other lesions 3. Administer or teach patient to administer prescribed antifungal mounth rinses or lozenges for oral candidiasis or acyclovir (Zovirax) for herpes simplex 4. Perform or encourage oral care two times to three times a day Minimizing the Effects of Diarrhea 1. Keep in mind that gastrointestinal infections and diarrhea decrease absortive efficiency 2. Tell patient to monitor stools for blood and try to determine if bleeding is before, with, or after bowel movement to help determine sources of bleeding 3. Monitor intake and output; assess skin and mucous membranes for poor turgor and dryness, indicating dehydration 4. Administer fluid and electrolytes as prescribed 5. Advise patient to eliminate caffiene, alcohol, dairy products, foods high in fats, fresh juices, and acidic juices. Drink liquids at room temperature. 6. Adise patient to avoid foods that increase intestinal motility and distention, such as gas-forming fruits and vegetables Managing Altered Thought Process 1. Provide daily assessment of mental status; monitor for changes in behavior, memory, concentration ability, and motor system dysfunction- patients may become vegetative and unable to ambulate 2. Reorient patient frequently; use calendar, clock, family/friends' pictures, lists, and structured plan of care. 3. Assess for depressive or suicidal symptoms- AIDS represents risk for suicide Reducing Fever 1. Frequently assess for chills, fever, tachycardia, and tachypnea 2. Teach patient/caregiver to keep a temperature chart 3. Encourage high fluid intake to replace insensible water losses incurred by fever/diaphoresis 4. Administer or teach patient to administer antipyretics as prescribed Improving breathing pattern 1. Provide supplemental oxygen as ordered 2. Watch for sudden change in respiratory function- patient may be developing a secondary infection 3. Administer or teach patient to administer prescribed narcotic for postinfectious cough, a complication of P. carinii pneumonia and viral pneumonia 4. Encourage smoking cessation to enhance pulmonary ciliary defense Health Education: y Eating a more nutritious diet. This can: o Help a person remain healthier overall despite the HIV infection. o Slow down the progression of HIV to AIDS. o Help prevent health problems related to malnutrition.
Help maintain a healthy weight and avoid the excess weight loss that can occur in HIV-infected individuals. A healthy diet for someone living with HIV is one that is rich in whole grains, low fat dairy products, protein, and lots of fresh fruits and vegetables. Include multivitamins, especially B12 and zinc, wherever possible. Remember that a healthy diet is also about what one doesnt eat: Try to cut out fried foods and sugary drinks as much as possible.
Quitting smoking. Close to three out of four people with HIV smoke a significantly higher rate of tobacco use than among people who do not have HIV (21 percent). Syracuse University researchers analyzed data from 212 adults with HIV and found that people with HIV who smoked also reported having more symptoms such as coughing and dizziness. Stopping illicit drug use. If a HIV-positive person is using illegal drugs such as cocaine, heroin, or methamphetamines, seek treatment for the addiction. Sharing needles to use such drugs can leave one vulnerable to other infections such as hepatitis, and that may lead to more rapid progression of HIV to AIDS. Illegal drug use could also affect the HIV disease itself. A recent study from the University of Pennsylvania School of Medicine demonstrated a dramatic increase in the ability of HIV to attack healthy cells when methamphetamine is present in the bloodstream. Getting moderate exercise. Being physically active three to six times a week can help improve ones mood and outlook as well as improve the overall quality of life. The benefits of exercise include fighting HIV symptoms of appetite loss and nerve pain, and reducing the risk of other chronic diseases such as diabetes, heart disease, and osteoporosis. Practicing safer sex. Having HIV does not mean the end of ones sex life but one should always use a new latex condom whenever engaging in sex. This will protect the partner from the HIV infection and will protect oneself from sexually transmitted diseases (STDs) that can complicate ones health status. Getting tested and treated for sexually transmitted diseases. Many people with HIV also have other STDs, even if they are asymptomatic. Get tested to find out whether any other infections are present and get treated if so. Taking medications as prescribed and visiting the doctor often. The doctor may have prescribed HIV medications to help the bodys immune system stay healthy longer. Taking those medications as prescribed, even though it may be difficult to keep up with the medication schedule, is extremely important. Taking medications on schedule is called adherence it is important because it will reduce the risk that HIV will become drug resistant and it will also give the body the best chance at keeping the virus under control. Taking steps to prevent infections. If one has HIV, one can get infections more easily. Many of the healthy lifestyle steps above will help avoid these infections for example, quitting smoking removes a significant contributor to lung infections. There are some other steps to take to reduce common causes of infection, such as washing hands well and often, practicing good food safety to avoid foodborne illness, and staying current on recommended vaccines. Making these changes in life will help one stay healthier longer, even with HIV.
