Escolar Documentos
Profissional Documentos
Cultura Documentos
Posterior Tibial Tendon Dysfunction
Enviado por
pioneers2011Descrição original:
Direitos autorais
Formatos disponíveis
Compartilhar este documento
Compartilhar ou incorporar documento
Você considera este documento útil?
Este conteúdo é inapropriado?
Denunciar este documentoDireitos autorais:
Formatos disponíveis
Posterior Tibial Tendon Dysfunction
Enviado por
pioneers2011Direitos autorais:
Formatos disponíveis
POSTERIOR TIBIAL TENDON DYSFUNCTION
ADULT ACQUIRED FLATFOOT
Tendons connect muscles to bones and stretch across joints, enabling you to bend that joint. One of the most important tendons in the lower leg is the posterior tibial tendon. This tendon starts in the calf, stretches down behind the inside of he ankle and attaches to bones in the middle of the foot. The posterior tibial tendon helps hold your arch up and provides support as you step off on your toes when walking. If this tendon becomes inflamed, over-stretched or torn, you may experience pain on the inner ankle and gradually lose the inner arch on the bottom of your foot, leading to flatfoot.
Signs
and symptoms of posterior tibial tendon dysfunction Pain and swelling on the inside of the ankle Loss of the arch and the development of a flatfoot Gradually developing pain on the outer side of the ankle or foot Weakness and an inability to stand on the toes Tenderness over the midfoot, especially when under stress during activity
Risk factors Posterior tibial tendon dysfunction often occurs in women over 50 years of age and may be due to an inherent abnormality of the tendon. But there are several other risk factors, including: Obesity Diabetes Hypertension Previous foot/ankle surgery or trauma Local steroid injections Inflammatory diseases such as rheumatoid arthritis, spondylosing arthropathy and psoriasis Athletes who are involved in sports such as basketball, tennis, soccer or hockey may tear the posterior tibial tendon. The tendon may also become inflamed if excessive force is placed on the foot, such as when running on a banked track or road.
_________________________________________________________________________________________________________________________ Brent D. Haverstock, DPM, FACFAS Podiatric Surgeon
Diagnosis The diagnosis is based on both a history and a physical examination. Your physician may ask you to stand on your bare feet facing away from him/her to view how your foot functions. As the condition progresses, the front of the affected foot will start to slide to the outside. From behind, it will look as though you have "too many toes" showing. You may also be asked to stand on your toes or to do a single heel rise: stand with your hands on the wall, lift the unaffected foot off the ground, and rise up on the toes of the other foot. Normally, the heel will rotate inward; the absence of this sign indicates posterior tibial tendon dysfunction. Your doctor may request X-rays, an ultrasound or a magnetic resonance image (MRI) of the foot. There are four stages of posterior tibial tendon dysfunction. Stage I The posterior tibial tendon is inflamed but has normal strength. There is little to no change in the arch of the foot. The patient can still perform a single-limb heel rise and has a flexible hindfoot. Orthotic treatment options include medial heel and sole wedges, arch support, and articulated AFOs The tendon is partially torn or shows degenerative changes and as a result loses strength. There is considerable flattening of the arch without arthritic changes in the foot. cannot perform single-limb heel rise. Pain is now present on the lateral aspect of the ankle. Orthotic treatment is the same as that in stage I, with the addition of more rigid arch supports. Results when the posterior tibial tendon is torn and not functioning. As a result the arch is completely collapsed with arthritic changes in the foot. solid ankle AFOs are suggested Is identical to stage three except that the ankle joint also becomes arthritic. With rigid AFO management as the orthotic treatment.
Stage II
Stage III
Stage IV
Treatment Without treatment, the flatfoot that develops from posterior tibial tendon dysfunction eventually becomes rigid. Arthritis develops in the hindfoot. Pain increases and spreads to the outer side of the ankle. The way you walk may be affected and wearing shoes may be difficult. The treatment your doctor recommends will depend on how far the condition has progressed. In the early stages, posterior tibial tendon dysfunction can be treated with rest, anti-inflammatory drugs such as aspirin or ibuprofen, and immobilization of the foot for 6 to 8 weeks with a rigid below-knee cast or boot to prevent overuse. After the cast is removed, shoe inserts such as a heel wedge or arch support may be helpful. If the condition is advanced, your doctor may recommend that you use a custom-made ankle-foot orthosis or support. Treatment of this condition begins with support of the foot. This is done with shoe modifications, orthotic arch support and, at times, a brace that is custom molded to the ankle. UCBL Orthotic The UCBL is a special orthotic which has a deeper heel cup and comes up higher in the arch. This is often referred to as a UCBL orthotic named after the lab where it was developed: The University of California Biomechanics Laboratory in San Francisco. It requires wearing a running shoe or lace-up casual shoe.
