Escolar Documentos
Profissional Documentos
Cultura Documentos
Ana Complete Proposal
Enviado por
zorrotranDescrição original:
Direitos autorais
Formatos disponíveis
Compartilhar este documento
Compartilhar ou incorporar documento
Você considera este documento útil?
Este conteúdo é inapropriado?
Denunciar este documentoDireitos autorais:
Formatos disponíveis
Ana Complete Proposal
Enviado por
zorrotranDireitos autorais:
Formatos disponíveis
Chapter 1 Introduction
According to the United Nations Childrens Fund (UNICEF) the mortality risk of a pregnant woman in Mexico is one in 370, while in the United States is one in 2500 (UNICEF, 2000). The National Institute of Statistics, Geography and Informatics of Mexico (INEGI), moreover has reported that the maternal mortality in recent years increased from 54 maternal deaths in 2000 to 66 in 2002 per 100,000 live births, being the third cause of death among women from 15 to 34 years (INEGI, 2003). These discouraging rates are associates that many women in Mexico receive late or no prenatal care, which increase the rate of maternal mortality and impacts the rate of infant mortality, where the 50% of infant death during the first year of life is directly attributed to conditions originating in the perinatal period (INEGI, 2003), and is increasing the rate of low birth weigh and very low birth weigh that may require prolonged care in neonatal units of high cost compared with the cost of prenatal care. Prenatal care (PNC) is one of the most widely used preventive health service worldwide and represents the cornerstone in the health care of pregnant women and future newborn. The consensus within the international community is that early and adequate PNC supplied by a health care provider improves perinatal outcome (World Health Organization [WHO], 2003). As same as the WHO the Official Mexican Norm Attention of the Pregnant Woman recommends that the initiation of the PNC must be during the first 12 weeks of pregnancy (Secretary of Health of Mexico, 1993; WHO, 2003). WHO highlights the importance of the first prenatal visit since this is when a careful assessment of the womans antecedents is done through the anamnesis, physical exam and laboratory tests that will guide the development of a plan to maintain a healthy pregnancy. Moreover, they mention
that the first visit is important as it begins educating the woman about labor and delivery, risks prevention and warning signs of possible complications of pregnancy (WHO, 2003). Early initiation of prenatal care has been associated to increase birth weight, lower newborn hospitalization, and reduced rates of low birth weight and very low birth weight in vulnerable women than are at great risk for adverse pregnancy outcomes (Michigan Department of Community Health, 2004; Reichman & Florio, 1996). Moreover, has been reported that prenatal care was a protective factor for stillbirth (Romero-Gutierrez, Martinez-Ceja, Abrego-Olvira & Ponce-Ponce, 2005). Others authors (Byrd, Muller, Selwyn & Lorimor, 1996) emphasize that the early initiation of PNC brings important benefits as the promotion of an adequate nutrition, to inform on use of drugs and alcohol, the early diagnoses of pregnancy problems and to treat sexually transmitted infections (STI) that may endanger the mother and the fetus. Even with all this scientific evidence of the benefits of an early PNC initiation, in Mexico only 29.6% of the women in the 2000 National System for Open Population initiated PNC during the first trimester of pregnancy, 34.4% did in the second trimester and 36.0% in the third trimester (INEGI, 2000). The deficient initiation of PNC in Mexico may be due to multiple associated causes to this behavior, and not only for a poor utilization of available services. A review of prenatal programs in the United States (US) has shown that efforts to improve access to PNC fail because of poor utilization of health services due to multiple biopsichosocials factors that affect the decision of the pregnant women to initiate an early prenatal care (Cook, Seling, Wedge & Gohn-Baube, 1999; Hulsey, 2001). In Mexico, some descriptive studies have reported sociodemographic and socioeconomic barriers for early initiation of PNC such as low socioeconomic level, low education, transportation problems and multiparity (Bronfman-Pertzovsky, Lpez-Moreno, MagisRodrguez, Moreno-Altamirano & Rutstein, 2003; Frank, et al., 2004; Martnez-Gonzlez, Reyes-Frausto & Garca-Pea, 1996).
As it becomes necessary to know more about the biopsychosocial factors affecting the decision to initiate an early PNC, the role of professional nursing as a health provider in promoting health behaviors that increase the quality of life of the populations is evident. Nursing should participates increasing knowledge and understanding of the different predictive factors of the initiation of PNC, and in the identification of those women at risk for late or no prenatal care. In order to achieve this, it is necessary to study this phenomenon as a whole throughout an appropriate conceptual theoretical framework that offers to considerate all the biopsichosocial factors that affect the decision of the pregnant women to engage in this health behavior. Because theory-linked research is conceived and conducted within the framework of theory, the findings of the research have greater potential for contributing to the development of useful knowledge, giving a most complete vision and explanation of the phenomenon in study (Chinn & Kramer, 1995; Silva, 2004). The theories are used in a deductive manner as base to generate specific explicative prediction, if they are data sustained increase the credibility of the theory (Fawcett, 1999; Polit & Hungler, 2000). The Health Promotion Model (HPM) (Pender, Murdaugh & Parsons, 2002), was selected to guide this study because is a nursing model than was proposed as guide to explore complex biopsichosocial processes that motivate individuals to engage in behaviors directed toward the enhancement of health. Applying this theoretical model (HPM) to the initiation of prenatal care will allow a most complete explanation and understanding of the pregnant womans behavior one allow to find the demographic, psychological, and sociocultural factors that influence in the perception of motivators and barriers of initiation of PNC. The main purpose of this study is to uncover predictive explicative factors of initiation of prenatal care in Mexico through the multivariate HPM theoretical framework (Pender et al., 2002), than may affect the likelihood that the pregnant women initiate the
prenatal care, and to generate an explicative middle-range theory to enlarge our understanding of what is the reason that many women in Mexico delay initiate of PNC. This knowledge will assist nursing to design appropriate interventions promoting early initiation of prenatal care and health-seeking behaviors to improve perinatal outcomes. A descriptivecorrelation-predictive study design is proposed.
Conceptual Theoretical Framework In this section, a review of the theoretical model that guide this study is described as well as the relationship of the chosen concepts of the Health Promotion Model and the operational and theoretical definitions of each concept. A diagram of the initial model and the interrelations of the concepts to be proved are shown. Pender et al. (2002) describe health promotion as a behavior motivated by the desire to increase well-being and actualize human health potential. On the other hand, health protection is a behavior motivated by the desire to actively avoid illness, detect it early, or maintain functioning within the constraints of illness. According to these authors, the behaviors of health promotion and health protection are complementary processes and both are critical to the quality of life at all stages of human development. The HPM (Pender et al., 2002) integrates constructs from the expectancy-value theory (EVT) and social cognitive theory (SCT), within a nursing perspective. The HPM describes the multidimensional nature of persons interacting with their interpersonal and physical environment as they pursue health. To this study, five of ten concepts described by the HPM which and are congruent with the purpose of this study will be measured and proved. Through the conceptual theoretical empirical structure the concept are defined from a most abstract level to a most concrete level through specific empirical indicators to initiation of prenatal care behavior (Appendix A).
The HPM provides flexibility in the selection of variables to be measures as individual characteristics and past experiences in such a way to allow the capture of variables. These variables may be highly relevant to a specific health behavior or a particular target population but are less specific when applied to others health behaviors or others populations. The concepts and their interrelations are described subsequently following the way in which the HPM proposes to group them as individual characteristics and experiences, behavior -specific cognitions and affect, and behavioral outcome. Pender et al. (2002) propose that each person has unique characteristics and experiences that influence subsequent action. These characteristics and experiences may act as developers or obstacles to carry out the desired behavior. According to the HPM, the prior experience behavior of a person may have a direct and indirect effect on the likelihood of engaging in health promoting behaviors. The direct effect would be given to habit formation, predisposing one to engage in the behavior automatically, or placing little attention to the specific details of its execution. The indirect influence of prior experience on health promoting behavior can be seen in an individuals perception of benefits and barriers. If the benefits are experienced early in the course of the behavior, there is more probability that this behavior be repeated. On the other hand, if barriers are experienced, these are stored in memory as obstacles. Only when these obstacles are removed, will the individual be able to engage successfully in the behavior. Each incident of a behavior is also accompanied by emotions or affect that can be given in a positive or negative way, during or after the behavior. This is then encoded into memory as information that is recalled while engaging in the behavior on subsequent occasions. Prior experience-behavior is proposed as shaping all of these behavior-specific cognitions that may improve or diminish the likelihood to engage in a specific health promoting behavior. In the literature review, PNC perception as being less important, tends to diminish the early initiation of PNC and is more frequently seen in older women with
greater experience of prior pregnancies (Roberts, et all., 1998). It is proposed for this study that prior related experience will be the positive or negative experience of a prior pregnancy that will include: experience of prenatal care, pregnancy problems, deliveries experiences, miscarriage, and children born with health problem. According to Pender et al. (2002), the relevant personal factors predictive of a given behavior are shaped by the target behavior being considered. Between the personal characteristics that would affect the execution of a health behavior would be biological, psychological and sociocultural factors. The HPM propose that personal factors may have a direct influence over the health behavior, or may have an indirect influence through the perception of barriers and motivators. Knowing the existence of many personal factors, only will be included the ones than are relevant to explain or predict the specific behavior. According to the literature, the probability to initiate PNC is affected by biological factors as mothers age and parity (Delgado-Rodriguez, Gmez-Olmedo, Bueno-Cavanillas & Glvez-Vargas, 1997; Hulsey, 2001; Johnson et al., 2003); demographic factors such as marital status of the mother, socioeconomic level, educational level, health insurance, mothers occupation and number of children living with her (Bloom et al., 2004; DelgadoRodriguez et al., 1997; Erci, 2003; Fuller & Gallagher, 1999; Johnson et al., 2003; Hulsey, 2001); psychological factors such as depression and stress (Cook et al., 1999; DelgadoRodriguez et al., 1997; Erci, 2003; Johnson et al., 2003; Roberts et al., 1998; Tyson, Higgins & Tyson, 1999); and finally, the most reported sociocultural factors are family dysfunction and domestic violence (El-Mohandes et al., 2003; Huth-Bocks, Levendosky & Bogat, 2002; McFarlene, Parker & Soeken, 1996; Tyson et al., 1999). For this study, personal factors will be all those demographic, psychological and sociocultural factors that may increase or decrease the likelihood of early initiation of prenatal care. Demographic factors will be maternal age, parity, marital status, socioeconomic level, educational level, mothers occupation and number of relatives living
