Escolar Documentos
Profissional Documentos
Cultura Documentos
The Effect of Sub Inguinal Varicocelectomy On Semen Parameters
Enviado por
Mohamed AlhawaryDescrição original:
Título original
Direitos autorais
Formatos disponíveis
Compartilhar este documento
Compartilhar ou incorporar documento
Você considera este documento útil?
Este conteúdo é inapropriado?
Denunciar este documentoDireitos autorais:
Formatos disponíveis
The Effect of Sub Inguinal Varicocelectomy On Semen Parameters
Enviado por
Mohamed AlhawaryDireitos autorais:
Formatos disponíveis
THE EFFECTS OF SUBINGUINAL VARICOCELECTOMY ON SEMEN PARAMETERS
ABSTRACT
Purpose: We studied the effect of varicocele ligation on Kruger strict morphology criteria and semen parameters in patients with infertility. Materials and Methods: A total of 90 patients diagnosed with varicoceles and a normal morphological sperm ratio of less than 14% were evaluated before and 6 months after varicocelectomy. Preoperatively and postoperatively sperm density, motility and morphology using Kruger strict criteria were analyzed. The Wilcoxon test was used to measure levels of statistical significance in all analyses. Results: Significant improvement in sperm concentration and motility was evident after varicocele ligation (p _0.0002 and _0.0001, respectively). Using the Kruger classification sperm morphology evaluation revealed a significant increase in the percent of normal forms, and of forms with head and acrosome defects (p _0.0001, _0.0014 and _0.0028, respectively). There were no concomitant changes in strict morphology in forms with mid piece and tail defects or immature forms (p _0.05). Of the 90 patients 18 (20%) achieved a successful full-term pregnancy, including 14 via natural cycle intercourse and 4 by intrauterine insemination. Conclusions: Surgical correction of varicocele was associated with significant improvement in density, motility and sperm morphology evaluated using the Kruger classification. Varicocele has been considered a reversible cause of male subfertility for more than 40 years.1 Varicocele is present in approximately 15% of the general population, in 19% to 41% of men with primary infertility and in 45% to 81% of men with secondary infertility.2, 3 More recent studies validate the observations of significant improvements in testicular size, histology, sperm density and motility after varicocelectomy.4 The effects of this operation on sperm morphology have been controversial, particularly since the criteria for detecting morphological improvement have not been considered objective.5 Sperm morphology according to Papanicolaou staining modified for spermatozoa has been a standard component of routine semen analysis according to WHO criteria.6 However, numerous studies suggest that assessing sperm morphology using additional criteria may be a significant predictor of the fertilization rate in vitro.7 Use of the Kruger strict criteria to characterize sperm morphology has become the gold standard at many laboratories since its introduction.8, 9 We retrospectively analyzed 90 patients who underwent semen evaluation in regard to sperm parameters and sperm morphology, which was assessed by Kruger morphological criteria before and after subinguinal varicocelectomy. Since existing data on the effects of varicocelectomy on sperm morphology according to Kruger principles is lacking, we performed
this study to evaluate the effects of subinguinal varicocelectomy on sperm parameters. PATIENTS AND METHODS A total of 90 male partners of couples with a history of primary infertility for at least 1 year, varicocele and a normal morphological sperm ratio of less than 14% were included in this study at the Gulhane Military Medical Academy hospital andrology clinic and in vitro fertilization unit between September 1997 and June 2001. To exclude female factors a gynecologist evaluated the female partners. A detailed history and physical examination were performed in all patients. Varicocele diagnosed by physical palpation with the patient standing with and without the Valsalva maneuver was confirmed by color Doppler ultrasound. Varicocele size was classified as large (grade III), moderate (grade II) and small (grade I). Varicoceles were graded subclinical when palpation was negative but color Doppler ultrasound was positive. When there was no more than a 20% difference in Kruger spermiography results, spermiography was performed at least twice in separate samples preceding surgery and the mean values were calculated to serve as the preoperative value. When values differed by more than 20%, a third test was done.10 Semen analyses were done in the first 6 cases a minimum of 3 months after varicocele repair but semen analyses and semen samples in these cases were repeated at month 6 to ensure standardization. All semen samples were obtained by masturbation after 3 days of sexual abstinence and analyzed after liquefaction according to WHO guidelines. 