Escolar Documentos
Profissional Documentos
Cultura Documentos
Edited Schistosomiasis
Enviado por
Karen AlcamporDescrição original:
Direitos autorais
Formatos disponíveis
Compartilhar este documento
Compartilhar ou incorporar documento
Você considera este documento útil?
Este conteúdo é inapropriado?
Denunciar este documentoDireitos autorais:
Formatos disponíveis
Edited Schistosomiasis
Enviado por
Karen AlcamporDireitos autorais:
Formatos disponíveis
Name of Patient: ---------------------------------Name of Informant: -----------------------------Date Interviewed: ______________________ (Please fill in the data being asked) A.
General Data Name: Emerita Flores Age: 57 years old Nationality: Filipino Marital Status: Married Place of Residence: 1331 Magnolia st. Maricaban, Pasay City Date of Consultation: May 2, 2011 Patient E.F., 57 years-old, female, Filipino, (RELIGION???), presently residing at 1331 Magnolia St., Maricaban, Pasay City sought consultation last May 02, 2011 at San Pablo Health Center. B. Chief Complaint The patient complaints pain on her lower right abdomen that radiates at the back. She thought that it was appendicitis. Abdominal Pain C. History of Present Illness 2004- The patient had been taking Nifedipine= used in the treatment of high blood pressure as her maintenance medication for her high blood pressure. She states that shes been experiencing headache with a pain scale of 5 or moderate pain, (0- representing the lowest pain level & 10representing the painful level), she also states that the pain lasts for hours. -Shes been experiencing headache for over a year.
THIS SHOULD BE INCLUDED IN THE PAST MEDICAL HISTORY February 2011- Her first visit at Klinika ng Masa near to her residence, with her purpose to know her blood pressure and remedy for her headache. - With the same complaints of high blood pressure and headache, the Dr. (Dont know his name) prescribed her to take Metropolol= a drug that controls the activity of the heart, and is used to treat high blood pressure and Mefenamic acid= used to treat headache. THIS SHOULD BE INCLUDED IN THE PAST MEDICAL HISTORY March 2- May 3- her nephew & his wife arrived from Samar, and stayed with the patients house for 1 month. IS THIS INFO REALLY NEEDED FOR YOUR HISTORY OF PRESENT ILLNESS??? April 7- she went back to Klinika ng Masa for check-up for her regular blood pressure check-up. - Dr. from Klinika ng Masa, advised her to do an ECG (electrocardiogram)= recording of the electrical activity of the heart. April 14- she took an ECG test April 16- result of ECG April 29- Dr. G. Perez of Claudio Medical Clinic read and interprets her ECG result - Prescribed he to take omeprazole= used to treat gastric ulcer, and and amlodipine= used to treat hypertension - After reading her ECG result, Dr. Perez advised her to take 4 tests, but the patient failed to follow the Drs order. THIS SHOULD BE INCLUDED IN THE PAST MEDICAL HISTORY
May 2- Her first visit to San Pablo Health Center, with a chief complaints of pain on her right abdomen, she thought that it was appendicitis. - said that shed been experiencing abdominal pain since the year 2011 starts. - With a pain scale of 2 - First meeting with Dr. Carl Antonio - Dr. Antonio advised her to take an ultrasound test. WHEN DID THE ABDOMINAL PAIN STARTED??? LOCATION? PRECIPITATING FACTORS??? RELIEVING FACTORS?? SEVERITY??? TIMING??? THERE ARE NO DATA on THE ABOVE STATEMENTS tells us that? WHAT ARE THE ASSOCIATED SIGNS AND SYMTOMS? ANY MEDS TAKEN BEFORE CONSULTATION? ANY CONSULTATION DONE BEFORE CONSULTATION? May 9-18- she had a vacation at Samar, the pain on her abdomen is still present, with a pain scale of 2. May 31- She went to San Pablo Health Center, to check her cervical lymph nodes or kulani present in her neck - Dr. Antonio prescribed her to take amoxicillin= used to treat infections. AGAIN WHAT HAPPENED TO THE