Escolar Documentos
Profissional Documentos
Cultura Documentos
Malaria in the Philippines
Enviado por
Jovelyn BucsitDescrição original:
Título original
Direitos autorais
Formatos disponíveis
Compartilhar este documento
Compartilhar ou incorporar documento
Você considera este documento útil?
Este conteúdo é inapropriado?
Denunciar este documentoDireitos autorais:
Formatos disponíveis
Malaria in the Philippines
Enviado por
Jovelyn BucsitDireitos autorais:
Formatos disponíveis
Subject: FCM III Topic: MALARIA Lecturer: DR. FLORES Shifting /Date: 2nd Shifting/ Sept.
12, 2008 Trans group: we-love-brothers-sandwich group
Impact Worldwide
Malaria causes about 350-500 million infections in humans Approximately 1.3-3 million deaths annually - this represents at least one death every 30 seconds. Occur in children under the age of 5 years, in vast majority of cases and pregnant women are also vulnerable. Death rate is expected to double in the next twenty years. Precise statistics are unknown because many cases occur in rural areas where people do not have access to hospitals andlor the means to afford health care. Consequently, many cases are undocumented. Malaria is the most common and most persistent mosquito-borne infection in the Philippines although cases and deaths have gone down. Endemic areas are usually rural, hilly or mountainous, and hard to reach.
Usual transmission is through the infective bite of this female anopheles mosquito and rarely through blood transfusion, placenta and sharing of contaminated needles. There are several types of mosquitoes but only certain species that belong to the Genus Anopheles transmit malarial parasites. Must be recognized promptly in order to treat the patient in time and to prevent further spread of infection in the community
High-risk groups consist of upland subsistence farmers, forest-related workers, indigenous peoples and settlers in frontier areas, and Migrant agricultural workers. Disease transmission perennial generally higher during the rainy season than the dry season Incidence rate of malaria Decreased from 101 cases per 100,000 population in 1996 to 67 per 100,000 in 2000, a 34 percent reduction within four years
Should be considered a potential medical emergency and should be treated accordingly Delay in diagnosis and treatment IS a leading cause of death in malaria patients in the United States. Can be suspected based on the patient's symptoms and the physical findings at examination. However, for a definitive diagnosis to be made, laboratory tests must demonstrate the malaria parasites or their components. Diagnosis of malaria can be difficult.
Malaria is more common in rural areas than in cities; this is in contrast to dengue fever where urban areas present the greater risk. For example, the cities of the Philippines, Thailand and Sri Lanka are essentially malaria-free, but the disease is present in many rural regions. By contrast, in West Africa, Ghana and Nigeria have malaria throughout the entire country, though the risk is lower in the larger cities.
Where malaria is not endemic any more (such as the United States), health care providers are not familiar with the disease Clinicians seeing a malaria patient may forget to consider malaria among the potential diagnoses .and not order the needed diagnostic tests. Laboratorians may lack experience with malaria and fail to detect parasites when examining blood smears under the microscope. Malaria transmission in some areas is so mtense that a large proportion of the population is infected but not made ill by the parasites. Such carriers have developed just enough immunity to protect them from malarial illness but not from malarial infection. In that situation, finding malaria parasites in an ill person does not necessarily mean that the illness is caused by the parasites. OF MALARIA
OVERVIEW OF MALARIA Malaria is a disease caused by one or more species of the protozoan parasites called plasmodium. Mosquito: the malaria vector The natural vector is the female mosquito that is part of the biological environment.
SIGNIFICANT BIOLOGICAL FEATURES VECTORS IN THE PHILIPPINES:
TO CONTROL THE LARVAE Changing the environmental condition can make it
MARY YVETTE ALLAIN TINA RALPH SHERYL BART HEINRICH PIPOY KC JAM CECILLE DENESSE VINCE HOOPS CES XTIAN LAINEY RIZ KIX EZRA GOLDIE BUFF MONA AM MAAN ADI KC PENG KARLA ALPHE AARON KYTH ANNE EISA KRING CANDY ISAY MARCO JOSHUA FARS RAIN JASSIE MIKA SHAR ERIKA MACKY VIKI JOAN PREI KATE BAM AMS HANNAH MEMAY PAU RACHE ESTHER JOEL GLENN TONI
Subject: FCM III Topic: MALARIA
Page 2 of 8 unsuitable for larval development & can destroy the aquatic stages Predators such as fishes eat the mosquito larvae.
TO CONTROL THE ADULT MOSQUITOES Spraying insecticides on the walls and other surfaces where the mosquitoes rest before and after biting can control the adults Insecticide treated mosqUito nets are also used to control the adult population.
Climactic conditions
Prolonged dry season reduces the availability of surface water for breeding other mosquitoes leads to reduction of malarial transmission. Even distribution of rainfall, temperature between 20-30C and humidity >60 % on the other hand are very favorable to malarial transmission. In general, transmission is higher during rainy season than during dry season.