DIABETES MELLITUS Assessment: a. Polyuria, polydipsia, polyphagia (more common in type 1 diabetes mellitus) b. Hyperglycemia c. Weight loss (common in type 1 diabetes mellitus, rare in type 2 diabetes mellitus d. Blurred vision e. Slow wound healing f. Vaginal infections g. Weakness and paresthesias h. Signs of inadequate circulation to the feet i. Signs of accelerated Atherosclerosis (renal, cerebral, cardiac, peripheral) Issues: y April is deemed Foot Issues Related to Diabetes Awareness Month. Unfortunately, many people with diabetes are unaware of the importance of routine foot care. Physicians and educators are constantly reminding the public of the importance of measuring insulin levels and making sure to follow a diet and exercise plan. What about checking your feet for ulcers, callous and sores? This is a critically important preventive measure as it can potentially save your limb. y Recent statistics show that more than half of the 20 million Americans with diabetes have no idea what a foot ulcer is, yet more than three million (15%) of them will develop a foot ulcer, and 25% of those will require a lower limb amputation as result of their ulcer not healing and becoming infected. y The child with type 1 DM Trends: Islet Transplant for Type I Diabetes During an islet transplant for type 1 diabetes, insulin-producing beta cells contained in clusters called islets are isolated from a cadaver donor's pancreas, then injected through the skin into the portal vein of the recipient's liver. The islet cells flow into the liver, lodge in small blood vessels and release insulin. The procedure temporarily reverses diabetes, allowing many recipients to discard their blood glucose meters, pumps and syringes to live free from diabetes for the first time in their lives. But much work remains to be done. After a transplant, recipients must take immunosuppressive medications which have potential side effects for the rest of their lives to prevent transplant rejection. Management: Diet 1. Dietary control with caloric restriction of carbohydrates and saturated fats to maintain ideal body weight.
2. The goal of meal planning is to control blood glucose and lipid levels 3. Weight reduction is a primary treatment for type 2 DM Exercise Regularly scheduled exercises to promote the utilization of carbohydrates, assist with weight control, enhance the action of insulin, and improve cardiovascular fitness. Medication 1. Oral antidiabetic agents for patients with type 2 DM who do not achieve glucose control with diet and exercise only a. Act by a variety of mechanisms, including stimulation of insulin secretion from functioning beta cells, reduction of hepatic glucose production, enhancement of peripheral sensitivity to insulin, and reduced absorption of peripheral sensitivity to insulin, and reduced absorption of carbohydrates from the intestine. b. Sulfonylureas and meglitinide analogues may cause hypoglycemic reactions c. Biguanides, alpha-glucosidase inhibitors, and megalinited analogues may cause significant flatus and gastrointestinal adverse effects 2. Insulin therapy for patients with type 1 DM who require replacement a. May also used for type 2 DM when unresponsive to diet, exercise, and oral antidiabetic therapy b. Hypoglycemia may result, as well as rebound hyperglycemia (Somogyi Effect) c. Often results in increased appetite and weight gain Nursing Intervention Improving Nutrition 1. Assess current timing and content of meals 2. Advise patient on the importance of an individualized meal plan in meeting weight-loss goals 3. Discuss the goals of dietary therapy for the patient 4. Assist the patient to identify problems that may have an impact on dietary adherence and possible solutions to these problems 5. Explain the importance of exercise in maintaining/reducing body weight. a. Caloric expenditure for energy in exercise b. Carry-over of enhanced metabolic rate and efficient food utilization 6. Assist patient to establish goals for weekly weight loss and incentives to assist in achieving them 7. Strategize with the patient to address the potential social pitfalls of weight reduction Teaching About Insulin 1. Assist patient to reduce fear of injection by encouraging