10 Sperm motility and density were determined using a Makler chamber at 20_ magnification. Motile and immotile sperm were scored to determine motility using a hand counter. The quality of forward movement of the sperm was scored in 4 groups, including score asperm moving in a straight line with high speed, score bsperm moving in a reasonably straight line with moderate speed, score csperm moving with a slow, meandering forward progression and score dsluggish or nonprogressive movement, or no motility.4 While interpreting motility in our study, we included preoperative and postoperative differences of scores a plus b preceding and after the operation. Sperm morphology was evaluated by examining stained smears of 5 to 10 _l. semen. All samples were assessed using the Kruger classification. Staining was performed using the Diff Quick staining kit (Baxter Healthcare Corp., Miami, Florida). Briefly, slides were fixed with Diff Quick fixative for 15 seconds, stained with Diff Quick solution I for 10 seconds and finally stained with Diff Quick solution II for 5 seconds. Excessive stain is removed immediately by applying distilled water to the end of the slides. The slides are dried at room temperature. Using these criteria spermatozoa are considered normal when the head has a smooth oval configuration
with a well defined acrosome involving 40% to 70% of the sperm head, there are absent neck, mid piece and tail defects, and there are no cytoplasmic droplets of more than half the size of the sperm head. The length of the sperm head should be 5 to 6 _m. and the diameter should be 2.5 to 3.5 _m. The classification is such that borderline normal forms are considered abnormal. All morphological evaluations of Kruger stained slides were performed within 24 hours of sample technician collection in blinded fashion. At least 200 spermatozoa were evaluated at 1,000_ magnification using bright filled illumination. Evaluation was done by 1 of 2 trained technicians with samples assigned at random. Morphology evaluation was periodically monitored by 2 technicians using sets of 3 slides from various donors. The samples were assigned a code number and evaluated every other week on a regular basis, which was considered an appropriate way of introducing routine quality control into the assessment of sperm morphology. Differences between 10% and 20% in readings of the same sample were considered acceptable.8, 9 In addition, readings of the same sample by each of the 2 technicians were compared and differences no greater than 20% were noted. Modified subinguinal varicocelectomy using spinal anesthesia with preservation of the spermatic artery and lymphatic glands was performed in all patients. When present, external venous collaterals were ligated. Under 3.5_ loupe magnification the dilated internal spermatic veins were doubly ligated with 2-zero silk suture. No attempt was made to deliver the testis. All procedures were performed by same urologist (Y. K.). Preoperatively the patients were stratified according to sperm concentration into 3 groups, including group 1sperm concentration greater than 20 million per ml., group 2between 5 and 20 million sperm per ml. and group 3less than 5 million sperm per ml. A sperm concentration exceeding 20 million per ml., sperm motility 50% or greater with forward progression (score a _ b) and greater than 14% by the Kruger classification were considered normal. Followup assessment was done by chart review and telephone. The information included details on patient history and physical examination, semen parameters and pregnancy outcome (spontaneous and/or assisted). The mean interval between varicocele repair and mean followup was 18 months (range 12 to 28). Average values of semen parameters in the study group are expressed as the mean plus or minus standard error. Differences in sperm density, motility and morphology before and after subinguinal varicocelectomy were evaluated for significance using the nonparametric Wilcoxon signed rank test. RESULTS All men had primary infertility. Mean hospitalization was 1.2 day. Mean operative time was 45 minutes in unilateral and 75 minutes in bilateral varicocele cases. The mean age of the spouse was 26 _ 1.1 years (range 22 to 42). Varicocele was grades I to III in 16, 24 and 50 cases, respectively.
