Escolar Documentos
Profissional Documentos
Cultura Documentos
Nurse As An Educator
Enviado por
Erl D. MelitanteDescrição original:
Título original
Direitos autorais
Formatos disponíveis
Compartilhar este documento
Compartilhar ou incorporar documento
Você considera este documento útil?
Este conteúdo é inapropriado?
Denunciar este documentoDireitos autorais:
Formatos disponíveis
Nurse As An Educator
Enviado por
Erl D. MelitanteDireitos autorais:
Formatos disponíveis
THE NURSE AS AN EDUCATOR
INTRODUCTION The teaching-learning process primarily involves the teacher, the learner and the subject matter. The success of this process rests mainly on the shoulders of the teacher. POHL (1988) Says that teaching is an integral part of the nursing process and the nurse is teaching whether directly or indirectly, in every contact with potential learners. ROLES AND FUNCTIONS OF THE EDUCATOR ALEGADO (1996) The teacher should possess the necessary attitude and competencies to effectively create a productive atmosphere related to the teaching-learning process. He also said that good teachers know how to help people become conscious of their own values that are more satisfying to society. Based on these perspectives, one can conclude that aside from the usual goal of learning, which is the acquisition of the necessary knowledge, attitudes and skills, the incorporation of values in the curriculum is also a must. In todays healthcare practice, the scenario has shifted from hospital care to communitybased care which places its emphasis on health promotion and disease prevention. The nurse educator is not only a teacher but is also an advocate of tender loving care and she is mandated to incorporate this doctrine into the practice of her profession. PATRICIA BENNER Provided a model, from Novice to Expert, where she contends that as a nurse gains experience, clinical knowledge becomes a blend of practical and theoretical knowledge. FIVE LEVELS OF COMPETENCY IN NURSING PRACTICE : 1. 2. 3. 4. 5. novice advanced beginner competent proficient expert
This conceptualization concentrates on excellence. According to her, experienced-based skill acquisition is safer and quicker when it rests upon a sound educational base.
BARCELO (2001) According to him, nursing leaders have to decide whether at the entry level of professional practice, the need is for a generalist or a specialist and to come upwith an acceptable list of minimum competencies that a fresh graduate of BSN must possess. PARADIGM SHIFT IN THE CONCEPT OF HEALTH (WHO) 1995 The World Health Organization issued a policy statement which included a paradigm shift in the concept of health from being disease-centered to human development a change from physician-dependent cure and sustained health through people-empowered healthy options. The shift to promotion of health and illness has been more the concern of the community health nurse rather than the hospital staff nurse, but not anymore. THE LEGAL BASIS OF HEALTH EDUCATION IN THE PHILIPPINES The Philippine constitution of 1987, Art.11, Sec.15 states that: The state shall protect and promote the right to health of the people and instill health consciousness among them This goal of protecting and promoting the peoples birthright to health and instilling the knowledge, attitudes and practices (KAP) which will enable them to adopt a healthy behaviors and lifestyles can principally be achieved through health education. Art. XIII, Sec. 11 states that: The state shall adopt an integrated and comprehensive approach to health development which shall endeavor to make essential goods, health and other social services available to all people at affordable cost. There shall be priority for the needs of the under previleged sick, elderly, disabled, women and children. THE LEGAL BASIS OF HEALTH EDUCATION IN THE NURSING CURRICULUM The teaching function has always been viewed as an essential function of a nurse whether she is taking care of a well or an ill person, patients family members, nursing students, hospital or clinical staff nurses or a group of mothers in the community. One of the more important functions of the nurse is as a health educator and this is explicitly stated in The Duties of a Nurse in Rule IV, Art VI, Sec. 28 of the Philippine Nursing Act of 2002 also known as RA 9173, among which are to: 1. Provide health education to individuals, families and communities ; and
2. Teach, guide and supervise students in nursing education programs including the administration of nursing services in varied settings like hospitals and clinics. Specifically, it states that The nursing education program shall provide sound general and professional foundation for the practice of nursing taking into consideration the learning outcomes based on national and universal nursing core competencies. The learning experience shall adhere strictly to specific requirements embodied in the prescribed curriculum as promulgated by the Commission on Higher Educations policies and standards of nursing education. ROLE is defined as a function, responsibility, job, duty, task, position, or behavior that includes accountability and responsibility for the position that one holds. As a teacher, the nurse performs multiple roles as ,manager, facilitator, a source of motivation and inspiration, an agent for social change, role model, and resources person. HEIDGERKEN (1965) defined the role functions of the nurse educator as the: 1. instructional role, 2. faculty role, 3. individual role. Instructional roles are the central functions of a nurse educator as the: 1. Planning and Organizing course : a. selecting objectives, substantive content and teaching and learning activities (for classroom, laboratory, the clinical and community settings) b. correlating them with other courses in the curriculum. 2. Creating and Maintaining a Desirable group climate which will encourage and enhance learning that will eventually lead to the development of the learners selfdiscipline. 3. Adopting Teaching Methods and preparing instructional materials according to the varying interests, needs and abilities of the students. 4. Motivating and Challenging students to pursue and sustain learning activities which will lead them toward acceptance of responsibility for their own learning. 5. Teaching which consists of a complex role involving a series of activities: a. supplying information needed or telling the students where it may be obtained.