verbalization of fears regarding insulin injections, conveying a sense of empathy, and identifying supportive coping techniques 2. Demonstrate and explain thoroughly the procedure for insulin self-injection 4. Review dosage and time of injections in relation to meals, activity, and bedtime based on patient's individualized insulin regimen Preventing Injury Secondary to Hypoglycemia 1. Closely monitor blood glucose levels to detect hypoglycemia 2. Instruct patient in the importance of accuracy in insulin preparation and meal timing to avoid hypoglycemia 3. Assess patient for signs and symptoms of hypoglycemia a. Adrenergic- sweating, tremor, pallor, tachycardia, palpitations, nervousness from the release of adrenalin when blood glucose falls rapidly b. Neurologic- headache, light headedness, confusion, irritability, slurred speech, lack of coordination, staggering gait from depression of central nervous system as glucose level progressively falls 4. Treat hypoglycemia promptly with 10 to 15 g of fast-acting carbohydrates 5. Encourage patient to carry a portable treatment for hypoglycemia at all times Improving Activity Tolerance 1. Advise patient to assess blood glucose level before and after strenuous exercise 2. Instruct patient to plan exercises on a regular basis each day 3. Encourage patient to eat a carbohydrate snack before exercising to avoid hypoglycemia 4. Advise patient that prolonged strenuous exercise may require increase food at bedtime to avoid nocturnal hypoglycemia 5. Instruct patient to avoid exercises whenever blood glucose levels exceed 250 mg/d and urine ketones appear 6. Counsel patient to inject insulin into the abdominal site on days when arms or legs are exercised Maintaining Skin Integrity 1. Assess feet and legs for skin temperature, sensation, soft tissue injuries, corns, calluses, dryness, hammer toe or bunion deformation, hair distribution, pulses, deep tendon reflexes 2. Maintain skin integrity by protecting feet from breakdown a. Use heel protectors, special mattresses, foot cradles for patients on bed rest b. Avoid applying drying agents to skin (eg. alcohol) c. Apply skin moisturizers to maintain suppleness and prevent cracking and fissures 3. Instruct patient in foot care guidelines 4. Advise the patient who smokes to stop smoking or reduce if possible, to reduce vasoconstriction and enhance peripheral blood flow. Help patient to establish behavior modification techniques to eliminate smoking in the hospital and to continue them at home for smoking cessation program
Health education: Choose healthy foods and maintain a healthy weight. Losing just 5 to 10 percent of ones body weight (if overweight) can make a significant difference in the blood sugar control. A healthy diet is one full of fruits, vegetables, whole grains and legumes, with a limited amount of saturated fat. Make physical activity part of a daily routine. Regular exercise can help prevent pre-diabetes and type 2 diabetes, and it can help those who already have diabetes to maintain better blood sugar control. Thirty minutes of moderate exercise such as brisk walking most days of the week is recommended. A recent study found that a combination of exercises aerobic exercises, such as walking or dancing, most days, combined with resistance training, such as weight lifting or yoga twice a week helps control blood sugar more effectively than either type of exercise alone. Lifestyle for type 1 and type 2 diabetes : Identify oneself. Wear a tag or bracelet that says one has diabetes. Keep a glucagon kit nearby in case of a low blood sugar emergency and make sure the significant others know how to use it. Schedule a yearly physical and regular eye exam. The regular diabetes checkups aren't meant to replace yearly physicals or routine eye exams. During the physical, the doctor will look for any diabetes-related complications and screen for other medical problems. The eye care specialist, on the other hand, will check for signs of retinal damage, cataracts and glaucoma. Keep the immunizations up-to-date. High blood sugar can weaken ones immune system. Get a flu shot every year, and get a tetanus booster shot every 10 years. The doctor will likely recommend the pneumonia vaccine, as