Escolar Documentos
Profissional Documentos
Cultura Documentos
PANRE and PANCE Review Emergency Medicine
Enviado por
The Physician Assistant LifeDireitos autorais
Formatos disponíveis
Compartilhar este documento
Compartilhar ou incorporar documento
Você considera este documento útil?
Este conteúdo é inapropriado?
Denunciar este documentoDireitos autorais:
Formatos disponíveis
PANRE and PANCE Review Emergency Medicine
Enviado por
The Physician Assistant LifeDireitos autorais:
Formatos disponíveis
www.thepalife.
com
Emergency Medicine
aaoaoooaoaaaaaoaoSaoaooaooaaaoaooaaaaoaaaaaooooaaaaaoaa
Dr. Donald Sefcik
Donald J. Sefcik is the Associate Dean at the Chicago College of Osteopathic Medicine (CCOM), Midwestern University (N[WU), in Downers Grove, IL. He is a tenured professor and board certified in both Emergency Medicine and Family Medicine. From June 1997 through May 2000, Dr. Sefcik served as Medical Director for the Physician Assistant Program, Coliege of Health Sciences (CHS), at MWU. Dr. Sefcik's lectures are based upon his experiences as a clinician and preceptor, tenure as a medical school faculty member, and his student assessrnent research.
Dr. Sefcik has practiced with physician assistants since 1988 and been involved in the clinical training of physician assistants since 1990. Prior to joining Midwestem University's faculty, Dr. Sefcik was a faculty member in the Pharmacology Department at Butler University and in the Nursing Department at Marian College, both in Indianapolis, Indiana. Dr. Sefcik has a Bachelor of Science in Pharmacy (1981), a Master of Science in Pharmacology (1994), both from Butler University, ffid an MBA (May 2004) from Purdue University.
CME Resources Certification & Recertification Exam Review
www.thepalife.com
Cerffication & RecertiJication Exam Review
CME Resources 2004
Emergency Medicine Topics Donald J. Sefoik, D.O., FACOEP
Learning Objectives
Upon completion of flris portion of the review course, the participant should be able to:
2. Describe colnmon toxidromes and their management. 3. Differentiate the three common causes of primary headaches. 4. Discuss cofirmon secondary headaches. 5. Describe the evaluation/management of common ophthahnologic fraumatic injuries. 6. Discuss hyperkalemia - its presentation and management. 7. Discuss cerebrovascular accidents and traumatic brain injuries. 8. List and describe corrmon abnormal findings in urine specimens. 9. List and describe common physical examination "signs" and findings.
1.
Discuss the basic principles of toxicolory.
www.thepalife.com
Overdose Sfafes
ldentifu the Druq
A, History
Who was there ? What did they find out ? Are there any bottles ? Abiliiy to 'quantity'the ingestion ? Pafient's medical history ?
'
Time since ingestion
B. Physical Data
1 Rate-----r ,Z-.1 gz SignsBiood Pressure / Toxidrome \ (-symptoms. Temperature / -1 \Heart Rate Respiratory * Level of consciousness, Pupil size, Breath..,.etc.
Toxidromes
Signs
VIChssic Toxidromes ,-+ AnTih"sIr rer,AGS q)9..d\.W \ LhS''- L Cholinergic Aqents nnticno[nerqic A
-.
S - Salivaiion
..Nff)
opiates
(-
L.
Lacrimaiion
U - Urination D - Defecation G - Gl Distress
E - Emesis
Hyperemia (Red as a Beet) Dry Skin (Dry as a Bone) Dilated Pupils (Blind as a Bat) Delirium (Mad as a Hatter) Tachycardia
IVliosis Bradycardia Hypotension
Iin;.t\ p.ry',r(
ftr'\.rxo^e-\
Hypoveniilation Reduced LOC
Flo'ir:;
sG'rr'r'u-u
?d^pt(
Nomoqrams
Acute, One-time lnqestions
*Acetarninophen - Rumack-Matthew
*
Aspirin -
Done
( b e".,e
ncr\v:.ig-^
Y1
\
)
www.thepalife.com
(G
eneralizations - Common F eatures)
CIIARACTERISTICS
Age of Onset
MIGRAINE
Childhood-< 3Oyo
TENSION
Eariy Adulthood
CLUSTER
20-40
LIt".u" Lln s)
F>M
Frequenelt
M>>F
Variable
30 min - weelcs Cyclic,
yo \ (,f .. t 1
l-4 /.month
(Muitipie/day) Duratiott
Description Site Time of Onsa Associated Featura
+-tzLrs
"Throbbiag"
Unilateral (65%) Variable (often AIv!
