Escolar Documentos
Profissional Documentos
Cultura Documentos
Dengue Febrile Syndrome: (Clinical Instructor)
Enviado por
Aira AbastillasDescrição original:
Título original
Direitos autorais
Formatos disponíveis
Compartilhar este documento
Compartilhar ou incorporar documento
Você considera este documento útil?
Este conteúdo é inapropriado?
Denunciar este documentoDireitos autorais:
Formatos disponíveis
Dengue Febrile Syndrome: (Clinical Instructor)
Enviado por
Aira AbastillasDireitos autorais:
Formatos disponíveis
Republic of the Philippines Southern Luzon State University College of Allied Medicine Lucban, Quezon A.Y.
2011-2012
Dengue Febrile Syndrome
A Case Study Presented to The Faculty of College of Allied Medicine Southern Luzon State University Lucban, Quezon
Submitted to:
Mr. Marc Oneel C. Alvarez (Clinical Instructor)
In Partial Fulfillment of the Requirements for the Subject Related Learning Experience
Submitted by:
Abastillas, Aira B. BSN III A Group 9
I.
OBJECTIVES A. General Objectives After establishing Nurse-Patient Interaction, thorough, keen and comprehensive physical assessment, providing care to the client and developing a careful study of the clients condition, the student will acquire appropriate knowledge, develop and utilize skills and enhance attitude through the proper use of nursing process as the basis of care and management of the patient with Dengue Febrile Syndrome
B. Specific Objectives On completion of this case study, the student will be able to: 1. Understand what Dengue Febrile Syndrome is. 2. Define the terminologies used in the case study 3. Identify its clinical manifestations 4. Establish a good and therapeutic nurse-patient interaction 5. To build a trusting relationship with both the patient and significant others. 6. Trace the pathophysiology of the disease 7. Recapitulate the anatomy and physiology of the body parts involved. 8. Determine the clients health status through: a. General and Demographic Data b. History of Present Illness c. Past Medical History d. Personal and Family History e. Physical Examination f. Course in the ward 9. Utilize skills in performing physical examination to the patient. 10. Analyze laboratory results and correlate it with patients condition 11. Familiarize self to some medical and diagnostic procedures related to the patients present condition. 12. Determine the relevance of the drugs or medication to the patient. 13. Formulate nursing diagnosis and provide necessary nursing
management and interventions 14. Determine the rationale behind the applied nursing interventions 15. Render quality-nursing care through implementation of the Nursing Care Plan 16. Evaluate effectiveness of Nursing Care Plan and medical management 17. Provide continuity of care by giving health teachings not only to patient but also as well the Significant Others.
II.
INTRODUCTION
Dengue fever is an infectious disease carried by mosquitoes and caused by any of four related dengue viruses. This disease used to be called breakbone fever because it sometimes causes severe joint and muscle pain that feels like bones are breaking, hence the name. Health experts have known about dengue fever for more than 200 years. Dengue fever is found mostly during and shortly after the rainy season in tropical and subtropical areas of Africa Southeast Asia and China India Middle East Caribbean and Central and South America Australia and the South and Central Pacific An epidemic in Hawaii in 2001 is a reminder that many states in the United States are susceptible to dengue epidemics because they harbor the particular types of mosquitoes that transmit it. Worldwide, more than 100 million cases of dengue infection occur each year. This includes 100 to 200 cases reported annually to the Centers for Disease Control and Prevention (CDC), mostly in people who have recently traveled abroad. Many more cases likely go unreported because some health care providers do not recognize the disease. During the last part of the 20th century, many tropical regions of the world saw an increase in dengue cases. Epidemics also occurred more frequently and with more severity. In addition to typical dengue, dengue hemorrhagic fever and dengue shock syndrome also have increased in many parts of the world. Dengue fever can be caused by any one of four types of dengue virus: DEN-1, DEN-2, DEN-3, and DEN-4. You can be infected by at least two, if not all four types at different times during your lifetime, but only once by the same type. You can get dengue virus infections from the bite of an infected Aedes mosquito. Mosquitoes become infected when they bite infected humans, and later transmit infection to other people they bite. Two main species of mosquito , Aedes aegypti and Aedes albopictus, have been responsible for all cases of dengue transmitted in this country. Dengue is not contagious from person to person. Symptoms of typical uncomplicated (classic) dengue usually start with fever within 5 to 6 days after you have been bitten by an infected mosquito and include High fever, up to 105 degrees Fahrenheit Severe headache Retro-orbital (behind the eye) pain
Severe joint and muscle pain Nausea and vomiting Rash The rash may appear over most of your body 3 to 4 days after the fever begins. You may get a second rash later in the disease. Symptoms of dengue hemorrhagic fever include all of the symptoms of classic dengue plus Marked damage to blood and lymph vessels Bleeding from the nose, gums, or under the skin, causing purplish bruises This form of dengue disease can cause death. Symptoms of dengue shock syndrome-the most severe form of dengue disease-include all of the symptoms of classic dengue and dengue hemorrhagic fever, plus Fluids leaking outside of blood vessels Massive bleeding Shock (very low blood pressure) This form of the disease usually occurs in children (sometimes adults) experiencing their second dengue infection. It is sometimes fatal, especially in children and young adults. III. ANATOMY AND PHYSIOLOGY
The Circulatory System
The Circulatory System is the main transportation and cooling system for the body. The Red Blood Cells act like billions of little UPS trucks carrying all sorts of packages that are needed by all the cells in the body. Instead of UPS, I'll call them RBC's. RBC's carry oxygen and nutrients to the cells. Every cell in the body requires oxygen to remain alive. Besides RBC's, there are also White Blood Cells moving in the circulatory system traffic. White Blood Cells are the paramedics, police and street cleaners of the circulatory system. Anytime we have a cold, a cut, or an infection the WBC's go to work.
