Escolar Documentos
Profissional Documentos
Cultura Documentos
Motivating Change With Mobile, Seven Guidelines - 2012
Enviado por
stephhabifDescrição original:
Título original
Direitos autorais
Formatos disponíveis
Compartilhar este documento
Compartilhar ou incorporar documento
Você considera este documento útil?
Este conteúdo é inapropriado?
Denunciar este documentoDireitos autorais:
Formatos disponíveis
Motivating Change With Mobile, Seven Guidelines - 2012
Enviado por
stephhabifDireitos autorais:
Formatos disponíveis
FORUM
HE ALTH MAT TERS
This forum is dedicated to personal health in all its many facets: decision-making, goal setting, celebration, discovery, reflection, coordination even entertainment. Well look at innovations in interactive technologies and how they help address current critical healthcare challenges. Elizabeth D. Mynatt, Editor
Motivating Change with Mobile: Seven Guidelines
Margaret E. Morris
Intel | margaret.morris@intel.com
People are becoming more resourceful in the ways they use their mobile devices to take care of themselves. This can be explained by the convergence of three major forces: the rise in chronic disease, decreased access to clinical care, and staggering innovation in mobile technology. Phones and other mobile devices, along with their applications, hold great promise for promoting health and associated lifestyle changes. Always at ones side, these devices are trusted allies that know more about individuals lifestyles than most clinicians. They are also portals into the growing participatory medicine and Quantified Self movements, in which people track, analyze, and share data typically managed by clinicians or businesses. To have a significant impact, health messaging on these devices must engage people emotionally and motivate sustained lifestyle change. Many of the behavioral shifts that improve health outcomessuch as consuming less, exercising more, or weighing oneself dailyare relatively simple. The challenge lies in persuading people to initiate and sustain changes that fly in the face of habit, culture, convenience, and immediate gratification. Behavior change is the science of motivating these difficult lifestyle shifts and helping people align
everyday choices with long-term values. Here I draw upon relevant research in health psychology, psychotherapy, behavioral economics, and influence. The seven guidelines below are based on a range of techniques that have been evaluated for either health intervention [1] or persuasive communication [2]. Remind people of who they want to be. To drive lifestyle change, health messaging should remind people of previously expressed self-ideals. This follows from research on cognitive dissonance, the discomfort with conflicts between ones behavior and values [3]. People may reformulate their values to accommodate for recent behaviors. And, when asked about intentions, people tend to give socially desirable responses and follow through on actions consistent with those intentions [4]. This tendency to follow through on previously articulated intentions can be applied in a variety of ways, such as health contracts, to influence exercise and diet. Contracts should link healthful behaviors with an individuals values. A contract, such as I agree to avoid salt because it will help me manage my heart condition and spend more time with my grandchildren can be renewed daily and shared to enhance accountability. A variety of applications (e.g., Withings) permit immediate shar-
ing of weight and other data across social network platforms. Health messaging should reference relationships and other powerful incentives for making difficult lifestyle changes to remind people of their values and previously set intentions. Iconic images such as interlocking hands can be used to signify family and community, and images of nature can similarly allude to outdoor activities or travel. Alternatively, customized content can be created with a patients own photos or by mining photos of friends or peers through tools such as Flickr. Juxtaposed images can drive an association between tough daily behaviors and life valuesan important component of Acceptance Commitment Therapy. Figure 1, a research prototype developed for Intel-GE Care Innovations, shows this concept. The images are pushed to the phone at the time individuals take medication to convey that adherence will enable them to pursue favorite activities, such as gardening. Another way to appeal to selfideals is through positive characterization. When people are ascribed character strengths, they are more likely to behave consistently with those strengths. For example, those told You are characterized as an above-average citizen likely to vote
26
interactions
M a y + J u n e 2 0 12
HE ALTH MAT TERS
FORUM
and participate in political events were significantly more likely to vote than people who did not receive this message [5]. By extension, technologies can draw personal data to formulate characterizations such as People like you, who are highly motivated and curious, enjoy learning new forms of exercise and developing new areas of expertise, while keeping fit. Foster an alliance. The very close relationships that people have with their devices set the stage for meaningful health coaching. A close bond between a therapist and patient is a key factor in successful psychotherapy [6]. This trusting alliance, fostered through empathy, co-investigation, and joint problem solving in therapy, can also be developed with a technology that interacts collaboratively. For example, dialogue such as Lets figure out what might be causing the rise in your blood pressure is preferable to Your blood pressure is high; answer the questions below. Similarly, statements about the importance of catching symptoms early will reinforce honest reporting of symptoms and behaviors. As in therapy, visual metaphors can ease dialogue: Weight gain due to water retention in a patient with heart failure, for example, can be communicated with stigma-free images such as rising tides. Health applications should also integrate with calendars and other tools to help people work around perceived logistical barriers. Just as the therapeutic alliance evolves over the duration of treatment, health technologies must develop greater understanding of users over time and adapt to their changing needs. Insight and confidence in ones ability to change results from a strong therapeutic alliance. A therapists interpretations that
Figure 1. Link health behaviors to life values.