Endemic areas are usually~ rural, hilly or mountainous, and hard to reach. MALARiA CONTROL in the Philippines in the 1990s had Significantly reduced cases by 60% (from 89,047 in 1990 to 34,787 in 2001) Still malaria remains endemic in 65 of the 78 provinces, 760 of the 1,600 municipalities and 9, 345 of the 42, 979 barangays nationwide. At risk of malaria nationwide are 11 million Filipinos mainly living in the remote hard to reach areas. Endemicity is now generally moderate to low, With pockets of high endemicity, persisting along the provincial/regional borders in frontier areas, places populated by indigenous cultural groups and areas with socio-political conflicts. It constitutes to be a major impediment to human and economic development in areas where it persists It still costs the economy over 100 million pesos to sustain control efforts
Socioeconomicand behavioral factors that favor the increase of malaria transmission: Population movement related to socioeconomic activities (logging, mining "kaingin" farming) sociopolitical factors (peace and order problems) Poor housing condition readily exposes the occupation to mosquito bites Poor compliance to control measures including treatment Poor economy and inadequate political will to sustain the control program Lack of poor difficult roads in endemic areas. Prevalence and Incidence of Infection The Prevalence of a condition is the percentage of population which was affected at a single point in time. The prevalence of malaria infection is generally used to characterize the level of transmission. Prevalence of malaria infection is measured in 3 main ways: o Parasite rate: through microscopy of blood films o Spleen rate: spleen palpation o Seroprevalence rate: serologic methods The methods mentioned previously can be used to quantify the intensity of transmission e.g. force of infection (%) based on the parasite rate or seroprevalence. Hypoendemic Mesoendemic Hyoerendemic Holoendemic Spleen Rate (%) 0-10 11-50 >75 (low in adult) >75 (low in adult) Parasite Rate (%) 0-10 11-50 51-75 >75
Geographical distribution of Malaria Philippines Category A Provinces - 25 Provinces - No significant changes in the last 10 yrs - More than 1000 cases/ year - or situation worsened in the last 5 years Category B Provinces - 22 Provinces - 100 to 1000 casesl year - Situation has improved in the last 5 yrs Category C Provinces - 18 Provinces - less than 100 cases I year - Significant reduction in the last 5 yrs Category D Provinces - Provinces that are already malaria-free (no more indigenous cases for at least 3 years - Some are potentially malarious due to the presence of the vector
Category A Provinces -Apayao -Quezon -Misamis Oriental -Kalinga -Zamboanga del -Davao del sur -Ifugao Sur -Davao del Norte
-Mt. Provihce -Bukidnon -Compostela -lsabela -Quirino Valley -Cagayan -Zambales -Saranggani -Mindoro Occidental
-Palawan -Agusan del Sur Occidental -Basilan -Agusan del Norte -Sulu -Tawi tawi -Surigao del Sur
NATIONAL SITUATION
Malaria is the most common and most persistent mosquitoborneinfection in the Philippines although cases and deaths have gone down.
Category A fn 25 provinces 90% of cases nationwide 348 of the 760 endemic municipalities 4,407 of the 9, 345 barangays (distncts)
Subject: FCM III Topic: MALARIA
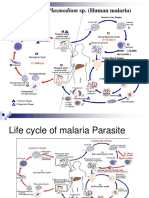
Page 3 of 8 Endemic population of 6,205,08 50-60% of endemic areas categorized under the lowest income group nationally Indigenous peoples (IPs) constitutes 90% of the endemic population Category D Provinces that are already malaria free (no more indigenous cases for at least 3 yrs Cateqorv D Provinces Bohol Siquojor Capiz Leyte Norte Biliran Camiguin Catanduanes Iloilo Guimaras Leyte Aklan Cebu Sulu Northern Samar After at least 6 days the parasites (merozoite stage) are released from the liver cells to the bloodstream and invade the blood cells. Further development and multiplication of the parasites occurs in the RBC. Ultimately the infected RBCs are destroyed. the parasites are released and invade other RBCs This time there may be prodromal symptoms ( Low grade fever, nausea, vomiting, headache.) The development cycle in the RBCs is repeated every 36 to 48 hrs for P. falcifarum, every 48 hrs for P vivax and P. ovate; and every 72 hours for P. malaria. The periodic destruction and subsequent invasion of the RBCs by the parasites cause periodic occurrence of signs and symptoms of malaria typically the paroxysms of chills, fever, and sweating. After 2 to 3 cycles in the red blood cells, some merozoites . give rise to sexual forms (gametocytes). During the blood feeding of the mosquito, the different stages of the parasites are ingested All except the gametocytes are destroyed. A series of development occurs until the sporozoites are developed and congregate in the salivary glands ready for transmission during biting. Usually the developmental cycle in the mosquito takes about 14 days. In other words the parasites can only be transmitted to another person after 14 days from the day the parasite (gametocyte) were ingested by the mosquito. ln cases of P.vivax and P.ovale, some sporozoites develop into the dormant stage called hypn020ites in the liver. The activation of this dormant stage and its subsequent development in the liver and in the RBC causes relapse. In some areas, malaria transmission is so intense that a large proportion of the population is infected but not made ill by the parasites. Such carriers have developed just enough immunity to protect them from malarial illness but not from malarial infection.
Malaria Control Program Program Thrust Vision: Malaria Frep- Philippines by the year 2020 Mission: To empower the health workers, the population at risk and all other concerned to eliminate malaria in the Philippines
Goal: Malaria is eliminated as apublic health problem in endemic provinces
National Health Objectives for 2004 Health Status Objectives -To reduce malaria mortality to 20% annually -To reduce mortality by 10% annually -To prevent the recurrence of transmission in malaria free provinces Risk Reduction Objectives -Increase household utilization of mosquito nets -Increase compliance rate on malaria treatment -Increase coverage of streams that serve as' breeding sites seeded with larvivorous fish -Increase coverage of streams that serve as breeding site cleared Strategies -Provision of early diagnosis and prompt treatment -Planning and implementation of selective or prevention of malaria epidemics -Strengthening local capabilities in basic and applied research to promote assessment of the country's malaria situation
LIFE CYCLE The cycle begins with the introduction of the parasites (sporozoite stage) in the bloodstream of man through the bite of infective female Anopheles mosquito.