well. The Centers for Disease Control and Prevention (CDC) also currently recommends hepatitis B vaccination if one hasnt previously been vaccinated against hepatitis B and is an adult aged 19 to 59 with type 1 or type 2 diabetes. The most recent CDC guidelines advise vaccination as soon as possible after diagnosis with type 1 or type 2 diabetes. If one is aged 60 or older and have diabetes and haven't previously received the vaccine, talk to the doctor about the whether it's right to get immunizations. Pay attention to the feet. Wash the feet daily in lukewarm water. Dry them gently, especially between the toes. Moisturize with lotion, but not between the toes. Check the feet every day for blisters, cuts, sores, redness or swelling. Consult the doctor if a sore or other foot problem is noticed, which doesn't start to heal on its own. Dont cut nails too short. It may cause unnoticed injury to fingers and toes. Choose footwear carefully. Avoid wearing open shoes or sandals. The shoes should neither be tight-fitting nor very loose. The insides should be soft, smooth, without sharp edges, and well cushioned. Never walk barefooted even inside the house. Keep the blood pressure and cholesterol under control. Eating healthy foods and exercising regularly can go a long way toward controlling high blood pressure and cholesterol. Medication may be needed, too. Take care of ones teeth. Diabetes may leave a person prone to gum infections. Brush and floss at least twice a day. And if one has type 1 or type 2 diabetes, schedule dental exams at least once a year. Consult the dentist right away if the gums bleed or look red or swollen. If one smokes or uses other types of tobacco, ask the doctor to help quit. Smoking increases the risk of various diabetes complications, including heart attack, stroke, nerve damage and kidney disease. Smokers who have diabetes are more likely to die of cardiovascular disease than are nonsmokers who have diabetes, according to the American Diabetes Association. Talk to the doctor about ways to stop smoking or to stop using other types of tobacco. If one drinks alcohol, do so responsibly. Alcohol can cause either high or low blood sugar, depending on how much a person drinks and if he/she eats at the same time. If one chooses to drink, do so only in moderation one drink a day for women and two drinks a day for men and always with food. Remember to include the carbohydrates from any alcohol one drinks in the daily carbohydrate count. Take stress seriously. If a person is stressed, it's easy to abandon the usual diabetes management routine. The hormones that the body may produce in response to prolonged stress may prevent insulin from working properly, which only makes matters worse. To take control, set limits. Prioritize tasks. Learn relaxation techniques. Get plenty of sleep. Above all, stay positive. The good habits one adopts today can help enjoy an active, healthy life with diabetes. Spiritual needs: y All individuals have spiritual needs, regardless of religious belief or personal philosophy of life. y Individuals with Chronic Illness have identified spirituality spirituality as a resource that promotes quality of life y In the study of nurses perceptions of patients spiritual needs , Boutell and Bozeht identified the concept of FAITH ( in religious belief), PEACE (inner strength), HOPE, TRUST ( in the importance of religious practice), COURAGE and LOVE. 1. Hope And now O Lord, what do I wait for? My hope is in you. (Psalm 39: 7) ~"Focusing of attention, affectivity and commitment to action toward the future goal of fulfillment in God, the realization of the reign of God". 2. Trust I trust in you, O Lord. I say, You are my God. (Psalm 31:14) ~ "A feeling that somehow tomorrow will not be beyond our capacities. A sense of security that Gods healing power will be operative in our life". 3. Courage I took courage for the hand of the Lord, my God, was upon me. (Ezra 7:28) ~ "The ability to transcend ones fears, to choose to actively face what needs to be" (Ruth Stoll) 4. Faith Daughter, Your faith has healed you (Luke 8:48) ~The basis of our personal relationship with God on whose strength and absolute sureness we can literally stake our lives.