10-120 mi:r
"Vise-like'l
Biiateral
Later in day
t'Boring"
Peri-orbital Uniiateral
Bed time
AA{A/
(75o/o)
Anorexia
Muscle tendemess
Ipsilateral
AI,IS Dvsfxn
Anu&x"cr--f f\C^u\C4 t t'O''ASl
Aggravatkg Factors (Precipitdingfaaors)
Clinical Appestance
Tredtments
Phono/photophobia 70% Fam.IIx C/assic - aura Common - no aura
Lacrimation Rhinorrhea Ptosis/miosis Stess/Fatigue
Multiple
Withdrawal from activify
Prescription Rx
Aicohol
Pace
Mild disability
MildAaalgesics
Agitated
02
Many Rxs
Abortive
Prophylactic
hsgrp"d','.\ h nl
s*-:t<;;Ae
rale,
www.thepalife.com
elect S econdarv Ileadaches
SUBARACHNOI D HEMORRHAGE Sudden Onset & Severity
Usually innamanial areurysm (beny) rupture
50%(+; with Altered LOC Average age = 50yq,..: . "Sentinel" Headache Hx in 30% 75% Neck Stifiness V.f e e-,),,n5 15% New-onset Seizures CT Scan Misses 10-20% (False Negative) If CT Scan is negative and suspicion is high, DO A LUMBAR PLINCTTIRE
- ,f s,3
Hemo6hagrt fup (False Positive) a i;t-) a;t $Rr-'! ,\ isl'\i.tr '' ltuf b. Cerebral Aagiography is the "GOLD" standard for diagnosis/aneurysm location RE FENNAL TO NE UROS URGE ON
a,
ii$e-
BRAIN TUMOR HEADACHES
Dull, deep aching, nondescript, progressive
Often worse on awakening Usually worsened by valsalva maneuver or exerlion May have nausea/vomiting or focal furdings Vomiting that precedes headache- think posterior fossa fimor
crscans$S+t,
MEI-.llNGtTlS HEADACHE
Usualiy involves entire head Often associated with feverivomiting Often associated with Nuchal signs
Kcrnig's Sign Brudzinski's sign
Diagnosis requires high index of suspicion and a lumbar pulcture
q HYPERTENSIVE HEADACHE
Usually a throbbing, occipital headache Most often a morning headache Usually does not occur until the diqslolic biood pressure ir Often overdianosed cause of headaches Treafinent- Antihypertensives
o:gi-]{mmHg'
\4.
L TEMPORAL ARTERITIS
Pa1*-*^g.r,.
Rh"o*.";!z^ Lfncrc\
Infiln'ation of Temporal Artery with lymphocytes, plasma cells and multinucleate giant cells Disease of patients over 50yo/ESR> 50 t Women with 4:1 predorninance \i LUI<a { c:hcui'} Unilaterai, jabbing pain/worse at night Artery tender/pulseless- Biopsy=Diagnosis '*?t'* 'r', \e154\ sui''i'h to prevent biindness ?,0 High dose
rry
pt7
i*Y
www.thepalife.com
Ophthalmologic Trauma
ORBIT & LID
L Contusion ("Black Eye") a, RIO Other Injury
2, Orb it al Wall' Fr hittn'
a.
e' 1;'
bi o,w o ut Fr ac fiir e ")
Flydraulic forces tbroughout the globe; rupture of medial wall and floor, fapping faVmuscle and occasionally injuring nerve
b, Findings: - Diplopia on upward gaze - Enophthalmos
)r
' Infraorbital anesthesia - Subcutaneous emphysema ;'glsuding" of Maxillary Sinus
Consult
c. Treatrnent-
CORNEA A CONJUNCTWA
-1..
Chemical Init;a:ies Do NOT Delay Treannent
!!!
a.
Alkali Bums - Liquefaction Nemosis - Irrigate (sometimes 24 hrs+) Check pH with litnus paper -Refer/ConsultNOW !
b. Acid Burns
- Coagulation Necrosis - hrigate & Consult
3. Radiation
Butns (Iieratitis)($T Vrr,*
I' beqn sK'rq\ 1 s*'b'<th'n1 *A
a.IJV radiation causes comeal epithelial sweliing; pain & bluned vision, hours afterthe
exposure
a^reas
,s
ut4\})
Jce r,vr k RiSn
g(i\6b Lorrta {*TfD,.Ly. bdY
r
b.
Findings
Multiple Punctate
on fluorescein
staining
b,
Trearnent
- Mydriatic - Systemic Analgesic - Follow-up
agent
()- p*,{Jt \:2/
www.thepalife.com
4. Corneal Abrasions
a. b.
Complaint of foreign body "feeling"
Findings
- Foreign Body (+l) s Check Lid in eversion
c.
"Ice Rink Sign" with fluorescein
Treatnent
- Cycloplegic Agent
- Antibiotic topically - Follow-up in 24-48 hrs
. Sub conj
mctiv al Hemorchage
a. Bright Red blood overlying sciera b. Be sure no bleeding diathesis exists c. Blood Stops at limbus
d. Should NOT affect vision
e. No specific therapy
ANTERTOR CHAMBER & LENS
l.