W/in 30 mins the sporozoites will invade the liver cells. There will undergo development in the liver, the infected person remains asymptomatic and the parasites cannot be seen yet in the blood.
Subject: FCM III Topic: MALARIA
Page 4 of 8 In that situation. finding malaria parasites in an ill person does not necessarily mean that the illness is caused by the parasites. In many malaria-endemic countiies lack of resources is a major barrier to reliable and timely diagnosis. Health personnel are undertrained, underequipped and underpaid. They often face excessive patient loads, and must divide their attention between malaria and other equally severe infectious diseases such as pneumonia, diarrhea, tuberculosis and HIV/AIDS. children and pregnant women are especially vulnerable Splenomegaly (enlarged spleen) severe headache cerebral ischemia and hemoglobinuria with renal failure may occur. These are more striking and may increase the suspicion index for malaria. Thus, in most cases the early clinical findings in malaria are not typical and need to be confirmed by a laboratory test.
Transmission and symptoms Malaria is caused by protozoan parasites of the genus Plasmodium (phylum Apicomplexa): o P falciparum
Social and economic effects The disease has been associated with major negative economic effects on regions where it is widespread. There has been demonstration of developmental impairments in children who have suffered episodes of severe malaria. o A comparison of average per capita GOP in 1995, (adjusted to give parity of purchasing power) between malarious and non-malarious countries demonstrate a five-fold difference (US$1 ,526 versus US$8,268). o Moreover, in countries where malaria is common, average per capita GOP has risen (between 1965 and 1990) only 0.4% per year, compared to 2.4% per year in other countries. In its entirely, the economic impact of malaria has been estimated to cost Africa US$12 billion every year
o
o
P. malariae P.ovale P. vivax.
P. falciparum is responsible for about eighty percent of infections and ninety percent of deaths. Infections with P. knowlesi and P. simiovale are also known to cause malaria but are of limited public health importance. The parasite's primary hosts and transmission vectors are female mosquitos of genus Anopheles; Humans act as intermediate hosts.
Methods of Mosquito Control -Controlling mosquitoes, and exposure to diseases they may carry, can be done by chemical and non-chemical methods Your first line of defense begins at home. What you can do to control mosquitoes around the home o Remove their habitat (where they live and breed) Eliminate standing water in rain gutters, old tires, buckets, plastic covers, toys, or any other container where mosquitoes can breed Empty and change the water in bird baths, fountains, wading pools, rain barrels, and potted plant trays at least once a week to destroy potential mosquito habitats Drain or fill temporary pools of water with dirt Keep swimming pool water treated and circulating. o Prevent your exposure to mosquitoes Use EPA-registered mosquito repellents when necessary and follow label directions and precautions closely. Use head nets, long sleeves and long pants if you venture into areas with high mosquito populations, such as salt marshes. If there is a mosquito-borne disease warning in effect, stay inside during the evening when mosquitoes are active. Make sure window and door screens are "bug tight."
Clinical Diagnosis Clinical diagnosis is based on the patient's symptoms and on physical findings at examination. The first symptoms of malaria (most often fever, chills, sweats, headaches, muscle pains, arthralgia, nausea and vomiting, severe anemia caused by hemolysis, hemoglobinuria) are often not specific and are also found in other diseases (such as the "flu" and common viral infections). Likewise, the physical findings are often not specific (elevated temperature, perspiration, tiredness). There may be the feeling of tingling in the skin, particularly with malaria caused by P. falciparum.
In severe malaria (caused by Plasmodium falciparum) , clinical findings (confusion, coma, neurologic focal signs, severe anemia, respiratory difficulties, death if untreatedyoung
Subject: FCM III Topic: MALARIA
Page 5 of 8 Replace your outdoor lights with yellow "bug" lights which tend to attract less mosquitoes than ordinary lights. The yellow lights are NOT repellents, however. o Neighborhoods are occasionally sprayed to prevent disease and nuisance caused by large mosquito numbers (If you have any questions about mosquitoes and their control, contact your local mosquito control district or health department.)
Liquid larvicide products are applied directly to water using backpack sprayers and truck or aircraft-mounted sprayers. Tablet, pellet, granular, and briquet formulations of larvicides are also applied by mosquito controllers to breeding areas.