The highway system of the Circulatory System consists off a lot of one way streets. The superhighways of the circulatory system are the veins and arteries. Veins are used to carry blood *to* the heart. Arteries carry blood *away* from the heart. Most of the time, blood in the veins is blood where most of the oxygen and nutrients have already been delivered to the cells. This blood is called deoxygenated and is very *dark* red. Most of the time blood in the arteries is loaded with oxygen and nutrients and the color is very *bright* red. There is one artery that carries deoxygenated blood and there are some veins that carry oxygenated blood. To get to the bottom of this little mystery we need to talk about the Heart and Lungs. The Heart This is a subject that is near and dear to my heart. The heart is a two sided, four chambered pump. It is made up mostly of muscle. Heart muscle is very special. Unlike all the other muscles in the body, the heart muscle cannot afford to get tired. Imagine what would happen if every 15 minutes or so the pump got tired and decided to take a little nap! Not a pretty sight. So, heart muscle is always expanding and contracting, usually at between 60 and 100 beats per minute. The right side of the heart is the low pressure side. Its main job is to push the RBC's, cargo bays mostly empty now, up to the lungs (loading docks and filling stations) so that they can get recharged with oxygen. Blood enters the right heart through a chamber called the Right Atrium. Atrium is another word for an 'entry room.' Since the right atrium is located *above* the Right Ventricle, a combination of gravity and an easy squeeze pushes the blood though the Tricuspid Valve into the right ventricle. The tricuspid valve is a valve made up of three 'leaflets' that allows blood to go from top to bottom in the heart but closes to prevent the blood from backing up into the right atrium when the right ventricle squeezes. After the blood is in the right ventricle, the right ventricle begins its contraction to push the blood out toward the lungs. Remember that this blood is deoxygenated. The blood leaves the right ventricle and enters the *pulmonary artery.* This artery and its two branches are the only arteries in the body to carry deoxygenated blood. Important: Arteries carry blood *away* from the heart. There is nothing in the definition that says blood has to be oxygenated. When the blood leaves the pulmonary arteries it enters *capillaries* in the lungs. Capillaries are very, very small blood vessels that act as the connectors between veins and arteries. The capillaries in the lungs are very special because they are located against the alveoli or air sacks. When blood in the capillaries goes past the air sacks, the RBC's pick up oxygen. The alveoli are like the loading docks where trucks pick up their load. Capillaries are so small, in some places, that only one RBC at a time can get through. When the blood has picked up its oxygen, it enters some blood vessels known as the *cardiac veins.* This is fully oxygenated blood and it is now in veins. Remember: Veins take blood to the heart. The cardiac veins empty into the *left atrium.* The left side of the heart is the high pressure side, its job is to push the blood out to the body. The left atrium sits on top of the *left ventricle* and is separated from it by the *mitral valve*. The mitral valve is named this because it resembles, to some people, a Bishop's Mitered Hat. This valve has the same function as the tricuspid valve, it prevents blood from being pushed from the left ventricle back up to the left atrium. The left ventricle is a very high pressure pump. Its main job is to produce enough pressure to push the blood out of the heart and into the body's circulation. When the blood leaves the left ventricle it enters the Aorta. There are valves located at the opening of the Aorta that prevent the blood from backing up into the ventricle. As soon as the blood is in the aorta, there are arteries called *coronary arteries* that take some of the blood and use it to nourish the heart muscle. Remember: the heart is like James
Brown, it's the hardest working muscle in the body (in case you don't know, James Brown says he's the hardest working man in show business). The Aorta and the Arterial System The aorta leaves the heart and heads toward, what else, the head. We have to keep our brains well nourished so we can make good grades in school. The arteries that take the blood to the head are located on something called the *aortic arch.* After the blood passes through the aortic arch it is then distributed to the rest of the body. The *descending aorta* goes behind the heart and down the center of the body. Sometimes, if you are lying flat on your back, you can look down toward your feet and actually see your abdomen pulsate with each heart beat. This pulsation is really the aorta throbbing with each heart beat. Do not be alarmed, this is normal. From the aorta, blood is sent off to many other arteries and arterioles (very small arteries) where it gives oxygen and nutrition to *every* cell in the body. At the end of the arterioles are, guess what, capillaries. The blood gives up its cargo as it passes through the capillaries and enters the venous system. The Venous System The venous system carries the blood back to the heart. The blood flows from the capillaries, to venules (very small veins), to veins. The two largest veins in the body are the *superior* and *inferior* vena cavas. The superior vena cava carries the blood from the upper part of the body to the heart. The inferior vena cava carries the blood from the lower body to the heart. In medical terms, *superior* means above and *inferior* means under. Many people believe that the blood in the veins is *blue*; it is not. Venous blood is really dark red or maroon in color. Veins do have a bluish appearance and this may be why people think venous blood is blue. Both the superior and inferior vena cava end in the right atrium. The superior vena cava enters from the top and the inferior vena cava enters from the bottom. Blood Function and Composition Blood facts Approximately 8% of an adult's body weight is made up of blood. Females have around 4-5 litres, while males have around 5-6 litres. This difference is mainly due to the differences in body size between men and women. Its mean temperature is 38 degrees Celcius. It has a pH of 7.35-7.45; making it slightly basic (less than 7 is considered acidic). Whole blood is about 4.5-5.5 times as viscous as water, indicating that it is more resistant to flow than water. This viscosity is vital to the function of blood because if blood flows too easily or with too much resistance, it can strain the heart and lead to severe cardiovascular problems. Blood in the arteries is a brighter red than blood in the veins because of the higher levels of oxygen found in the arteries. An artificial substitute for human blood has not been found. Functions of blood Blood has three main functions: > Transport
> Protection > Regulation. Protection Blood has several roles in inflammation: Leukocytes, or white blood cells, destroy invading microorganisms and cancer cells Antibodies and other proteins destroy pathogenic substances Platelet factors initiate blood clotting and help minimise blood loss Regulation Blood helps regulate: pH by interacting with acids and bases Water balance by transferring water to and from tissues Composition of blood Blood is classified as a connective tissue and consists of two main components: Plasma, which is a clear extracellular fluid Formed elements, which are made up of the blood cells and platelets The formed elements are so named because they are enclosed in a plasma membrane and have a definite structure and shape. All formed elements are cells except for the platelets, which tiny fragments of bone marrow cells. Formed elements are: Erythrocytes, also known as red blood cells (RBCs) Leukocytes, also known as white blood cells (WBCs) Platelets Blood Function and Composition White blood cells Granulocytes Agranulocytes Platelets Vascular spasm Platelet plug formation Coagulation Production of blood Haemopoiesis Erythropoesis Leukopoiesis Thrombopoiesis