with her. Psychological factors will be the mothers stress and depression. The cause of stress is associated to environmental and internal demand and conflicts among them, which tax or exceed a persons resources, and it is linked to decreased life satisfaction (Pender et al., 2002). Sociocultural factors will refer to domestic violence defined by the WHO (1994) as: any act of gender-based violence result in, or is likely to result in, physical, sexual, or psychological harm or suffering to women, including threat of such acts, coercion or arbitrary deprivation of liberty, whether occurring in public or in private life (p.1). According with the HPM an environment loaded with cues that trigger action, as is domestic violence, may have a direct influence to avoid performing the behavior or an indirect influence through the increase barriers perception (Pender et al., 2002). The behavior-specific cognitions and affect in the HPM are considered to be of major motivational significance. These variables constitute the critical core for a future nursing intervention since they are subject to modification through the actions of nursing. In this study, three of the concepts that compose this level were considered because they are associated to the purpose of this research proposal. Perceived benefits of the HPM, are seen as the direct motivator of the behavior. Anticipated benefits of action are mental representations of the positive consequences that will bring the execution of a behavior. The motivational importance of anticipated benefits is based on personal knowledge of the outcome of prior experience with the behavior. Individuals tend to invest time and resource in activities with a high likelihood of increasing their experiences of positive outcomes, and benefits from performing these behaviors may be intrinsic or extrinsic. The intrinsic benefits include personal perceptions; on the other hand the extrinsic can include economic rewards or social interaction that may occur as a result of engaging in the behavior. Initially, extrinsic benefits of health behaviors may be of high motivational significant, whereas intrinsic benefits may be more powerful in
motivating continuation of health behaviors. The literature mentions that women, who perceive having a healthy baby and learning about pregnancy health care as benefits, wanted to be prepared for delivery and motherhood, were more likely to initiate early PNC (Byrd et al., 1996; Erci, 2003; Fuller & Gallegher, 1999). In this study, perceived benefit will be considered every factor that motivates the behavior of early initiation of PNC and will include personal perception of pregnancy benefits (to have a healthy baby, to learn about pregnancy health care and to be prepared for motherhood), and perception about structural benefits of health system (clinic with good service or access to PNC). The barriers are perceptions concerning the unavailability, inconvenience, expense, difficulty, or time-consuming nature of a particular action. These barriers, according to the HPM (Pender et al., 2002), may be real or imagined and are often viewed as the blocks, hurdles, and personal costs of undertaking a given behavior. The barriers usually arouse motives of avoidance in relation to a given behavior. For this study, perceived barriers will be considered all factors reported by the pregnant woman that impeded or delays to engage in the behavior of an early initiation of PNC. These will be divided into personal barriers (embarrassed to be examined, inconvenient to attend appointments, difficulties with the health provider, cigarette, and alcohol or drug consumption antecedents) and as structural barriers (difficulty to obtain appointments, transportation problems, prolonged time of wait, full clinics). Interpersonal influences are cognitions concerning the behaviors, beliefs or attitudes of others. The main source of interpersonal influences in promoting health behavior are the family, the peers and the health care provider affecting behavior through social pressures or encouragement to commit to a plan of action. According to the HPM, individuals vary in the extent to which they are sensitive to the desires, examples and praise of others. In order for interpersonal influences to have an effect, individuals must attend to the behavior, wishes,
and inputs of other; comprehend them; and assimilate them into cognitive representations related to given behaviors (Pender et al., 2002). In this study, interpersonal influences of early or late initiation of PNC include support or lack of support by family members (partner, mother, sister, other), peers (friends, neighbor, coworkers) and health care providers (physician, nurse and social worker); throughout instrumental stimuli (providing help for transportation, child care, economic stimuli) and emotional support (encouraged or discouraged to get PNC). In the HPM, the health promoting behavior is the final point of action outcome and should be the behavior that seeks a positive health outcome for the client. In this study, the health promoting behavior will be defined as the time of initiation of PNC, and this will be established by the difference between the date of the last menstrual period and the date of the first PNC visit. Figure 1 shows the proposed initial explicative model with the direct and indirect effect than may have the 5 concept of the HPM, with the outcome variable. Each one of the proposal variables will be probed through this study to generate the middle range theory of predictive explicative factors of initiation of PNC in Mexico.
10
Individual Characteristics and Experiences
Prior experience: prior PNC, type delivery, abortion, pathology.
Behaviors-Specific Cognitions and Affect
Behavioral Outcome
Demographic factors: age, marital status, education, work, income, number family members, parity.
Perceived benefits to PNC: Personal: to have a healthy baby, to learn about the pregnancy health care, to be prepared for motherhood. Structural: clinical with good service and access to PNC.
Psychological factors: Stress and depression in current pregnancy.
Interpersonal influences: social support Initiation of PNC
Sociocultural factors: Domestic violence
Perceived barriers to PNC: Personal: negative attitude toward pregnancy and PNC, problem with health providers, smoke, alcohol, and drug. Structural: difficulty with clinic, inconvenient to attend for transportation or childcare problems.
Figure 1: Initial model of predictive factors of initiation of PNC. Adapted from the Health Promotion Model (Pender et al., 2002).
11
Literature review. A review of the prominent literature related to the variables in this study and the factors affecting early versus late initiation of PNC in different populations is discussed here. This literature review includes literature published internationally, literature from Mexico, and a synthesis of barriers and motivating factors affecting PNC behavior. There is one study that is review than is a validating model to predict PNC utilization. As a factor determining initiation of prenatal care, prior experience to seek PNC in a health center has been less reported. In a study carried out in middle to upper class Midwestern, US community, Roberts et al. (1998) noted that women 35 years of age and above with prior pregnancy experience appeared to place slightly less importance on PNC than women without previous pregnancy. Authors mention that older women, with more pregnancy experience, may feel they need less medical attention during pregnancy since they learned a great deal during their previous experience. Nevertheless, the authors concluded that they can not explain this behavior through this study. Another study reports that women with a prior experience-behavior of not enrolling in PNC and an associated history of family dysfunction tended to repeat the behavior of no PNC (Tyson et al., 1999). Bloom et al. (2004) applied the Melnyks Barriers Scale in a population of homeless, pregnant women where 91.5% of the group declared to have been a victim of physical violence during the past year. The authors found that 75.61% of the sample study perceived barriers to initiation of PNC. Such barriers being factors related to accessibility to PNC, followed by problems of health provider/patient relationships, inconvenient, fear, and cost. The number of children living with the woman and the perception that this made prenatal care an inconvenience was significant as a barrier, mainly because they had no one to take care of the children during their PNC appointment. Fuller and Gallagher (1999) studied a sample of low income pregnant women in Northeastern Pennsylvania where the most reported barrier was displeasure with having to undergo pelvic exam and blood tests,
12
followed by problems concerning payment and transportation to and from the health center for their prenatal appointment. Cook et al. (1999) designed a study to determine which social, environmental, and psychological barriers were most likely to interfere with the early and regular use of prenatal health services in a population of low-income adult women hospitalized on postpartum unit of a large urban medical center of US. The authors reported eleven significant barriers to receiving inadequate PNC such as: being depressed or unhappy about pregnancy, too tired, too many personal problems took priority, clinic too crowded, clinic too far away, didnt know if wanted the baby, didnt want family or friend to know was pregnant, people in personal life wouldnt help get to clinic, being homeless, embarrassed about pregnancy and didnt like kind of care received at clinic. They also went on to say that a woman, who does not want her family to be informed of the pregnancy, is nearly five times more likely to receive inadequate PNC than a woman without this problem. Women who lacked the support of family and friends for transportation to the clinic were three times more likely to get inadequate PNC, women with personal problems were four times more likely to receive inadequate PNC, and those who had received uncomplimentary information about the care at the clinic delayed their PNC visit. A 2003 study by Johnson et al. involving African American women in Washington, D.C reported that variables contributing to late PNC initiation included maternal age, unemployment, consideration of abortion, lack of money to pay for PNC, and no motivation to learn how to protect ones health. In the multivariate analysis of association of factors for PNC initiation, the authors reported that those who could not afford a consultation, or were considering abortion, were less likely to initiate early prenatal care and the most frequently reported reason for late prenatal care was due to indecisiveness while considering termination of pregnancy. In this sample 75.1% of the women that initiated early PNC did not consider abortion; on the other hand 53.3% of the ones that initiated late PNC were
13
considering it. Finally, the authors conclude that psychosocial barriers occur more frequently than structural barriers. Byrd et al. (1996) studied a group of pregnant Latin Americans residing in the US to understand why Hispanic women begin prenatal care in the later stage of pregnancy than non-Hispanic women. Of this group, 71% were Mexican women who identified barriers as long waiting times, embarrassment from the physical examination, and lack of transportation. Moreover, the authors do emphasize that the women were dissatisfied when, after a long waiting period, the doctor spent little or no time with them and offered no time to ask questions. It is suggested that this lack of interaction between doctor and patient is particularly uncomfortable for Hispanic patients who expect to have a more personal relationship and place total confidence in the health care provider. In a qualitative study was described that the experience of pregnant women-health provider may act as a motivator or barrier to PNC and it will depend on credibility, attitude, interaction style, conduct of power, and relationship capability of the health provider (Sword, 2003). Regarding this issue, a study in Mexico of patient satisfaction in PNC clinics for open population got a paradoxical result. On one hand, the treatment received during the visit was evaluated through direct observation reporting that 51.6% of the mothers received inadequate treatment. Moreover, the average waiting period was as long as 106.2 minutes with a range of 60 225.5 minutes. In spite of this, when mothers were asked about satisfaction with the visit, 92.1% said they were satisfied with the visit. The researchers suggest that by declining to declare their dissatisfaction may be related to low socioeconomic status and lack of education, but that a long waiting time may function like a barrier for utilization of the PNC service thus impeding the opportunity to screen for potential complications and diagnose and treat serious pathology (Bronfman-Pertzovsky et al., 2003). The association between PNC initiation and undesired or unplanned pregnancy has been reported as a significant barrier that can predict late start of PNC (Delgado-Rodriguez
14
et al., 1997; Husley, 2001). Another predictor of late start of PNC is domestic violence (Huth-Bocks et al., 2002; McFarlane et al., 1996; Tyson et al., 1999). McFarlane et al. reported that abused women were twice as likely to begin prenatal care during the third trimester, with abuse preceding late entry. In Mexico, there is a 24.5% of violence in pregnancy with a significant tendency towards the emotional type, but the association of violence with late initiation of PNC is not reported (Castro, Peek-Asa & Ruiz, 2003). Valdez-Santiago and Sanin-Aguirre (1996) studied a sample of pregnant women of Morelos-Mexico; they reported that the lack of PNC increased significant in the group of pregnant women that reported domestic violence. Finally, the consumption of illicit substances such as alcohol and drugs has been reported as a barrier of PNC initiation in a qualitative study done by Jessup, Humphreys, Brindis & Lee (2003). This study used the Mandelbaum Model as its conceptual framework to describe dimensions, turning, adaptation of the participants and mentioned that the majority of the pregnant women sought prenatal care but identified fear of punitive action from the health care facility and/or health care provider as a major barrier. Another study explored the role of maternal drug use and the timing of PNC and estimated that after adjusting for age, race/ethnicity, education, parity, and attitude toward pregnancy, cocaine use was strongly associated with timing of PNC (Brady, Visscher, Feder & Burns, 2003). Motivators for early PNC initiation have been less reported in the literature. Johnson et al. (2003) identified two variables that predicted the early initiation of PNC: encouragement to enter PNC by family members, and provision of child care by family members and friends. Other authors showed that some socio-demographic variables, such as being 24 years of age and older with health insurance, with a planned pregnancy were associated with early initiation of PNC (Byrd et al., 1996; Fuller et al., 1999). Those who planned pregnancy were eager to learn the stages of development corresponding to