Controlling Adult Mosquitoes Adult mosquito control may be undertaken to combat an outbreak of mosquito-borne disease or a very heavy nuisance infestation of mosquitoes in a community. Pesticides registered for this use are known as adulticides and are applied either by aircraft or on the ground employing truck-mounted sprayers. State and local agencies commonly use the organophosphate insecticides malathion and naled and the synthetic pyrethroid insecticides permethrin, resmethrin, and sumithrin for adult mosquito control. Mosquito adulticides are applied as ultra-low volume (ULVj sprays ULV sprayers dispense very fine aerosol droplets that stay aloft and kill flying mosquitoes on contact. lILV applications involve small quantities of pesticide active ingredient in relation to the ~ize of the area treated, typically less than 3 ounces per acre, which minimizes exposure and risks to people and the environment. Adulticides can be used for public health mosquito control programs without posing unreasonable risks to the general population or to the environment when applied according to the pesticide label. (For more Information on pesticides commonly-used in public health mosquito control programs, see the specific fact sheets mentioned below.) o Malathion for Mosquito Control o Larvicides for Mosquito Control o Naled for Mosquito Control o Permethrin, Resmethrin, Sumithrin (Synthetic Pyrethroids) o for Mosquito Control
Methods used by federal, state and local agencies in mosquito control: Surveillance as First Step in Mosquito Control o The first step in mosquito control is surveillance. State or local mosquito specialists conduct surveillance for diseases harbored by domestic and nonnative birds, including sentinel chickens (used as virus transmission indicators), and mosquitoes. o State and local mosquito control authorities also conduct surveillance for larval habitats by using maps and aerial photographs, and by evaluating larval populations. o ( Other tecnniques include various light traps, biting counts, and analysis of reports from the public. Mosquito control programs also put high priority on trying to prevent a large population of adult mosquitoes from developing so that additional controls may not be necessary Since mosquitoes must have water to breed, methods of prevention may include: o controlling water ievels in lakes, marshes, ditches, or other mosquito breeding sites; o eliminating small breeding sites if possible;
stocking bodies of water with fish species that feed on larvae. Both chemical and biological measures may be employed to kill immature mosquitoes during larval stages. Chemical or Biological Measures to Control Mosquitoes Controlling mosquitoes at the larval stage
Larvicides target larvae in the breeding habitat before they can mature into adult mosquitoes and disperse. Larvicides include: Bacterial Insect Growth Organophosphate lnsecticides Inhibitor Insecticide Methoprene Temephos Bacillus thuringiensis israelensis Bacillus sphaericus
Presumptive Treatment ln highly endemic areas (particularly in Africa), the great prevalence of asymptomatic infections and lack of resources (such as microscopes and trained microscopists) have led peripheral health facilities to use "presumptive treatment" Patients who suffer from a fever that does not have any
Other Materials Mineral oils Monomolecular films Oils and films disperse as a thin layer on the surface of the water which cause larvae and pupae to drown.
Subject: FCM III Topic: MALARIA
Page 6 of 8 obvious cause are presumed to have malaria and are treated for that disease. based only on clinical suspicion, and without the benefit of laboratory confirmation This practice is dictated by practical considerations and allows the treatment of a potentially fatal disease. But it also leads frequently to incorrect diagnoses and unnecessary use of antimalarial drugs. -This results in additional expenses and increases the risk of selecting for drug-resistant parasites. Serology detects antibodies against malaria parasites, using either indirect immunofluorescence (IFA) or enzyme-linked immunosorbent assay (ELISA). Serology does not detect current infection but rather measures past experience.
Drug Resistance Tests Drug resistance tests are performed in specialized laboratories to assess the susceptibility to antimalarial compounds of parasites collected from a specific patient. Two main laboratory methods are available: 1. In vitro tests: The parasites are grown in culture in the presence of increasing concentrations of drugs; the drug concentration that inhibits parasite growth is used as endpoint: 2. Molecular characterization: molecular markers assessed by PCR or gene sequencing allow also the prediction, to some degree, of resistance to some drugs; however, the predictive values of these molecular tests are still being evaluated Information for The General Public Malaria can be a sel/ere, potentially fatal disease (especially when caused by Plasmodium falciparum) and treatment should be initiated as soon as possible.
Microscopic diagnosis Malaria parasites can be identified by examining under the microscope a drop of the patient's blood, spread out as a "blood smear" on a microscope slide. Prior to examination, the specimen is stained (most often with the Giemsa stain) showing a white blood cell (on left side) and several red blood cells, two of which are infected with Plasmodium falciparum (on right side). The Giemsa stain gives to the parasites a distinctive appearance. This technique remains the gold standard for laboratory confirmation of malaria However, it depends on the quality of the reagents, of the microscope, and on the experience of the laboratorian Alternate methods for laboratory diagnosis include: Antigen Detection Various test kits are available to detect antigens derived from malaria parasites. Such immunologic ("immunochromatographic") tests most often use a dipstick or cassette format, and provide results in 2-10 minutes. These "Rapid Diagnostic Tests" (ROTs) currently used in some clinical settings and programs, offer a useful alternative to microscopy in situations where reliable microscopic diagnosis is not available These Malaria ROTs however, befc~e they car. be widely adopted, should address several Issues such as Improving their accuracy; lowering their cost; and ensuring their adequate performance under adverse field conditions Malaria ROTs are currently not approved by the U. S. Food and Drug Administration (FDA) for use in the United States The World Health Organization's Regional Office for the Western Pacific (WHOM'PRO) provides technical information, including a list of commercially available malaria ROTs Molecular Diagnosis Parasite nucleic acids are detected using polymerase chain reaction (PCR). This technique is more accurate than microscopy. However, it is expensive, and requires a specialized laboratory (even though technical advances will likely result in field-operated PCR machines). Other techniques related to malaria diagnosis are: Serology
In endemic areas, the World Health Organization recommends that treatment be started within 24 hours after the first symptoms appear. Treatment of patients with uncomplicated malaria can be conducted on an ambulatory basis (without hospitalization) but patients with severe malaria should be hospitalized if possible. In areas where malaria is not endemic, all patients with malaria (uncomplicated or severe) should be kept under clinical observation if possible. Patients who have severe P. falciparum malaria or who cannot take oral medications should be given the treatment by continuous intravenous infusion. In some countries (but not the United States) sdme antimalarial drugs are found in suppository form Several antimalarial drugs are available for treatment by continuous intravenous infusion. Most drugs used in treatment are active against the parasite forms in the blood (the form that causes disease) and include: o chloroquinesulfadoxine-pyrimethamine (Fansidar) o mefloquine (Lariam) o atovaquone-proguanil (Malarone) o quinine o doxycycline artemisin derivatives (not licensed for use in the United o States, but often found overseas) In addition, primaquine is active against the dormant parasite liver forms (hypnozoites) and prevents relapses.