b. explaining, classifying and interpreting c. demonstrating or explaining a procedure, a process or exhibiting materials. d. serving as a resource person for group projects to the individual students. e. supervising students performance in the classroom, laboratory and in any other setting where the student of nursing may be having learning experiences. f. evaluating all the planned learning and teaching activities and student outcomes related to the courses assigned to her to teach. Faculty role will depend on the size, control and complexity of the institution. The nurse educator can be: 1. chairwoman, secretary or member of one committee responsible for planning and coordinating the total educational offering for a particular program or other committee which engages in policy making or administration. 2. counselor or students in academic or non-academic matters 3. a researcher 4. resource person to groups outside of he institution 5. a representative to professional nursing organizations 6. a public relations agent where she will be able to interpret the objectives and the policies of her institution and helps in recruitment, among others. Individual role the teacher functions as a member of a family, church, community and as a citizen. As an individual, she brings her basic dignity and distinct personality everywhere she goes. PARADIGM SHIFT IN THE ROLE OF THE NURSE EDUCATOR The teacher used to be the omnipotent fountain of wisdom, the transmitter of information and knowledge, the all-knowing mentor and the student was likened to a sponge which soaks up whatever the teacher says or do. Today, a paradigm shift has occurred where the focus of the teaching-learning process has transferred from the teacher and the teaching endeavor to the learner and the learning process. Hence, the primary role of the nurse educator is not to teach or educate but to provide the opportunities for the learner to be actively involved in the learning process and to create an environment that will inspire or motivate the learner to apply the
knowledge and skills to assess, criticize, and select the best possible solutions to situations or problems. NURSING CORE COMPETENCIES The core competency standards will gauge the minimum knowledge, skills and attitudes that a graduate nurse possesses to be able to provide efficient and quality nursing care in her level as a beginning nurse practitioner. THE NURSING CORE COMPETENCY STANDARDS There are eleven nursing core competencies (araes of expertise fundamental or essential to a particular job or function) that are included in the Nurses Licensure Examination. These are: 1. Safe quality nursing care 2. management of resources and environment 3. Health education 4. Legal responsibility 5. Ethnic-moral responsibilities 6. Personal and professional development 7. Quality improvement 8. Research 9. Records management 10. Communication 11. Collaboration and teamwork CORE COMPETENCY 1 : Assesses the learning needs of the patient and family. INDICATORS: 1. Obtains learning information through interview, observation and validation 2. Defines relevant information 3. Completes assessment records appropriately 4. Identifies priority needs Authors Note: Needs assessment will serve as the starting point for the development of the program of health education and the formulation of specific action plans. It will determine the rationale, nature and scope of the program. How to conduct needs assessment. The health educator should: 1. Know how to locate and obtain valid sources of information pertaining to the target population which may be primary or secondary data
2. Know how to use the the family assessment guide or the community assessment guide, whichever the case may be, in identifying the health threats, health deficits, foreseeable crisis/ stress points and in priority setting or ranking 3. be able to analyze the data and prioritize the areas for health education planning 4. Utilize Maslows Hierarchy of Needs to determine the priorities for patient care
CORE COMPETENCY 2 : Develops health education plan based on assessed and anticipated needs. INDICATORS: 1. Considers the nature of the learner in relation to: social, cultural, political, economic, educational and religious factors. Authors notes: In developing the health education plan, the health educator must know and understand the nature of the target population or clientele: What is their level of understanding regarding the current problem/issue? Do they consider this a high level priority which needs immediate attention and intervention? Who or what elicit their active participation in the program? The health education plan should: 1. be based on the assessed health needs, problems and perceptions of the clientele which will be the basis of the goals and objectives of the teaching plan; 2. be evaluated according to the extent to which for goals and objectives have been met; 3. be a result of the active participation and cooperation of the interested stakeholders like the community leaders, sectoral or group representatives, opinion leaders and representatives of the target population 4. contain appropriate interventions to meet goals and objectives.
