Escolar Documentos
Profissional Documentos
Cultura Documentos
Reis and Nicolela Rates of Change in The Visual Field and Optic Disc in Patients With Distinct Patterns of Glaucoma To Us Optic Disc Damage Ophtalmology 2011
Enviado por
Alexandre ReisTítulo original
Direitos autorais
Formatos disponíveis
Compartilhar este documento
Compartilhar ou incorporar documento
Você considera este documento útil?
Este conteúdo é inapropriado?
Denunciar este documentoDireitos autorais:
Formatos disponíveis
Reis and Nicolela Rates of Change in The Visual Field and Optic Disc in Patients With Distinct Patterns of Glaucoma To Us Optic Disc Damage Ophtalmology 2011
Enviado por
Alexandre ReisDireitos autorais:
Formatos disponíveis
Rates of Change in the Visual Field and Optic Disc in Patients with Distinct Patterns of Glaucomatous Optic Disc
Damage
Alexandre S. C. Reis, MD,1,2 Paul H. Artes, PhD,1 Anne C. Belliveau, BSc,1 Raymond P. LeBlanc, MD,1 Lesya M. Shuba, MD, PhD,1 Balwantray C. Chauhan, PhD,1 Marcelo T. Nicolela, MD1
Purpose: To investigate the rate of visual eld and optic disc change in patients with distinct patterns of glaucomatous optic disc damage. Design: Prospective longitudinal study. Participants: A total of 131 patients with open-angle glaucoma with focal (n 45), diffuse (n 42), and sclerotic (n 44) optic disc damage. Methods: Patients were examined every 4 months with standard automated perimetry (SAP, SITA Standard, 24-2 test, Humphrey Field Analyzer, Carl Zeiss Meditec, Dublin, CA) and confocal scanning laser tomography (CSLT, Heidelberg Retina Tomograph, Heidelberg Engineering GmbH, Heidelberg, Germany) for a period of 4 years. During this time, patients were treated according to a predened protocol to achieve a target intraocular pressure (IOP). Rates of change were estimated by robust linear regression of visual eld mean deviation (MD) and global optic disc neuroretinal rim area with follow-up time. Main Outcome Measures: Rates of change in MD and rim area. Results: Rates of visual eld change in patients with focal optic disc damage (mean 0.34, standard deviation [SD] 0.69 dB/year) were faster than in patients with sclerotic (mean 0.14, SD 0.77 dB/year) and diffuse (mean 0.01, SD 0.37 dB/year) optic disc damage (P 0.003, KruskalWallis). Rates of optic disc change in patients with focal optic disc damage (mean 11.70, SD 25.5 10 3 mm2/year) were faster than in patients with diffuse (mean 9.16, SD 14.9 10 3 mm2/year) and sclerotic (mean 0.45, SD 20.6 10 3 mm2/year) optic disc damage, although the differences were not statistically signicant (P 0.11). Absolute IOP reduction from untreated levels was similar among the groups (P 0.59). Conclusions: Patients with focal optic disc damage had faster rates of visual eld change and a tendency toward faster rates of optic disc deterioration when compared with patients with diffuse and sclerotic optic disc damage, despite similar IOP reductions during follow-up. Financial Disclosure(s): Proprietary or commercial disclosure may be found after the references. Ophthalmology 2012;119:294 303 2012 by the American Academy of Ophthalmology.
Rates of visual eld and optic disc change are among the most relevant clinical parameters in the management of glaucoma, providing an indication of the adequacy of treatment and overall prognosis.13 Most patients with glaucoma show evidence of change if observed sufciently long enough. In some patients, these changes are detectable only after many years or even decades and may have minimal impact on quality of life. Other patients have rapid rates of change that cause a substantial risk of visual impairment. Glaucoma is a progressive optic neuropathy with a wide clinical spectrum, and patients vary with respect to the sensitivity to intraocular pressure (IOP), presence of other ocular and systemic risk factors, and overall prognosis of the disease.4 7 Although this diversity has been widely recognized, there have been relatively few attempts to identify subgroups of open-angle glaucoma (OAG) that have a more or less aggressive course of the disease.8 11
Different patterns of glaucomatous damage to the optic disc have been described.12,13 There are patients who develop a more focal loss of tissue in the optic disc,14,15 which occurs from within the cup (notch) and is more frequently identied at the superior and inferior poles. The remaining neuroretinal rim is usually well preserved. Other patients have a more diffuse loss of rim tissue, with concentric cup enlargement, and no localized areas of loss or pallor.16 A third common pattern is sclerotic, where the optic disc cup is characteristically saucerized, which refers to a shallow cupping extending to the disc margins with retention of a central pale cup. This type of damage is associated with marked areas of peripapillary atrophy and choroidal sclerosis.17 Examples of these patterns of optic disc damages are shown in Figure 1. We undertook this study to investigate the rates of change in glaucomatous patients with these 3 distinct patISSN 0161-6420/12/$see front matter doi:10.1016/j.ophtha.2011.07.040
294
2012 by the American Academy of Ophthalmology Published by Elsevier Inc.