Subject: FCM III Topic: MALARIA
Page 7 of 8 Primaquine should not be taken by pregnant women or by people who are deficient in G6PD (glucose-6phosphate dehydrogenase). Patients should not take primaqUine until a screening test has excluded G6PD deficiency It is probable that the second-line drugs distributed by the national government are routinely used in place of the unavailable first-line drugs (chloroquine pius sulfadoxine-pyrimethamine). The risk is that the prar.tice may hasten the development of resistance to second-line drugs. There are signs that the level of drug-resistant cases of malaria is increasing in some areas. Further investigation by DOHand medical institutions is necessary to confirm and address this problem.
How to treat a patient with malaria depends on: The type (species) of the infecting parasite
The area where the infection was acquired and its drug resistance status The clinical status of the patient Any accompanying illness or condition Pregnancy Drug allergies. or other medications taken by the patient The incidence rate of malaria decreased from 101 cases per 100,000 population in 1996 to 67 per 100,000 in 2000, a 34 percent reduction within four years Mortality rate from malaria 'has remained below one death per 100,000 populations since 1995 (PHS 2000) The case detection rate for malaria has also continued to decrease from 1996 to 2000. Provinces have been categorized according to the number and trend of cases. o Category A refers to highly endemic provinces
Goal: Malaria burden is significantly reduced in endemic areas and the malaria-free status for 13 provinces is maintained. (A province is considered malaria-free when there is no reported indigenous case for three consecutive years) Comparison of Etiologic Agents P. The most common in the Philippines, around falciparum 70 % of cases. Causes severe malaria and death if not treated promptly appropriately Resistance to antimalarial drugs in the country is widespread P. vivax Comprise about 30% of cases Very rarely causes severe disease Sensitive to antimalarial drugs relapse is common if not treated adequately with anti-relapse drug P. malariae Very rare in the Philippines less than 1% of cases in the country Infection is usually not severe but many last up to 50 yrs if not treated Drug resistance has not yet been documented P. ovale Rarely found in the Philippines present in some African countries Relapse may occur If not treated adequately with anti-relapse drug drug resistance is not yet been documented P. falciparum 12 (9-14) 5.5 7 40,000 48 Younger cells (but invades cells of all ages) No 36 to 48 16-36 or longer Severe in non-immune ++ P. vivax 13 ( 12 to 17) 6-8 10,000 42 - 48 Reticulocyte s Yes 48 8 to 12 Mild severe to P. malariae 28 (18-40) 12 16 2,000 72 Older cells
o o
Category B are those classified moderately endemic. o Category C are low endemic provinces Category D are those declared as malaria-free
There are 26 Category A provinces which continue to carry the burden of at least 90 percent of all malaria cases in the country despite the reported sustained treatment of ail confirmed cases of malaria, and the 100 percent coverage of blood smear examination for the clinically diagnosed malaria patients. The 13 malaria-free provinces composed of Aklan, Biliran, Sohol, Camiguin, Capiz, Catanduanes, Cebu, Guimaras, Iloilo, Leyte, Southern Leyte, Northern Samar and Siquijor continue to be malaria free as of 2003 Several international health and bUSiness organizations support maiana control initiatives in different parts of the country such that quality assurance measures are done for various program components: clinical and laboratory diagnosis, drug supply management and case treatment. Population groups in malaria-endemic areas are often geographicaiiy and socioeconomically marginalized and rely on the local government for medical assistance. However, the procurement of first-line anti-malaria drugs by local governments is not assured. On the other hand, the drugs bought by the national government are only for the few cases requiring second-line drugs (artemisinines).
Characteristics Incubation (days) Exoerythrocytic cycles (days) No. merozoites/liver cell Erythrocytic cycle RBC preference
Relapses Fever periodicity (hours) Febrile paroxysm length Severity of attacks Drug resistance
No 72 8 to 10 Mild
Subject: FCM III Topic: MALARIA
Page 8 of 8 Species dist. in the Phil 70% 30% <1%
In collaboration with LGUs which provides direct service delivery to the populace in households located in all endemic barangays suchas indigenous people, night shift and forest workers, especially in Category A endemic localities using standard DOH treatment protocols in areas where malaria has been eliminated.