describe the patients main conflict in the contexts of her current situation, her personal history, and the dynamics within the therapeutic relationship are catalysts for insight. Interpretations are a challenge for technology: How can
a device go beyond merely listening and then responding with precisely the information people request? This is currently the most we expect of Siri and similar listening applications. Whether we request an instant purchase or
27
interactions
M a y + J u n e 2 0 12
FORUM
HE ALTH MAT TERS
Figure 2. Data mining for social norms.
directions to the nearest cupcake shop, or need to tell our friend we are running late, our technology should know that what we ask for is not always in our best interests. And when it comes to important personal transitions, it is often difficult to know the desired destination or even how to frame a question: We may simply have an idea we want more novelty, more fun, or stronger relationships. Our apps and devices need to listen for our goals over time, challenge us when our immediate requests run counter to them, and steer us in the right direction. Apply social influence. Our technologies know a tremendous amount about us and others. This knowledge, which now guides Google searches, Amazon purchases, and a wide array of other consumer profiling, can also drive healthful change. For example, personal data can be used to reference peer groups who engage in healthful habits. The most relevant and specific peer group should be identified for such referencing. Social comparison has been used to influence behavior in
many contexts, from clinical interventions for substance abuse to social psychology experiments on environmentalism. To curtail substance abuse, it has been effective to inform heavy drinkers about the lower consumption of their peers, using feedback such as You drink a six-pack every Friday and Saturday; most men your age have only two drinks a week [7]. Similarly, hotel guests are far more likely to reuse their towels for the length of their stay when they are told that the majority of other guests who stayed in the same room had done so [8]. By extension, health technologies can deliver statements such as You exercised once last week. Eighty percent of women your age exercise daily. To motivate change, the statements must accurately reference desirable behavior, rather than unfortunate behavioral trends and their deleterious effects. Advertising campaigns about litter and the destruction of nature, although emotionally moving, have generally not been helpful [9]. Health appeals should avoid
statistics about rampant overeating or sedentary lifestyles. Instead, normative appeals should highlight and invite people to join positive trends. Data mining, social networking applications, and mobile technologies can be used for powerful, timely nudges (shown in Figure 2 in a concept developed for Intel). Detailed narratives or videos depicting the successful strategies of others can provide role modeling and thereby foster self-efficacy. It can also be helpful to learn from others struggles, as long as such accounts do not normalize behaviors and thereby encourage lapses. These scenarios can be sourced from a video library designed expressly for peer role modeling (e.g., realtimehealth.com or icyou.com) or from mining YouTube and other social media based on the patients health concerns and demographics. Show people what they could lose. People need help understanding the health losses they could experience as a result of poor self-care. Behavioral economics describes errors in human decision making, such as the tendency to undervalue long-term financial and health investments in favor of immediate gratification [10]. Value perceptions of long- and short-term goals cross at the moment of pivotal decisions; for example, the high priority given to weight loss when setting New Years resolutions frequently gives way to dessert the very next time one confronts a restaurant menu. This discounting of long-term goals is particularly strong for health and economic choices. Numerous strategies can be employed to counteract this tendency. One is to anticipate potential losses, building on the finding that we are often more motivated by concrete losses of what we already posses than by abstract promises of future rewards [11].