Reis et al
Rates of Change in Different Disc Phenotypes
terns of optic disc damage (i.e., focal, diffuse, and sclerotic) when treated according to current Canadian guidelines for the management of glaucoma.18 20
Materials and Methods
Study Design and Material
Patients with OAG were recruited from the practices of 2 of the authors (M.T.N. and R.P.L). In accordance with the Declaration of Helsinki, all subjects gave informed consent to participate in the study, and the study was approved by the Research Ethics Review Board of the QEII Health Sciences Centre in Halifax, Nova Scotia. One author (M.T.N.), masked to patients identity and clinical information, reviewed optic disc stereo photographs of patients before their clinical visits and consecutively selected patients with optic disc damage characteristic of focal, diffuse, or sclerotic damage (Fig 1). The patterns of optic disc damage, as well as the intra- and interobserver agreement of its classication, have been discussed in detail elsewhere.13,21,22 Other inclusion criteria were a diagnosis of OAG, including primary, pseudoexfoliative, or pigmentary glaucoma; bestcorrected visual acuity 0.3 (20/40) logarithm of the minimum angle of resolution in the study eye; refraction within 6.00 diopters sphere and 3.00 diopters astigmatism; and visual eld damage, dened as a Glaucoma Hemield Test outside normal limits or a mean deviation (MD) worse than 2.0 dB. Exclusion criteria were concomitant ocular disease, systemic medication known to affect the optic nerve or visual eld, and an MD worse than 20.0 dB. If both eyes were eligible, 1 eye was randomly chosen as the study eye. Each selected patient underwent a comprehensive ophthalmologic examination during a baseline visit, including standard automated perimetry (SAP), confocal scanning laser tomography (CSLT), IOP measurement, corneal pachymetry, and stereoscopic optic disc photography. The baseline visit was followed by a second visit 1 month later, after which patients were examined every 4 months for a period of 4 years. Patients were treated according to a predened study protocol based on current Canadian guidelines for the management of glaucoma.18 20 The goal of the therapy was to decrease IOP by at least 30% from untreated levels or 21 mmHg, whichever was the lowest. Initially, the IOP was reduced by medical topical treatment. Subsequently, other forms of treatment, including laser trabeculoplasty and ltration surgery, could also be used. If, during the study, the disease had progressed according to the physicians judgment, a new target pressure was set.
Clinical Tests Included in this Current Analysis
Intraocular Pressure Measurements. Intraocular pressure was measured with Goldmann applanation tonometry (Haag-Streit, Kniz, Switzerland). The mean of 2 consecutive readings was recorded for analysis. The IOP measurements performed after ltration surgery were excluded from comparative analysis of IOP among the 3 groups. Untreated IOP, obtained from the clinical charts, was recorded for analysis. Reduction of IOP was dened as untreated IOP minus mean IOP during follow-up. Visual Field Assessment. Standard automated perimetry was performed using the Humphrey Field Analyzer (Carl Zeiss Meditec, Dublin, CA), SITA standard strategy, program 24-2. Two baseline visual elds were performed (baseline and 1-month visit) and at each follow-up visit thereafter. We used the MD to evaluate global rates of visual eld change. Only eyes with at least 5 visual eld tests were included in this analysis.
Figure 1. A, Focal optic disc damage with localized inferotemporal neuroretinal rim loss (notch), with the remaining neuroretinal rim relatively well preserved. B, Diffuse optic disc damage with uniformly enlarged and round cup, with no localized areas of neuroretinal rim tissue loss. C, Sclerotic optic disc damage with shallow and gently sloping cup, surrounded by peripapillary atrophy and with signs of choroidal sclerosis.
295
Ophthalmology Volume 119, Number 2, February 2012
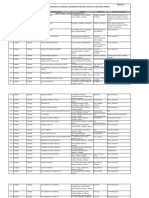
Table 1. Demographic and Clinical Data from Patients in Different Optic Disc Damage Groups
Total (n Female gender, n (%) Age (y), mean (SD) Diagnosis (POAG/PG/PXFG), n Follow-up (mos), mean (range) Untreated IOP (mm Hg), mean (SD) Baseline IOP (mm Hg), mean (SD) 131) Focal (n 45) Diffuse (n 42) Sclerotic (n 44) P value* 0.11 0.003 0.54 0.81 0.11 0.16 standard
67 (51%) 68.1 (11.3) 106/7/18 43.7 (1356) 24.8 (7.2) 16.0 (3.9)
27 (60%) 69.3 (11.8) 37/4/4 42.6 (1656) 24.0 (7.6) 15.2 (3.8)
16 (38%) 63.3 (11.5) 34/1/7 44.8 (1355) 26.6 (8.0) 16.7 (4.3)
24 (54%) 71.4 (8.9) 35/2/7 43.8 (2352) 24.0 (5.7) 16.3 (3.7) pseudoexfoliative glaucoma; SD
IOP intraocular pressure; PG pigmentary glaucoma; POAG primary open-angle glaucoma; PXFG deviation. *Pearsons chi-square test for categoric data and KruskalWallis test for continuous data. Refers to PXFG difference among the groups.
Confocal Scanning Laser Tomography. Confocal scanning laser tomography of the optic nerve head was performed with the Heidelberg Retina Tomograph II (Heidelberg Engineering GmbH, Heidelberg, Germany). Examinations were performed at baseline and at every visit during the follow-up period. One observer (ASCR) drew the contour lines in the baseline image. Images obtained after ltration surgery were excluded from the analysis to avoid artifactual increases in rim area induced by ltration surgery.23 To evaluate rates of optic disc change, we computed the global rim areas for each image using the xed standard reference plane.24 Only eyes with at least 5 scans were included in this analysis.
change observed in patients with glaucoma followed over time.31,32
Data Analysis
Analyses of categoric data were performed using Pearson chisquare tests, and continuous data were compared with Kruskal Wallis nonparametric analysis of variance. Multiple regression analyses were carried out to investigate the effects of baseline visual eld damage, baseline rim area, and age. Analyses were performed in R (R Foundation for Statistical Computing, Vienna, Austria, 2005). Robust regressions were computed with the lmrob function (R package robustbase, version 0.7-6).