________________________________________________________________________________________________________________________ 2 Brent D. Haverstock, DPM, FACFAS Podiatric Surgeon
The Ritchie Brace The Ritchie Brace is a custom ankle brace (ankle foot orthosis/AFO) designed to treat chronic conditions of the foot and ankle. It has revolutionized the non-operative approach to the treatment of posterior tibial tendon dysfunction.
Surgical Reconstruction If conservative treatments don't work, your doctor may recommend surgery. Several procedures can be used to treat posterior tibial tendon dysfunction; often more than one procedure is performed at the same time. Your doctor will recommend a specific course of treatment based on your individual case. Surgical options include: Tenosynovectomy. In this procedure, the surgeon will clean away (debride) and remove (excise) any inflamed tissue surrounding the tendon. Osteotomy: This procedure changes the alignment of the heel bone (calcaneus). The surgeon may sometimes have to remove a portion of the bone. Tendon transfer: This procedure uses some fibers from another tendon (the flexor digitorum longus, which helps bend the toes) to repair the damaged posterior tibial tendon. Lateral column lengthening: In this procedure, the surgeon removes a small wedge-shaped piece of bone from the hip and places it into the outside of the calcaneus. This helps realign the bones and recreates the arch. Arthrodesis: This procedure welds (fuses) one or more bones together, eliminating movement in the joint. This stabilizes the hindfoot and prevents the condition from progressing further.
________________________________________________________________________________________________________________________ 3 Brent D. Haverstock, DPM, FACFAS Podiatric Surgeon
Você também pode gostar
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeNo EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeNota: 4 de 5 estrelas4/5 (5794)
- The Yellow House: A Memoir (2019 National Book Award Winner)No EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Nota: 4 de 5 estrelas4/5 (98)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceNo EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceNota: 4 de 5 estrelas4/5 (895)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersNo EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersNota: 4.5 de 5 estrelas4.5/5 (344)
- The Little Book of Hygge: Danish Secrets to Happy LivingNo EverandThe Little Book of Hygge: Danish Secrets to Happy LivingNota: 3.5 de 5 estrelas3.5/5 (399)
- The Emperor of All Maladies: A Biography of CancerNo EverandThe Emperor of All Maladies: A Biography of CancerNota: 4.5 de 5 estrelas4.5/5 (271)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaNo EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaNota: 4.5 de 5 estrelas4.5/5 (266)
- Never Split the Difference: Negotiating As If Your Life Depended On ItNo EverandNever Split the Difference: Negotiating As If Your Life Depended On ItNota: 4.5 de 5 estrelas4.5/5 (838)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryNo EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryNota: 3.5 de 5 estrelas3.5/5 (231)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureNo EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureNota: 4.5 de 5 estrelas4.5/5 (474)
- Team of Rivals: The Political Genius of Abraham LincolnNo EverandTeam of Rivals: The Political Genius of Abraham LincolnNota: 4.5 de 5 estrelas4.5/5 (234)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyNo EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyNota: 3.5 de 5 estrelas3.5/5 (2259)
- The Unwinding: An Inner History of the New AmericaNo EverandThe Unwinding: An Inner History of the New AmericaNota: 4 de 5 estrelas4/5 (45)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreNo EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreNota: 4 de 5 estrelas4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)No EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Nota: 4.5 de 5 estrelas4.5/5 (120)