28
interactions
M a y + J u n e 2 0 12
HE ALTH MAT TERS
FORUM
Figure 3. Visualizing loss.
For example, the losses that follow dietary lapses can be made tangible with precise language and evocative images. Such a message is shown in Figure 3 on the Intel-GE Care Innovations Guide, which tracks vital signs and self-reported behaviors and alerts patients and clinicians to potential problems. A challenge is to present potential losses as palpable, immediate consequences instead of abstract, distant risks. Loss aversion can also be used playfully. Several applications that invite people to share their health goals with friends use loss as a game mechanic. In Stickk.com, friends bet on their ability to follow through on a goal. Financial losssometimes donations to a
cause or political party selected by a friendfollows failures. A Facebook application called With a Little Help from My Friends (a collaboration between the author and Cognitive Media shown in Figure 4) operates on the same principle but uses social capital as the motivational structure . Failure to follow through on a goal is reflected in the fading of friends faces and blocking of posts. The social dynamics of these apps can be used for support, role modeling, or as an incentive structure. Put the message where the action is. Posters about public-health problems such as drunk driving and obesity elicit strong emotional reactions at the moment they are read, but they may not influence behav-
iors that occur in other settings. The closer to the time and place of the target activity that a reminder occurs, the more effective it will be. Time- and place-based prompting has shown promise for medication adherence in tests of products such as Vitality Glow Caps. A wide range of other health choices, from immediate meal decisions to enrollment in exercise classes, can be guided and simplified through contextual prompting. Such choice architecture can increase the odds that people will stick to their health goals. Too many choices, such as the wide array of 401K options offered to many employees, can overwhelm and paralyze people from making the logical choices that are in
29
interactions
M a y + J u n e 2 0 12
FORUM
HE ALTH MAT TERS
Figure 4. Loss of social capital depicted in With a Little Help from My Friends.
Figure 5. Cognitive reappraisal cue [16].
their best interest [12]. Instead of encyclopedic nutritional indices, health messaging should use simple heuristics, such as the popular reference to the palm of ones hand as a guide for portion size. Suggestions such as Consider these alternatives to salt or Chop extra vegetables for tomorrows snacks accompanied by appealing, realistic images can guide people at the moment of meal preparation. A variety of smartphone applications and builtin notification systems such as Siri allow people to set health reminders for themselves throughout the day, enabling compelling options for contextual prompting. As the phone becomes a payment device, it should be possible for people to set up alerts to reconsider impulse purchases or even to freeze the phone if it tries to buy a product that isnt aligned with health goals [13]. Raise emotional awareness. Emotional dynamics play a strong role in motivation, with negative moods associated with impaired negotiating skills [14] and consequent lapses from health goals. By checking in with their current mood and emotional patterns, individuals can understand their vulnerabilities to such lapses and develop alternative coping strategies. Mindfulness can also foster emotional resilience, which itself has value for mental and physical health. Emerging mobile applications and on-the-body sensors allow individuals to reflect on emotional, physiological, and behavioral patterns. Increasingly, sensor data will be transmitted directly to the cloud, removing the need for uploading data via other devices. Cloud computing facilitates analysis of individual and group data, and allows prompt feedback to individuals about their own trends and how they compare to others.