Analysis of Rate of Change
Linear regression of MD and global rim area was performed with follow-up time as the independent variable, separately for each patient. Rates of change over the follow-up period (dB/year with MD and mm2 10 3/year with rim area) were estimated from the slope coefcient of the regression equation. Because ordinary least-squares regression is highly sensitive to outliers often present in clinical data,25,26 we used a recently developed robust regression technique that combines a high tolerance to outliers with high statistical efciency (MM estimation).2730 In brief, the method iteratively down-weights data points that appear inconsistent with the relationship between dependent and independent variables suggested by most other data points.30 Rapid rates of visual eld and optic disc change were dened as slopes more negative than 0.5 dB/year and 10.0 mm2 10 3/year with MD and rim area, respectively, statistically different from zero at a P value less than 0.05. These rates of change are approximately 5 times worse than the mean rate of
Results
A total of 131 eyes of 131 patients with OAG were enrolled in this study (45 with focal, 42 with diffuse, and 44 with sclerotic optic disc damage). Of these patients, 131 (100%) were included in visual eld analysis (at least 5 SAP tests) and 126 (96%) were included in the optic disc analysis (at least 5 CSLT tests). The 5 patients excluded from the optic disc analysis had ltration surgery before 5 scans were acquired. Table 1 summarizes the baseline information. Patients with diffuse optic disc damage were younger than those with focal and sclerotic damage (63.3 years vs. 69.3 and 71.4 years, respectively, P 0.003). Patients in the 3 groups had similar IOP reductions from untreated levels (38%, 37%, and 35%, in patients with focal, diffuse, and sclerotic optic disc damage, respectively, P 0.64), although patients with focal damage had lower mean IOP during follow-up (14.0 mm Hg vs. 15.5 and 15.1 mm Hg in patients with diffuse and sclerotic damage, respectively, P 0.02, Table 2).
Table 2. Intraocular Pressure (mm Hg) Characteristics, Number of Laser, and Filtration Surgery from Patients in Different Optic Disc Damage Groups
Total (n Mean IOP during follow-up (mm Hg), mean (SD) Absolute reduction of IOP (mm Hg), mean (SD) Relative reduction of IOP (%), mean (SD) Laser, n (%) Filtration surgery, n (%) 131) Focal (n 45) Diffuse (n 42) Sclerotic (n 15.1 (2.9) 8.9 (5.0) 35% (13%) 3 (7%) 8 (20%) 44) P value* 0.02 0.59 0.64 0.24 0.55
14.8 (2.8) 10.0 (7.0) 37% (16%) 15 (11%) 22 (17%)
14.0 (2.6) 10.0 (7.2) 38% (18%) 8 (18%) 9 (20%)
15.5 (2.5) 11.0 (8.5) 37% (16%) 4 (9%) 5 (12%)
IOP intraocular pressure; SD standard deviation. *Pearsons chi-square test for categoric data, KruskalWallis for continuous data. Argon laser trabeculoplasty and selective laser trabeculoplasty.
296
Reis et al
Rates of Change in Different Disc Phenotypes
Table 3. Characteristics of Standard Automated Perimetry and Confocal Scanning Laser Tomography Series
Total SAP Eyes (n) SAP examinations (n), median (range) MD baseline (dB), mean SD CSLT Eyes (n) CSLT examinations (n), median (range) Disc area baseline (mm2), mean (SD) Rim area baseline (mm2), mean (SD) CSLT confocal scanning laser tomography; MD *KruskalWallis test. 131 13 (516) 4.9 (3.8) 126 11 (514) 2.16 (0.40) 1.18 (0.28) Focal 45 13 (515) 6.7 (4.4) 43 11 (513) 2.03 (0.39) 1.14 (0.26) Diffuse 42 13 (514) 3.6 (3.0) 41 11 (714) 2.21 (0.38) 1.12 (0.28) Sclerotic 44 13 (816) 4.2 (3.2) 42 11 (513) 2.26 (0.40) 1.27 (0.29) standard deviation. P value*
0.001
0.04 0.05
mean deviation; SAP
standard automated perimetry; SD
Patients with focal optic disc damage had worse baseline MD ( 6.7 dB), followed by those with sclerotic ( 4.2 dB) and diffuse damage ( 3.6 dB, P 0.001). Patients with focal optic disc damage had smaller disc areas (2.03 mm2) compared with the others (2.21 and 2.26 mm2 for diffuse and sclerotic groups, respectively, P 0.04). In addition, the global rim area was larger in patients with sclerotic optic disc damage (1.27 mm2 vs. 1.14 and 1.12 mm2 for focal and diffuse groups, respectively, P 0.05, Table 3). Figure 2 and Table 4 show the rates of visual eld change in the 3 groups. The mean rate of visual eld change was fastest in patients with focal optic disc damage (mean 0.34, standard deviation [SD] 0.69 dB/year), followed by patients with sclerotic and diffuse optic disc damage (mean 0.14, SD 0.77 dB/year and mean 0.01, SD 0.37 dB/year, respectively, P 0.003). More patients with focal optic disc damage had rapid visual eld change (22% vs. 18% and 7% for sclerotic and diffuse, respectively, P 0.11), particularly compared with patients with diffuse damage. Because patients with diffuse damage were younger and had less advanced visual eld damage at baseline, age and baseline MD were entered as covariates in a multiple regression analysis to minimize potentially confounding effects (Table 5). This did not alter the ndings. Rates of visual eld change were not related to baseline MD (P 0.57) but were weakly related to age (P 0.08). However, given the small effect of age on the rates of change (Table 5), the difference in age between patients with focal damage and those with diffuse damage (6.0 years) did not fully explain the more negative slopes in patients with focal damage (mean difference between those with focal and diffuse damage, 0.35 dB/year). Figure 3 and Table 4 show the rates of