15
gestational age, adopt healthy habits, wanted benefits for the baby, and learn about labor and delivery increasing the likelihood of early prenatal care. Social support, reported by Erci (2003) in a sample study in Turkey, by family members or employers for a woman who desires pregnancy, was a significant incentive for early initiation of prenatal care. They found that maternal social support protects against the effects of violence for several health outcomes (Huth-Bocks et al., 20020) and a clear identification of specific sources of support has been related to positive pregnancy outcome for low income black women (Norbeck & Anderson, 1989). Few published studies in Mexico mention motivators of early PNC initiation. Some of the psychosocial variables reported are employment, possessing a basic knowledge of pregnancy and possible complications, being pregnant for the first time, and being attended to by the same health care provider in the medical facility for the entire pregnancy (Frank et al., 2003; Martinez-Gonzalez et al., 1996). Sword (2003) studies a sample of women in Canada, where a universal health insurance system affords financial access to prenatal care. Still, women of low income seek medical later in pregnancy and attend fewer visit than do women of median and high income. Through a qualitative approach this author provides a theoretical explanation that deciding whether to access prenatal care is based in women weigh the pros and cons of the behavior, and then take charge, ultimately making a decision in terms of its meaning for self. Others authors (Campbell, Mitchell, Stanford & Ewigman, 1995) proposed a model to predict prenatal care utilization centering in the concept of a social pregnancy identify. The results confirmed the following dimensions: awareness of pregnancy, acceptance of pregnancy, self-care, communication with family, communication with partner, social attitudes toward prenatal care, and attitudes toward the health care provider. The model has the potential for predicting the utilization of PNC, but explores only nonstructural barriers.
16
The results also suggest that a womans relationship with her prenatal care provider is important to obtaining adequate PNC. After reviewing the literature related to the chosen theme, it is evident that there are many publications identifying barriers to early prenatal care in low socioeconomic American population but there seems to be a lack of studies identifying the motivators of early prenatal care initiation. This may be due to researchers being more interested in identifying obstacles to behavior to assist in the development of intervention programs for groups at risk. As a synthesis, the most significant barriers throughout the cited literature are: the unplanned or undesired pregnancy, transportation problems, prolonged wait time, low educational level, and negative attitude over the pregnancy and PNC. From these barriers the probability to initiate a late PNC increased when the pregnancy was not desired, did not want others to know of the pregnancy, considering abortion, and having family and personal problems. Of the studies reviewed, none describes the utilization of one nursing theoretical model as a guide for its study. Motivators of early PNC initiation are: the perception of benefits for the baby, the pregnancy desired, to be between 24 and 35 years old, to get structural as emotional family support. The behavior that greater predicted the early initiation of PNC was family support. A lack of scientific literature relating to this issue is found throughout the Mexican population, and it can not be inferred that factors affecting PNC initiation in U.S and Canada population will correlate to Mexico where there is a totally different context, especially because the cultural, contextual and income characteristics vary enormously among these countries.
17
Hypothesis: H1. The perceived barriers and benefits of prenatal care are related to the prior pregnancy related experience, demographic factors, psychological factors (stress, depression), sociocultural factors (domestic violence) and interpersonal influences (social support) of the pregnant women. H2. Prenatal care initiation is related to the prior pregnancy related experience, demographic factors, psychological factors, sociocultural factors, interpersonal influences, perceived benefits and perceived barriers of the pregnant woman. H3. A direct relationship exists between sociocultural factors and initiation of prenatal care.
18
Chapter II Method
This chapter reveals the methodological aspects and the research design of the present proposal. It includes the population description, type of sampling, selection of sample and inclusion criteria of the subjects. A description of the instruments selected for this study is reviewed and how they were adapted for this project. The data collection procedure is explained, identifying how prospective participants are selected, as well as a time-line for the study. A description of ethical considerations and statistical analyses that are proposed will follow and the result of the pilot test are described.
Research Design The design of the study is descriptive-correlational-predictive. A descriptive analysis and the synthesis of variables will be carried out through averages and percentages to identify the characteristics of the study group. Correlation between the predictive variables with the outcome variable of time of initiation of PNC will be obtained. Prediction of the outcome variable will be performed through the different proposed variables of this study. Within the descriptive correlational design, a predictive design is developed to predict the value of one variable on the basis of values obtained from other variables. Prediction is one approach to examining causal relationship and to predict the level of the dependent variable (DV) from the independent variables (IVs) (Burns & Grove, 2001; Polit & Hungler, 1999). For this study initiation of PNC is the dependent variable (DV), and the explicative factors of the model than determine the initiation of PNC are the independent variables (IVs).
19
Population, sampling and sample The target populations to participate in this study are pregnant women that belong to the open health system. The investigator will focus this study to women that belong to the open health system because they are at high risk of late PNC initiation as have been reported by the Institute of Statistics of Mexico (INEGI, 2000), and is the target population for later nursing interventions. The open health system population is the one that do not have health insurance and it has been estimated that from 53 millions women that Mexico will have for the year 2006, an average of 29 millions will not have health insurance (Health Secretary of Mexico, 2000). The University Hospital Dr. Jose Eleuterio Gonzalez will be the place where the sample will be collected because is a hospital that has a PNC clinic that attends a great number of the Monterrey, Mexico population. Through personal interview with the Chief of Nursing in the Obstetrics Unit of the University Hospital (P., Rodriguez, personal communication, November 26, 2004), it is known that this hospital has a exclusive PNC clinic for open system population. This clinic is open from Monday to Friday from 8 BM to 2 AM, with and average of 7 visits of pregnant than are initiating PNC and 20 than are already involve in PNC. Because the study phenomenon is the initiation of PNC and in this target population is a homogeneous behavior, since they are all in PNC, a convenient sample will be gathered that meets the sampling criteria and that voluntary accept to participate in the study. The sample size was calculated using a power statistical program nQuery Advisor, version 4. The sample estimated for logistic regression power analysis was obtained: for a power of .96, Odds Ratio = 2.0, R Squared = .3 and Alpha = .05. Where the power is the probability of rejecting a false null hypothesis and it should be close to one; Odd Ratio is the R2 achieved to multivariate correlation coefficient with including covariable in the
20
model; and Alpha is the probability of rejecting a true null hypothesis (Polit, 1996; Polit & Hungler, 2000). The result was a sample size of 270 subjects.
Sampling Criteria The following sampling criteria were selected considered the elimination of sample biases. To be eligible for the study women need to be a) pregnant women in the first visit of PNC in the Clinic of the University Hospital Dr. Jose Eleuterio Gonzalez, b) belong to the open health system, and c) understand and speak Spanish. The sampling criteria will be verified before to invite her to voluntary participate in the study.
Instruments There is not instrument with accepted reliability and validity in Mexico that approach the phenomenon of PNC initiation as a whole, and less that are congruent with the Health Promotion Model that is guiding this research. For this reason, the instruments that will be used in this study were adapted from Barriers, Motivators and Facilitators of Prenatal Care Utilization in Washington, DC (BMFPNC) (Johnson et al., 2003), and the Woman Sexual Abuse Screen (WAS) (Champion, 2001). The instruments were provided by their authors in their original English version. The first step adapting the instruments to the Mexican population was translation into Spanish. The English version was given to two bilingual professionals with broad and recognized experience in working in health science translations. Once the translation was completed, the second step was a review of the instruments content by experts in this field. Subsequently, a group of expert nurses in prenatal care and the main investigator carried out the review of the content of the instruments to ensure the questionnaire included all the major elements relevant to the construct being measured for the study, and its congruence with the HPM theoretical framework.
21
The questionnaire BMFPNC (Jonhson et al., 2003) had questions that differ from the objective of this study. These questions were a list of structural motivators than were offer to the pregnant women and she was asked if this thing will improve her initiation of PNC. Because these are question than measure the commitment to action of an unreal situation, these questions were removed. The group that reviews the instrument added four new questions to achieve the gathering of information more complete about three variables. Two questions were added to the variable prior experience and were: did any of your children need a hospitalization after born?, and in how many of your pregnancy you seek PNC before 6 month the child was born?; the other two questions were one barrier: you were too busy with some responsibility and you can not go to PNC?; and one was a social support: did you get help to pay PNC?. To achieve coherence with the HPM, it was necessary to categorize the information in a new instrument which name in Spanish is Cuestionario de Motivadores y Barreras del Control Prenatal. The word facilitator was deleted because the items pertaining to facilitators were removed. Description of the new questionnaire is as follow: a) socio-demographic information contains 10 questions about socio demographic and economic aspects of the subject and correspond to the variable of personal characteristics; b) reproductive history contains 18 questions about antecedents of previous pregnancies and correspond to the variable of prior experience; c) current pregnancy information contains nine questions about the present pregnancy including a section of psychological factors with seven questions on stress and depression; d) motivators and barriers of prenatal care is divided into six questions on personal benefits, four questions on structural benefits, ten questions on negative attitude to pregnancy and prenatal care, ten questions on personal barriers and ten questions related to structural barriers; e) information on behavior factors contains three questions on the use of
22
alcohol, cigarette and drugs; f) social support contains seven questions about sources and type of support (Appendix B). The questionnaire answers are dichotomous with yes = 1, or no = 0. Each category or subscale have a score than is achieved adding all the affirmative answers and the higher the score the higher the presence of the variable. The subscale of stress and depression the highest score is seven points; in the subscale of motivators the highest score is 10 points; in the subscale of barriers the highest score is 30 points; and in the subscale of social support the highest score is seven points. The Women Abuse Screen (Champion, 2001) had the same process of adaptation review for the BMFPNC. The WAS keeps all the questions and was necessary to add one item: make you feel afraid to say your thought because someone gets angry? The instrument in Spanish was named Cuestionario de Abuso de la Mujer. This instrument has nine questions asking about the experience of violence in her current relationship or a past relationship with either the current partner or a different partner. The questions are classified as: a) four questions of psychological violence, b) two questions of physical violence and c) three questions of sexual violence (Appendix C). The answers are dichotomous with yes = 1 and no = 0, and the highest score is nine points, indicating that has a high level of violence.