SYMPTOM? DOES IT WORSENS? ANY APPEARANCE OF NEW SYMPTOMS? MEDS TAKEN? CONSULTATION DONE? July 13- the day of her ultrasound test, got the result on the same day. July 15- she went back to the clinic and Dr. Domingo from San Pablo Health Center read the result. - The patient been diagnosed of Schistosomiasis - Dr. Domingo prescribed her to take Praziquantel= antihelminthic drug used to eliminate tapeworms and schistosomes. - Dr. Domingo advised the patient to take laboratory tests (cbc, fecalysis, urinalysis, SGOT,SGPT, APTT and kato katz test) July 20- result of laboratory tests, except for the kato katz test, that
has not been perform yet July 22- went to the clinic - Dr. Domingo read the and interpret the result - The patient has Urinary Tract Infection - Prescribed to take Cefalexin= used to treat urinary tract infections The patient complaints pain on her right shoulder with a pain scale of 5 she states that she could not lift arm. Dr. prescribed her to take paracetamol= used to treat mild or moderate pain August 19- she visit San Pablo Health Center, just to check her pressure. As of this time the patient still experiencing pain on her right abdomen and has not been performing kato katz test.
D. Past Medical History a. Disease:
The patient has a history of Hypertension, no diabetes, no asthma and other forms of disease. b. Previous hospitalizations, surgeries, accidents: The patient been hospitalized when she gave birth to her children. E. Personal/Social Histoy a. Smoking and Drinking history The patient is a non smoker and non-alcoholic b. Educational Attainment The patient is a high school graduate of Pambuhan National High School c. Number of children The patient has three children. The eldest is Ramil Flores 33 y.o, a high school graduate, married, currently living with his own family. The second child is Ryan Flores 31 y.o, single, a computer software graduate, and currently working as waiter in Jeddah, Saudi Arabia. The youngest is Ruby Rose Flores, 18y.o, single, lives with her mother, a 3rd year college student taking up Office Management Course at City University of Pasay. d. Occupation The patient stays at her house, Her son who works abroad supports their daily living. e. Lifestyle: Diet, physical activity The patient includes fish, vegetable and banana and eggs as part of her diet. She washes clothes, cooks, and regularly went to the marketplace as her work of exercise. f. Hobbies
The patient is fond of cross-stitching and bag making made by beads. F. Family History Father side- in paternal side of the patient, hypertension, asthma, diabetes is their heredofamilial disease. G. Obstetric History a. Menarche: Year 1967. The patient was 14 years old b. Last normal menstrual period: when she was 46 y.o/ Menopausal period c. Sanitary pads consumed per day? Slightly, moderate or heavily soaked: slightly soaked, 2 pads per day. d. Gravida? Parity? OB score: G4P3T3P0A1L3 The patient has been pregnant 4 times. She gave birth to her first child at 36 weeks, her second pregnancy resulted to miscarriage at 8 weeks, her third pregnancy was delivered at 36 weeks, and her fourth pregnancy was delivered at 36 weeks. J. Physical Assessment A. Vital signs Temperature: 36 Celsius Pulse rate: 64 bpm Respiratory rate: 18 bpm Blood Pressure: 160/100 Head and Neck The head is proportional to the size of the body, therefore, the head is normocephalic (normal shape of the head). Her scalp has no presence of nits lice and dandruff. Hair is black with gray strands, hair is evenly distributed. There is no palpable lymph nodes on the neck. Skin There is no presence of lesions or the like on the skin of the patient. Eyes, Ears, Nose, Throat