optic disc change in the 3 groups. The rate of optic disc change was fastest in patients with focal optic disc damage (mean 11.70, SD 25.5 10 3 mm2/ year), followed by patients with diffuse and sclerotic optic disc damage (mean 9.16, SD 14.9 10 3 mm2/year and mean 0.45, SD 20.6 10 3 mm2/year, respectively), although the differences among the 3 groups did not achieve statistical significance (P 0.11). More patients with focal damage had rapid rim area change (27% vs. 17% and 14% for diffuse and sclerotic damage, respectively, P 0.35). Rates of rim area change were not related to age (P 0.89) or baseline rim area (P 0.79), and the differences among the 3 groups remained similar when these variables were entered as covariates in a multiple regression, with signicant differences particularly when comparing the rates of change from the focal and sclerotic groups (Table 5).
Case Examples
Figures 4 to 6 illustrate visual eld and optic disc change in 3 selected cases. Each example consists of plots of MD (dB) and global rim area (mm2) over time (years). In addition, visual elds (gray scale, total deviation, and pattern deviation probability maps) and CSLT (topography and reectance images) from the baseline, mid follow-up, and nal visits are presented. The corresponding dates are shown on the x-axis of the plots and indicated by open circles.
Discussion
Previous studies have shown that particular types of OAG are characterized by more rapid rates of change than others. A recent report from the Early Manifest Glaucoma Trial3 showed that patients with pseudoexfoliation had the fastest
Figure 2. Rates of MD change in patients with focal, diffuse, and sclerotic optic disc damage. The bold circles represent statistically signicant (P 0.05) negative or positive slopes, and the dashed line represents a criterion for rapid negative change ( 0.5 dB/year). The horizontal and vertical lines represent the means and their 95% condence intervals. dB decibels; MD mean deviation.
297
Ophthalmology Volume 119, Number 2, February 2012
Table 4. Mean Deviation (dB/Year) and Global Rim Area (mm2/Year 10 Damage Groups
Total Mean deviation slope (dB/y) Mean (SD) [95% CI] P value* Rapid rates of visual eld change, n (%) Global rim area slope (mm2/y 10 3) Mean (SD) [95% CI] P value* Rapid rates of optic disc change, n (%) 0.16 (0.65) [ 0.27 to 0.05] P 0.005 21 (16%) 7.12 (21.3) [ 10.8 to 3.4] 0.001 25 (20%) Focal 0.34 (0.69) [ 0.54 to 0.13] P 0.002 10 (22%) 11.70 (25.5) [ 19.5 to 3.8] 0.004 12 (27%)
3
Unit) Slopes from Patients in Different Optic Disc
Diffuse 0.01 (0.37) [ 0.11 to 0.12] P 0.861 3 (7%) 9.16 (14.9) [ 13.8 to 4.4] 0.001 7 (17%) Sclerotic 0.14 (0.77) [ 0.38 to 0.09] P 0.221 8 (18%) 0.45 (20.6) [ 6.7 to 6.0] 0.888 6 (14%) P Value 0.003
0.11 0.11
0.35
CI condence interval. *One-sample t test. Pearsons chi-square test for categoric data and KruskalWallis for continuous data.
rates of MD loss, and patients with normal tension glaucoma had the slowest rates of MD loss. As yet, few studies have compared rates of change in patients characterized by distinct morphologic patterns of optic disc damage.21 The current study investigated whether patients with focal, diffuse, and sclerotic optic disc damage have different rates of visual eld and optic disc change when treated similarly according to current guidelines.18 20 We observed differences in the rates of change among the 3 groups, despite similar IOP reductions from untreated levels. Patients with focal optic disc damage had the fastest rates of change in both visual eld and optic disc, although only the differences in visual eld rates were statistically signicant. This suggests that patients with focal optic disc damage may have more aggressive disease, possibly associated with nonIOP-related risk factors for progression, such as vasospasm and disturbed autoregulation.4,5 Other studies have suggested that focal optic disc damage is more common in women and that systemic risk factors, such as
Table 5. Multiple Regression of Visual Field and Optic Disc Rates of Change
Visual Field Rate of Change (dB/y) Estimate Diffuse, mean (SE)* Sclerotic, mean (SE)* Age, mean (SE) MD at baseline, mean (SE) RA at baseline, mean (SE) 0.27 (0.15) 0.19 (0.14) 0.01 (0.005) 0.01 (0.02) P Value 0.08 0.18 0.08 0.57 Optic Disc Rate of Change (mm2/y 10 3 unit) Estimate 2.7 (4.7) 10.9 (4.7) 0.02 (0.2) 1.8 (6.7) P value 0.57 0.02 0.89 0.79
migraine and peripheral vasospasm, are more prevalent in this group.12,13 In addition, optic disc hemorrhages are seen more frequently in patients with focal optic disc damage.7,14 The Collaborative Normal Tension Glaucoma Study demonstrated that female patients and patients with migraine benet from IOP reduction,33 and it is possible that patients with focal optic disc damage would benet from more aggressive IOP reduction than in the current study. However, this hypothesis still needs to be tested. Patients with sclerotic optic disc damage had the slowest rate of optic disc change. The loss of neuroretinal rim tissue in discs with sclerotic damage produces shallow cupping and gently sloping cup margins, in contrast with the deep and steep excavations observed with diffuse and focal damage.12 It is possible that these anatomic factors reduce
MD mean deviation; RA rim area; SE standard error. *Coefcients relate to differences compared with patients with focal optic disc damage. For each year older. For each dB worse. For each mm2 smaller.