Data Collection Recruitment will be carried out among the pregnant visiting the prenatal clinic of the University Hospital Dr. Jose Eleuterio Gonzalez, with astimation time of 3 to 4 months to recruit all the sample size. Each day the research will identified eligible subject through the appointment list of women to pursue PNC. The eligible women will be approach in the waiting room of the clinic by the research and asked if they want to voluntary participate in the study. The details of the study will be explained in lay terms to women who are willing
23
to participate. Those women who agree to be interviewed will receive the informed consent to get them signatures. All the study data will be collected by the main researcher. Women will be interviewed to obtain information on demographic background; psychological factors; sociocultural influences; reproductive history; actual pregnancy; motivators and barriers of PNC; substance use; and social support. The instruments will be applied in the following order: first, Questionnaire of Determinants of Prenatal Care, and second, Questionnaire of Domestic Violence. As the questions are read to the participant by the interviewer, the participant will be able to follow the questions on cards provided to her to use as a guide (Appendix D). After each question the woman will answer aloud and the interviewer will write the answer in the questionnaire. The average time calculated to complete the interview according to pilot test is 30 minutes by each subject. Upon completion of the interview, the researcher will express appreciation for the time and effort contributed by the participant. Responses will be recorded on a worksheet developed by the researcher and entered into the Statistical Program for the Social Sciences (SPSS) for data storage and analyses. All data entry will be performed by the main researcher and stored in a secure area. No one but the researcher will have access to these files to ensure confidentiality and anonymity.
Ethics Considerations This study will adhere to the requirements of the General Law and Regulation about Health Research stipulated in Chapter 1 of this regulation (Secretary of Health, 1987). Before being applied, the instruments will be submitted for approval to the Commission of Ethics and Research of the Nursing Faculty of the University Autonomous of Nuevo Leon and the Ethic Board of the University Hospital. Informed consent will be obtained in accordance with guidelines outlined in Article 21 and will be read aloud and presented in writing as stipulated in Article 14, clause V
24
(Appendix D). Without exception, the signature of every participant on the informed consent must be collected prior to the start of the interview. This research, according to the Article 17, clause 1, is considered to be of minimal risk due to the sensitive nature of the Questionnaire of Domestic Violence and possible repercussions to her and those people around her. For this reason, to assure the appropriate handling of the participant that may reveal domestic violence, the researcher has consulted with the Chief of Nursing in the Obstetrics Unit of the University Hospital, who has explained that University Hospitals protocol agree with the Official Mexican Norm , Rule for the health attention of the domestic violence (Secretary of Health, 1999). One important step to manage domestic violence requires the abused woman to report acts of violence to the physician providing prenatal care and the social worker of the institution. The researcher has guaranteed that any participant who reports domestic violence will be referred to appropriate legal and psychological professionals per the institutions protocol for domestic violence management.
Statistic Analysis This time of initiation of PNC will allow to development two variables. In one hand will be used as a continue variable and will be the real time when the women initiated PNC; this variable will be name time of PNC. On the other hand, the gestational week in which the PNC was initiated will be used to develop a dichotomous variable for timing of PNC initiation. Women who had their first PNC visit prior or at their 12th week of gestational will be classified as having early PNC initiation, while those who stared after their 12th week of gestation will be classified as late PNC initiation. The development of the dichotomous variable for timing of PNC utilization was conducted fallowing the Mexican Norm for PNC utilization (Secretary of Health of Mexico, 1993).
25
The data will be processed through the computer statistic package SPSS (Statistic Package for the Social Sciences) version 12. The statistical analysis process will be performed in three stages. The first stage will be an exploratory step, where the prevalence of the prior experience of prenatal care, demographic factors, psychological factors, sociocultural factors, barriers of prenatal care, motivators of prenatal care and interpersonal influences will be examined. To achieve this, descriptive and inferential statistics will be performed to calculate the frequencies, proportions, central tendency measures and variance measures. The test of Kolmogorov-Smirnov will be performing to estimate is the sample has a normal distribution or a distribution-free, and depending of this will be used parametric or nonparametric test. Bivariate correlation will be used to investigate associations between time of initiation of PNC (continue variable) and all the variables such as the prior experience of prenatal care, demographic factors, psychological factors, sociocultural factors, motivators of PNC, barriers of PNC and interpersonal influence. The second stage a multiple lineal regressions will be utilized to observe the stronger predictor between prior experience of prenatal care, demographic factors, psychological factors, sociocultural factors and interpersonal influences with perception of motivators and barriers of prenatal care (hypothesis 1). In the third phase the multivariate relationship will be investigated using binary logistic regression. This statistical analysis will estimate the maximum probability occurrence of the categorical dependent variable of early initiation of PNC versus late initiation of PNC relating to the multiple independent variables of the model (hypothesis 2). A prediction model will be developed for early start of PNC and for late start of PNC. Domestic violence will be tested as a direct predictor of the late start of the PNC with analysis of binary logistic regression (hypothesis 3).
Preliminary study
26
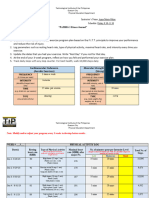
A preliminary study was conducted with a sample of minority pregnant women during January 2005. The convenience sample was recruited at 4 PNC facilities of the University of Nuevo Leon located in Monterrey-Mexico. For the women, the criteria for participation were the same than for the present proposal study. At each facility, women were approached in the waiting room by the research and screened to determinate if they met the criteria for participation. The details of the preliminary study were explained in lay terms to eligible women, who were then asked if they were willing to participate. Using these procedures the 97% (N = 34) of the women eligible to participate were recruited. Every woman singed an informed consent and to assure the confidentiality the interview were carried out in a closed private place. All the interviews were performed by the research and first the Determinant of Prenatal Care Questionnaires was applied, followed by the Domestic Violence Questionnaire. The average time for interview was 30 minutes with range between 20 to 40 minutes. The demographic characteristics of the participants were: 61.8% were older than 18 years old; 61.8% were never married; 79.4% had below High School; 91.2% were not employed outside home; 88.2% live with the partner; 52.9% live with more than 5 people at home; 61.8% had monthly income less than $ 4,000 Mexican pesos; 50% were the first pregnancy; and 44.1% initiate early PNC (Table 1).
Table 1 General characteristics of the participants Characteristics % (n = 34) Age (years) 18 38.2 % > 18 61.8 % Marriage status % early PNC 46.2 % 42.9 %
27
Single Married Study level Less that High school High school or more Work out home Yes No First pregnancy Yes No Live with partner Yes No Early initiation PNC Yes No
61.8 % 38.2 %
38.1 % 53.8 %
79.4 % 20.6 %
44.4 % 42.9 %
8.8 % 91.2 %
41.9 % 66.7 %
50 % 50 %
52.9 % 35.3 %
88.2 % 11.8 %
50.0 % 0.0 %
44.1 % 55.9 %
-------
The third phase was to test the instrument through a preliminary study that was preformed in a sample (n: 34) with similar characteristics to the population in the proposed research study. The internal consistency was calculated through the computer statistical program SPSS (Statistic Package for the Social Sciences) version 12, with the test of reliability of 20 Kuder-Richardson (KR-20) because the answers of the questionnaire are dichotomous (Burn & Grove, 2001; Polit & Hungler, 1999). The reliability coefficient for categories was as follows: subscale of stress and depression, alpha .84; subscale of motivators of prenatal care, alpha .72; subscale of barriers of prenatal care, alpha .76; subscale of social support, alpha .73. The Questionnaire of Domestic Violence obtained an alpha .75. The result of the test of Kolmogorov-Smirnov to see normality showed that the sample had a distribution-free, and a nonparametric statistic analysis was performed. Any of the demographics characteristics had significance correlation with early initiation of PNC. The
28
correlation matrix of the subscales with the variable time of initiation of PNC showed that gestational age of initiation of PNC had an inverse association with perception of motivators (r = -.27) and with social support (r = -.32), being statistic significant (p < .05). A positive and significant association (p < .01) obtain the time of PNC with perception of barriers (r = .76) and the perception of stress and depression during pregnancy (r = .66) (Table 2).
Table 2 Intercorelations between subscales and time of PNC initiation Variables 1. Time of PNC initiation 2. Total Motivators 3. Total Barriers 4. Stress and depress 5. Social support 6. Total Domestic violence 1.00 -.27 1.00 .76** -.42* 1.00 .66** -.41* .82** 1.00 -.32 .05 -.31 -.36* 1.00 .11 -.18 .08 .20 -.30 1.00 1 2 3 4 5 6
** p < .01. * p < .05
Table 2 show the positive relationship and statistic significant (p < .01) between the perception of barriers and the perception of stress and depress. To graphic the relation of these two variables together a scatter plot is show in Figure 3, that is showing the positive associations of this two variables and when the perception of barriers increase, the stress and depression increase also; and both increase the late initiation of prenatal care.
29
14 12
10 8
total barreras
0 -2 -1 0 1 2 3 4 5 6 7
estres y depresion
Figure 3. Relationship between perception of barriers and perception of stress and depression than affect the early initiation of PNC.