30
interactions
M a y + J u n e 2 0 12
HE ALTH MAT TERS
FORUM
Reframe challenges. Examining ones immediate interpretations of daily events and considering alternatives helps people respond to challenging situations in more constructive ways. Whether fuming over a perceived slight from a colleague or berating oneself for having blown a diet, reframing the event in situational terms helps curtail negative emotions and facilitates more adaptive behaviors. An example of this reframing is attributing a dietary lapse, such as eating fast food, not to a lack of willpower but to unpreparedness for a long car ride. The latter interpretation generates practical solutions, such as packing snacks, rather than self-recrimination. Self-monitoring, cognitive reappraisal, and development of alternative coping strategies are wellevidenced elements of cognitive behavioral therapy (CBT) [15]. CBT is now being applied to physical as well as mental health, particularly weight loss and smoking cessation. A core principle is attributing disappointing outcomes to situational factors rather than enduring personal characteristics, and opening up the sense of personal changeability. Many good online CBT programs have been evaluated, including CRUFAD and the consumer-oriented MoodGym, but to date most have been designed for desktop interaction. Mobile technologies are particularly well suited for CBT, since they can push contextually sensitive notifications for self-monitoring and the practice of new response styles. A mobile therapy application that coupled experience sampling of mood with cues for cognitive reappraisal, constructive communication, and relaxation showed promise for stress management (see Figure 5) [16]. This approach logically
extends to many other aspects of wellbeing and behavior change. Conclusion In many respects we are left to our own devices when it comes to health and many other areas of our lives. Constraints in clinical care converge with staggering technical innovation, leading to a new resourcefulness in the use of devices, applications, and data for self care. Always with us and intertwined with almost all aspects of life, mobile technology is well suited to guide daily health choices. To change behavior, mobile health applications need to go beyond selftracking, providing tips or access to an online community. Such applications need to address disconnects between long-term intentions and moment-to-moment choices. The most effective tools will creatively instantiate well-evidenced behaviorchange principles with data mining, social networking, location awareness, and other capabilities of mobile technologies. Consumers will adopt these products in unexpected ways, generating new ways of thinking about health intervention. Here we focused on health, but the seven guidelines for motivating change have far broader applicability. The guidelines can be used in concert with emergent capabilities of the phonefor payment, contextual awareness, and detection of other people, for exampleto help people align daily choices with a wide range of financial, productivity, and interpersonal goals.
ENDNOTES:
1. Webb, T.L., Joseph, J., Yardley, L., and Michie, S. Using the Internet to promote health behavior change: A systematic review and meta-analysis of the impact of theoretical basis, use of behavior change techniques, and mode of delivery on efficacy. J. Med. Internet Res. 12, 1 (2010): e4. 2. Cialdini, R.B. Influence: Science and Practice (4th ed.). Allyn & Bacon, Boston, 2001.
3. Aronson, E. The theory of cognitive dissonance: A current perspective. In Advances in Experimental Social Psychology (vol. 4). L. Berkowitz, ed. Academic Press, New York, 1969. 4. Greenwald, A.G., Carnot, C.G., Beach, R., and Young, B. Increasing voting behavior by asking people if they expect to vote. Journal of Applied Psychology 72, 2 (1987), 315-318. 5. Tybout, A.M. and Yalch, R.F. The effect of experience: A matter of salience? Journal of Consumer Research 6, 4 (1980), 406-413. 6. Horvath, A.O. and Luborsky, L. The role of the therapeutic alliance in psychotherapy. Journal of Consulting and Clinical Psychology 61, 4 (1993), 561-573. 