Figure 3. Rates of rim area change in patients with focal, diffuse, and sclerotic optic disc damage. The bold circles represent statistically signicant (P 0.05) negative or positive slopes, and the dashed line represents a criterion for rapid rate of change ( 10.0 10 3 mm2/year). The horizontal and vertical lines represent the means and their 95% condence intervals.
298
Reis et al
Rates of Change in Different Disc Phenotypes
Figure 4. Left eye of a 59-year-old patient with focal optic disc damage. A, The MD changed rapidly ( 0.8 dB/year), and this was statistically signicant (P 0.001) despite large variability. B, The visual eld showed enlargement and deepening of existing scotomas in both superior and inferior hemields. C, The rate of change in rim area was slow ( 9.4 10 3 mm2/year) and not statistically different from zero (P 0.32). D, The topography image was consistent with a loss of rim tissue inferiorly. dB decibels; MD mean deviation.
the ability of CSLT to detect structural change in patients with sclerotic optic disc damage. Patients in this study were recruited consecutively, and therefore the groups were not identical in age, baseline visual eld loss, and baseline rim area. Because these differences might have inuenced the subsequent rates of change, we performed multiple regression analyses to minimize confounding effects on our analysis. Age marginally affected the rate of MD change (P 0.08) such that MD slopes were more negative by 0.01 dB/year for each year
of increasing age. By itself, this effect was too small to explain the substantial differences between the rates of change observed in this study. Rates of change with MD and rim area were not related to baseline values, and the latter had no meaningful effect on our results when they were included in a multiple regression analysis. In a previous study,21 our group reported that patients with sclerotic optic disc damage had the lowest incidence of visual eld and optic disc progression, with no apparent difference between patients with focal and diffuse optic disc
299
Ophthalmology Volume 119, Number 2, February 2012
Figure 5. Left eye of a 45-year-old patient with diffuse optic disc damage. A, The MD improved ( 0.4 dB/year, P 0.017). B, The visual eld showed a diffuse and apparently stable mild defect. C, There was a rapid and statistically signicant loss of rim area over time ( 57.3 10 3 mm2/year, P 0.001). The global rim area changed from 1.37 mm2 at baseline to 1.22 mm2 at last visit. D, The topography image showed a diffuse enlargement of optic disc cup over time. dB decibels; MD mean deviation.
damage. However, the cohort of that study had not been specically selected according to the pattern of optic disc damage. In contrast with the present study, the number of patients with specic patterns of damage was small, and patients were not treated according to a dened protocol. Moreover, our previous study reported on the incidence of progression with predened event-based end point criteria, rather than on rates of change as in the present report. Despite the differences in study design, the ndings of the current study agree with our previous results, particularly
with respect to optic disc changes, in that patients with sclerotic disc damage had the lowest rates of rim loss. This study evaluated rates of change based on global indices (MD and global rim area). These indices are most appropriate for measuring the overall speed of disease progression, but they are largely insensitive to localized change that are often the rst clinical signs of progression.34 The ability to measure change with a given test depends on the frequency of the examinations, variability of the measurements, and duration of follow-up.35 Perimetry is a subjec-
300
Reis et al
Rates of Change in Different Disc Phenotypes
Figure 6. Left eye of a 76-year-old patient with sclerotic optic disc damage. A, C, There was a rapid rate of change in both MD and rim area over time ( 0.7 dB/year and 27.1 10 3 mm2/year, respectively); both were statistically signicant (P 0.001 and P 0.021, respectively). B, D, The visual eld showed increasing loss superiorly, corresponding with a loss of neuroretinal rim area inferiorly. In addition, the area of peripapillary atrophy increased. dB decibels; MD mean deviation.
tive test and dependent on factors such as the patients reliability and fatigue. CSLT, though objective, is inuenced by the quality of the images.36,37 Functional and structural measurements vary from 1 examination to the next, even if no real change has taken place. In this study, we used 2 strategies to minimize this variability. First, in the CSLT analysis we used a reference plane xed to its position in the baseline image. This provides for lower variability of rim area measurements in longitudinal series.24 Second, by using a robust linear regression technique, we
minimized the effect of outliers on the estimated rates of change.30 The results of this study indicate that the morphologic type of optic disc damage may provide important clues on the speed of progression. A previous study demonstrated that experienced clinicians could distinguish between different patterns of optic disc damage with reasonable accuracy and precision.22 Identifying these morphologic optic disc types is feasible in clinical practice and might be clinically relevant.