CORE COMPETENCY 3 : Develops learning materials for health education. INDICATORS: 1. Involves the patient, family, significant others and other resources 2. Formulates a comprehensive health education plan with the following components: objectives, content, time allotment, teaching-learning resources and evaluation parameters
3. Provides for feedback to finalize the plan Authors notes: In developing the learning materials for health education, the health educator: must be able to get the cooperation, pro-active involvement and commitment of the learners or target population to ensure the success of the program; must apply pertinent principles of teaching and learning: must be able to formulate a comprehensive teaching-lan (will be discussed after chapter 5) must have a wide array of teaching strategies like buzz sessions, brainstorming, role playing, socio-drama, forum lecture, use of audiovisual materials. CORE COMPETENCY 4 : Implements the health education plan. INDICATORS: 1. Provides for conductive learning situation in terms of time and place 2. Considers family and clients preparedness 3. Utilizes appropriate strategies 4. Provides reassuring presence through active listening, touch, facial expression and gestures 5. Monitors client and familys responses to health education Authors notes: The health educator must be able to: determine what strategies will be most effective in discussing the problem/issue identify, by consulting with the clients what would be the most convenient time, day and place to hold these discussions/brainstorming or lessons find out if they need financial assistance or childcare while attending the health education class monitor if there is a positive change or improvement in the clients knowledge, attitudes, skills and values as a result of the health teachings mainly through observation and interview. CORE COMPETENCY 5 : Evaluates the outcome of health education. INDICATORS: 1. Utilizes evaluation parameters 2. Documents outcome of care 3. Revises health education plan when possible
Authors notes: As in all undertakings, an evaluation process must be undertaken to determine the strengths and weaknesses of the program, the areas that need to be modified, revised or eliminated. formulate goals and objectives that are simple, measurable, attainable, realistic and time-bound (SMART) find out if the goals and objectives have been met by comparing these with results; develop an evaluation plan which involves - developing and administering evaluation tests - conducting surveys - observing behavior - other methods of data collection for evaluation analyze and interpret the data collected and property document the results of the evaluation use the results of the evaluation to modify, improve, revise or even change the existing or future programs. ROLES AND RESPONSIBILITIES OF HEALTH EDUCATORS The Responsibilities and competencies for Entry-level Health Educators are embodied in A Competency-Based Framework for Professional Development of Certified health Education Specialists, NCHEC, New York, 1996 (Cottrell, Girvan Mckenzie, 2001) Among the responsibilities of a health educator are: 1. assessing individual and community needs for health education 2. planning effective health education programs 3. implementing health education programs 4. evaluating effectiveness of health education programs 5. coordinating provisions of health services 6. acting as a resource person in health education 7. communicating health and health education needs, concerns and resources. IN THE CODE OF ETHICS ( Unabridged Version ) Society for public health education, Inc., Article IV deals with the Responsibility in Employing Educational Strategies and methods and states that, In designing strategies and methods, the health educator should be aware of his/her possible impact on the community and other health professionals and must not place the burden of change solely on the target population but must involve other appropriate groups to bring about effective changes. Obligation to two principles:
1. the people have a right to make decisions affecting their lives 2. there is moral imperative to provide people with all relevant information and resources possible to make their choices freely and intelligently (Cottrell, Girvan, & Mckenzie, 2001)
ETHICO-LEGAL BASIS OF HEALTH EDUCATION The right of the patient to accurate and adequate information regarding his or her health condition, medications or treatments and the possible risks or adverse reactions and alternative treatments available are all spelled out in the Patients Bill of Rights (American Health Association, 1975). Professional nurses are mandated to provide patient education by organizational policy including federal and state regulations and failure to comply may be penalized by a fine and/or a citation by the Department of Health in many states in the USA especially in healthcare facilities with Medicaid and Medicare funding. Ethico- Legal Considerations Among the ethico-legal aspects of care which involve the teaching skills of the nurse is the right of the patient to adequate information related to his/her medical condition, treatments and medications, and the pertinent risks and hazards involved as well as alternative modes of treatment. This is in relation also to the doctrine of informed consent which is specifically stated in the Patients Bill of Rights (AHA, 1975)
ECONOMIC CONSIDERATONS Todays realities point to the logic of shorter stay of the patient in the hospital and the emphasis on satellite types of ambulatory and home care services considering the enormity of the cost of human and material resources and at the same time, the growing scarcity of nursing manpower and personnel. IMPORTANCE OF DOCUMENTATION For a hospital to be able to qualify for Medicaid and Medicare reimbursement, it has to show proof that patient health education has been part of the care given to its patients and/or their family members which should be properly documented in the patient record (Boyd, et. al., 1998)
This protects the health personnel as well as the institution from the presumption that what you did not chart, you did not do or what was not written was not done. An interdisciplinary method of documenting patient educaton was proposed by Snyder in 1996 using a flow sheet containing: 1. an assessment of the education needs of the client and/or his family which includes: a. the clients readiness to learn b. barriers to learning due to language, poor hearing c. referrals to a patient advocate or another health personnel. 2. a space for documenting the: a. name of the recipient of health education b. what was taught like insulin injection c. when was it taught d. how the client responded to instruction CASEY (1995) stated that documentation of patient teaching is probably, the most undocumented skill service because nurses do not realize the scope and depth of the teaching they do. BASTABLE (2003) also said that lack of time may be a barrier for the nurse to provide sufficient information for self-care, and illness acuity level interferes with the patients ability to process information necessary to meet his/her physical and emotional needs. The importance of health teachings is very crucial in the post discharge planning and care of the patient whether in the home or in an ambulatory or community care setting. Clearly, the primary end-users of the governments health and social services are the depressed, oppressed, powerless and exploited members of the society and the primary tool for setting these programs on the right direction is through health education.
Você também pode gostar
- A Handbook for Student Nurses, 2015–16 edition: Introducing Key Issues Relevant to PracticeNo EverandA Handbook for Student Nurses, 2015–16 edition: Introducing Key Issues Relevant to PracticeNota: 5 de 5 estrelas5/5 (2)
- The Care Process: Assessment, planning, implementation and evaluation in healthcareNo EverandThe Care Process: Assessment, planning, implementation and evaluation in healthcareAinda não há avaliações
- Health Educ1Documento6 páginasHealth Educ1Märsh Pascual-DapunAinda não há avaliações
- COMMUNITY HEALTH NURSE: Passbooks Study GuideNo EverandCOMMUNITY HEALTH NURSE: Passbooks Study GuideAinda não há avaliações