7. Miller, W.R. and Rollnick, S. Motivational Interviewing: Preparing People to Change. Guilford Press, New York, 2002. 8. Goldstein, N.J., Cialdini, R.B., and Griskevicius, V. A room with a viewpoint: Using normative appeals to motivate environmental conservation in a hotel setting. Journal of Consumer Research 35, 3 (2008), 472-482. 9. Cialdini, R.B., Demaine, L.J., Sagarin, B.J., Barrett, D.W., Rhoads, K., and Winter, P.L. Managing social norms for persuasive impact. Social Influence 1, 1 (2006), 3-15. 10. Ainslie, G. Breakdown of Will. Cambridge University Press, New York, 2001. 11. Kahneman, D. and Tversky, A. Prospect theory: An analysis of decisions under risk. Econometrica 47, 2 (1979), 263-292. 12. Iyengar, S.S., Huberman, G., and Jiang, W. How much choice is too much: Determinants of individual contributions in 401K retirement plans. In Pension Design and Structure: New Lessons from Behavioral Finance. O.S. Mitchell and S. Utkus, eds. Oxford University Press, Oxford, 2004, 83-95. 13. Dolan, B. How mobile payments might drive health behavior change. MobiHealthNews (Mar. 6, 2012); http://mobihealthnews.com/16553/how-mobilepayments-might-drive-health-behavior-change/ 14. Lerner, J.S., Small, D.A., and Loewenstein, G. Heart strings and purse strings: Carry-over effects of emotions on economic decisions. Psychological Science 15, 5 (2004), 337-341. 15. DeRubeis, R.J., Siegle G.J., and Hollon, S.D. Cognitive therapy versus medication for depression: Treatment outcomes and neural mechanisms. Nature Reviews Neuroscience 9 (2008), 788-796. 16. Morris, M.E., Kathawala, Q., Leen, T.K., Gorenstein, E.E., Guilak, F., Labhard, M., and Deleeuw, W. Mobile therapy: Case study evaluations of a cell phone application for emotional selfawareness. J. Med. Internet Res. 12, 2 (2010): e10; http://www.jmir.org/2010/2/e10/
ABOUT THE AUTHOR
Margaret (Margie) Morris is a clinical psychologist and senior researcher at Intel. She examines how people relate to technology, and creates mobile and social applications to support selfawareness and change. Morris completed her B.A. at Haverford College, her Ph.D. at the University of New Mexico, and post-doctoral fellowship at Stanford University. Prior to joining Intel, she studied technology adoption at Sapient. DOI: 10.1145/2168931.2168939 2012 ACM 1072-5220/12/05 $10.00
interactions
M a y + J u n e 2 0 12
31
Você também pode gostar
- The Yellow House: A Memoir (2019 National Book Award Winner)No EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Nota: 4 de 5 estrelas4/5 (98)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeNo EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeNota: 4 de 5 estrelas4/5 (5794)
- The Little Book of Hygge: Danish Secrets to Happy LivingNo EverandThe Little Book of Hygge: Danish Secrets to Happy LivingNota: 3.5 de 5 estrelas3.5/5 (400)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureNo EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureNota: 4.5 de 5 estrelas4.5/5 (474)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryNo EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryNota: 3.5 de 5 estrelas3.5/5 (231)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceNo EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceNota: 4 de 5 estrelas4/5 (895)
- Team of Rivals: The Political Genius of Abraham LincolnNo EverandTeam of Rivals: The Political Genius of Abraham LincolnNota: 4.5 de 5 estrelas4.5/5 (234)
- Never Split the Difference: Negotiating As If Your Life Depended On ItNo EverandNever Split the Difference: Negotiating As If Your Life Depended On ItNota: 4.5 de 5 estrelas4.5/5 (838)
- The Emperor of All Maladies: A Biography of CancerNo EverandThe Emperor of All Maladies: A Biography of CancerNota: 4.5 de 5 estrelas4.5/5 (271)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaNo EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaNota: 4.5 de 5 estrelas4.5/5 (266)