Aging changes in the blood Platelets Platelets are small fragments of bone marrow cells and are therefore not really classified as cells themselves. Platelets have the following functions:
Secrete vasoconstrictors which constrict blood vessels, causing vascular spasms in broken blood vessels Form temporary platelet plugs to stop bleeding Secrete procoagulants (clotting factors) to promote blood clotting Dissolve blood clots when they are no longer needed Digest and destroy bacteria Secrete chemicals that attract neutrophils and monocytes to sites of inflammation Secrete growth factors to maintain the linings of blood vessels The first three functions listed above refer to important haemostatic mechanisms in which platelets play a role in during bleeding: vascular spasms, platelet plug formation and blood clotting (coagulation). Vascular spasm This is a prompt constriction of the broken blood vessel and is the most immediate protection against blood loss. Injury stimulates pain receptors. Some of these receptors directly innervate nearby blood vessels and cause them to constrict. After a few minutes, other mechanisms take over. Injury to the smooth muscle of the blood vessel itself causes a longer-lasting vasoconstriction where platelets release a chemical vasoconstrictor called serotonin. This maintains vascular spasm long enough for the other haemostatic mechanisms to come into play. Platelet plug formation Under normal conditions, platelets do not usually adhere to the wall of undamaged blood vessels, since the vessel lining tends to be smooth and coated with a platelet repellent. When a vessel is broken, platelets put out long spiny extensions to adhere to the vessel wall as well as to other platelets. These extensions then contract and draw the walls of the vessel together. The mass of platelets formed is known as a platelet plug, and can reduce or stop minor bleeding. Coagulation This is the last and most effective defence against bleeding. During bleeding, it is important for the blood to clot quickly to minimise blood loss, but it is equally important for blood not to clot in undamaged vessels. Coagulation is a very complex process aimed at clotting the blood at appropriate amounts. The objective of coagulation is to convert plasma protein fibrinogen into fibrin, which is a sticky protein that adheres to the walls of a vessel. Blood cells and platelets become stuck to fibrin, and the resulting mass helps to seal the break in the blood vessel. The forming of fibrin is what makes coagulation so complicated, as it involved numerous chemicals reactions and many coagulation factors. Production of blood Thrombopoiesis Thrombopoiesis refers to the production of platelets in the blood, because platelets used to be called thrombocytes. This starts when a haemocytoblast develops receptors for the hormone thrombopoietin which is produced by the liver and kidneys. When these receptors are in place, the haemocytoblast becomes a committed cell called a megakaryoblast. This replicates its DNA, producing a large cell called a megakaryocyte, which breaks up into tiny fragments that enter the bloodstream. About 25-40% of the platelets are stored in the spleen and released as needed. The remainder circulate freely in the blood are live for about 10 days.
IV.
OVERVIEW OF THE DISEASE
Review of Related Literature A. DEFINITION Dengue fever is an acute febrile disease caused by infection with one of the serotypes of dengue virus which is transmitted by mosquito genus Aedes. It refers to a benign form of disease with systemic symptoms, fever, and often rash associated with pain behind the eyes, the joints and bones. Dengue hemorrhagic fever is a severe, sometimes fatal manifestation of dengue virus infection characterized by a bleeding diathesis and hypovolemic shock. Etiologic agent 1. Flaviviruses 1,2,3,4, family of Togaviridae is small viruses that contain single strand RNA. 2. Arboviruses group B Mode of Transmission 1. By bite of an infected mosquito, principally the Aedes Egypti a. Aedes Egypti is a day biting mosquito (they appear two hours after sunrise and two hours before sunset). b. It breeds on stagnant water. c. It has limited and low flying movement d. It has fine white dots at the base of the wings; with white bands on the legs. 2. Aedesalbopictus may contribute to the transmission of dengue virus in rural areas. 3. Other contributory mosquitoes: a. Aedes polynensis b.Aedes scutellaris simplex Incubation period The incubation period is here or fourteen days; commonly seven to ten days. Period Of communicability 1. Patients are usually infected to mosquito from the day before the febrile period to the end of it. 2. The mosquito becomes infective from day 8 to 12 after the blood meal and remains infective all throughout life. Sources of infection 1. Infected persons- the virus is present in the blood of the patients during the acute phase of the disease and will become a reservoir of virus, sucked by mosquitoes which may then transmit the disease. 2. Standing water- any stagnant water along the household and premises are usual breeding places of these mosquitoes. Incidence 1. Age- Dengue fever may occur at any age, but it is common among children and peaks between 4 to years old. 2. Sex- Both sexes can be affected 3. Season- It is more frequent than rainy season. 4. Location- Dengue fever is more prevalent in urban communities Pathogenesis and Pathology 1. Infectious virus is deposited in the skin by the vector and initial replication occurs at the site of infection and in local lymphatic tissues. 2. Within a few days, viremia occurs, lasting until the fourth or fifth day after onset of symptoms. 3. Evidence indicates that macrophages are the principal sites of replication. 4. at the site of petechial rash, non-specific changes are noted which includes endothelial swelling, perivascular edema, and extravasation of blood.
5, there is marked increase in vascular permeability, hypotension, hemoconcentration, thrombocytopenia, with increased platelet agglutinability, and or moderate disseminated intravascular coagulation. 6. the most serious pathophysiological abnormality is hypovolemis shock resulting from increased permeability of the vascular endothelium and loss of plasma from the intravascular space. Clinical Manifestations A. Dengue Fever 1. Prodromal symptoms characterized by: a. malaise and anorexia up to 12 hours b. fever and chills accompanied by sever frontal headache, ocular pain, myalgia with severe backache, and athralgia 2. Nausea and vomiting 3. Fever is non-remitting and persists for three to seven days. 4. Rash is more prominent on the extremities and the trunk; it may involve the face in some isolated cases. 5. Petechiae usually appear near the end of the end of the febrile period and most common on the lower extremities. B. Dengue Hemorrhagic Fever This severe form of dengue virus infection is manifested by fever, hemorrhagic diathesis, and hepatomegally and hypovolemic shock. Phases of the Illnesses 1. Initial febrile phase lasting from 2 to 3days a. fever (39-40C) accompanied by headache b. febrile convulsions may appear c. palms and sole are usually flushed d. positive tourniquet test e. anorexia, vomiting, myalgia f. maculopapular or petechial rash may be present that usually starts in the distal portion of the extremities (sparing the axilla and chest), the skin appears purple with blanched areas with varied sizes, the Hermans sign known aspathognomonisto the disease. g. generalized or abdominal pain h. hemorrhagic manifestations like positive tourniquet test, purpura, epistaxis and gum bleeding may be present. 2. Circulatory Phase a. There is a fall of temperature accompanied by profound circulatory changes usually on the 3rd to 5th day. b. Patient becomes restless, with cool clammy skin.