- The Mindful Nurse: Using the Power of Mindfulness and Compassion to Help You Thrive in Your WorkNo EverandThe Mindful Nurse: Using the Power of Mindfulness and Compassion to Help You Thrive in Your WorkAinda não há avaliações
- Gerontological Nursing: Scope and Standards of Practice, 2nd EditionNo EverandGerontological Nursing: Scope and Standards of Practice, 2nd EditionAinda não há avaliações
- Nightingale's Vision: Advancing the Nursing Profession Beyond 2022No EverandNightingale's Vision: Advancing the Nursing Profession Beyond 2022Nota: 5 de 5 estrelas5/5 (1)
- Record Keeping for Nurses and Midwives: An essential guideNo EverandRecord Keeping for Nurses and Midwives: An essential guideAinda não há avaliações
- From Silence to Voice: What Nurses Know and Must Communicate to the PublicNo EverandFrom Silence to Voice: What Nurses Know and Must Communicate to the PublicAinda não há avaliações
- Mastering ICU Nursing: A Quick Reference Guide, Interview Q&A, and TerminologyNo EverandMastering ICU Nursing: A Quick Reference Guide, Interview Q&A, and TerminologyAinda não há avaliações
- Advanced Practice Nursing: Setting a New Paradigm for Care in the 21St CenturyNo EverandAdvanced Practice Nursing: Setting a New Paradigm for Care in the 21St CenturyAinda não há avaliações
- Fundamental Aspects of Legal, Ethical and Professional Issues in Nursing 2nd EditionNo EverandFundamental Aspects of Legal, Ethical and Professional Issues in Nursing 2nd EditionNota: 5 de 5 estrelas5/5 (4)
- Humanism, Nursing, Communication and Holistic Care: a Position Paper: Position PaperNo EverandHumanism, Nursing, Communication and Holistic Care: a Position Paper: Position PaperAinda não há avaliações
- Public Health Nursing: Scope and Standards of PracticeNo EverandPublic Health Nursing: Scope and Standards of PracticeNota: 5 de 5 estrelas5/5 (1)
- Nurse Commitment: How to Retain Professional Staff Nurses in a Multigenerational WorkplaceNo EverandNurse Commitment: How to Retain Professional Staff Nurses in a Multigenerational WorkplaceAinda não há avaliações
- Community Focused Nursing: Passbooks Study GuideNo EverandCommunity Focused Nursing: Passbooks Study GuideAinda não há avaliações
- Faith Community Nursing: Scope and Standards of PracticeNo EverandFaith Community Nursing: Scope and Standards of PracticeNota: 5 de 5 estrelas5/5 (1)
- Clinical Research Nursing: Scope and Standards of PracticeNo EverandClinical Research Nursing: Scope and Standards of PracticeNota: 5 de 5 estrelas5/5 (1)
- Nursing by Heart: Transformational Self-Care for NursesNo EverandNursing by Heart: Transformational Self-Care for NursesNota: 5 de 5 estrelas5/5 (1)
- Care For Vulnerable Populations during COVID-19 Pandemic: Clinical Updates in COVID-19No EverandCare For Vulnerable Populations during COVID-19 Pandemic: Clinical Updates in COVID-19Ainda não há avaliações
- How to Prepare for Interviews and Develop your Career: As a nurse or midwifeNo EverandHow to Prepare for Interviews and Develop your Career: As a nurse or midwifeAinda não há avaliações
- Nightingale's Legacy: The Evolution of American Nurse LeadersNo EverandNightingale's Legacy: The Evolution of American Nurse LeadersAinda não há avaliações
- The Art and Science of Nurse Coaching: The Provider's Guide to Coaching Scope and CompetenciesNo EverandThe Art and Science of Nurse Coaching: The Provider's Guide to Coaching Scope and CompetenciesNota: 5 de 5 estrelas5/5 (2)
- Code of Ethics for Nurses with Interpretive StatementsNo EverandCode of Ethics for Nurses with Interpretive StatementsNota: 5 de 5 estrelas5/5 (2)
- A Nurse’s Medicine Basket: Tools for Compassionate Self-CareNo EverandA Nurse’s Medicine Basket: Tools for Compassionate Self-CareAinda não há avaliações
- Home Health Nursing: Scope and Standards of PracticeNo EverandHome Health Nursing: Scope and Standards of PracticeNota: 5 de 5 estrelas5/5 (1)
- A Guide for the Nurse Entrepreneur: Make a DifferenceNo EverandA Guide for the Nurse Entrepreneur: Make a DifferenceAinda não há avaliações