301
Ophthalmology Volume 119, Number 2, February 2012
In conclusion, the present study demonstrated that patients with focal damage show signicantly more rapid visual eld deterioration and a trend toward faster optic disc deterioration. Patients with diffuse optic disc damage had the slowest rate of visual eld change, and patients with sclerotic optic disc damage had the slowest rate of optic disc change. These differences are likely to translate into different prognoses for patients with these distinct patterns of optic disc damage. Further work is needed to establish the mechanisms that cause different rates of functional and structural change in glaucoma in these patients.
management of glaucoma in the adult eye. Can J Ophthalmol 2009;44(Suppl):S793. LeBlanc RP. A Canadian glaucoma strategy. Can J Ophthalmol 2007;42:60 5. Damji KF, Behki R, Wang L, Target IOP Workshop participants. Canadian perspectives in glaucoma management: setting target intraocular pressure range. Can J Ophthalmol 2003; 38:189 97. Nicolela MT, McCormick TA, Drance SM, et al. Visual eld and optic disc progression in patients with different types of optic disc damage: a longitudinal prospective study. Ophthalmology 2003;110:2178 84. Nicolela MT, Drance SM, Broadway DC, et al. Agreement among clinicians in the recognition of patterns of optic disk damage in glaucoma. Am J Ophthalmol 2001;132:836 44. Lesk MR, Spaeth GL, Azuara-Blanco A, et al. Reversal of optic disc cupping after glaucoma surgery analyzed with a scanning laser tomograph. Ophthalmology 1999;106:1013 8. Poli A, Strouthidis NG, Ho TA, Garway-Heath DF. Analysis of HRT images: comparison of reference planes. Invest Ophthalmol Vis Sci 2008;49:3970 5. Owen VM, Strouthidis NG, Garway-Heath DF, Crabb DP. Measurement variability in Heidelberg Retina Tomograph imaging of neuroretinal rim area. Invest Ophthalmol Vis Sci 2006;47:532230. Liu X, Cheng G, Wu JX. Identifying the measurement noise in glaucomatous testing: an articial neural network approach. Artif Intell Med 1994;6:40116. Rousseeuw PJ, Yohai VJ. Robust regression by means of S-estimators. In: Franke J, Hardle W, Martin RD, eds. Robust and Nonlinear Time Series Analysis: proceedings of a workshop organized by the Sonderforschungsbereich 123 Stochastische Mathematische Modelle, Heidelberg 1983. New York: Springer-Verlag; 1984:256 76. Lecture Notes in Statistics, vol. 26. Available at: ftp://ftp.win.ua.ac.be/pub/preprints/84/ Robreg84.pdf. Accessed May 7, 2011. Salibian-Barrera M, Yohai VJ. A fast algorithm for S-regression estimates. J Comput Graph Stat 2006;15:414 27. Yohai VJ. High breakdown-point and high efciency estimates for regression. Ann Stat 1987;15:64256. Hubert M, Rousseeuw PJ, van Aelst S. High-breakdown robust multivariate methods. Stat Sci 2008;23:92119. See JL, Nicolela MT, Chauhan BC. Rates of neuroretinal rim and peripapillary atrophy area change: a comparative study of glaucoma patients and normal controls. Ophthalmology 2009; 116:840 7. Chauhan BC, Mikelberg FS, Artes PH, et al, Canadian Glaucoma Study Group. Canadian Glaucoma Study: 3. Impact of risk factors and intraocular pressure reduction on the rates of visual eld change. Arch Ophthalmol 2010;128:1249 55. Drance S, Anderson DR, Schulzer M. Risk factors for progression of visual eld abnormalities in normal-tension glaucoma. Am J Ophthalmol 2001;131:699 708. Wild JM, Hussey MK, Flanagan JG, Trope GE. Pointwise topographical and longitudinal modeling of the visual eld in glaucoma. Invest Ophthalmol Vis Sci 1993;34:190716. Chauhan BC, Garway-Heath DF, Goni FJ, et al. Practical recommendations for measuring rates of visual eld change in glaucoma. Br J Ophthalmol 2008;92:569 73. Tattersall CL, Vernon SA, Menon GJ. Mean deviation uctuation in eyes with stable Humphrey 24-2 visual elds. Eye (Lond) 2007;21:362 6. Strouthidis NG, White ET, Owen VM, et al. Factors affecting the test-retest variability of Heidelberg retina tomograph and Heidelberg retina tomograph II measurements. Br J Ophthalmol 2005;89:142732.
19. 20.
21.
22.