A linear regression analysis was performed to predict which variables influent the perception of motivators and barriers. Both regression models used the same predictor variables as level of income, first pregnancy, marriage, educational level, work out of home, number of people living with her at home, total subscale stress and depression, total subscale social support, and total subscale of domestic violence. The regression model for motivators explain the 65% of the variable (R = .81) and was significant (p < .01). The model for barriers explain the 69% of the variable (R = .83) and was significant (p < .01).
30
These model show than both motivators and barriers are significant influenced by stress and depression (p < .01) (Table 3).
Table 3 Models of multiple regression of motivators and barriers through 11 predictors (n = 33) Motivators Variable Actual age Married Live with partner Total people home Educational level Work out home First pregnancy Total social support Total violence domestic Level income stress and depression -.28 -.18 .40 ** -.08 .16 -.08 .25 .23 -.26 .14 -.67** r -.32 -.29 .23 .11 .16 -.16 -.03 -.10 -.12 -.01 -.60** .15 -.20 -.46*** .29* -.16 -.11 -.06 -.34* .11 -.31 .79*** r Barriers .30 -.14 -.06 -.07 -.22 -.14 .17 .00 -.06 -.05 .78***
R2 R2 adjusted F (11, 21)
.66 .48 3.65***
.69 .53 4.26***
31
* p < .05 ** p < .01 *** p < .005
Logistic regression analysis was used to estimate the likelihood to initiate an early PNC. Some of the variables were not considerate because the sample size was not big enough (n = 33) to perform this analysis with all the predictor variables. Only six of the variables were used in the model to predict the behavior. As show Table 4 the prediction model was statistical significant (model X2 =32.45, p <.00005).
Table 4 Model of prediction of early PNC initiation Variables Predictoras Total motivators Total Barriers Stress and Depression Social support Violence Domestic Age of mother Constant b -1.87 -3.52 -.07 -.44 -1.06 -.09 31.52 Wald 2.31 3.90* .00 .60 1.69 .23 2.88 Odd ratio .15 .02 .92 .63 .34 .91
-2 Log likelihood Model Chi-square (df = 6) p Overall rate of correct classification
12.535 32.45 .0000 57.58%
Unstandardized logistic regression coefficients.
*p < .05
32
The predictor variable of barriers was statistic significant (p <.05) associated with an inverse probability of early initiation of PNC. The Figure 4 shows how the probability to initiate early PNC has an important decrease when are present two to four barriers.
1.0
.8
.6
.4
Predicted Value
.2
0.0
-.2 -2 0 2 4 6 8 10 12 14
total barreras
Figure 4. Predicted value of barriers in the behavior of early PNC initiation.
With this preliminary study was tested the questionnaires of the present proposal study, and the reliability that was gotten is adequate for each subscale. Moreover, the result of the proposal model of prediction of PNC initiation shows that the perceived barriers are the stronger predictors of the behaviors. Due to the sample size, the entire model was not tested. This analysis will be performed with the final proposal study and will allow explaining the behaviors of initiation of PNC.
33
References
Bloom, K.C., Bednarzyk, M.S., Devitt, D.L., Renault, R.A., Teaman, V. & Van Loock, D. (2004). Barriers to prenatal care for homeless pregnant women. Journal of Ginecologies and Neonatal Nursing, 33(4), 428-435. Brady, T.M., Visscher, W., Feder, M. & Burns, A.M. (2003). Maternal drug use and the timing of prenatal care. Journal of Health Care for the Poor and Underserved, 14(4), 588. Bronfman-Pertzovsky, M.N., Lpez-Moreno, S., Magis-Rodrguez, C., Moreno-Altamirano, A. & Rutstein, R. (2003). Atencin prenatal en el primer nivel de atencin: caractersticas de los proveedores que influye en la satisfaccin de las usuarias. Revista de Salud Pblica de Mxico, 45(6), 445-454. Burns, N., & Grove, S. (2001). Selecting a research design. In N. Burns & S. Grove (Eds). The practice of nursing research: Conduct, critique, and utilization (pp. 247, 286). Philadelphia, Pennsylvania, USA: W.B. Saunders Company.
34
Byrd, T.L., Muller, P.D., Selwyn, B.J. & Lorimor, R. (1996). Initiation of prenatal care by low-income Hispanic women in Houston. Public Health Reports, 111(6), 536-540. Castro, R., Peek-Asa, C. & Ruiz, A. (2003). Violence against women in Mexico: A study of abuse before and during pregnancy. American Journal of Public Health, 93(7), 1110-1116. Comisin Nacional Para la Prevencin y Control del SIDA, (2000). Gua para el Manejo de la Mujer Embarazada con Infeccin por VIH. (3ra. ed. ISBN 968-811-921-0) Distrito Federal, Mxico.: Autor. Cook, C.A., Seling, K.L., Wedge, B.J. & Gohn-Baube, E.A. (1999). Access barriers and the use of prenatal care by low-income, inner-city women. Social Work, 44(2), 129-139. Champion, J. D. (2001). Women Sexual Abuse Screen. The University of Texas, Health Science Center, Tx, USA.: Autor. Delgado-Rodrguez, M., Gmez-Olmedo, M., Bueno-Cavanillas, A. & Glvez-Vargas, R. (1997). Unplanned pregnancy as a major determinant in inadequate use of prenatal care. Journal of Preventive Medicine, 26(6), 834-838. Erci, B. (2003). Barriers to utilization of prenatal care service in Turkey. Journal of Nursing Scholarship, 35(3), 269-273. El-Mohandes, A., Herman, A.A., El-Khorazaty, M.N., Katta, P.S., White, D. & Grylack, L. (2003). Prenatal care reduce the impact of illicit drug use on perinatal outcome. Journal of Perinatology, 23, 354-360. Frank, R., Pelcastre, B., Salgado de Snyder, N., Frisbie, P.W., Potter, J.E. & BronfmanPertzovsky, M.N. (2004). Low birth weight in Mexico: New evidence from a multisite postpartum hospital survey. Revista de Salud Pblica de Mxico, 46 (1), 1-9.
35
Fuller, Ch.A. & Gallegher, R. (1999). Whats happening, perceived benefits and barriers of prenatal care in low income women. Journal of the American Academy of Nurse Practitioners, 11(12), 527-532. Hulsey, T.M. (2001). Association between early prenatal care and mothers intention of and desire for the pregnancy. Journal of Ginecologies and Neonatal Nursing, 30(3), 275282. Huth-Bocks, A., Levendosky, A. & Bogat, A. (2002). The effects of domestic violence during pregnancy on maternal and infant health. Violence and Victims, 17(2), 169. Instituto Nacional de Estadstica Geogrfica e Informtica, (2000). Consultas a embarazadas por trimestres y tipo de consulta. Cobertura nacional. Tipo de consulta: primera vez. Recuperado el 24 de septiembre de 2004, de http://dgcnesyp.inegi.gob.mx/cgiwin/sisesim.exe/Consultar Instituto Nacional de Estadstica Geogrfica e Informtica, (2003). Estadsticas Demogrficas del 2002. (Ed. 2003, cuaderno Nmero 15, cuadros 2.21, 4.13.4, 4.13.9 y 4.13.12). Mxico.: Autor. Jessup, M.A., Humphreys, J.C., Brindis, C.D. & Lee, K.A. (2003). Extrinsic barriers to substance abuse treatment among pregnant drug dependent women. Journal of Drug Issues, 33(2), 285-304. Jonhson, A.A., El-Khorazaty, M.N., Hatcher, B.J., Wingrove, B.K., Milligan, R., Harris, C. & Richards, L. (2003). Determinants of late prenatal care initiation by African American women in Washington, D.C. Maternal and child health journal, 7(2), 103114. Levine, G. (2001). Pregnancy and substance abuse. Breaking down the barriers to prenatal care. The Professional Medical Assistant, 34(4), 19-23.
36
Kiely, J. & Kogan, M. (2001). Reproductive health of women: Prenatal care. From data to action. Centers for Disease Control and Prevention, public health surveillance for women infant and children. Hyattsville, Maryland. USA. Kogan, M.D., Alexander, G.R., Jack, B.W. & Allen, M.C. (1998). The association between adequacy of prenatal care utilization and subsequent pediatric care utilization in the United State. Apediatrics. 102(1), 25-30. Martnez-Gonzlez, L., Reyes-Frausto, S. & Garca-Pea, M. (1996). Utilizacin adecuada de la atencin prenatal en el Instituto Mexicano del Seguro Social. Revista de Salud Pblica de Mxico, 38(5), 341-351. McFarlane, J., Parker, B. & Soeken, K. (1996). Abuse during pregnancy: Associations with maternal health and infant birth weight. Nursing Research. 45(1), 37-42. Michigan Department of Community Health. (2004). Pregnancy Risk Assessment Monitoring System Delivery. Prenatal care in Michigan, 3(3), 1-4. Norbeck & Anderson, (1989) Organizacin Mundial de la Salud (1994). Declaracin de Eliminacin de Violencia en contra de la Mujer. New York, United Nations, (Resolution No. A/RES/48/104). Recuperado el 9 de Marzo de 2004, de http://www.who.int/violence_injury_prevention/injury/ definitions/def20/en/print.html. Organizacin Mundial de la Salud (2003). Nuevo modelo de control prenatal de la OMS: Las mejores prcticas en salud reproductiva. (1era. Ed.) [Folleto]. Ginebra, Suiza.: Autor. Pender, N., Murdaugh, C. & Parsons, M. (2002). The health promotion model. In N. Pender, C. Murdaugh & M. Parsons. Health Promotion in Nursing Practice (pp. 5978). New Jersey, USA: Upper Saddle River.