c. Cyanosis is present. d. Profound thrombocytopenia accompanies the onset of shock. e. Bleeding diathesis may become more severe with GIT haemorrhage. f. Shock may occur due to loss of plasma from intravascular spaces and hemoconcentration with markedly elevated hematocrit is present. g. Pulse is rapid and weak; pulse pressure becomes narrow and blood pressure may drop to an unobtainable level. h. Untreated shock may result to comma, metabolic acidosis and death may occur within two days. i. With effective therapy, recovery may follow in two to three days. Classification According to Severity (Halstead & Nimmanitya) Grade I There is fever accompanied with non-specific constitutional symptoms and the only hemorrhagic manifestation is positive (+) in torniquet test. Grade II All signs of Grade I plus spontaneous bleeding from the nose, gums, GIT are present. Grade III There is the presence of circulatory failure as manifested by weak pulse, narrow pulse pressure, hypotension, cold clammy skin, and restlessness. Grade IV There is profound shock, undetectable blood pressure, and pulse. Complications 1. Dengue Fever a. Epistaxis; menorrhagia b. Gastrointestinal bleeding c. Concomitant gastrointestinal disorder (peptic ulcer) 2. DHF a. Metabolic acidosis b. Hyperkalemia c. Tissue anoxia d. Hemorrhage into the CNS or adrenal glands e. Uterine bleeding may occur f. Myocarditis 3. Severe manifestations
Dengue encephalopathy is manifested by increasing restlessness, apprehension or anxiety, disturbed sensorium, convulsions, spacity, and hyporeflexia.
Diagnostic Tests 1. Tourniquet Test- screening test, done by occluding the arm veins for about five minutes to detect capillary fragility. 2. Platelet count (decreased)-confirmatory test 3. Hemoconcentration-an increase of at least 20 percent in hematocrit or steady rises in hematocrit. 4. Occult blood 5. Hemoglobin determination
Treatment Modalities There is no effective antiviral therapy for dengue fever. Treatment is entirely symptomatic. 1. Analgesic drugs other than aspirin maybe required for relief of headache, ocular pain, and myalgia. 2. Initial phase may require intravenous infusion to prevent dehydration and replacement of plasma. 3. Blood transfusion is indicated in patient with severe bleeding. 4. Oxygen therapy is indicated to all patients in shock. 5. Sedatives maybe needed to allay anxiety and apprehension.
Prevention and Control 1. Early detection and treatment of cases will not worsen the victims condition 2. Treat mosquito nets with insecticides. 3. House spraying is advised. 4. Eliminate vector by: a. changing water and scrubbing sides of lower vases once a week. b. destroying the breeding places of mosquitoes by cleaning the surroundings, c. keeping the water containers covered. 5. Avoid too many hanging clothes inside the house
V.
CASE STUDY PROPER
General Data
Admission No Patients Name Ward Permanent Address Birth date Age Civil Status Birthplace Nationality Religion Admission Date Discharge Date Admitting Physician Attending Physician Chief complain Admitting Diagnosis Final Diagnosis
: : : : : : : : : : : : : : : : :
11089089 Y.S Infectious ward (Pedia ward) Brgy. 8 Lucena City July 7, 2006 5y/o child Lucena City Filipino Roman Catholic August 22, 2011 August 25, 2011 Dr. Toledo Dr. Tolentino On and off fever for 5 days DFS; UTI DFS; UTI
A. History of Present Illness: Patient Y.S is 5 years old from Lucena City. Last August 22, 2011 after suffering from on and off fever for the past 5 days his parents decided to have him admitted at Quezon Medical Center, as after he had his checkup from Dr. Gonzales his parents said that the fever did not subside and that they were scared because of the rising cases of dengue in their area. B. History of Past Illness: According to the patients SOs, the patient had suffered from colds and coughs but did not seek treatment but when the patient had suffered from fever, weeks before admission and they seek for consultation to Dra. Amor Gonzales, who ordered for diagnostic test such as CBC and UA. As stated by the SOs she prescribed co-trimoxazole as treatment after the result was obtained. C. Familial Health History: Through the interview the SOs stated that their family has a history of hypertension, UTI and DM. They also stated that Jay was the first one to have Dengue in their family. D. Personal and Social History: The patient is living a simple life. At his age of 5, he is into exploring and maintaining his social relationship with his playmates. According to his parents, Y.S spends most of his time playing with his playmates and with them.
E. Physical Assessment General Appearance Conscious and coherent Slightly pale in appearance Slightly weak in appearance
Vital signs Aug 22, 2011 Temp Pulse rate Respiration rate Blood Pressure 38.4C 96 bpm 32 bpm 80/60mmHg Aug 23, 2011 36.0C 84bpm 36bpm 90/60mmHg Aug 24, 2011 36.2C 86bpm 36bpm 80/60mmHg Aug 25, 2011 36.6C 94bpm 32bpm 80/60mmHg
Skin > > > Absence of cyanosis With dry skin With fair skin turgor
Head/Face > > > With good hair distribution No dandruffs and scalp damage noted With symmetrical facial features
Eyes > > > > > eyebrows evenly distributed, symmetrically aligned with equal movement eyelids intact, no discoloration and closes symmetrically With whitish sclera With pale conjunctiva With pupils equally round and reactive to light accommodation
Ears > > > > > With fair hearing ability Negative discharges No tenderness or pain upon palpation of the mastoid process auricles are mobile, firm, non-tender pinna recoils after folded
Nose > > > symmetrical with nasal septum intact and on midline No nasal flaring
> > > Chest > >
No discharges noted
Mouth/Throat with dry and pale lips tongue is in central position and moves freely
With symmetrical chest expansion upon breathing With clear breath sounds heard on both lung fields upon
auscultation Abdomen > > > > > > > VI. abdomen not enlarged with soft ,warm to touch and tender abdomen
Genito-urinary with a positive urine output with active bowel movement
Extremities With scars on both upper and lower extremities With slightly pale nailbeds on both upper and lower extremities With capillary refill time of 1-2 secs.