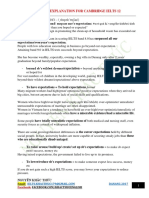
Grade I varicoceles were bilateral in 4 cases and on the left side in 12, grade II varicoceles were bilateral in 6 and on the left side in 18, and grade III varicoceles were on the right side in 4, left side in 36 and bilateral in 10. Median age and the mean duration of infertility were 26 (range 22 to 42) and 3.8 _ 1.0 years in the grade I, 27 (range 21 to 38) and 4.7 _ 1.6 years in the grade II, and 30 (range 22 to 36) and 5.1 _ 1.1 years in the grade III groups, respectively. Table 1 lists clinical varicocele grades and mean infertility times. Semen volume. Volume was 1 to 6 ml. Preoperative evaluation showed 2 cases (2.2%) of abnormally low ejaculate volume (range 1 to 1.5 ml.) and 1 (1.1%) of high volume (6 ml.). Volume in the remaining 87 cases was between 2 and 4 ml. These men with low ejaculate volume were excluded from data analysis. Preoperative mean semen volume was 2.8 _ 0.2 ml., which did not significantly differ from the postoperative value of 2.6 _ 0.3 ml. (p _0.05, table 2). Sperm concentration. Based on the preoperative concentrations 32, 30 and 28 patients were assigned to groups 1 to 3, respectively. All group 1 cases remained in group 1 postoperatively. Preoperative and postoperative mean sperm concentration in group A was 42.4 _ 3.1 million and 44.1 _ 3.5 million per ml., respectively. There was no statistical change postoperatively in patients with a preoperative sperm concentration of greater than 20 million per ml. (p _0.05). Of the 58 patients in groups 2 and 3, 44 (75.8%) improved to groups 1 and 2 after varicocelectomy, 23 who began in group 2 improved postoperatively to group 1, 5 remained in group 2 and 2 dropped to group 3. Eight of the 28 patients who began in group 3 improved to group 1, 13 improved to group 2 and 7 remained in group 3. The preoperative mean sperm concentration of 22.1 _ 4.2 million per ml. (range 6 million to 68 million) increased to 38.3 _ 6.1 million per ml. at postoperative month 6. Using the Wilcoxon signed rank test sperm concentration improved significantly after varicocelectomy (p _0.0002, table 2). Sperm motility. A total of 68 patients had abnormal sperm motility (score a _ b less than 50%, range 0% to 47%). Only 22 patients had normal sperm motility preoperatively. Mean sperm motility increased from 23.2% _ 2.2% to 45.1% _ 1.9% at postoperative month 6 (p _0.0001). Postoperative improvement was noted in 40 of the these 68 patients (58.8%) (table 2). Of the 68 men 20 showed no improvement after varicocelectomy, including 12, 6 and 2 with a sperm concentration of less than 5 million, between 5 and 20 million, and greater than 20 million per ml., respectively. Effects of varicocelectomy on Kruger morphology. Using the normal morphological sperm ratio of 14% according to the Kruger criteria all 90 patients had abnormal preoperative sperm morphology. There were fewer than 4% normal sperm forms less in 68 groups 1 and 2 patients, including 36 in group 1 with a normal morphological sperm ratio of 0% and 32 in group 2 with a ratio of 4% or less. In 22 men in group 3 the ratio was between 4% and 14%. The normal morphological sperm level increased from a mean of 2.6% _ 0.5% to 10.2% _ 0.9% at postoperative month 6.