37
Polit, D.F. & Hungler, B.P. (1999). Investigacin Cientfica en Ciencias de la Salud (R. Palacios & G. Feher de la Torre, Trads.). Philadelphia. EE.UU.: Lippincott Williams & Wilkins. Programa Nacional de Salud, 2001-2006 (2001). La democratizacin de la salud en Mxico: Hacia un sistema universal de salud (p.90). Mxico D.F., Mxico. Reichman, N.E. & Florio, M.J. (1996). The effects of enriched prenatal care service on Medicaid birth outcomes in New Jersey. Journal of Health Economics. 15(4), 455477. Roberts, R.O., Yawn, B.P., Wickes, S.L., Field, Ch.S., Garretson, M. & Jacobsen, S. (1998). Barriers to prenatal care: factors associated with initiation of care in middle-class Midwestern community. Journal of Family Practice, 47(1), 53-61. Romero-Gutierrez, G., Martinez-Ceja, C., Abrego-Olvira, E. & Ponce-Ponce, A. (2005). Multivariate anlisis of risk factors for stillbirth in Leon, Mexico. Acta Obstretricia et Gynecologica Scandinava, 84, 2-6. Rooks, J.P. (1998). Benefits and limitations of prenatal care. Journal of American Medicine Association, 280(24), 2072. Rosenberg, K.D. (1998). Benefits and limitations of prenatal care. Journal of American Medicine Association, 280(24), 2072. Secretara de Salud (1987). Reglamento de la Ley General de Salud en Materia de Investigacin. Recuperada el 20 de octubre de 2004 en http://www.hgm.salud.gob.mx/servmed/reg_investigacion.pdf. Secretara de Salud (1993). Norma oficial Mexicana Atencin de la mujer durante el embarazo, parto y puerperio y del recin nacido. Criterios y procedimientos para la prestacin del servicio. (NOM-007-SSA2-1993). Mxico.: Autor. Sword, W. (2003). Prenatal care use among women of low income: a matter of Taking care of self. Qualitative health research, 13(3), 319-332.
38
Tyson, H., Higgins, R.D. & Tyson, I. (1999). Family dysfunction and native American women who do not seek prenatal care. Archives of Family Medicine, 8, 111-117. Valdez-Santiago, R. & Sanin-Aguirre, L. (1996). La violencia domestica durante el embarazo y su relacion con el peso al nacer. Revista de Salud Publica de Mexico, 38, 352-362.
Appendix A UNIVERSIDAD AUTNOMA DE NUEVO LEN FACULTAD DE ENFERMERA SUBDIRECCIN DE POSGRADO E INVESTIGACION Determinants of Prenatal Care Questionnaire Now I'm going to ask you a number of questions about your personal history, your pregnancy history, your beliefs about prenatal care, and your feelings about the prenatal care system in the District. Please try to give frank and complete answers to each of the questions you will be asked. Subject id number: Label
Date of interview Start hour interview
End time interview
39
Date first prenatal care visit
Gestational age
PART A:
SOCIO-DEMOGRAPHIC INFORMATION
First I will ask you some questions about general information. A1. What is your actual age? ___ ___ YEARS OLD A2. What is your current marital status? Are you: Currently Married,..............................1 Divorced,............................................2 Widowed,............................................3 Separated,............................................4 Or Have you Never Been Married?.....5 A3. Do you currently live with a partner or husband? YES........................1 NO ........................0 How many people (including yourself) live in your household? __ __ How many of these people are: a) adults over 18 years? b) children under 5 years? c) children aged 5-12 years? d) teenagers aged 13-18 years? e) Total
A4.
A5.
__ __ __ __ __ __ __ __ __ __ NOTE: THIS SHOULD AGREE WITH Q. A4
A6.
What is the highest grade or year in school you have completed? NO SCHOOLING..............00 ELEMENTARY/MIDDLE SCHOOL..01 02 03 04 05 06 07 08 09 HIGH SCHOOL/GED...........10 11 12 UNIVERSITY/COLLEGE........13 14 15 16 17 plus years Are you currently employed outside of the home? YES...........................1 NO.............................0 A7a. Are you employed
A7.
40
part-time or ...................1 full time ? .....................2 A8. Which one is the income at your total household income from all of the sources at your home. Please include your income and the income for all the other people in your household who share expenses. You can tell me either weekly or monthly, which ever is easiest for you. Weekly < 500 500 to 999 1000 to 1499 1500 to 1999 2000 to 2499 2500 or more DONT KNOW REFUSED Every 15 day < 1000 1000 to 1999 2000 to 2999 3000 to 3999 4000 to 4999 5000 or more Monthly < 2000 2000 to 3999 4000 to 5999 6000 to 7999 8000 to 9999 10000 or more
1 2 3 4 5 6 98 99 A9.
How do you pay for prenatal care? NO PAY. ....... ...................... 0 PAY PART COST............... 1 SELF-PAY........................... 2 OTHER .. ......... 3 DONT KNOW............... 98 _______________________________ (SPECIFY) How will you pay for your delivery? NO PAY. ....... ...................... 0 PAY PART COST............... 1 SELF-PAY........................... 2 OTHER .. ......... 3 DONT KNOW................ 98 _______________________________ (SPECIFY)
A10.
PART B.
REPRODUCTIVE HISTORY (Prior experience)
Now, I'd like to ask you a few questions about your past pregnancy history. B1. How old were you when you had your first menstrual period? ___ ___ YEARS OLD
41 98.........DONT KNOW B2. Is your current pregnancy your first? YES....................1 NO.....................0 B3. How old were you when you became pregnant for the very first time? ___ ___ YEARS OLD AT FIRST PREGNANCY B4. Including this pregnancy, how many times have you been pregnant? Please include all pregnancies, that is all those resulting in live births, stillbirths, abortions or miscarriages. ___ ___ TIMES PREGNANT B5. How many babies have you had born alive? ___ ___NUMBER OF BABIES BORN ALIVE 00..NONE B6. How many stillbirths have you had? (A baby born dead after at least 20 weeks). ___ ____NUMBER OF STILLBIRTHS 00......NONE B7. How many miscarriages have you had? (Spontaneous delivery of a baby before 20 weeks, when the baby is born dead). ___ ___NUMBER OF MISCARRIAGES 00 ....NONE B8. How many abortions have you had? (A pregnancy ended by a medical procedure). ___ ___NUMBER OF ABORTIONS 00 ....NONE Have any of your children died within their first year of life? YES....................1 NO.....................0 SKIP TO Q. B10 B9a. How many of your children have died in the first year of life? ___ ___CHILDREN HAVE DIED
B9.
B10.
Have any of your liveborn children weighed less than 2.5 Kg. when they were born?
42
YES....................1 NO.....................0
SKIP TO Q. B11
B10a. How many of your liveborn children weighed less than 2.5 Kg. when they were born? ___ ___CHILDREN B11. Were any of your liveborn children born early (less than 37 weeks gestation)? YES....................1 NO.....................0 SKIP TO Q. B12 B11a. How many of your liveborn children were born early (at less than 37 weeks)? ___ ___CHILDREN B12. How many of your liveborn children are living now? ___ ___LIVEBORN CHILDREN STILL LIVING Did any of your children need a hospitalization after born? YES. 1 NO 0 SKIP TO Q. B14 B13a How many of your babies were hospitalized? ____ ____ NUMBER OF CHILDREN B14. When did your last pregnancy end? Please include any outcome, such as, live birth, stillbirth, abortion or miscarriage. __ __ - __ __ - __ __ DAY MONTH YEAR In how many of yours pregnancy did you get prenatal control at less 6 months before birth? 1. all of them 2. some of them (number..) 3. none of them How many normal delivered have you had? ___ ___ NUMBER OF DELIVERED B17. How many cesarean have you had? ___ ___ NUMBER OF CESAREAN
B13.
B15.
B16.
B18.
Do you have any of these problems during yours pregnancies? 1. Yes 0. No
a) Bleeding before delivered
43
b) Break your bag of waters c) High blood pressure d) Gestational diabetic e) Baby not growing well f) Problem with the baby at delivered g) Baby born with problem h) Infections i) Other
PART C.
CURRENT PREGNANCY INFORMATION
I will now ask you some questions about your current pregnancy. C1. When was your last menstrual period? ___ ___ ___ ___ ___ ___ DAY MONTH DONT KNOW .......98 C2. What is your due date? ___ ___ ___ ___ __ __ __ __ DAY MONTH YEAR DON'T KNOW........98 C3. What made you think you were pregnant? missed period ................ 01 felt sick/upset stomach.. 02 intuition/had a feeling... 03 felt baby move ............ 04 saw spotting.................. 05 felt bloated.................. 06 tender breasts................ 07 felt tired.................... 08 needed to urinate often...... 09 other......................... 10 ____________________________________ (SPECIFY) C4. Did you go to a doctor, clinic or hospital to make sure you were pregnant? YES...................1
YEAR
44
NO....................0 C4a.
SKIP TO Q. C5
Where did you go to make sure you were pregnant? SAME LOCATION AS INTERVIEW....... 1 DIFFERENT PLACE.................. 2 ___________________________________ (SPECIFY)
C5.
How many weeks pregnant were you when you had the pregnancy test done? __ __WEEKS PREGNANT 96..DIDNT GO 98......DONT KNOW
C6.
How many days or weeks was it from the time you first knew you were pregnant until you contacted the clinic or office to make an appointment? __ __DAYS AND __ __WEEKS AND __ __MONTHS OR 97...SAME DAY How many days or weeks was it from the time you made your first prenatal appointment until the actual day of your visit? __ __DAYS __ __WEEKS __ __MONTHS 97...SAME DAY
C7.
AND AND OR C8.
Did you visit an emergency room during this pregnancy for any reason related to your health or pregnancy? YES...................1 NO....................0
SKIP TO Q. C9
C8a. How many times have you gone to an emergency room during this pregnancy? ___ ___ TIMES C9. Have you had or have any of these problems during your current pregnancy? 1. Yes a) Bleeding before delivered b) Break your bag of waters 0. No
45
c) High blood pressure d) Gestational diabetic e) Baby not growing well f) Problem with the baby g) Infections h) Other disease
C10.
PSYCOLOGICAL FACTORS: Please tell me if any of these happened during this pregnancy (Stress and Depression factors). YES NO a) you did not feel well 1 0 b) c) you had family problems you had problems with your husband or boyfriend you had been under stress you were depressed you had personal problems you were not thinking straight 1 0
1 1 1 1 1
0 0 0 0 0
d) e) f) g)
PART D. D1.
MOTIVATORS AND BARRIERS OF PRENATAL CARE
I will now read some reasons why some women start prenatal care. Please tell me whether or not that reason made you start prenatal care. Did you start prenatal care...... YES a) to learn how to protect your health because you were afraid that you would have problems during the pregnancy without prenatal care to talk to someone about your pregnancy 1 NO 0
b)
1 1
0 0
c)
46
d)
to learn better health habits to learn about labor and delivery to have a healthy baby
e)
1 1
0 0
f)
Now I am going to ask you some facilities that you may have to star prenatal care. D2. Can you travel easily to your prenatal care appointments? YES....................1 NO.....................0 D2a. How did you get to this prenatal appointment? WALK.......................................1 BUS...........................................2 CAR...........................................3 TAXI..........................................4 TRAIN/SUBWAY/METRO......5 OTHER......................................6 _______________________________(SPECIFY) How long did it take you to travel to this prenatal appointment? __ __ MINUTES AND __ __ HOURS OR 98.........DONT KNOW
D2b.