Laboratory Analysis and Examination
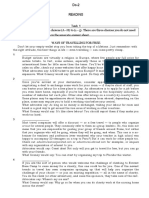
Date of Examination: August 23, 2011 Type of examination: Hematology
CBC Hemoglobin Hematocrit WBC Neutrophils Lymphocytes Platelet Count
RESULT 9-10 gm/L 33% 2,400 49 51 126,000
NORMAL VALUE 14.0-18 gm/L 40-50% 5,000-10,000/mm3 40-60 35-40 150,00-450,000
INTERPRETATION Below normal Below normal Infection Normal Infection Bleeding
Date of Examination: August 24, 2011 Type of examination: Hematology
CBC Hemoglobin Hematocrit WBC
RESULT 11.7 gm/L 35.1% 14,300
NORMAL VALUE 14.0-18 gm/L 40-50% 5,000-10,000/mm3
INTERPRETATION Below normal Below normal Infection
Neutrophils Lymphocytes Platelet Count
53 56 120,000
40-60 35-40 150,00-450,000
Normal Infection Bleeding
Date of Examination: August 25, 2011 Type of examination: Hematology
CBC Hemoglobin Hematocrit WBC Neutrophils Lymphocytes Platelet Count
RESULT 12.4 gm/L 27% 11,300 49 51 146,000
NORMAL VALUE 14.0-18 gm/L 40-50% 5,000-10,000/mm3 40-60 35-40 150,00-450,000
INTERPRETATION Below normal Below normal Infection Normal Infection Bleeding
Nursing Responsibilities: Infection Assessed the general condition of the patient Monitored v/s esp. Temp. Encouraged to do proper and frequent hand washing Instructed on proper way of food handling, preparation and storage Encouraged SO to keep surroundings clean Instructed to include green leafy vegetables and vit. C -rich foods Provided adequate rest and sleep Bleeding Assessed the general condition of the patient Monitored v/s esp. RR Reviewed the current laboratory result Instructed to SO to apply pressure on the bleeding site when bleeding occurred Encouraged SO to notify NOD if bleeding occurred Encouraged to do breathing exercises Provided adequate rest and sleep periods Encouraged to include iron-rich foods such as organ meat in diet when diet resumed Re-assessed the patient
Altered tissue perfusion
Assessed General condition Monitored v/s esp. RR Reviewed the current laboratory result Encouraged to have adequate fluid intake Encouraged to do breathing exercises Provide rest and sleep periods Encouraged to include iron-rich foods such as organ meat in diet when diet resumed Re-assessed the patient
Date of Examination: August 23, 2011 Type of Examination: Urinalysis Characteristics Color Normal Result Light straw Results to yellow Interpretation Normal
amber yellow Transparency PH Sugar Pus cells Clear 4.5-8.0 negative negative Slightly turbid 6.4 negative 5-10/Hpf Risk for infection Normal Normal Infection and pus formation Specific gravity RBC 1.005-1.030 Rare 1.015 2-4/Hpf normal Bleeding
Nursing Responsibilities: Infection Assessed the general condition of the patient Monitored v/s esp. Temp. Encouraged to do proper and frequent handwashing Instructed on proper way of food handling, preparation and storage Encouraged to keep surroundings clean Instructed to include green leafy vegetables and vit c-rich foods when diet resumed Provided adequate rest and sleep Bleeding Assessed the general condition of the patient Monitored v/s esp. RR Encouraged to include iron-rich foods such as organ meat in diet when diet resumed
Provided adequate rest and sleep periods Encouraged to do breathing exercises Administered iron supplement as ordered Reviewed the current laboratory result Re-assessed the patient
Acidosis Assessed the general condition of the patient Monitored v/s esp. Temp and RR Monitored intake and output Encouraged to increase fluid intake when diet resumed Instructed SO to never leave patient Reviewed the current laboratory result Re-assessed the patient
VII.
Course in the Ward
August 22, 2011
Patient Y.S was admitted at 1:45pm at Quezon Medical Center, Pedia ward, with a chief complaint of on and off fever for 5 days, under the request of his admitting physician Dr. Toledo. Upon the admission the consent was secured. Dr. Toledo, his admitting doctor ordered to monitor his vital signs, diet as tolerated and for a platelet count. An IV of PLR was hooked 1L x 12. Medication was also ordered such as: Paracetamol 250mg sup q4 for fever. Lastly, the doctor ordered to refer to the P- ROD. Later that day, after the platelet count result was obtained, an order of Diet as tolerated except highly colored food was ordered including to follow of 2nd PLR with same rate and diagnostic tests such as repeat CBC and PC tomorrow AM and for HHP monitoring OD. Medication were also ordered such as Ampicilin 400mg IV q6 ANST (-), Ranitidine 25mg IVP q8, OMX capsule 1 capsule BID, and Paracetamol 250mg/5ml syrup 3.5ml q4 for fever. Lastly, she also ordered to watch out for bleeding and to refer. August 23, 2011
Dr. Toledo ordered HHP monitoring OD continue present medications and same IVF to follow. August 24, 2011
Dr. Toledo ordered HHP for tomorrow. August 25, 2011
Dr. Toledo ordered MGH if with normal HHP. With take home meds Cefalexin 125mg/5ml syrup 1 tablespoon TID for 7 days and OMX cap 1 capsule BID for 3 days.
XI. EVALUATION
After the interdisciplinary management of medical approach and nursing interventions done to the client, the patient was still confined to the hospital for further evaluation of his condition. The doctor ordered to continually adhere to all the treatment regimen and laboratory and diagnostic procedure. The patient as well as his relative really adheres to what the situation is needed after some explanations. But on August 25, 2011 the doctor explained to the SOs that once the hematocrit, hemoglobin and platelet of the pt is already normal they will be allowed to go home. When the doctor saw that it was already within the normal level she allowed them to go home.
After conducting the study the student have understood and was able to identify what DFS is. After conducting the study the student was able to correlate every doctors orders to the condition of the patient and understood why they have been ordered. The student also understood how the prescribed drugs exert their actions, determined their possible harms or side effects for the patient as well as the appropriate nursing interventions for this. After the study the student was able to teach and give health teachings for the patient and significant others regarding the disease including its causes, manifestations and preventions. From the
newly acquired knowledge the student was able to provide the necessary and appropriate care for patient.