y y
y y
y y
5. Peace May the Lord give strength to His people, may the Lord bless His people with peace (Psalm 29:11) ~"A sense of being undisturbed, a feeling of freedom from anxiety and fear. Theologically, peace is a right relationship with God, which entails forgiveness, reconciliation and union". 6. Love How precious is your steadfast love, O God. (Psalm 36:7) ~Gods love encompasses human love for God, for neighbor, for creation and for self. Gods love declares I will never leave you or forsake you. Other Spiritual needs of DIABETIC PATIENT y Emotional support is critical to being able to conquer patients diabetes and defeat it. Emotional support also helps to reduce the stress in our lives. Without the support of patients mother, daughter, sister, and brother, the author believes that the patient would either still be diabetic today or dead. y Social support is also critical to being able to conquer patients diabetes and defeat it. Social support is an aspect of diabetes management that most diabetes programs fail to address. There are many places where patient can obtain emotional and social support: y Patients family members and friends y patients community, e.g. a local support group y Patients church, e.g. pastor, church leader, church member y Patients inner spirit (spirituality) y A member of patients healthcare team, i.e. dietitian, health coach y Training class, workshop, webinar, teleseminar y Internet, e.g. online support group y Educational materials, e.g. diabetes book, DVD For HIV/AIDS: y Spiritual care of the person living with HIV or AIDS may take many forms depending on the stage and current symptomatology of the illness. Spiritual needs of HIV infected person: listening to the patient's "stories" surrounding the illness offering small gestures of friendship providing empathy and emotional support allowing the patient to take the lead in the offering of prayer presenting the patient with a nonjudgemental attitude y For the HIV- positive individual who is physically and cognitively well enough to participate, activities such as creating and appreciating religious art or poetry may provide healing for the heart REFERENCES: th Saunders Comprehensive Review 4 Ed. Retrieve from the world wide web http://aids.about.com/od/howtostayhealthy/tp/hivissues.htm http://www.cdc.gov/hiv/topics/surveillance/index.htm http://www.everydayhealth.com/hiv-aids/healthy-lifestyle-choices-for-people-with-hiv.aspx http://www.who.int/nmh/publications/ncd_report_chapter1.pdf http://www.battlediabetes.com/diabetes-foot-issues http://www.ucsfhealth.org/conditions/diabetes_mellitus/treatment.html http://www.mayoclinic.com/health/diabetes/DS01121/DSECTION=lifestyle-and-home-remedies http://www.spirituallygrowingwithcancer.org/Spiritual_Needs_for_Living_With_Chronic_Illness_page.html http://www.umm.edu/altmed/articles/spirituality-000360.htm on February 14, 2012.
Prepared and Compiled by: Chua, Kristina Ngo, Jason N. Panong, Sheena Marie Sajiran, Qhartinee Sali, Mohammad Elshad Trota, Rizza Lousie BSN IV-A
Você também pode gostar
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceNo EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceNota: 4 de 5 estrelas4/5 (895)
- Literature Review On Male CircumcisionDocumento7 páginasLiterature Review On Male Circumcisionafmzodjhpxembt100% (1)
- Never Split the Difference: Negotiating As If Your Life Depended On ItNo EverandNever Split the Difference: Negotiating As If Your Life Depended On ItNota: 4.5 de 5 estrelas4.5/5 (838)
- Pandemic Threat Planning, Preparation, and Response Reference GuideDocumento22 páginasPandemic Threat Planning, Preparation, and Response Reference GuideMartin MendezAinda não há avaliações
- The Yellow House: A Memoir (2019 National Book Award Winner)No EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Nota: 4 de 5 estrelas4/5 (98)
- Learning Competencies 2nd To 4th QuarterDocumento744 páginasLearning Competencies 2nd To 4th QuarterHazel Tangca-agAinda não há avaliações
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeNo EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeNota: 4 de 5 estrelas4/5 (5794)
- Prevention of DiseaseDocumento18 páginasPrevention of Diseaserajforever17Ainda não há avaliações
- Instruction: Stay Home / Stay Alert / Stay Safe / Control Virus / Win CovidDocumento6 páginasInstruction: Stay Home / Stay Alert / Stay Safe / Control Virus / Win Covidrenugadevi_dAinda não há avaliações
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaNo EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaNota: 4.5 de 5 estrelas4.5/5 (266)