National Objectives for 2005-2010 Objective Malaria cases are reduced least 70 percent in 26 Category A provinces Transmission of malaria in the general population is reduced Indicator Morbidity rate of malaria per 100,000 population in 26 provinces Proportion of population malaria-risk areas using insecticide treated bed nets Proportion of children under five years old sleeping under insecticide treated bed nets Morbidity rate and mortality rate of malaria per 100,000 Population in Category B & C provinces Number of provinces declared as malaria-free Target 15 cases per 100,000 26 Category A provinces Baseline Data & Source 50.3 case per 100,000 population Field Health Service InformationSyste m, 2002 TBD
TBD
TBD
TBD
Morbidity and mortality are reduced by at least 50 percent in Category B and Category C provinces Malaria-free status is achieved
Morbidity 2.6 cases or less per 100,000 Mortality and 0.04 death or less per 100,000 popn
Morbidity 5.1 cases per 100,000 population Mortality: 007 death per 100,000 popn National Center for Disease Prevention and Control, DOH 13 provinces are malaria-free
(DOH Administrative Reports)
13 provinces maintained as malariafree 5 more provinces declared as malaria-free
Strategic Thrusts for 2005-2010 Ensure the availability of anti-malaria drugs to endemic areas through centralized procurement and distribution Promote effective and regUlar use of insecticidetreated bed nets Plan and implement malaria control measures with specific target population groups Promote early diagnosis, management and referral of malaria cases Mobilize local government and community resources for malaria case surveillance case detection and case management in 26 Category A provinces
Você também pode gostar
- Malaria 1. Who and How?: P. Falciparum P. VivaxDocumento6 páginasMalaria 1. Who and How?: P. Falciparum P. VivaxAdriana del RioAinda não há avaliações
- Malaria: Lyndon L. Lee Suy, MD, MPHDocumento30 páginasMalaria: Lyndon L. Lee Suy, MD, MPHPurplesmilezAinda não há avaliações
- Malaria ReviewerDocumento6 páginasMalaria ReviewerManis SantiagoAinda não há avaliações
- MalariaDocumento11 páginasMalariaGaro AllieAinda não há avaliações
- Epidemiology and Control of Malaria (With A Focus On Sub-Saharan Africa)Documento30 páginasEpidemiology and Control of Malaria (With A Focus On Sub-Saharan Africa)Suchie ILyasAinda não há avaliações
- Invited Speakers' Abstracts: Track 1: Infectious and Neglected DiseasesDocumento47 páginasInvited Speakers' Abstracts: Track 1: Infectious and Neglected DiseasesMiguel AlcaAinda não há avaliações
- Malaria: Key FactsDocumento7 páginasMalaria: Key FactseenAinda não há avaliações
- New and Improved MethodsDocumento16 páginasNew and Improved MethodsDegee GonzalesAinda não há avaliações
- WHO - MalariaDocumento7 páginasWHO - Malariareborn007Ainda não há avaliações
- Roll Back Malaria Supports Reducing Malaria Burden in PregnancyDocumento2 páginasRoll Back Malaria Supports Reducing Malaria Burden in PregnancyDesya SilayaAinda não há avaliações
- Insecticide ResistanceDocumento3 páginasInsecticide ResistanceGenniAinda não há avaliações
- Consensus On Malaria Control and Elimination in The Asia-PacificDocumento20 páginasConsensus On Malaria Control and Elimination in The Asia-PacificbondanrahmawatiAinda não há avaliações
- Expanded Program On ImmunizationDocumento7 páginasExpanded Program On ImmunizationVanessa Abboud100% (1)
- Malaria Prevention TreatmentDocumento6 páginasMalaria Prevention TreatmentjoelAinda não há avaliações
- Guidelines South African Guidelines For The Prevention of Malaria 2017 Final - zp135472Documento43 páginasGuidelines South African Guidelines For The Prevention of Malaria 2017 Final - zp135472Sudhakar Kuppireddy100% (1)
- Tropical Med Int Health - 2009 - Mendis - From Malaria Control To Eradication The WHO PerspectiveDocumento8 páginasTropical Med Int Health - 2009 - Mendis - From Malaria Control To Eradication The WHO PerspectiveDircia D'silvaAinda não há avaliações
- Malaria in SE Asia Region: Myths, Realities, and the Need for a Paradigm ShiftDocumento3 páginasMalaria in SE Asia Region: Myths, Realities, and the Need for a Paradigm ShiftmonanarayanAinda não há avaliações
- Malaria JournalDocumento11 páginasMalaria JournalEstiPramestiningtyasAinda não há avaliações
- Malaria - Assignment'''''''workedDocumento10 páginasMalaria - Assignment'''''''workedEvans Danso100% (1)
- NIP2Documento52 páginasNIP2Angela Joy AmparadoAinda não há avaliações
- Ethiopia's Vector Control Manual for Malaria EliminationDocumento64 páginasEthiopia's Vector Control Manual for Malaria EliminationAbbi NathiAinda não há avaliações
- Emergency Plan Updated Rusaiffah CampDocumento42 páginasEmergency Plan Updated Rusaiffah CampiMaaz RameyAinda não há avaliações
- Youth culture and subcultures in EuropeDocumento15 páginasYouth culture and subcultures in EuropeDenisa IoanaAinda não há avaliações