Você também pode gostar
- A Simple Guide to Pulmonary Infarction, Diagnosis, Treatment and Related ConditionsNo EverandA Simple Guide to Pulmonary Infarction, Diagnosis, Treatment and Related ConditionsAinda não há avaliações
- Case Study - Septic ShockDocumento16 páginasCase Study - Septic ShockIrene Mae Villanueva Ariola100% (2)
- Superior Vena Cava Syndrome, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsNo EverandSuperior Vena Cava Syndrome, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsAinda não há avaliações
- Termpaper DPTDocumento80 páginasTermpaper DPTAsha jiluAinda não há avaliações
- Heart Valve Diseases, A Simple Guide to These ConditionsNo EverandHeart Valve Diseases, A Simple Guide to These ConditionsAinda não há avaliações
- Biodata and AnaphyDocumento3 páginasBiodata and AnaphyhahahahaaaaaaaAinda não há avaliações
- A Writer's Guide to Medicine: Volume 2: Illness & InjuryNo EverandA Writer's Guide to Medicine: Volume 2: Illness & InjuryAinda não há avaliações
- Structure of Blood Vessels (Autosaved)Documento98 páginasStructure of Blood Vessels (Autosaved)Lednew MatiasAinda não há avaliações
- AnatomyDocumento3 páginasAnatomyKim CarpioAinda não há avaliações
- Health Disorders 1Documento3 páginasHealth Disorders 1sugandhdon77Ainda não há avaliações
- Case StudyDocumento15 páginasCase StudyLesten Mei Capulso100% (1)
- 1B. Cinta Mentari - Bhs InggrisDocumento8 páginas1B. Cinta Mentari - Bhs InggrisRiska NataliaAinda não há avaliações
- Pneumonia - Adults (Community Acquired) : Causes, Incidence, and Risk FactorsDocumento7 páginasPneumonia - Adults (Community Acquired) : Causes, Incidence, and Risk FactorsDEth JU NafenAinda não há avaliações
- Case Presentation MucormycosisDocumento10 páginasCase Presentation MucormycosiskunaidongAinda não há avaliações
- CHF Case Study (Documento35 páginasCHF Case Study (EzraManzanoAinda não há avaliações
- Prevention: Blood Pressure Body Weight Here BMIDocumento8 páginasPrevention: Blood Pressure Body Weight Here BMILuthfi Rama MaulanaAinda não há avaliações
- Pregnancy-Induced Hypertension CASE REPORTDocumento31 páginasPregnancy-Induced Hypertension CASE REPORTMylene Angelie Bognot100% (2)
- The Pathway: The Human Respiratory SystemDocumento25 páginasThe Pathway: The Human Respiratory SystemKenneth Decker PrietoAinda não há avaliações
- Respiratory System: VocabularyDocumento4 páginasRespiratory System: VocabularyFely NatadAinda não há avaliações
- Acute Respiratory Distress SyndromeDocumento30 páginasAcute Respiratory Distress SyndromeOya Zuraini KamalAinda não há avaliações
- TiKa TaKa PediatricsDocumento86 páginasTiKa TaKa PediatricsEmad MerganAinda não há avaliações
- Pointers To ReadDocumento10 páginasPointers To ReadTrixie Jane P ManaayAinda não há avaliações
- Anatomy of The Heart: Epicardium Myocardium EndocardiumDocumento8 páginasAnatomy of The Heart: Epicardium Myocardium EndocardiumTrishna ShahAinda não há avaliações
- Respi and CircuDocumento52 páginasRespi and Circuelianamarie OronganAinda não há avaliações
- ReviewerDocumento10 páginasReviewerMaybelyn Rivera PagkatotohanAinda não há avaliações
- Unit Human Respiratory & Circulatory System Class NotesDocumento4 páginasUnit Human Respiratory & Circulatory System Class NotesAiza SulemanAinda não há avaliações
- Dengue Case StudyDocumento16 páginasDengue Case StudyJayselle FelipeAinda não há avaliações
- Primary Koch's InfectionDocumento34 páginasPrimary Koch's InfectionLinkin Panet RNAinda não há avaliações
- TOFDocumento17 páginasTOFMaryel PascualAinda não há avaliações
- Checklists of Respiratory System AssessmentDocumento22 páginasChecklists of Respiratory System AssessmentDhrumini PatelAinda não há avaliações
- A Case Study About Cardiovascular DiseaseDocumento10 páginasA Case Study About Cardiovascular DiseaseBarben Balaquit100% (1)
- Anatomy Case StudyDocumento15 páginasAnatomy Case StudyHazreen HazwanyAinda não há avaliações
- Case Study On Lung CancerDocumento50 páginasCase Study On Lung CancerAna Marie Besa Battung-Zalun78% (9)
- Tetralogy of FallotDocumento5 páginasTetralogy of FallotCharity OaniaAinda não há avaliações
- Candon City, Ilocos Sur Grade 9 Reviewer School Year 2021 - 2022Documento7 páginasCandon City, Ilocos Sur Grade 9 Reviewer School Year 2021 - 2022Aleah TungbabanAinda não há avaliações
- Chronic Obstructive Pulmonary DiseaseDocumento15 páginasChronic Obstructive Pulmonary Diseasermarty_35Ainda não há avaliações
- Disorders of Arteries and VeinsDocumento143 páginasDisorders of Arteries and VeinsJisha JanardhanAinda não há avaliações
- Pregnancy Induced Hypertension (PIH) Is ADocumento14 páginasPregnancy Induced Hypertension (PIH) Is APaul John HipolitoAinda não há avaliações
- Parts of The Respiratory System and Their FunctionDocumento34 páginasParts of The Respiratory System and Their Functiontangent12100% (1)
- Case Study - PneumoniaDocumento15 páginasCase Study - PneumoniaArgenic BernzAinda não há avaliações
- Heart: Right Heart Left Heart. Fish in Contrast Have Two Chambers, An Atrium and A Ventricle, WhileDocumento5 páginasHeart: Right Heart Left Heart. Fish in Contrast Have Two Chambers, An Atrium and A Ventricle, WhileMiguel PatrickAinda não há avaliações
- Know Your BodyDocumento107 páginasKnow Your BodyEs EAinda não há avaliações
- The Epidemilogical Traid Model Final ProjectDocumento18 páginasThe Epidemilogical Traid Model Final ProjectCristal ThomasAinda não há avaliações
- Pregnancy Induced HypertensionDocumento7 páginasPregnancy Induced HypertensionRalph Emerson RatonAinda não há avaliações
- UK Anatomy The Lungs and Respiratory Tract LeafletDocumento6 páginasUK Anatomy The Lungs and Respiratory Tract LeafletsuryaAinda não há avaliações