- Api StaphDocumento4 páginasApi Staphsam214100% (1)
- The Little Book of Hygge: Danish Secrets to Happy LivingNo EverandThe Little Book of Hygge: Danish Secrets to Happy LivingNota: 3.5 de 5 estrelas3.5/5 (400)
- OKU Musculo Infection CH 04Documento12 páginasOKU Musculo Infection CH 04Jose Enrique FonsecaAinda não há avaliações
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureNo EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureNota: 4.5 de 5 estrelas4.5/5 (474)
- Chen Et Al., 2020Documento3 páginasChen Et Al., 2020Amanda Cristina MosiniAinda não há avaliações
- Otitis Media Nurisng Care PlanDocumento11 páginasOtitis Media Nurisng Care PlanRnspeakcom100% (1)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryNo EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryNota: 3.5 de 5 estrelas3.5/5 (231)
- A MatrixDocumento11 páginasA MatrixChristian MakandeAinda não há avaliações
- Science Keybook-G 4-CompleteDocumento42 páginasScience Keybook-G 4-CompleteAyomide MatthewAinda não há avaliações
- The Emperor of All Maladies: A Biography of CancerNo EverandThe Emperor of All Maladies: A Biography of CancerNota: 4.5 de 5 estrelas4.5/5 (271)
- Guidline NTM 2020Documento36 páginasGuidline NTM 2020irfanAinda não há avaliações
- The Unwinding: An Inner History of the New AmericaNo EverandThe Unwinding: An Inner History of the New AmericaNota: 4 de 5 estrelas4/5 (45)
- Antibiotics: Microbial Control Antimicrobial AgentsDocumento25 páginasAntibiotics: Microbial Control Antimicrobial AgentsMohammed Moutasim AyoubAinda não há avaliações
- Hepati Tac AbstractDocumento296 páginasHepati Tac AbstractMagda MagAinda não há avaliações
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersNo EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersNota: 4.5 de 5 estrelas4.5/5 (345)
- Fevers SeminarDocumento20 páginasFevers Seminardagnenegash987Ainda não há avaliações
- Team of Rivals: The Political Genius of Abraham LincolnNo EverandTeam of Rivals: The Political Genius of Abraham LincolnNota: 4.5 de 5 estrelas4.5/5 (234)
- Soroori-Motlagh Nastaran 200705 (SCID)Documento29 páginasSoroori-Motlagh Nastaran 200705 (SCID)Charles IppolitoAinda não há avaliações
- Journal Article 1 PDFDocumento8 páginasJournal Article 1 PDFgerald davidAinda não há avaliações
- Artikel Bahasa InggrisDocumento2 páginasArtikel Bahasa InggrisTahsya Ria Shafira100% (1)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreNo EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreNota: 4 de 5 estrelas4/5 (1090)
- Approach To The Patient With Rheumatic DiseaseDocumento11 páginasApproach To The Patient With Rheumatic DiseasetedplushAinda não há avaliações
- Bacterial Pathogenesis - Unhalu09Documento44 páginasBacterial Pathogenesis - Unhalu09MardhisemAinda não há avaliações
- Bio Q4 Module 1 - Week 1Documento21 páginasBio Q4 Module 1 - Week 1Ronaldo E. De LeonAinda não há avaliações
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyNo EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyNota: 3.5 de 5 estrelas3.5/5 (2259)
- Prevention of Nosocomial Infections As Percieved by Staff Nurses - For SubmisionDocumento31 páginasPrevention of Nosocomial Infections As Percieved by Staff Nurses - For SubmisionDhonnalyn Amene CaballeroAinda não há avaliações
- Common Illnesses: 1. Write The Correct Illness After Reading The Clues. Each Illness Has Two CluesDocumento4 páginasCommon Illnesses: 1. Write The Correct Illness After Reading The Clues. Each Illness Has Two Cluesmcarmendgj74Ainda não há avaliações
- Siemens Arcadis Varic ReplacementDocumento96 páginasSiemens Arcadis Varic ReplacementLeonardo ChirinosAinda não há avaliações
- Clsi Ila23 ADocumento52 páginasClsi Ila23 ACristian Gutiérrez VeraAinda não há avaliações
- Bakteri PenginfeksiDocumento3 páginasBakteri PenginfeksiVenita NapitAinda não há avaliações
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)No EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Nota: 4.5 de 5 estrelas4.5/5 (121)
- BordetellaDocumento54 páginasBordetellatummalapalli venkateswara rao100% (2)
- Philippine Health Advisories, 2012 PDFDocumento170 páginasPhilippine Health Advisories, 2012 PDFRyan Michael OducadoAinda não há avaliações
- Please, Take The Big 5 of The Most Disease That Occure in Your Workplace and Make A Resume From That SituationDocumento8 páginasPlease, Take The Big 5 of The Most Disease That Occure in Your Workplace and Make A Resume From That Situationtrah starkAinda não há avaliações
- MD PaediatricsDocumento23 páginasMD PaediatricsRutuja DevghareAinda não há avaliações