D3.
Are the clinic hours convenient for you? YES. 1 NO.. 0 Was it easy to get appointment? YES. 1 NO.. 0 Are the clinic services good for you? YES. 1 NO.. 0 D5a. There is any other service that do you like to get in this clinic? YES 1 NO. 0
D4.
D5.
47
____________________________ (SPECIFY) D5b. There is any other motivation to start prenatal care for you? YES.. 1 __________________(SPECIFY) NO. 0
D6.
Do you have a preference for the sex of your doctor? YES...................1 NO....................0 SKIP TO PART E7 D6a. Which sex would you prefer your doctor to be? MALE...................1 FEMALE...............2 Did you initiate prenatal care late because of the sex of your doctor? YES.. 1 NO 0
D6b.
D7.
Please tell me if these reasons occurred to you during this pregnancy (Negative Attitude toward the pregnancy and PNC). YES NO a) b) you went in late for a pregnancy test you did not think you needed early prenatal care you prefer to go the emergency room when there is a problem you can take care of yourself during pregnancy you get better advice about pregnancy from family and friends you did not want people to know you were pregnant the pregnancy was unplanned you were unhappy about being pregnant you were thinking of having an abortion 1 1 0 0
c)
d)
e)
f)
1 1
0 0
g) h)
i)
48
j)
you forgot the appointment
D8.
The following is a list of personal things that affect women's decisions to start prenatal care. Please tell me if these reasons caused you to start prenatal care later than you intended. Did you start prenatal care later because.... a) you had no money to pay for prenatal care you had no health insurance you did not know you could get help paying for prenatal care you did not know where you could get prenatal care you didn't like the attitudes of the staff you didn't think you could communicate with the staff you were afraid of or did not like medical tests and examinations generally, you do not like health care workers you didnt know you was pregnant you were busy with other responsibilities that you couldnt go to prenatal care YES NO
1 1
0 0
b) c)
d)
e)
f)
g)
h)
1 1
0 0
i) j)
D9.
The following is a list of things that affect women's decisions to start prenatal care. Please tell me if these reasons caused you to start prenatal care later than you intended. Did you start prenatal care later because.... a) you could not get an appointment YES 1 NO 0
49
b)
your appointment was cancelled by the clinic the hours at the clinic are not convenient for you you had to wait too long to get an appointment you had transportation problems you could not get time off from work you have had to wait too long in the waiting room to see your health care provider you were moving a lot you were/are homeless you were afraid of crime near your home or the clinic
c)
d)
1 1 1
0 0 0
e) f) g)
1 1 1
0 0 0
h) i) j)
D10.
There is any other barrier for you to start prenatal care? YES 1 NO. 0 __________________ (SPECIFY)
PART E.
INFORMATION ABOUT BEHAVIORAL FACTORS
The next section addresses some of the lifestyle behaviors that pregnant women may participate in. Your honest answers will help us to design appropriate services based on your needs. The questions apply to your current pregnancy. E1. Please tell me which of the following statements about smoking and pregnancy apply to you? Did not smoke before pregnancy/never smoked............1 Quit smoking but not because of pregnancy..................2 SKIP TO Q. E2 Quit smoking because of pregnancy...............................3
Currently smoke but I cut back because of pregnancy...4 Currently smoke the same as before pregnancy.............5 E1a. How many cigarettes per day do you smoke? __ __ CIGARETTES PER DAY E1b. Did you start prenatal care later because you didn't want others to know you were smoking during your pregnancy? YES....................1 NO.....................0 E2. Now, which of the following statements about alcohol and pregnancy apply to you? Did not drink alcohol before pregnancy/never drank.....1 Stopped drinking but not because of pregnancy.............2 Stopped drinking because of pregnancy.........................3 Currently drink but I cut down because of pregnancy....4 Currently drink the same as before pregnancy...............5
SKIP TO Q. E3
E2a. About how often on average do you drink any kind of alcoholic beverage? Would you say. Daily................................................1 Almost daily 3 to 6 days a week.....2 1 to 2 days a week...........................3 Several times a month.....................4 Monthly or less but at least once.....5 E2b. About how many drinks do you have on those days when you are drinking? Usual number of drinks __ __
E2c. Did you start prenatal care later because you didn't want others to know you were drinking during your pregnancy? YES....................1 NO.....................0 The next questions are about drug use during pregnancy. Please answer these questions honestly, we will not tell anyone about your answers. We are interested in street drugs, those for which you don't have a prescription. E3. Please, which of the following statements about drugs and pregnancy apply to you?
02/08/12 pntal_qx.v7
51 Did not use drugs before pregnancy.......................................1 Stopped using drugs but not because of pregnancy................2 SKIP TO PART F Stopped using drugs because of pregnancy............................3 Currently use drugs but I cut down because of pregnancy.....4 Currently use drugs the same as before pregnancy................ 5 E3a. Do you use... SI 1. Cocaine 2. Crack cocaine 3. Heroin 4. Marijuana 5. Anything else NO E3b. How often do you use... DAILY WEEKLY
MONTHLY
E3c.
Did you start prenatal care later because you didn't want others to know you were using drugs during your pregnancy? YES....................1 NO.....................0
PART F.
SOCIAL SUPPORT (Interpersonal Influences)
I am going to read a list of things that women have told us make it easier for them to start prenatal care. Please tell me whether or not each one made it easier for you to start prenatal care. Was it easier for you to start prenatal care because..... F1. Someone encouraged you to seek prenatal care? YES 1 NO. 0 F1a Who encouraged you more? Someone from your family 1 Your husband or partner. 2 Your friends 3 Your health care or social worker 4 Other person. 5 Someone help you with transportation. YES.. NO 1 0
_____________(SPECIFY)
F2.
52 F2a. Who helped you more with transportation? Someone from your family 1 Your husband or partner. 2 Your friends 3 Your health care or social worker 4 Other person. 5 _____________(SPECIFY)
F3.
Someone come with you to the appointment? YES.. NO F3a. 1 0
Who comes with you? Someone from your family Your husband or partner. Your friends Your health care or social worker Other person.
1 2 3 4 5
_____________(SPECIFY)
F4.
Did you get help with child care? YES. NO.. NOT APPLY.. F4a. 1 0 00
Who helps you with child care? Someone from your family Your husband or partner. Your friends Your health care or social worker Other person.
1 2 3 4 5
_____________(SPECIFY)
F5.
Did you get help with cost of visit? YES. NO.. 1 0
F4a. Who helps you to pay the visit? Someone from your family Your husband or partner. Your friends Your health care or social worker Other person.
1 2 3 4 5
_____________(SPECIFY)
53 F6. Has someone had given you information on why to go to prenatal care and how to care in this pregnancy? YES...........1 NO............0
SKIP TO Q. F7
F6a. Tell me who has given you the most important information about this pregnancy? Someone from your family 1 Your husband or partner. 2 Your friends 3 Your health care or social worker 4 Other person. 5 _____________(SPECIFY) F7. Do you have anyone to turn to in times of emotional need? YES...................1 NO....................0 F7a. Who can you turn to most often? Someone from your family Your husband or partner. Your friends Your health care or social worker Other person. 1 2 3 4 5
_____________(SPECIFY)
Appendix B UNIVERSIDAD AUTONOMA DE NUEVO LEON FACULTAD DE ENFERMERA SUBDIRECCIN DE POSGRADO E INVESTIGACION Woman Abuse Questionnaire A lot of women have had bad problems with men; some are even badly hurt, or killed. Please tell me if any of these things have happened to you.
54
1.
Has anyone ever constantly criticized or put you down? 1. Yes 0. No a. Who did it? (Check all that apply) 1. Boyfriend/husband 4. Friend/acquaintance 2. Parent 5. Stranger ____________(specify) 3. Relative b. How many times did it happen? 1. Once 2. A few times c. Do this happen now? 1.Yes 0. No
3. Over and over
2. Make you feel afraid to say your thought because someone gets angry. 1. Yes 0. No a. Who did it? (Check all that apply) 1. Boyfriend/husband 2. Parent 3. Relative
4. Friend/acquaintance 5. Stranger ____________(specify)
b. How many times did it happen? 1. Once 2. A few times c. Do this happen now? 1. Yes 0. No
3. Over and over
3. Tried to force you into doing something you didnt want to do, by threatening to hurt you? 1. Yes 0. No a. Who did it? (Check all that apply) 1. Boyfriend/husband 4. Friend/acquaintance 2. Parent 5. Stranger ____________(specify) 3. Relative b. How many times did it happen? 1. Once 2. A few times 3. Over and over c. Do this happen now? 1. Yes 0. No 4. Acted with extreme jealousy, like hes your owner? a. Who did it? (Check all that apply) 1. Boyfriend/husband 2. Parent 3. Relative 1. Yes 0. No
4. Friend/acquaintance 5. Stranger ____________(specify)
b. How many times did it happen? 1. Once 2. A few times
3. Over and over
55 c. Do this happen now? 5. 1.Yes 0. No 1. Yes 0. No
Used a knife, gun or other weapon against you? a. Who did it? (Check all that apply) 1. Boyfriend/husband 2. Parent 3. Relative
4. Friend/acquaintance 5. Stranger ____________(specify)
b. How many times did it happen? 1. Once 2. A few times c. Do this happen now? 6. 1.Yes 0. No
3. Over and over
Forcefully held you down, punched, kicked or tried to choke you? a. Who did it? (Check all that apply) 1. Boyfriend/husband 2. Parent 3. Relative
1. Yes 0. No
4. Friend/acquaintance 5. Stranger ____________(specify)
b. How many times did it happen? 1. Once 2. A few times c. Do this happen now? 7. 1. Yes
3. Over and over 0. No 1. Yes 0. No
Made you have sex when you didnt want to? a. Who did it? (Check all that apply) 1. Boyfriend/husband 2. Parent 3. Relative
4. Friend/acquaintance 5. Stranger ____________(specify)
b. How many times did it happen? 1. Once 2. A few times c. Do this happen now? 8. 1. Yes
3. Over and over 0. No 1. Yes 0. No
Knowingly hurt you physically during sex? a. Who did it? (Check all that apply) 1. Boyfriend/husband 2. Parent 3. Relative
4. Friend/acquaintance 5. Stranger ____________(specify)
b. How many times did it happen? 1. Once 2. A few times
3. Over and over
56
c. Do this happen now? 9.