Kruger morphology improved significantly after varicocele repair (p _0.0001). Forms with head defects decreased from a mean of 55.2% _ 3.4% to 22.7% _ 2.9% (p _0.0014). Forms with acrosomal defects also decreased from a mean of 16.8% _ 1.7% to 8.9% _ 0.8% (p _0.0028). On the other hand, the preoperative mean of 17.9% _ 0.9% of forms with mid piece defects was 18.2% _ 0.7% at postoperative month 6 (p _0.05). Before varicocele repair mean tail defective was 8.4% _ 1.1% and mean immature forms were 2.2% _ 0.8%, which changed to 7.0% _ 1.0% and 2.0% _ 0.9% after varicocelectomy, respecTABLE 1. General characteristics of the study population by grade Varicocele Size I II III No. pts. 16 24 50 Median age (range) 26 (2242) 27 (2138) 30 (2236) Mean yrs. infertility _ SD 3.8 _ 1.0 4.7 _ 1.6 5.1 _ 1.1 No. location: Rt. 0 0 4 Lt. 12 18 36 Bilat. 4 6 10 TABLE 2. Semen parameters before and after varicocelectomy Parameter Mean Preop. _ SD Mean 6 Mos. Postop. _ SD p Value Semen vol. (ml.) 2.8 _ 0.2 2.6 _ 0.3 _0.05 Sperm concentration (million/ml.) 22.1 _ 4.2 38.3 _ 6.1 _0.0002 % Sperm motility 23.2 _ 2.2 45.1 _ 1.9 _0.0001 TABLE 3. Sperm morphology evaluated using the Kruger classification in the study group before and after varicocelectomy Forms Mean % Preop. _ SD Mean % 6 Mos. Postop. _ SD p Value Normal morphology 2.6 _ 0.5 10.2 _ 0.9 _0.0001 Head defects 55.2 _ 3.4 22.7 _ 2.9 _0.0014 Acrosomal defects 16.8 _ 1.7 8.9 _ 0.8 _0.0028 Mid piece defects 17.9 _ 0.9 18.2 _ 0.7 _0.05 Tail defects 8.4 _ 1.1 7.0 _ 1.0 _0.05 Immature/other 2.2 _ 0.8 2.0 _ 0.9 _0.05 TABLE 4. Preoperative and postoperative ratio of morphologically normal sperm according to strict morphological criteria Group Ratio (%) No. Preop. No. 6 Mos. Postop.
1 0 36 4 2 4 or Less 32 4 3 414 22 52 (26 _ 10 _ 8 _ 8) 4 14 or Greater 0 30 (6 _ 18 _ 6)
Você também pode gostar
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeNo EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeNota: 4 de 5 estrelas4/5 (5784)
- The Yellow House: A Memoir (2019 National Book Award Winner)No EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Nota: 4 de 5 estrelas4/5 (98)
- Never Split the Difference: Negotiating As If Your Life Depended On ItNo EverandNever Split the Difference: Negotiating As If Your Life Depended On ItNota: 4.5 de 5 estrelas4.5/5 (838)
- The Emperor of All Maladies: A Biography of CancerNo EverandThe Emperor of All Maladies: A Biography of CancerNota: 4.5 de 5 estrelas4.5/5 (271)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceNo EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceNota: 4 de 5 estrelas4/5 (890)
- The Little Book of Hygge: Danish Secrets to Happy LivingNo EverandThe Little Book of Hygge: Danish Secrets to Happy LivingNota: 3.5 de 5 estrelas3.5/5 (399)
- Team of Rivals: The Political Genius of Abraham LincolnNo EverandTeam of Rivals: The Political Genius of Abraham LincolnNota: 4.5 de 5 estrelas4.5/5 (234)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaNo EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaNota: 4.5 de 5 estrelas4.5/5 (265)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryNo EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryNota: 3.5 de 5 estrelas3.5/5 (231)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureNo EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureNota: 4.5 de 5 estrelas4.5/5 (474)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersNo EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersNota: 4.5 de 5 estrelas4.5/5 (344)
- The Unwinding: An Inner History of the New AmericaNo EverandThe Unwinding: An Inner History of the New AmericaNota: 4 de 5 estrelas4/5 (45)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyNo EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyNota: 3.5 de 5 estrelas3.5/5 (2219)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreNo EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreNota: 4 de 5 estrelas4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)No EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Nota: 4.5 de 5 estrelas4.5/5 (119)