- Youth Guide To The Global Fund To Fight Tuberculosis, Malaria and HIVDocumento44 páginasYouth Guide To The Global Fund To Fight Tuberculosis, Malaria and HIVAB-Ainda não há avaliações
- Budgetary Control Process at Vizag SteelDocumento96 páginasBudgetary Control Process at Vizag SteelP.lakshmanareddyAinda não há avaliações
- WHO 2019 NCoV SARI Toolkit 2020.1 EngDocumento196 páginasWHO 2019 NCoV SARI Toolkit 2020.1 EngIrinAinda não há avaliações
- Doh Community Health ProgramsDocumento48 páginasDoh Community Health ProgramsHope CarenaAinda não há avaliações
- Jurnal MalariaDocumento18 páginasJurnal MalariaFahmi Essa SyafriansyahAinda não há avaliações
- Malaria Manual of Procedures 2018Documento147 páginasMalaria Manual of Procedures 2018Jovie Anne CabangalAinda não há avaliações
- Epidemiological Perspective of Dengue - Sagar ParajuliDocumento31 páginasEpidemiological Perspective of Dengue - Sagar ParajuliSagar ParajuliAinda não há avaliações
- Prepared by Shanaz Marazi DPC Kupwara Under The Supervision of DTO Kupwara)Documento53 páginasPrepared by Shanaz Marazi DPC Kupwara Under The Supervision of DTO Kupwara)Mir JavidAinda não há avaliações
- Community Mobilisation and Participation in HealthDocumento33 páginasCommunity Mobilisation and Participation in HealthMayom MabuongAinda não há avaliações
- Communicable vs Non-Communicable DiseasesDocumento147 páginasCommunicable vs Non-Communicable Diseaseschristine gisembaAinda não há avaliações
- Financial Management of Not-for-Profit Organizations: White PaperDocumento9 páginasFinancial Management of Not-for-Profit Organizations: White PaperGaurav KushwahaAinda não há avaliações
- VaccinationDocumento28 páginasVaccinationM AQIB ASLAMAinda não há avaliações
- Universalimmunisationprogram 171120044520Documento22 páginasUniversalimmunisationprogram 171120044520Gagan GargAinda não há avaliações
- Project Augustine AbisolaDocumento59 páginasProject Augustine AbisolaRoseline Omoare100% (1)
- Awareness and Use of Malaria Prevention Measures Among Child-Bearing Aged Women in Jere Local Government Area, Borno State, NigeriaDocumento21 páginasAwareness and Use of Malaria Prevention Measures Among Child-Bearing Aged Women in Jere Local Government Area, Borno State, NigeriaIJMSRTAinda não há avaliações
- 2.dynamic of Diseases Transmission - Copy 2Documento54 páginas2.dynamic of Diseases Transmission - Copy 2Fatimah Abd-alhadiAinda não há avaliações
- Healthpromotlectamany 150627111718 Lva1 App6892Documento56 páginasHealthpromotlectamany 150627111718 Lva1 App6892B 70 Mohit KumarAinda não há avaliações
- Malaria Operational Manual 2009Documento275 páginasMalaria Operational Manual 2009Ram Mohan SAinda não há avaliações
- Malaria in PregnancyDocumento19 páginasMalaria in PregnancyOjambo FlaviaAinda não há avaliações
- Malaria Journal PDFDocumento10 páginasMalaria Journal PDFRuslan La Ane100% (1)
- Reproductive and Child HealthDocumento18 páginasReproductive and Child HealthSoumya BiswasAinda não há avaliações
- Seminar 1: Principles and Practices of Health PromotionDocumento46 páginasSeminar 1: Principles and Practices of Health PromotionFathir Iskandar100% (1)
- Malaria Control Program: Printer-Friendly PDFDocumento3 páginasMalaria Control Program: Printer-Friendly PDFdaryl ann dep-asAinda não há avaliações
- NVBDCPDocumento29 páginasNVBDCPMadathiparambil ManuAinda não há avaliações
- Child Immunization Coverage - A Critical Review: ArticleDocumento7 páginasChild Immunization Coverage - A Critical Review: ArticlenamitaAinda não há avaliações
- Epidemiological Perspective of Malaria - Sagar ParajuliDocumento27 páginasEpidemiological Perspective of Malaria - Sagar ParajuliSagar Parajuli100% (1)
- Communicable Disease GuideDocumento43 páginasCommunicable Disease Guiderceponelas1127Ainda não há avaliações
- Zika Virus: TransmissionDocumento3 páginasZika Virus: TransmissionMarlie VillanuevaAinda não há avaliações
- Physical Examination: Purpose of Newborn AssessmentDocumento16 páginasPhysical Examination: Purpose of Newborn AssessmentLiela B. SeveroAinda não há avaliações
- National Health Programmes in IndiaDocumento8 páginasNational Health Programmes in IndiaRohit SharmaAinda não há avaliações
- National Vector Borne Disease Control ProgrammeDocumento100 páginasNational Vector Borne Disease Control ProgrammeThe ThemerAinda não há avaliações
- Malaria Manual Final ReportDocumento64 páginasMalaria Manual Final ReportMaheshAinda não há avaliações
- Immunization and Its Importance: A Literature ReviewDocumento5 páginasImmunization and Its Importance: A Literature ReviewIJRASETPublicationsAinda não há avaliações
- Project Paper On Malaria: Department of Public HealthDocumento18 páginasProject Paper On Malaria: Department of Public HealthNikoAinda não há avaliações
- MALARIA: CAUSES, SYMPTOMS, DIAGNOSIS AND TREATMENTDocumento57 páginasMALARIA: CAUSES, SYMPTOMS, DIAGNOSIS AND TREATMENTsemere demissieAinda não há avaliações