- The Unwinding: An Inner History of the New AmericaNo EverandThe Unwinding: An Inner History of the New AmericaNota: 4 de 5 estrelas4/5 (45)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersNo EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersNota: 4.5 de 5 estrelas4.5/5 (345)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyNo EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyNota: 3.5 de 5 estrelas3.5/5 (2259)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreNo EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreNota: 4 de 5 estrelas4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)No EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Nota: 4.5 de 5 estrelas4.5/5 (121)
- Goal Setting LessonDocumento14 páginasGoal Setting Lessonapi-262527285Ainda não há avaliações
- Human Resource Management - 13t - Gary DesslerDocumento39 páginasHuman Resource Management - 13t - Gary Desslerhayelom0% (2)
- GradesDocumento8 páginasGradesSushii MaeAinda não há avaliações
- PersonalityDocumento45 páginasPersonalityPayal Gagneja100% (3)
- Case Chapter 15 - Nugraheni Vita Dyana - 041724353022Documento6 páginasCase Chapter 15 - Nugraheni Vita Dyana - 041724353022vidia2000Ainda não há avaliações
- Final Leadership PresentationDocumento42 páginasFinal Leadership PresentationSravya Akula100% (1)
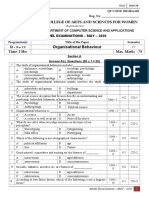
- Organisational Behaviour Model QP Set BDocumento4 páginasOrganisational Behaviour Model QP Set BKRISHNAMOORTHY KAinda não há avaliações
- Part 2 B, B1, B2, B3Documento23 páginasPart 2 B, B1, B2, B3Putri SeptiaAinda não há avaliações
- Bruce Perry PresentationDocumento8 páginasBruce Perry Presentationapi-24822325567% (3)
- Where Are Memories Stored - Queensland Brain Institute - University of QueenslandDocumento6 páginasWhere Are Memories Stored - Queensland Brain Institute - University of QueenslandHearthstone GiveawaysAinda não há avaliações
- CH 4 Discover My Values Plan of AnalysisDocumento2 páginasCH 4 Discover My Values Plan of Analysisapi-277405228Ainda não há avaliações
- Motivational Theories: Bba Group G Group 1 Organizational BehaviourDocumento41 páginasMotivational Theories: Bba Group G Group 1 Organizational BehaviourZargulAinda não há avaliações
- Combined Behavioral Intervention (CBI) : Project COMBINEDocumento360 páginasCombined Behavioral Intervention (CBI) : Project COMBINEКонстантин КрахмалевAinda não há avaliações
- What Your Handwriting Says About YouDocumento3 páginasWhat Your Handwriting Says About YouNestor LopezAinda não há avaliações
- Chapter 6 IctDocumento37 páginasChapter 6 IctJood ObeidatAinda não há avaliações
- Chapter 6 - Part 2 PDFDocumento31 páginasChapter 6 - Part 2 PDFFelicity JulietAinda não há avaliações
- Leader in MeDocumento17 páginasLeader in Mesalahmalik80% (5)
- Gratitude - WikipediaDocumento8 páginasGratitude - WikipediaDiana GhiusAinda não há avaliações
- DR Zarawi Mat Nor (USM)Documento39 páginasDR Zarawi Mat Nor (USM)Persatuan Pengajar Sains Kesihatan Bersekutu Malaysia (MAHSTA)Ainda não há avaliações
- (In An Acknowledged Overstatement... ) "Personality Is The Essence of A Human Being." (Hall & LindzeyDocumento4 páginas(In An Acknowledged Overstatement... ) "Personality Is The Essence of A Human Being." (Hall & LindzeyMichael AdamsAinda não há avaliações
- Toxic School EnvironmentDocumento2 páginasToxic School EnvironmentBernard Ah Thau TanAinda não há avaliações
- Marital Happiness ScaleDocumento1 páginaMarital Happiness ScaleJeffrey TurnerAinda não há avaliações
- Developmental and Learning TheoriesDocumento9 páginasDevelopmental and Learning TheoriesMer OyhAinda não há avaliações
- Organizational Communication WorksheetDocumento8 páginasOrganizational Communication WorksheetSyed Qaiser HussainAinda não há avaliações
- Stress LP AbrvDocumento3 páginasStress LP Abrvapi-307361008Ainda não há avaliações
- Dr. Robert AnthonyDocumento7 páginasDr. Robert AnthonyPramod B.Wankhade50% (2)
- How The Cannon-Bard Theory Works: Feel FearfulDocumento10 páginasHow The Cannon-Bard Theory Works: Feel Fearfulmarie geronaAinda não há avaliações
- Teaching PhilosophyDocumento5 páginasTeaching Philosophyapi-272013505Ainda não há avaliações
- Leadership & Team BuildingDocumento45 páginasLeadership & Team BuildingSachita Nand Mishra100% (1)
- Child and Adolescent Development LeakDocumento19 páginasChild and Adolescent Development LeakHailey ConstantinoAinda não há avaliações