- Lecture 1: Newton Forward and Backward Interpolation: M R Mishra May 9, 2022Documento10 páginasLecture 1: Newton Forward and Backward Interpolation: M R Mishra May 9, 2022MANAS RANJAN MISHRAAinda não há avaliações
- B. Ing Kls 6Documento5 páginasB. Ing Kls 6siskaAinda não há avaliações
- IMM Indian Oil Case Group 3Documento13 páginasIMM Indian Oil Case Group 3Soniya AgnihotriAinda não há avaliações
- What is zone refining processDocumento1 páginaWhat is zone refining processKeshav MadanAinda não há avaliações
- Job Description Support Worker Level 1Documento4 páginasJob Description Support Worker Level 1Damilola IsahAinda não há avaliações
- 00 CCSA TestDocumento276 páginas00 CCSA TestPedro CubillaAinda não há avaliações
- Laws of MotionDocumento64 páginasLaws of MotionArnel A. JulatonAinda não há avaliações
- ME6404 Thermal EngineeringDocumento18 páginasME6404 Thermal EngineeringAnonymous mRBbdopMKfAinda não há avaliações
- Modul-Document Control Training - Agus F - 12 Juli 2023 Rev1Documento34 páginasModul-Document Control Training - Agus F - 12 Juli 2023 Rev1vanesaAinda não há avaliações
- How To Check PC Full Specs Windows 10 in 5 Ways (Minitool News)Documento19 páginasHow To Check PC Full Specs Windows 10 in 5 Ways (Minitool News)hiwot kebedeAinda não há avaliações
- JSA - 0026 Chipping & Granite cutting and lying Work At PB-19Documento2 páginasJSA - 0026 Chipping & Granite cutting and lying Work At PB-19Koneti JanardhanaraoAinda não há avaliações
- Ground Water Resources of Chennai DistrictDocumento29 páginasGround Water Resources of Chennai Districtgireesh NivethanAinda não há avaliações
- WassiDocumento12 páginasWassiwaseem0808Ainda não há avaliações
- Daftar PustakaDocumento4 páginasDaftar PustakaRamli UsmanAinda não há avaliações
- Inbound 9092675230374889652Documento14 páginasInbound 9092675230374889652Sean Andrew SorianoAinda não há avaliações
- Learning Stations Lesson PlanDocumento3 páginasLearning Stations Lesson Planapi-310100553Ainda não há avaliações
- ROPE TENSIONER Product-Catalog-2019Documento178 páginasROPE TENSIONER Product-Catalog-2019jeedanAinda não há avaliações
- VEGA MX CMP12HP Data SheetDocumento2 páginasVEGA MX CMP12HP Data SheetLuis Diaz ArroyoAinda não há avaliações
- Transformer Oil Testing MethodsDocumento10 páginasTransformer Oil Testing MethodsDEE TOTLVJAAinda não há avaliações
- Impact of Bap and Iaa in Various Media Concentrations and Growth Analysis of Eucalyptus CamaldulensisDocumento5 páginasImpact of Bap and Iaa in Various Media Concentrations and Growth Analysis of Eucalyptus CamaldulensisInternational Journal of Innovative Science and Research TechnologyAinda não há avaliações
- Unit 1 Writing. Exercise 1Documento316 páginasUnit 1 Writing. Exercise 1Hoài Thương NguyễnAinda não há avaliações
- Weir Stability Analysis Report PDFDocumento47 páginasWeir Stability Analysis Report PDFSubodh PoudelAinda não há avaliações
- Your Inquiry EPALISPM Euro PalletsDocumento3 páginasYour Inquiry EPALISPM Euro PalletsChristopher EvansAinda não há avaliações
- Reinvestment Allowance (RA) : SCH 7ADocumento39 páginasReinvestment Allowance (RA) : SCH 7AchukanchukanchukanAinda não há avaliações
- Henny Penny 500-561-600 TM - FINAL-FM06-009 9-08Documento228 páginasHenny Penny 500-561-600 TM - FINAL-FM06-009 9-08Discman2100% (2)
- Environmental Technology Syllabus-2019Documento2 páginasEnvironmental Technology Syllabus-2019Kxsns sjidAinda não há avaliações
- IELTS Vocabulary ExpectationDocumento3 páginasIELTS Vocabulary ExpectationPham Ba DatAinda não há avaliações
- Living Nonliving DeadDocumento11 páginasLiving Nonliving DeadArun AcharyaAinda não há avaliações
- Budget ControlDocumento7 páginasBudget ControlArnel CopinaAinda não há avaliações
- Rheology of Polymer BlendsDocumento10 páginasRheology of Polymer Blendsalireza198Ainda não há avaliações