- Public Health Approaches to Controlling MalariaDocumento24 páginasPublic Health Approaches to Controlling MalariaTanni ChowdhuryAinda não há avaliações
- Malaria in Pregnancy1Documento30 páginasMalaria in Pregnancy1ijojo elizabethAinda não há avaliações
- DSM Criteria For DiagnosisDocumento3 páginasDSM Criteria For DiagnosisnidakecilAinda não há avaliações
- DSM Criteria For DiagnosisDocumento3 páginasDSM Criteria For DiagnosisnidakecilAinda não há avaliações
- Awakenings AnalysisDocumento1 páginaAwakenings AnalysisJovelyn BucsitAinda não há avaliações
- Idiomatic ExpressionDocumento6 páginasIdiomatic ExpressionJovelyn BucsitAinda não há avaliações
- Seasonal PatternsDocumento5 páginasSeasonal PatternsJovelyn BucsitAinda não há avaliações
- Malaria Treatment Guideline 2012Documento38 páginasMalaria Treatment Guideline 2012van_cristiano100% (3)
- Epidemiology Prevention & Control of Malaria: Dr. Neha Tyagi Assistant Professor Department of Community MedicineDocumento29 páginasEpidemiology Prevention & Control of Malaria: Dr. Neha Tyagi Assistant Professor Department of Community MedicineShashi TyagiAinda não há avaliações
- Micro-Para Answer Key-PINK PACOPDocumento31 páginasMicro-Para Answer Key-PINK PACOPArk Olfato ParojinogAinda não há avaliações
- Manual For The Laboratory Diagnosis of Malaria.Documento126 páginasManual For The Laboratory Diagnosis of Malaria.Mustafa Khandgawi100% (1)
- Tugas Bahasa Inggris Progsus s1 KeperrawatanDocumento15 páginasTugas Bahasa Inggris Progsus s1 Keperrawatanida alifiuAinda não há avaliações
- Asymptomatic Malaria Infection and Associated Factors Among Blood Donors Attending Arba Minch Blood Bank, Southwest EthiopiaDocumento19 páginasAsymptomatic Malaria Infection and Associated Factors Among Blood Donors Attending Arba Minch Blood Bank, Southwest EthiopiaDella Retno NingrumAinda não há avaliações
- WHO Global Malaria Program AchievementsDocumento74 páginasWHO Global Malaria Program AchievementsMary Ruth Aujero Sanchez-Benzon100% (1)
- Wa0045Documento96 páginasWa0045Nasser HashimAinda não há avaliações
- Class 12Documento4 páginasClass 12royAinda não há avaliações
- Guidelines Malaria Di MalaysiaDocumento61 páginasGuidelines Malaria Di MalaysianalmifaAinda não há avaliações
- Malaria & Cerebral Malaria: Livia Hanisamurti, S.Ked 71 2018 045Documento40 páginasMalaria & Cerebral Malaria: Livia Hanisamurti, S.Ked 71 2018 045Livia HanisamurtiAinda não há avaliações
- Parasitology Micro D&R AgamDocumento108 páginasParasitology Micro D&R AgamNirosha Arul100% (1)
- Plasmodium Malariae: Parasite and Disease: William E. Collins and Geoffrey M. JefferyDocumento14 páginasPlasmodium Malariae: Parasite and Disease: William E. Collins and Geoffrey M. JefferyReynaldi FirmansyahAinda não há avaliações
- Mastoiditis Infection Behind EarDocumento5 páginasMastoiditis Infection Behind EarRhea SaglesAinda não há avaliações
- ZOOLOGY PREVIOUS EAMCET QUESTIONSDocumento2 páginasZOOLOGY PREVIOUS EAMCET QUESTIONSGaganpreetSinghAinda não há avaliações
- Article 47162Documento9 páginasArticle 47162Annisa FadillahAinda não há avaliações
- MalariaDocumento17 páginasMalariaDestri NeliAinda não há avaliações
- DUMMYS153 : Centre LPL - Production Test CollectionDocumento2 páginasDUMMYS153 : Centre LPL - Production Test Collectionvinaykumar reddiAinda não há avaliações
- ParasitologyDocumento27 páginasParasitologyDreyden HaloAinda não há avaliações
- The Life Cycle & The Transmission Dynamic Versi 1Documento14 páginasThe Life Cycle & The Transmission Dynamic Versi 1rayAinda não há avaliações
- Chapter 8 Infectious Diseases Robbins and Cotran Pathologic Basis of DiseaseDocumento12 páginasChapter 8 Infectious Diseases Robbins and Cotran Pathologic Basis of DiseaseArun Nayak86% (7)
- Malaria Elimination Lab Diagnosis Quality Assurance Manual 2Documento52 páginasMalaria Elimination Lab Diagnosis Quality Assurance Manual 2Abbi Nathi100% (1)
- Problems On EpidemiologyDocumento146 páginasProblems On EpidemiologyAnnie HadassahAinda não há avaliações
- Malaria in JordanDocumento6 páginasMalaria in JordanLucas TobingAinda não há avaliações
- Patogenesis Malaria - Dr. A. Visi Kartika, SP - PADocumento26 páginasPatogenesis Malaria - Dr. A. Visi Kartika, SP - PAahmadyawidyatmaAinda não há avaliações
- Comparative Analysis of Nested PCR and Conventional Microscopic Examination With MalariaDocumento59 páginasComparative Analysis of Nested PCR and Conventional Microscopic Examination With MalariaRAHMA TRIYANAYAinda não há avaliações
- Ashley2018 Lancet - MALARIA PDFDocumento14 páginasAshley2018 Lancet - MALARIA PDFAngel Orlando LanderAinda não há avaliações
- Dr. Ali’s Uworld Notes For Step 2 CK Infectious DiseasesDocumento40 páginasDr. Ali’s Uworld Notes For Step 2 CK Infectious Diseasesmarina shawkyAinda não há avaliações
- Rabies, Malaria, Tetanus PSBIM Review 2014Documento52 páginasRabies, Malaria, Tetanus PSBIM Review 2014Argyll Lorenzo BongosiaAinda não há avaliações
- Sella Modul TropisDocumento34 páginasSella Modul TropissellasellaAinda não há avaliações