- Lead Like A Nurse: Leadership in Every Healthcare SettingNo EverandLead Like A Nurse: Leadership in Every Healthcare SettingNota: 4.5 de 5 estrelas4.5/5 (2)
- Applications of Public Health Education and Health Promotion InterventionsNo EverandApplications of Public Health Education and Health Promotion InterventionsAinda não há avaliações
- Nursing: Scope and Standards of PracticeNo EverandNursing: Scope and Standards of PracticeNota: 5 de 5 estrelas5/5 (2)
- School Nursing: Scope and Standards of Practice, 3rd EditionNo EverandSchool Nursing: Scope and Standards of Practice, 3rd EditionNota: 5 de 5 estrelas5/5 (1)
- Holistic Nursing: Scope and Standards of Practice, 3rd EditionNo EverandHolistic Nursing: Scope and Standards of Practice, 3rd EditionNota: 5 de 5 estrelas5/5 (2)
- Surviving the ICU: A Toolkit for the Critical Care NurseNo EverandSurviving the ICU: A Toolkit for the Critical Care NurseAinda não há avaliações
- The Balance Concept in Health and Nursing: A Universal Approach to Care and SurvivalNo EverandThe Balance Concept in Health and Nursing: A Universal Approach to Care and SurvivalAinda não há avaliações
- Personal Philosophy of Nursing Education PortfolioDocumento8 páginasPersonal Philosophy of Nursing Education Portfolioapi-360345296100% (2)
- Free Nursing Dissertation TopicsDocumento5 páginasFree Nursing Dissertation TopicsJamal P. AlawiyaAinda não há avaliações
- Guide to the Code of Ethics for Nurses: Interpretation and ApplicationNo EverandGuide to the Code of Ethics for Nurses: Interpretation and ApplicationAinda não há avaliações
- Heart Nursing: Learn, Grow & Succeed in the First Year of PracticeNo EverandHeart Nursing: Learn, Grow & Succeed in the First Year of PracticeNota: 4 de 5 estrelas4/5 (1)
- Boost Your Nursing Leadership Career: 50 Lessons that Drive SuccessNo EverandBoost Your Nursing Leadership Career: 50 Lessons that Drive SuccessAinda não há avaliações
- The Battle Against Covid-19 Filipino American Healthcare Workers on the Frontlines of the Pandemic ResponseNo EverandThe Battle Against Covid-19 Filipino American Healthcare Workers on the Frontlines of the Pandemic ResponseAinda não há avaliações
- Practicum Proposal For The Nurse Educator Role Kim GarzaDocumento33 páginasPracticum Proposal For The Nurse Educator Role Kim Garzaapi-47107860100% (3)
- Curriculum and Teaching Q N ADocumento10 páginasCurriculum and Teaching Q N ARonni Mae DeazetaAinda não há avaliações
- Clinical Practicum II ProposalDocumento30 páginasClinical Practicum II Proposalapi-281813422Ainda não há avaliações
- Analysis and Evaluation of TheoryDocumento11 páginasAnalysis and Evaluation of TheoryAris Kendell Bungabong100% (1)
- Nursing EducDocumento31 páginasNursing EducAnne Giselle PatocAinda não há avaliações
- Peplau TheoryDocumento9 páginasPeplau TheoryManish Tripathi100% (1)
- Outcome Based Education of NursingDocumento33 páginasOutcome Based Education of NursingAndrea Bone100% (1)
- Select Brochure Full - 2022 10 (October 01)Documento12 páginasSelect Brochure Full - 2022 10 (October 01)Erl D. MelitanteAinda não há avaliações
- ChemotherapyDocumento46 páginasChemotherapyErl D. Melitante100% (1)
- Introduction To BiostatisticsDocumento272 páginasIntroduction To BiostatisticsErl D. MelitanteAinda não há avaliações
- ChemotherapyDocumento7 páginasChemotherapySharifa Shierha HassanAinda não há avaliações
- Radiation TherapyDocumento22 páginasRadiation TherapyErl D. Melitante100% (1)
- BLOOD TRANSFUSION NotesDocumento7 páginasBLOOD TRANSFUSION NotesErl D. MelitanteAinda não há avaliações
- AnaphyDocumento47 páginasAnaphyErl D. MelitanteAinda não há avaliações
- MANILA, Philippines - It's A Breezy Afternoon in A Cold January, But It's Humid As Usual in This BlockDocumento6 páginasMANILA, Philippines - It's A Breezy Afternoon in A Cold January, But It's Humid As Usual in This BlockErl D. MelitanteAinda não há avaliações
- History of BiologyDocumento30 páginasHistory of BiologyErl D. MelitanteAinda não há avaliações
- Prelim OncologyDocumento10 páginasPrelim OncologyErl D. MelitanteAinda não há avaliações