Eyes are symmetrical and non-protruding (further forward than usual). Eyebrows are slightly curve, evenly distributed and symmetrical. The eyelashes are black in color and evenly distributed and slightly curved outward and upward. The eyelids are not inverted and no mass palpated. Lid margins are clear without scaling and secretions. Sclera is white and clear. Iris is proportional to the size of the eyes, round and black in color. The pupils are round , black in color and reactive to light and accommodation. Eyes can move in full motion. The patients left eye has a higher grade than the other side(the patient did not remember the grade of her eyeglasses) Ears are parallel, symmetrical, and proportional to the size of the head. Her ear canal has a small amount of cerumen, hearing acuity of both ears can hear whispers that were spoken 2 ft away. Nose in in normal position, located in the midline of the face. The internal nares is clean and slightly moist , with few nasocilliary hairs. The patient has no common colds, and no presence of nasal discharges. Mouth is symmetrical to the lip margin. The lips are moist and a bit pinkish in color. Gums are bit pinkish in color and not swelling. The tongue is freely movable, smooth. The patient feels areas of tenderness at the tip of her tongue. The palate is pinkish and in normal in dome shape. The throat is well modulated. Chest and Lungs The chest has a symmetrical expansion with breathing. The breath sound is normal and no abnormal sounds were heard. The patient is not experiencing difficulty of breathing. Bilaterally symmetrical of the vocal fremitus. Skin temperature of the chest of the chest are uniform. Cardiovascular The aortic and pulmonic areas have no pulsations as well as the tricuspid area of the heart. The PMI (point of maximal impulse) has visible pulsations. The heartbeat of the patient is in regular pattern. Gastrointestinal Tract The skin integrity of the abdomen is normal. The contour is flat, rounded convex. There is symmetric contour and abdominal movement. The patient is experiencing pain on her lower part of her
right abdomen. The borborygmy of the client is 18 movements per minute. The patients bowel movement has a rough texture the last time we visit her. Genitourinary Tract The patient has a history of urinary tract infection. She has no problem in urinating. Musculoskeletal The lower extremities of the patient are in normal condition, where she can move freely and the range of motion is done with ease. The left arm of the patient is freely movable but the right arm has limited movement because of the presence of pain. Neurologic (Cranial Nerves) I. Olfactory nerve The patients cranial nerve number 1 is functioning well because she was able to distinguish different stimuli. II. Optic nerve The patients optic nerve is functioning but the visual acuity of the patient is degraded. III. Oculomotor nerve The patient was able to follow and move her eyes in six ocular movements. IV. Trochlear nerve The patient was able to move her eyes downward easily. V. Trigeminal nerve Patient can clench teeth tightly. Masseter muscles bulge when teeth are clenched. On palpation, both masseter muscles feel equal in size and strength. VI. Abducens nerve The patient can easily move her eyes laterally.
VII. Facial nerve The patient has symmetrical facial contours and lines as well as symmetrical facial movements. The patient can also perform all facial expressions asked by the student nurse.
VIII. Vestibulo cochlear or Auditory nerve The patient has equal hearing in both ears. Air conducted tones are heard twice. The patient was able to balance herself in different normal positions. IX. Glossopharyngeal nerve and X. Vagus nerve The patient was able to identify the taste of the food given to her by the student nurse. The patient has normal gag reflex. The patient voice is clear and no horseness. XI. Spinal Accessory The patient can resist the force applied on her shoulder and jaw. XII. Hypoglossal nerve The patient can freely move her tongue up and down, left and right.