References
1. Artes PH, Chauhan BC. Longitudinal changes in the visual eld and optic disc in glaucoma. Prog Retin Eye Res 2005;24:33354. 2. Zeyen TG, Caprioli J. Progression of disc and eld damage in early glaucoma. Arch Ophthalmol 1993;111:625. 3. Heijl A, Bengtsson B, Hyman L, Leske MC, Early Manifest Glaucoma Trial Group. Natural history of open-angle glaucoma. Ophthalmology 2009;116:2271 6. 4. Fechtner RD, Weinreb RN. Mechanisms of optic nerve damage in primary open angle glaucoma. Surv Ophthalmol 1994; 39:23 42. 5. Harris A, Rechtman E, Siesky B, et al. The role of optic nerve blood ow in the pathogenesis of glaucoma. Ophthalmol Clin North Am 2005;18:34553, v. 6. Levin LA. Pathophysiology of the progressive optic neuropathy of glaucoma. Ophthalmol Clin North Am 2005;18:35564, v. 7. Shields MB. Normal-tension glaucoma: is it different from primary open-angle glaucoma? Curr Opin Ophthalmol 2008; 19:85 8. 8. Hitchings RA, Spaeth GL. The optic disc in glaucoma. I: Classication. Br J Ophthalmol 1976;60:778 85. 9. Spaeth GL, Hitchings RA, Sivalingam E. The optic disc in glaucoma: pathogenetic correlation of ve patterns of cupping in chronic open-angle glaucoma. Trans Sect Ophthalmol Am Acad Ophthalmol Otolaryngol 1976;81:21723. 10. Rahman R, Casson RJ, Gouveia SM, Salmon JF. Optic disc morphology on presentation of chronic glaucoma [letter]. Eye (Lond) 2002;16:6657. 11. Nakazawa T, Fuse N, Omodaka K, et al. Different types of optic disc shape in patients with advanced open-angle glaucoma. Jpn J Ophthalmol 2010;54:2915. 12. Broadway DC, Nicolela MT, Drance SM. Optic disk appearances in primary open-angle glaucoma. Surv Ophthalmol 1999;43(Suppl):S223 43. 13. Nicolela MT, Drance SM. Various glaucomatous optic nerve appearances: clinical correlations. Ophthalmology 1996;103:6409. 14. Geijssen HC, Greve EL. Focal ischaemic normal pressure glaucoma versus high pressure glaucoma. Doc Ophthalmol 1990;75:291301. 15. Spaeth GL. A new classication of glaucoma including focal glaucoma. Surv Ophthalmol 1994;38(Suppl):S9 17. 16. Pederson JE, Anderson DR. The mode of progressive disc cupping in ocular hypertension and glaucoma. Arch Ophthalmol 1980;98:490 5. 17. Geijssen HC, Greve EL. The spectrum of primary open angle glaucoma. I: Senile sclerotic glaucoma versus high tension glaucoma. Ophthalmic Surg 1987;18:20713. 18. Canadian Ophthalmological Society Glaucoma Clinical Practice Guideline Expert Committee. Canadian Ophthalmological Society evidence-based clinical practice guidelines for the
23. 24. 25.
26. 27.
28. 29. 30. 31.
32.
33. 34. 35. 36. 37.
302
Reis et al
Rates of Change in Different Disc Phenotypes
Footnotes and Financial Disclosures
Originally received: January 12, 2011. Final revision: July 11, 2011. Accepted: July 21, 2011. Available online: November 30, 2011.
1
Financial Disclosure(s): The author(s) have made the following disclosure(s): Dr. Chauhan, Heidelberg Engineering (research support). Manuscript no. 2011-57. Supported by grant MOP200309 from the Canadian Institute of Health Research (MTN); and Capes Foundation, Ministry of Educational of Brazil (ASCR). Correspondence: Marcelo T. Nicolela, MD, Department of Ophthalmology and Visual Sciences, Dalhousie University, 1276 South Park Street, Room 2035, Halifax, NS, Canada, B3H 2Y9. E-mail: nicolela@dal.ca.
Department of Ophthalmology and Visual Sciences, Dalhousie University, Halifax, Nova Scotia, Canada. Department of Ophthalmology, University of Sao Paulo, Sao Paulo, Brazil. Presented in part at: the annual meeting of the Association for Research in Vision and Ophthalmology, Fort Lauderdale, Florida, April 11, 2010.