- Applying Theories of Learning To Healthcare PracticeDocumento60 páginasApplying Theories of Learning To Healthcare PracticeErl D. MelitanteAinda não há avaliações
- Journal of Personality and Social Psychology VolumeDocumento11 páginasJournal of Personality and Social Psychology VolumeUswatun HasanahAinda não há avaliações
- Jon Pumper Uttoradhikar PDFDocumento56 páginasJon Pumper Uttoradhikar PDFArbanAinda não há avaliações
- Research PR1 C1 REVISEDDocumento8 páginasResearch PR1 C1 REVISEDellaAinda não há avaliações
- Characteristic of Human LanguageDocumento1 páginaCharacteristic of Human LanguageSatya Permadi50% (2)
- How To Solve A Case StudyDocumento2 páginasHow To Solve A Case StudySaYam ReHania100% (1)
- Examination: Session: Course Title: Semester: Course Code: Max Marks: Date: 3/10/2020 Time: 12pm To 11:59amDocumento2 páginasExamination: Session: Course Title: Semester: Course Code: Max Marks: Date: 3/10/2020 Time: 12pm To 11:59amsaqib aliAinda não há avaliações
- Emergence of OBDocumento4 páginasEmergence of OBBhavya VermaAinda não há avaliações
- Epidemiology Kept Simple An Introduction To Traditional and Modern Epidemiology 3rd Edition Chapter 1 Epidemiology Past and PresentDocumento35 páginasEpidemiology Kept Simple An Introduction To Traditional and Modern Epidemiology 3rd Edition Chapter 1 Epidemiology Past and PresentDeni HerdianaAinda não há avaliações
- Review Unit 456Documento6 páginasReview Unit 456Thanh ThủyAinda não há avaliações
- World War Two Unit PlanDocumento22 páginasWorld War Two Unit Planapi-280689729100% (1)
- Krista Pankau Cover LetterDocumento3 páginasKrista Pankau Cover Letterapi-514564329Ainda não há avaliações
- High School Report CardDocumento2 páginasHigh School Report Cardapi-517873514Ainda não há avaliações
- Planificare Lectii Limba Engleza GrădinițăDocumento4 páginasPlanificare Lectii Limba Engleza Grădinițăbaba ioanaAinda não há avaliações
- Laser TB CoverDocumento2 páginasLaser TB CoverNarine Hovhannisyan0% (1)
- Information Brochure & Guidelines For Filling of Online Application Form For Recruitment of Non-Teaching Positions in Delhi UniversityDocumento106 páginasInformation Brochure & Guidelines For Filling of Online Application Form For Recruitment of Non-Teaching Positions in Delhi UniversityVidhiLegal BlogAinda não há avaliações
- Communication Technology Definition PDFDocumento2 páginasCommunication Technology Definition PDFVictoriaAinda não há avaliações
- Article - Children Need To Play With Summary AssignmentDocumento6 páginasArticle - Children Need To Play With Summary Assignmentjuanjones5Ainda não há avaliações
- Technology and Literature Teaching: Using Fanfiction To Teach Literary CanonDocumento5 páginasTechnology and Literature Teaching: Using Fanfiction To Teach Literary Canonnita_novianti_2Ainda não há avaliações
- PERFORMANCE TASK NO 1. Workout Plan in SwimmingDocumento3 páginasPERFORMANCE TASK NO 1. Workout Plan in SwimmingErika BernardinoAinda não há avaliações
- Innovative Technologies For Assessment Tasks in Teaching andDocumento31 páginasInnovative Technologies For Assessment Tasks in Teaching andRexson Dela Cruz Taguba100% (3)
- GRADE 8 LP 2nd RevisionDocumento3 páginasGRADE 8 LP 2nd RevisionFrezlyn ManangbaoAinda não há avaliações
- Game Based Learning FoundationDocumento26 páginasGame Based Learning FoundationNessa BleuAinda não há avaliações
- Chess With MatthewDocumento9 páginasChess With MatthewsalihAinda não há avaliações
- Discuss About TM Malaysia Balance Scrore CardDocumento24 páginasDiscuss About TM Malaysia Balance Scrore CardSuzana Ithnain100% (2)
- Wim Coca L1Documento8 páginasWim Coca L1Abdul Shahfi DahalanAinda não há avaliações
- q2 Lesson 9 Concept PaperDocumento4 páginasq2 Lesson 9 Concept PaperShiela May DelacruzAinda não há avaliações
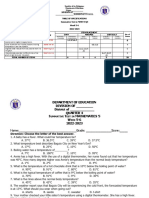
- ST3 - Math 5 - Q4Documento3 páginasST3 - Math 5 - Q4Maria Angeline Delos SantosAinda não há avaliações
- Chem Books AllDocumento4 páginasChem Books Allpmb2410090Ainda não há avaliações
- SCIENCE G8-Q2-Module 4Documento18 páginasSCIENCE G8-Q2-Module 4honey g100% (1)
- Lesson in JPL PDFDocumento12 páginasLesson in JPL PDFIsabela AndradaAinda não há avaliações