Você também pode gostar
- I.I Biographic DataDocumento10 páginasI.I Biographic DataRobby James RabeAinda não há avaliações
- Pedia - DengueDocumento10 páginasPedia - DengueJan Mikhail FrascoAinda não há avaliações
- College of Nursing: Panpacific University North PhilippinesDocumento20 páginasCollege of Nursing: Panpacific University North PhilippinesMar OrdanzaAinda não há avaliações
- Case Study CholecystitisDocumento33 páginasCase Study CholecystitisMelai de GuzmanAinda não há avaliações
- Case Presentation (Pneumonia)Documento41 páginasCase Presentation (Pneumonia)Rodney Reyes100% (1)
- BPHDocumento15 páginasBPH'mYk FavilaAinda não há avaliações
- A. Biographical DataDocumento6 páginasA. Biographical DataDRAAinda não há avaliações
- Medical Surgical Nursing MRS.H in The Lavender Room: Eka Rahayu (16012)Documento7 páginasMedical Surgical Nursing MRS.H in The Lavender Room: Eka Rahayu (16012)Eka RahayuAinda não há avaliações
- 3rd Year Precept Pedia Case 4 HydroceleDocumento4 páginas3rd Year Precept Pedia Case 4 Hydrocelekristel_nicole18yaho100% (1)
- Patient Health HistoryDocumento8 páginasPatient Health HistoryRafi LabAinda não há avaliações
- History of Past and Present IllnessDocumento10 páginasHistory of Past and Present IllnessRenea Joy ArruejoAinda não há avaliações
- Nursing History I. Client's ProfileDocumento6 páginasNursing History I. Client's ProfileLc RamboyongAinda não há avaliações
- Ward Paper LegitDocumento13 páginasWard Paper LegitLuigi FranciscoAinda não há avaliações
- Preterm Labor Case StudyDocumento26 páginasPreterm Labor Case StudyKirk Espanol Bigstone82% (11)
- Age - For SubmissionDocumento27 páginasAge - For SubmissionAdrian MallarAinda não há avaliações
- Case History The Chief Complaint (CC)Documento18 páginasCase History The Chief Complaint (CC)21912664Ainda não há avaliações
- A Care Study ON Normal Spontaneous Vaginal DeliveryDocumento35 páginasA Care Study ON Normal Spontaneous Vaginal DeliveryCharlskin LetzAinda não há avaliações
- Case Study - OTITIS MEDIADocumento9 páginasCase Study - OTITIS MEDIAHasing Amado100% (1)
- Nursing Case Study: UMC OR RotationDocumento32 páginasNursing Case Study: UMC OR RotationMaryjoy EstarisAinda não há avaliações
- Psychiatric History General DataDocumento2 páginasPsychiatric History General DataStarlet Rhonadez Bito-onon OrielAinda não há avaliações
- A Case Presentation In: Assigned Area: Ob Concept: "Care of Family and Family Health"Documento33 páginasA Case Presentation In: Assigned Area: Ob Concept: "Care of Family and Family Health"Maria Charis Anne IndananAinda não há avaliações
- Y3 T2 PAM CWU 2 - Acute BronchiolitisDocumento7 páginasY3 T2 PAM CWU 2 - Acute Bronchiolitisanon_67984147Ainda não há avaliações
- Hirschsprung'S Disease in A Child: Case ReportDocumento57 páginasHirschsprung'S Disease in A Child: Case ReportHans NatanaelAinda não há avaliações
- Sample HADocumento8 páginasSample HAFlorenceUyAinda não há avaliações
- POTT's DiseaseDocumento18 páginasPOTT's DiseaseDawn MarcoAinda não há avaliações
- Ward Work 1Documento6 páginasWard Work 1Jermaine SerranoAinda não há avaliações
- BPPV CaseDocumento24 páginasBPPV CaseAnonymous ZbVovJEFuAinda não há avaliações
- Vehicular AccidentDocumento9 páginasVehicular AccidentCharm TanyaAinda não há avaliações
- AppendicitisDocumento79 páginasAppendicitisMaria Paula Bungay100% (1)
- Sharon Owuor Case Study Rh1Documento19 páginasSharon Owuor Case Study Rh1Kuto Yvonne CheronoAinda não há avaliações