- Reviewer - Q1 Module 1 and 2Documento7 páginasReviewer - Q1 Module 1 and 2HANNAH MACUDAinda não há avaliações
- Samara University: Collage of Biomedical and Health Science Department of Public Health OfficerDocumento32 páginasSamara University: Collage of Biomedical and Health Science Department of Public Health Officergirma melakuAinda não há avaliações
- Evidence 2 Human Body CareDocumento12 páginasEvidence 2 Human Body CareAzael GómezAinda não há avaliações
- Pregnancy Induced HypertensionDocumento9 páginasPregnancy Induced HypertensionRiazell Antonio DungcaAinda não há avaliações
- Nursing Case StudyDocumento21 páginasNursing Case StudyJeyser T. GamutiaAinda não há avaliações
- Now Get From Our Live Expert On Rea Ltime Basis Join Us and Get Homework HelpDocumento17 páginasNow Get From Our Live Expert On Rea Ltime Basis Join Us and Get Homework HelplicservernoidaAinda não há avaliações
- Iii. Review of Anatomy and Physiology The Circulatory SystemDocumento3 páginasIii. Review of Anatomy and Physiology The Circulatory SystemLeris Luigi VictorioAinda não há avaliações
- Case Study PneumoniaDocumento14 páginasCase Study PneumoniaDOni CorleoneAinda não há avaliações
- The LungsDocumento5 páginasThe LungsMacmac CAsAinda não há avaliações
- Ingles 4. CardiologyDocumento8 páginasIngles 4. CardiologyFrankchesca S.GAinda não há avaliações
- Science 9 ReviewerDocumento7 páginasScience 9 ReviewerArgie MabagAinda não há avaliações
- Geriatric Case StudyDocumento15 páginasGeriatric Case StudyJobelle AcenaAinda não há avaliações
- Paper English Cardiovascular System: Compiled By: Group IVDocumento9 páginasPaper English Cardiovascular System: Compiled By: Group IVSuryantoAinda não há avaliações
- HlhsDocumento6 páginasHlhsapi-340384585Ainda não há avaliações
- CHN Review Questions 148Documento22 páginasCHN Review Questions 148Alibasher MacalnasAinda não há avaliações
- Multiple Dengue Virus Types Harbored by Individual MosquitoesDocumento7 páginasMultiple Dengue Virus Types Harbored by Individual MosquitoesYL Slalu BahagieaAinda não há avaliações
- Community Health Nursing p.31-55Documento25 páginasCommunity Health Nursing p.31-55Adrian MallarAinda não há avaliações
- Performance Evaluation of A Dengue Iggigm and ns1 Rapid Test Device For Profesional in Vitro Diagnostic Use in Whole BloDocumento3 páginasPerformance Evaluation of A Dengue Iggigm and ns1 Rapid Test Device For Profesional in Vitro Diagnostic Use in Whole BloHas SimAinda não há avaliações
- Diseases and Mosquito Biology ProjectDocumento8 páginasDiseases and Mosquito Biology ProjectCurnel MilletteAinda não há avaliações
- FadfdDocumento5 páginasFadfdVanessa MeanaAinda não há avaliações
- CPD ProposalDocumento46 páginasCPD ProposalAngelo Malonzo100% (1)
- Task 1 Read the text below. Match choices (А-Н) to (1-5) - There are three choices you do not need to use. Write your answers on the separate answer sheetDocumento7 páginasTask 1 Read the text below. Match choices (А-Н) to (1-5) - There are three choices you do not need to use. Write your answers on the separate answer sheetNazar KuzivAinda não há avaliações
- Dengue Bukhar Ka Ilaj Lakshan Karan Bachne Ke Upay in HindiDocumento2 páginasDengue Bukhar Ka Ilaj Lakshan Karan Bachne Ke Upay in HindiSumit upayAinda não há avaliações
- Dengue Control and Prevention ProposalDocumento7 páginasDengue Control and Prevention ProposalMark Jay BongolanAinda não há avaliações
- CD RationalizationDocumento19 páginasCD RationalizationAnastasya Gishella RorongAinda não há avaliações
- Chronic Disease BurdenDocumento2 páginasChronic Disease BurdenjcfloreshAinda não há avaliações
- Med Ward JournalDocumento1 páginaMed Ward JournallordwinjohnbernardoAinda não há avaliações
- Mosquito Borne DiseasesDocumento24 páginasMosquito Borne DiseasesSidney BowenAinda não há avaliações
- IMCI Flip ChartDocumento30 páginasIMCI Flip ChartChrizelle Esperanzate Florentino50% (2)
- Anh Văn Y4Documento25 páginasAnh Văn Y4Nhất DuyAinda não há avaliações
- Periodic TestDocumento6 páginasPeriodic TestDhang Nario100% (1)
- BookletDocumento14 páginasBookletIndra KelanaAinda não há avaliações
- WM68Documento8 páginasWM68JasminAinda não há avaliações
- LP Ena-1-60 PDFDocumento60 páginasLP Ena-1-60 PDFEnaAinda não há avaliações
- Whale Shark Research and Conservation, Southern LeyteDocumento13 páginasWhale Shark Research and Conservation, Southern LeytePauline Cristine BarondaAinda não há avaliações
- Dengue (Break Bone Fever) - FAQ, DPH-TAMIL NADU, IndiaDocumento3 páginasDengue (Break Bone Fever) - FAQ, DPH-TAMIL NADU, IndiaDr.SagindarAinda não há avaliações
- Why Do We Fall Ill Class 9 Mcqs Questions With AnswersDocumento7 páginasWhy Do We Fall Ill Class 9 Mcqs Questions With AnswersSCIENCE WORK [AMP] ActivitiesAinda não há avaliações
- 160 GMAT PREP RC Passages - Official AnswersDocumento180 páginas160 GMAT PREP RC Passages - Official AnswersjanuanuAinda não há avaliações
- Communicable Disease QuizDocumento2 páginasCommunicable Disease QuizPlacida Mequiabas National High SchoolAinda não há avaliações
- Revised Dengue Guideline 2020 PDFDocumento98 páginasRevised Dengue Guideline 2020 PDFAbid Hasan ZiKonAinda não há avaliações
- Dengue FeverDocumento39 páginasDengue FeverMuhammad Alauddin Sarwar100% (15)
- Pnle CHN PDFDocumento11 páginasPnle CHN PDFapremsAinda não há avaliações
- Medicine II - Topical Past Papers (2007-2019)Documento48 páginasMedicine II - Topical Past Papers (2007-2019)Humna YounisAinda não há avaliações
- Importance of Research Public HealthDocumento12 páginasImportance of Research Public HealthConcepcion MpsAinda não há avaliações