303
Você também pode gostar
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeNo EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeNota: 4 de 5 estrelas4/5 (5794)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceNo EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceNota: 4 de 5 estrelas4/5 (895)
- The Yellow House: A Memoir (2019 National Book Award Winner)No EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Nota: 4 de 5 estrelas4/5 (98)
- The Little Book of Hygge: Danish Secrets to Happy LivingNo EverandThe Little Book of Hygge: Danish Secrets to Happy LivingNota: 3.5 de 5 estrelas3.5/5 (400)
- The Emperor of All Maladies: A Biography of CancerNo EverandThe Emperor of All Maladies: A Biography of CancerNota: 4.5 de 5 estrelas4.5/5 (271)
- Never Split the Difference: Negotiating As If Your Life Depended On ItNo EverandNever Split the Difference: Negotiating As If Your Life Depended On ItNota: 4.5 de 5 estrelas4.5/5 (838)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyNo EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyNota: 3.5 de 5 estrelas3.5/5 (2259)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureNo EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureNota: 4.5 de 5 estrelas4.5/5 (474)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryNo EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryNota: 3.5 de 5 estrelas3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnNo EverandTeam of Rivals: The Political Genius of Abraham LincolnNota: 4.5 de 5 estrelas4.5/5 (234)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaNo EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaNota: 4.5 de 5 estrelas4.5/5 (266)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersNo EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersNota: 4.5 de 5 estrelas4.5/5 (345)
- The Unwinding: An Inner History of the New AmericaNo EverandThe Unwinding: An Inner History of the New AmericaNota: 4 de 5 estrelas4/5 (45)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreNo EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreNota: 4 de 5 estrelas4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)No EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Nota: 4.5 de 5 estrelas4.5/5 (121)
- Cni Hosptl Network PDFDocumento33 páginasCni Hosptl Network PDFBrraghavan RaghavanAinda não há avaliações
- 3D-19001205-Adlyn Firdaus Sopyan-Kodifikasi-Tugas 2Documento3 páginas3D-19001205-Adlyn Firdaus Sopyan-Kodifikasi-Tugas 2Anis KhoirunisaAinda não há avaliações
- Superficial Corneal Injury and Foreign BodyDocumento1 páginaSuperficial Corneal Injury and Foreign BodyandinurulpratiwiAinda não há avaliações
- Clinical Profile of Ptosis in A Tertiary Care CentreDocumento5 páginasClinical Profile of Ptosis in A Tertiary Care CentreInternational Journal of Innovative Science and Research TechnologyAinda não há avaliações
- Eye Care IntroductionDocumento66 páginasEye Care IntroductionEdeti RoneAinda não há avaliações
- Retinal DetachmentDocumento19 páginasRetinal DetachmentJohn Hans CaturasAinda não há avaliações
- Ophthalmology 2Documento235 páginasOphthalmology 2yididiyagirma30Ainda não há avaliações
- Smile Versus LasikDocumento5 páginasSmile Versus LasikCindyAinda não há avaliações
- Icd 16 5 Eng V2.1 PDFDocumento2 páginasIcd 16 5 Eng V2.1 PDFNatalija Takač SadorskiAinda não há avaliações
- Astin, W., Mulyadi - 2016 - Pengaruh Penggunaan Alat Pelindung Mata Terhadap Ketajaman Penglihatan Pekerja Las Di Kecamatan Mandau, BengDocumento11 páginasAstin, W., Mulyadi - 2016 - Pengaruh Penggunaan Alat Pelindung Mata Terhadap Ketajaman Penglihatan Pekerja Las Di Kecamatan Mandau, BengWina Istana PratiwiAinda não há avaliações
- Opticians Scam People, Just Like The Optician in 2002. My Info Isn't and It's FreeDocumento29 páginasOpticians Scam People, Just Like The Optician in 2002. My Info Isn't and It's FreeKeith Cordier100% (1)
- Choice of Artificial Tear Formulation For Patients With Dry Eye: Where Do We Start?Documento5 páginasChoice of Artificial Tear Formulation For Patients With Dry Eye: Where Do We Start?Priscila Verduzco100% (1)
- Prometric Exam Ophthalmology 28-3-2013Documento10 páginasPrometric Exam Ophthalmology 28-3-2013Hasan Dahamsheh100% (4)
- Konjungtivitis Dan KeratitisDocumento117 páginasKonjungtivitis Dan KeratitisResti Puteri ApriyuslimAinda não há avaliações
- Goldmann Applanation Tonometry Without FluoresceinDocumento3 páginasGoldmann Applanation Tonometry Without FluoresceinClintAinda não há avaliações
- Clinical OCT Angiography Atlas PDFDocumento186 páginasClinical OCT Angiography Atlas PDFPop Ana-MariaAinda não há avaliações
- Teodora Alonso: No. 6 Calle Magallanes. at The End of The TermDocumento3 páginasTeodora Alonso: No. 6 Calle Magallanes. at The End of The TermJason Orolfo Salvadora HLAinda não há avaliações
- Schwind Cam Perfect Planning - Wide Range of Applications: Ork-Cam Presbymax Ptk-CamDocumento8 páginasSchwind Cam Perfect Planning - Wide Range of Applications: Ork-Cam Presbymax Ptk-CamThales FerreiraAinda não há avaliações
- Ophthalmology SlidesDocumento279 páginasOphthalmology SlidesWasfy NabilAinda não há avaliações
- Essilor VariluxDocumento53 páginasEssilor VariluxBdv RaoAinda não há avaliações
- Retinal Vascular Diseas E: Christine Anne D. EspejaDocumento25 páginasRetinal Vascular Diseas E: Christine Anne D. EspejaPaolo QuezonAinda não há avaliações
- Prevalence of Canine Cataract: Preliminary Results of A Cross-Sectional StudyDocumento7 páginasPrevalence of Canine Cataract: Preliminary Results of A Cross-Sectional StudydrdavidlwilliamsAinda não há avaliações
- Refractive Mgmt/Intervention: Question 1 of 90Documento39 páginasRefractive Mgmt/Intervention: Question 1 of 90NoorAinda não há avaliações
- Clinical Ophthalmology Made Easy®Documento419 páginasClinical Ophthalmology Made Easy®Uzair Akhter100% (2)
- PhacoemulsificationDocumento22 páginasPhacoemulsificationchQAinda não há avaliações
- I Notes Ophthalmology PDFDocumento690 páginasI Notes Ophthalmology PDFpriya arrachman0% (1)
- 04 - Assessment of Eyes & EarsDocumento62 páginas04 - Assessment of Eyes & Earsisrar88990% (1)
- Proceeding Book PVSM 2020Documento150 páginasProceeding Book PVSM 2020brahmani pitanatriAinda não há avaliações
- Why 25 CMDocumento13 páginasWhy 25 CMEgiAinda não há avaliações
- 34Documento2 páginas34Walisson BarbosaAinda não há avaliações