- Nursing Case Study TAHBSODocumento17 páginasNursing Case Study TAHBSOandymojer85% (13)
- Case AppendicitisDocumento10 páginasCase AppendicitisNiña Montejo EaldamaAinda não há avaliações
- Weekly Requirement OB WardDocumento12 páginasWeekly Requirement OB WardXerxes DejitoAinda não há avaliações
- MS CaseDocumento28 páginasMS CaseJuwaka OsakaAinda não há avaliações
- Case Study Abdominal Blunt InjuryDocumento10 páginasCase Study Abdominal Blunt InjuryHomework PingAinda não há avaliações
- CWU 2 Epipepsy - West SyndromeDocumento10 páginasCWU 2 Epipepsy - West SyndromeZul Hisyam Fikri100% (1)
- OBDocumento4 páginasOBEllaAinda não há avaliações
- Intensive Case Study: Nursing Health History Biographic DataDocumento15 páginasIntensive Case Study: Nursing Health History Biographic Databojums67% (3)
- 13 Areas of Assessment I. Psychological StatusDocumento3 páginas13 Areas of Assessment I. Psychological StatusjoharaqohAinda não há avaliações
- HistoryDocumento5 páginasHistoryJenny MarquezAinda não há avaliações
- Pediatrics 2 LaboratoryDocumento40 páginasPediatrics 2 LaboratoryAmaetenAinda não há avaliações
- Case Write Up 1-CholecystitisDocumento9 páginasCase Write Up 1-CholecystitisAmbhi Gana100% (1)
- Prepared By: Sarra'a Fawaz AbbasDocumento36 páginasPrepared By: Sarra'a Fawaz AbbasSarraa NajimAinda não há avaliações
- Ii. Chief ComplaintsDocumento4 páginasIi. Chief ComplaintsArianne_Danglo_2118Ainda não há avaliações
- навыки 6 курсDocumento44 páginasнавыки 6 курсAshish R. JadhavAinda não há avaliações
- Coarctation of Aorta (Coa) in 1-Year 4-Month Old GirlDocumento21 páginasCoarctation of Aorta (Coa) in 1-Year 4-Month Old GirlJkp PhieAinda não há avaliações
- Sagun Pls Dont Dilit Huhuhhuhhu 123Documento85 páginasSagun Pls Dont Dilit Huhuhhuhhu 123Star SagunAinda não há avaliações
- Flail Chest (Tayug)Documento25 páginasFlail Chest (Tayug)Adrian MallarAinda não há avaliações
- Case Report Example - GynaecologyDocumento14 páginasCase Report Example - GynaecologyDr Onn Azli PuadeAinda não há avaliações
- History No. 2: Group 1-Section ADocumento61 páginasHistory No. 2: Group 1-Section ANikko Ryan C'zare AbalosAinda não há avaliações
- Final SDL 1Documento21 páginasFinal SDL 1Cy PilapilAinda não há avaliações
- Masquerade of Loneliness : Filamer Chistian University College of Nursing Roxas CityDocumento16 páginasMasquerade of Loneliness : Filamer Chistian University College of Nursing Roxas CityJason A. AdoyoganAinda não há avaliações
- Case StudyDocumento17 páginasCase StudyHomework PingAinda não há avaliações
- Pancreatic CancerDocumento15 páginasPancreatic CancerMutiana Muspita JeliAinda não há avaliações
- Our Lady of Fatima UniversityDocumento5 páginasOur Lady of Fatima UniversityEmmanuel De LeonAinda não há avaliações
- Case Presentation Final2Documento36 páginasCase Presentation Final2zerpthederpAinda não há avaliações
- Carbuncle, Incision, Drainage, DebridementDocumento11 páginasCarbuncle, Incision, Drainage, DebridementAlvin Germo PasuquinAinda não há avaliações
- MSDocumento2 páginasMSKaren AlcamporAinda não há avaliações
- Pentagon NLE Review NotesDocumento33 páginasPentagon NLE Review NotesChieChay Dub93% (123)
- Primary Open-Angle Glaucoma GenesDocumento9 páginasPrimary Open-Angle Glaucoma GenesKaren AlcamporAinda não há avaliações
- The Different Parts of Oxygen TanksDocumento6 páginasThe Different Parts of Oxygen TanksKaren Alcampor0% (1)