- ADHD is Awesome: A Guide to (Mostly) Thriving with ADHDNo EverandADHD is Awesome: A Guide to (Mostly) Thriving with ADHDNota: 5 de 5 estrelas5/5 (3)
- The Age of Magical Overthinking: Notes on Modern IrrationalityNo EverandThe Age of Magical Overthinking: Notes on Modern IrrationalityNota: 4 de 5 estrelas4/5 (30)
- Think This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BeNo EverandThink This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BeNota: 2 de 5 estrelas2/5 (1)
- Love Life: How to Raise Your Standards, Find Your Person, and Live Happily (No Matter What)No EverandLove Life: How to Raise Your Standards, Find Your Person, and Live Happily (No Matter What)Nota: 3 de 5 estrelas3/5 (1)
- LIT: Life Ignition Tools: Use Nature's Playbook to Energize Your Brain, Spark Ideas, and Ignite ActionNo EverandLIT: Life Ignition Tools: Use Nature's Playbook to Energize Your Brain, Spark Ideas, and Ignite ActionNota: 4 de 5 estrelas4/5 (404)
- The Ritual Effect: From Habit to Ritual, Harness the Surprising Power of Everyday ActionsNo EverandThe Ritual Effect: From Habit to Ritual, Harness the Surprising Power of Everyday ActionsNota: 4 de 5 estrelas4/5 (4)
- Summary: Outlive: The Science and Art of Longevity by Peter Attia MD, With Bill Gifford: Key Takeaways, Summary & AnalysisNo EverandSummary: Outlive: The Science and Art of Longevity by Peter Attia MD, With Bill Gifford: Key Takeaways, Summary & AnalysisNota: 4.5 de 5 estrelas4.5/5 (42)
- Raising Mentally Strong Kids: How to Combine the Power of Neuroscience with Love and Logic to Grow Confident, Kind, Responsible, and Resilient Children and Young AdultsNo EverandRaising Mentally Strong Kids: How to Combine the Power of Neuroscience with Love and Logic to Grow Confident, Kind, Responsible, and Resilient Children and Young AdultsNota: 5 de 5 estrelas5/5 (1)
- By the Time You Read This: The Space between Cheslie's Smile and Mental Illness—Her Story in Her Own WordsNo EverandBy the Time You Read This: The Space between Cheslie's Smile and Mental Illness—Her Story in Her Own WordsAinda não há avaliações
- Summary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedNo EverandSummary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedNota: 5 de 5 estrelas5/5 (81)
- Raising Good Humans: A Mindful Guide to Breaking the Cycle of Reactive Parenting and Raising Kind, Confident KidsNo EverandRaising Good Humans: A Mindful Guide to Breaking the Cycle of Reactive Parenting and Raising Kind, Confident KidsNota: 4.5 de 5 estrelas4.5/5 (170)
- The Body Keeps the Score by Bessel Van der Kolk, M.D. - Book Summary: Brain, Mind, and Body in the Healing of TraumaNo EverandThe Body Keeps the Score by Bessel Van der Kolk, M.D. - Book Summary: Brain, Mind, and Body in the Healing of TraumaNota: 4.5 de 5 estrelas4.5/5 (266)
- Dark Psychology & Manipulation: Discover How To Analyze People and Master Human Behaviour Using Emotional Influence Techniques, Body Language Secrets, Covert NLP, Speed Reading, and Hypnosis.No EverandDark Psychology & Manipulation: Discover How To Analyze People and Master Human Behaviour Using Emotional Influence Techniques, Body Language Secrets, Covert NLP, Speed Reading, and Hypnosis.Nota: 4.5 de 5 estrelas4.5/5 (110)
- Why We Die: The New Science of Aging and the Quest for ImmortalityNo EverandWhy We Die: The New Science of Aging and the Quest for ImmortalityNota: 4 de 5 estrelas4/5 (5)
- Summary: Limitless: Upgrade Your Brain, Learn Anything Faster, and Unlock Your Exceptional Life By Jim Kwik: Key Takeaways, Summary and AnalysisNo EverandSummary: Limitless: Upgrade Your Brain, Learn Anything Faster, and Unlock Your Exceptional Life By Jim Kwik: Key Takeaways, Summary and AnalysisNota: 5 de 5 estrelas5/5 (8)
- Empath: The Survival Guide For Highly Sensitive People: Protect Yourself From Narcissists & Toxic Relationships. Discover How to Stop Absorbing Other People's PainNo EverandEmpath: The Survival Guide For Highly Sensitive People: Protect Yourself From Narcissists & Toxic Relationships. Discover How to Stop Absorbing Other People's PainNota: 4 de 5 estrelas4/5 (95)
- The Courage Habit: How to Accept Your Fears, Release the Past, and Live Your Courageous LifeNo EverandThe Courage Habit: How to Accept Your Fears, Release the Past, and Live Your Courageous LifeNota: 4.5 de 5 estrelas4.5/5 (253)
- Mindset by Carol S. Dweck - Book Summary: The New Psychology of SuccessNo EverandMindset by Carol S. Dweck - Book Summary: The New Psychology of SuccessNota: 4.5 de 5 estrelas4.5/5 (328)
- Summary: Thinking, Fast and Slow: by Daniel Kahneman: Key Takeaways, Summary & Analysis IncludedNo EverandSummary: Thinking, Fast and Slow: by Daniel Kahneman: Key Takeaways, Summary & Analysis IncludedNota: 4 de 5 estrelas4/5 (61)
- The Obesity Code: Unlocking the Secrets of Weight LossNo EverandThe Obesity Code: Unlocking the Secrets of Weight LossNota: 4 de 5 estrelas4/5 (6)
- The Marshmallow Test: Mastering Self-ControlNo EverandThe Marshmallow Test: Mastering Self-ControlNota: 4.5 de 5 estrelas4.5/5 (59)
- Manipulation: The Ultimate Guide To Influence People with Persuasion, Mind Control and NLP With Highly Effective Manipulation TechniquesNo EverandManipulation: The Ultimate Guide To Influence People with Persuasion, Mind Control and NLP With Highly Effective Manipulation TechniquesNota: 4.5 de 5 estrelas4.5/5 (1412)
- Cult, A Love Story: Ten Years Inside a Canadian Cult and the Subsequent Long Road of RecoveryNo EverandCult, A Love Story: Ten Years Inside a Canadian Cult and the Subsequent Long Road of RecoveryNota: 4 de 5 estrelas4/5 (45)