1. Yes
0. No 1. Yes 0. No
Made you feel afraid to say no to sex? a. Who did it? (Check all that apply) 1. Boyfriend/husband 2. Parent 3. Relative
4. Friend/acquaintance 5. Stranger ____________(specify)
b. How many times did it happen? 1. Once 2. A few times c. Do this happen now? 10. 11. 1. Yes
3. Over and over 0. No
How old were you when this happened for the first time? Age___ When was the last time it happened? 1. 2. 3. 4. During the past week During the past month During the past 3 months During the past 6 months 5. During the past year 6. During the past 2 3 years 7. During the past 5 years 8. Over 5 years ago
12.
(If answered yes to 5, 6 and 7) Did you ever report what happened? 1. Yes 0. No
13. 14.
How old is the person? Age___ (For women under age 18 who said yes to 5, 6 y 7 and it is still happening) Do you want us to guide you to report it? 1. Yes 0. No
WE HAVE ENDED WITH THE QUESTIONNAIRES, THANK YOU FOR YOUR HELP; DO YOU HAVE ANY QUESTION THAT WOULD YOU LIKE TO ASK? Appendix D UNIVERSIDAD AUTNOMA DE NUEVO LEN FACULTAD DE ENFERMERA SUBDIRECCIN DE POSGRADO E INVESTIGACION Informed Consent
57
Study title: Factors than affect prenatal care initiation in Mexico Investigators: Ana Maria Quelopana Ms. Ana Maria Quelopana is studying the factors than affect prenatal care initiation in Mexico. Although the study will not benefit you directly, it will provide important information about barriers and motivators to prenatal care that might enable nurses to identify interventions to promote early initiation of prenatal care. The study has been approved by the appropriate people and review boards at The University of Nuevo Leon and University Hospital. The procedures include responding two questionnaires; the Determinant of prenatal care Questionnaire with question about a) Socio-demographic Information, b) Reproductive History, c) Current pregnancy Information and Psychological Factors, d) Motivators and Barriers of Prenatal Care, e) Information on behavior factors, and f) Social Support. The second questionnaire is the Domestic Violence Questionnaire. To assure confidentiality, the interview will be carried out in a closed private place. The interview in this study will take approximately 30 minutes. You are free to ask any questions about the study and you may call Ms Quelopana at (52 81) 8333 6866. Your participation in this study is voluntary; you are under no obligation to participate. You have the right to withdraw at any time and your relationship with the health provider will not be affected. The study data will be coded so they will not be linked to your name. Your identity will not be revealed while the study is being conducted or when the study is reported or published. All the study data will be collected by Ms. Quelopana, stored in a secure place, and not shared with any person.
I have read this consent form and voluntarily consent to participate in this study.
___________________________ Subjects Signatura
__________________ Date
Você também pode gostar
- 26-82000 Cau Hoi Thi A, B, CDocumento280 páginas26-82000 Cau Hoi Thi A, B, CngotrancheetahAinda não há avaliações
- 70 Test BDocumento503 páginas70 Test BzorrotranAinda não há avaliações
- 70 Test ADocumento439 páginas70 Test AzorrotranAinda não há avaliações
- 1500 Test CDocumento428 páginas1500 Test CngotuannghiaAinda não há avaliações
- Alterations in The Surgical Patient Updated 2010Documento122 páginasAlterations in The Surgical Patient Updated 2010zorrotranAinda não há avaliações
- The Rules of Word StressDocumento1 páginaThe Rules of Word StresszorrotranAinda não há avaliações
- British American ComparisonDocumento93 páginasBritish American ComparisonzorrotranAinda não há avaliações
- Variables in ResearchDocumento30 páginasVariables in Researchzorrotran100% (2)
- RootDocumento2 páginasRootzorrotranAinda não há avaliações
- The Yellow House: A Memoir (2019 National Book Award Winner)No EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Nota: 4 de 5 estrelas4/5 (98)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceNo EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceNota: 4 de 5 estrelas4/5 (895)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeNo EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeNota: 4 de 5 estrelas4/5 (5794)
- The Little Book of Hygge: Danish Secrets to Happy LivingNo EverandThe Little Book of Hygge: Danish Secrets to Happy LivingNota: 3.5 de 5 estrelas3.5/5 (400)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaNo EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaNota: 4.5 de 5 estrelas4.5/5 (266)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureNo EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureNota: 4.5 de 5 estrelas4.5/5 (474)
- Never Split the Difference: Negotiating As If Your Life Depended On ItNo EverandNever Split the Difference: Negotiating As If Your Life Depended On ItNota: 4.5 de 5 estrelas4.5/5 (838)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryNo EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryNota: 3.5 de 5 estrelas3.5/5 (231)
- The Emperor of All Maladies: A Biography of CancerNo EverandThe Emperor of All Maladies: A Biography of CancerNota: 4.5 de 5 estrelas4.5/5 (271)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyNo EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyNota: 3.5 de 5 estrelas3.5/5 (2259)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersNo EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersNota: 4.5 de 5 estrelas4.5/5 (344)
- Team of Rivals: The Political Genius of Abraham LincolnNo EverandTeam of Rivals: The Political Genius of Abraham LincolnNota: 4.5 de 5 estrelas4.5/5 (234)
- The Unwinding: An Inner History of the New AmericaNo EverandThe Unwinding: An Inner History of the New AmericaNota: 4 de 5 estrelas4/5 (45)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreNo EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreNota: 4 de 5 estrelas4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)No EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Nota: 4.5 de 5 estrelas4.5/5 (121)
- Aide Competency BookDocumento30 páginasAide Competency Booknursesandi1100% (1)
- LHV Diploma Course Prospectus 2023 Onward 1Documento35 páginasLHV Diploma Course Prospectus 2023 Onward 1Rashid MehmoodAinda não há avaliações
- Doroga Bahrm21s1 Pe003 Fitness Journal LogDocumento4 páginasDoroga Bahrm21s1 Pe003 Fitness Journal LogJeah Joyce LagrimasAinda não há avaliações
- Field Practice 2Documento17 páginasField Practice 2Lea Jane Laurete Calledo75% (4)
- Test Bank For Essentials of Health Information Management 4th Edition by BowieDocumento24 páginasTest Bank For Essentials of Health Information Management 4th Edition by BowieCarolynValentinebaep100% (43)
- Notice: Medical Devices: Premarket Approval Applications, List Safety and Effectiveness Summaries&rsquo AvailabilityDocumento2 páginasNotice: Medical Devices: Premarket Approval Applications, List Safety and Effectiveness Summaries&rsquo AvailabilityJustia.comAinda não há avaliações
- Canadian Coffee ConsumptionDocumento1 páginaCanadian Coffee ConsumptionThe Vancouver SunAinda não há avaliações
- Welcome To Course Title: Clinical Pharmacy Topic: TDM of DigoxinDocumento16 páginasWelcome To Course Title: Clinical Pharmacy Topic: TDM of DigoxinUmair MazharAinda não há avaliações
- Matrix Safety & Loss Control Overview)Documento10 páginasMatrix Safety & Loss Control Overview)Rahul_Gohil_1376Ainda não há avaliações
- Case Study - LacanganDocumento5 páginasCase Study - LacanganLacangan, Thea YvonneAinda não há avaliações
- IDocumento14 páginasIjasdeepkaurnagra100% (1)
- Nursing Care of Client With Kidney CancerDocumento19 páginasNursing Care of Client With Kidney CancerancoursAinda não há avaliações
- POLYPHASE 678 SdsDocumento8 páginasPOLYPHASE 678 SdsMarianna JassoAinda não há avaliações
- Application of Recombinant DNADocumento2 páginasApplication of Recombinant DNANathan B. MhineAinda não há avaliações
- Ayurveda Positive HealthDocumento2 páginasAyurveda Positive HealthmuralipmdAinda não há avaliações
- Benedict James Roldan BermasDocumento4 páginasBenedict James Roldan BermasBenedict James BermasAinda não há avaliações
- Term Paper-Draft Social Anxiety Disorder (Sad) Among AdultsDocumento13 páginasTerm Paper-Draft Social Anxiety Disorder (Sad) Among AdultsWafiAinda não há avaliações
- Exam Questions For Students 1-350Documento26 páginasExam Questions For Students 1-350Komal valve100% (2)
- Medical OncologyDocumento41 páginasMedical Oncologylavadey2Ainda não há avaliações
- General Dentistry Informed Consent FormDocumento3 páginasGeneral Dentistry Informed Consent FormNishtha KumarAinda não há avaliações
- Hajj Health Management in IndonesiaDocumento2 páginasHajj Health Management in IndonesiaTeguh YuwonoAinda não há avaliações
- (Chapter 7) EvidenceDocumento2 páginas(Chapter 7) EvidenceK59 LE THI NGOC THAOAinda não há avaliações
- The Medicinal Properties of Neem: Marlene AdelmannDocumento4 páginasThe Medicinal Properties of Neem: Marlene AdelmannPauloAinda não há avaliações
- ElephantiasisDocumento21 páginasElephantiasisPutri Anena AyuAinda não há avaliações
- Perception of Poverty - A Study On The Non-Social Work StudentsDocumento15 páginasPerception of Poverty - A Study On The Non-Social Work StudentsKoustab MajumdarAinda não há avaliações
- Full Download Health Safety and Nutrition For The Young Child 9th Edition Marotz Test BankDocumento26 páginasFull Download Health Safety and Nutrition For The Young Child 9th Edition Marotz Test Bankretainalgrainascjy100% (37)
- Gaceta Sanitaria 37 Comunica 23 FDocumento21 páginasGaceta Sanitaria 37 Comunica 23 FdsgonzalezAinda não há avaliações
- Sinopharm Vaccine - Guidelines - 06 - 06 - 2021updateDocumento18 páginasSinopharm Vaccine - Guidelines - 06 - 06 - 2021updateChinthana චින්තනAinda não há avaliações
- Sas 6 & 8Documento6 páginasSas 6 & 8Dummy AccountAinda não há avaliações
- Chronic Vs Aggressive PeriodontitisDocumento7 páginasChronic Vs Aggressive PeriodontitisSvnessa VanessaAinda não há avaliações