- Reading Test 2Documento16 páginasReading Test 2AliMoazzam0% (1)
- Annisya Handini 1Documento15 páginasAnnisya Handini 1Hafidh Alyza RAinda não há avaliações
- House Hearing, 111TH Congress - Direct-To-Consumer Genetic Testing and The Consequences To The Public HealthDocumento233 páginasHouse Hearing, 111TH Congress - Direct-To-Consumer Genetic Testing and The Consequences To The Public HealthScribd Government DocsAinda não há avaliações
- ACute Pylonephris Case PresentationDocumento6 páginasACute Pylonephris Case PresentationbantilanAinda não há avaliações
- GTG 33 Pcos 2014Documento15 páginasGTG 33 Pcos 2014Juan SetiajiAinda não há avaliações
- Wound Management Guide DigitalDocumento48 páginasWound Management Guide DigitalBrian NiuAinda não há avaliações
- Salicylate Intoxication in An Infant: A Case Report: Key PointsDocumento5 páginasSalicylate Intoxication in An Infant: A Case Report: Key PointsAna MariaAinda não há avaliações
- Safety Precautions For Attending Theocratic SchoolsDocumento2 páginasSafety Precautions For Attending Theocratic SchoolsRitaAinda não há avaliações
- Restrictive Lung DiseasesDocumento31 páginasRestrictive Lung DiseasesAnn FrancisAinda não há avaliações
- MST-2, 3 Ante and Postmortem ExaminationDocumento7 páginasMST-2, 3 Ante and Postmortem Examinationnimra100% (1)
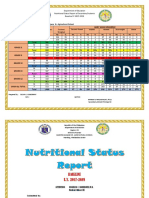
- Nutritional Status Report EndlineDocumento3 páginasNutritional Status Report EndlineOliva Cabrales CabornayAinda não há avaliações
- The Patient History An Evidence-Based Approach To Differential DiagnosisDocumento4 páginasThe Patient History An Evidence-Based Approach To Differential DiagnosisISAYK13% (8)
- DR Swamy PLAB Courses LTD.: Plab 1 Mock Test: 5 March 2019 Time Allowed: 3HrsDocumento31 páginasDR Swamy PLAB Courses LTD.: Plab 1 Mock Test: 5 March 2019 Time Allowed: 3HrsSualeha SohailAinda não há avaliações
- Anatomical Zodiacal Degrees PDFDocumento6 páginasAnatomical Zodiacal Degrees PDFMaria Marissa100% (2)
- Sample Questions For HAAD Prometric and DHA For NursesDocumento46 páginasSample Questions For HAAD Prometric and DHA For NursesJaezelle Ella Sabale100% (4)
- Edge Booty WorkbookDocumento102 páginasEdge Booty WorkbookEricaBerger94% (16)
- RJP Volume5 Issue3 Pages79-97Documento20 páginasRJP Volume5 Issue3 Pages79-97IDERMAinda não há avaliações
- Ginger Powder and Lotion Mixture Body Wrap To Reduce Belly FatsDocumento25 páginasGinger Powder and Lotion Mixture Body Wrap To Reduce Belly FatsKleina MendozaAinda não há avaliações
- NURSING CARE PLAN of Hodgkin's Lymphoma: Assessment Nursing Diagnosis Planning Nursing Interventions Rationale EvaluationDocumento5 páginasNURSING CARE PLAN of Hodgkin's Lymphoma: Assessment Nursing Diagnosis Planning Nursing Interventions Rationale Evaluationjoyrena ochondraAinda não há avaliações
- Test IntegumentaryDocumento2 páginasTest IntegumentaryRoshann_Larano_48Ainda não há avaliações
- MEDL The Integumentary SystemDocumento37 páginasMEDL The Integumentary SystemEmil LacanilaoAinda não há avaliações
- Assessment of Chest and LungsDocumento23 páginasAssessment of Chest and LungsBaniwas Marie Agnes100% (1)
- And Treatment Blepharokeratoconjunctivitis in Children: DiagnosisDocumento5 páginasAnd Treatment Blepharokeratoconjunctivitis in Children: DiagnosislordaponkAinda não há avaliações
- Patellofemoral Pain SyndromeDocumento21 páginasPatellofemoral Pain SyndromeAdvanced Physiotherapy100% (1)
- History TakingDocumento2 páginasHistory TakingAmbar Rashid100% (1)
- Vax Consent FormDocumento4 páginasVax Consent FormGrace C.Ainda não há avaliações
- Managemnet Arterial UlcersDocumento24 páginasManagemnet Arterial UlcersMohamad Zulfikar100% (1)
- Vanderlind - 2021Documento14 páginasVanderlind - 2021Sergio GarcíaAinda não há avaliações
- PHYSICAL FITNESS and Self Testing ActivitiesDocumento13 páginasPHYSICAL FITNESS and Self Testing ActivitiesSydney VersozaAinda não há avaliações
- CDC Malaria Program 2021Documento2 páginasCDC Malaria Program 2021Susila100% (1)