- Asymptomatic Lower Calyceal Renal Calculi - To Treat or Not To TreatDocumento2 páginasAsymptomatic Lower Calyceal Renal Calculi - To Treat or Not To TreatJuzteen Bianca Mae AndinoAinda não há avaliações
- Dosage Calc ReviewDocumento24 páginasDosage Calc ReviewKara Dawn Mason100% (1)
- LactationDocumento24 páginasLactationJenyl Bajado100% (1)
- Primum Press Kit 2012Documento13 páginasPrimum Press Kit 2012Karina EngraffAinda não há avaliações
- Aetna Hmo 20 GeorgiaDocumento94 páginasAetna Hmo 20 Georgiabill_w85081Ainda não há avaliações
- Sme Package Summary of Benefits (2305843009215646953)Documento7 páginasSme Package Summary of Benefits (2305843009215646953)RIVERA - SARVIDA CONSTRUCTION INC.Ainda não há avaliações
- Aroma N Masase KakiDocumento5 páginasAroma N Masase KakiAsmawati NadhyraAinda não há avaliações
- Esophageal EmergenciesDocumento15 páginasEsophageal EmergenciesOmar SolisAinda não há avaliações
- ACOG Guidelines For Exercise During PregnancyDocumento13 páginasACOG Guidelines For Exercise During Pregnancypptscribid100% (1)
- Mechanism of Labour (Normal and Abnormal)Documento27 páginasMechanism of Labour (Normal and Abnormal)Rani100% (1)
- The Five Tibetan RitesDocumento12 páginasThe Five Tibetan RitesFlorea Eliza100% (1)
- 100 Diseases Treated by Single Point of AcupunctureDocumento209 páginas100 Diseases Treated by Single Point of AcupunctureAgeng Rikhmawan100% (31)
- Fam CaseDocumento9 páginasFam Casefam111222Ainda não há avaliações
- BibliographyDocumento3 páginasBibliographyKim Andrei Estrella ApeñaAinda não há avaliações
- Pediatric Hematology Oncology JournalDocumento3 páginasPediatric Hematology Oncology JournalHawin NurdianaAinda não há avaliações
- HCIA Study Guide 2023Documento22 páginasHCIA Study Guide 2023consultasluisfloresdrAinda não há avaliações
- Normal Lab Values For PediatricsDocumento15 páginasNormal Lab Values For PediatricsJE MagbanuaAinda não há avaliações
- Pre Auricular Sinus ReviewDocumento6 páginasPre Auricular Sinus ReviewEthan LiaoAinda não há avaliações
- Medical Catastrophe PDFDocumento221 páginasMedical Catastrophe PDFghuoiAinda não há avaliações
- Gastritis Erosif PatofisiologiDocumento3 páginasGastritis Erosif PatofisiologiLargactil CpzAinda não há avaliações
- Hyperglycemia in PregnancyDocumento17 páginasHyperglycemia in PregnancyIza WidzAinda não há avaliações
- Theoretical Foundations in Nursing: Nursing As An Art and ScienceDocumento23 páginasTheoretical Foundations in Nursing: Nursing As An Art and ScienceRico Mae ValenciaAinda não há avaliações
- 03 The Role of "Smart" Infusion Pumps in Patient Safety PDFDocumento11 páginas03 The Role of "Smart" Infusion Pumps in Patient Safety PDFSaravanan NallasivanAinda não há avaliações
- Pneumonectomy Management PDFDocumento6 páginasPneumonectomy Management PDFMurali BalaAinda não há avaliações
- MenopauseDocumento14 páginasMenopauseMizna SabillaAinda não há avaliações
- Who 2011 Lagman RequestDocumento5 páginasWho 2011 Lagman RequestMulat Pinoy-Kabataan News NetworkAinda não há avaliações
- RMO Clinical HandbookDocumento533 páginasRMO Clinical HandbookRicardo TAinda não há avaliações
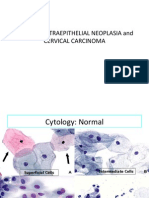
- 04 CIN and Cervical Cancer UNEDITEDDocumento120 páginas04 CIN and Cervical Cancer UNEDITEDRalph JuicoAinda não há avaliações
- Obstetric SBAs MCQDocumento5 páginasObstetric SBAs MCQCofeelovesIronman Javier100% (1)
- DR Aamir Advances EntDocumento36 páginasDR Aamir Advances EntAamir YousufAinda não há avaliações