Traumatic Hyphema
a. Blood in anterior charrber due to ciliary body or iris vessel disruption b. Best seen with patient sitting upright with slit lamp
c. Must R/O other iqiuries d. Findings - MaY be ary':nPtomatic - PainlPhotophobia.tslured Vision - May cause N & V e. Consult OphthaLnologist - Place a FOX Eye shield - Keep patient quiet @ 30-45 degree angle Risk of secondary glaucoma
2. Lens Dislocation a. Marked VA Decrease b. May be seen in Marfan's Syndrome
c. Consult your OphthaLnologist
3
. Tr^aumatic Mydriasis a.lmpairrrent of PSNS function b. Referffsualiy temporary
www.thepalife.com
^ ^ F{I?ERLATEMLA q R
t"rl
/o
L.,\rrnue\\u;\er
1. Definition
An elevated plasma potassium level (usually > 5.0 mEq/I-)
2. Pathophysiology
Hod\4/hy
does
it happen
Etiology L lncreased Potassium Load
a, Exogenous
t\,8
- Excess intake; Dietary; Suppiemental, .,
-Xedun'ibution t 'T uf)ll .r \r'so"o*htq\rb'^ Kt Y. 1, Hemolysis; lnsulin deirciency; Exercise . C'-t Acidosis: .KAJ 6r C G], \ 2. Decreased Excrerion b, Endogenous
Kr Lh.,ire kt" \
Renal Failure; Rx Effect: NSAIDs; ACE inhibitors; K-Sparing Diuretics
3. Factitious -
Hemolysis (of
Sims/Symptoms
sp
ecimen) ; Leuko cytosis ; Thromb
cyto sis ; Phiebotomy
Cardiac
Peaked T-waves
Fiat P-waves Widened QRS Y" V entricuiar fi brillation
^jU-*.-.-llh-t
Neuromusc-
Paresthesias
Weakness
Fiaccidity
^ni\**
/JWII.
3. Differential Diagnosis -
Hypocalcemia Neuromuscular disorder
EKG abnormalities from other cause
4. Treatment Plan a, Rx
Sodi'hpolystlrene
s{Y:}G\GXALATE)
orally or rectaiiy
More sevet'e cases (Cardiac arrhythnzias, etc) may require: Dextrose & Insulin fV - temporizing measure/shifts potassium intracellular S o dium B i carb onate - temp orizin g measure/shifts potas sium intraceilular Calcium Giuconate - cardioprotective/potassium antagonist c, Other
*\u_le"ut "{X s.
Hemodialysis
www.thepalife.com
Cerebrovascular Accidents (CVAs)
FACTS & FIGURES
A.
lncidence @ 730,000 per year
B. Risk Factors
Uncontrollable
a. b.
Advancing {ge - 2/3 occur in patients > 65 yo feach decade after 55 yo doubles the risk......] Gender:Verr t Women Diabetes mellitus:
c. Family History: CVA or TIA
d.
- 23 times the risk
Controllable
a.
b,
Hypertension:
- 4-
6 tirnes the risk
olo
A contributing factor in up to 70
of all CVAs
Atrial Fibrillaiion: - up to 6 iimes the risk A contribuiing factor in up to 15 % of all CVAs
lschemic Attack (TlA) Risk of a CVA is - 35 % wiihin 5 years
,c, Transient
d.
Cigarette smoking:
-2-3 times the risk
e.
Males:
Prior CVA
Females:
42 o/o risk of a second CVA within 5 years 24 % risk of a second CVA within S years
f,
Others: Myocardial lnfarction, Hypercholesterolemia, Sleep apnea
STROKE SYNDROMES
lschemic Attack (TlA) + - transient neurologic deficii, ihat by definition, lasts less than 24 hours rF 't - - 90 % last less than 60 minutes (many < 15 minutes) - Amaurosis fugax - transient, partial or complete monocular blindness - Rule of 1/3s r' 1/3 will have a CVA in \f l4l ,,r.,.1*",.trJ ./ 1/3 will have a second the future TIA ,/ 1/3 will have no sequelae \r rD^ lz.i fr. ir,l{ B, Lacunar lnfarct (Deep Subcortical/"Whiie Matter" Area Changes; - Contralateral PURE Motor Deficit (lnternal capsule) lj'T N) pt - Contralateral PURE Sensory Deficii (Thalamus) - Clumsy Hand - Dysarthria (Pons or lnternal capsule)
- Nofes
A. Transient
-LC
www.thepalife.com
Intracranial l{emorrhagic Events
Irrlr'acranial Hemorrhage
Snbarachnoitl llemorrhage
Cerebral Ischemic Evenl.s
l'hrombotic CYAs
Ernbolic CVAs
Onset/Progressiou
Ol-ten actiye at onset Rapid progression
May be active/nonactive Variable course
50% comatose at
Nonacl.ive at onset - 60 % during sleep Gradual progl'ession
Active at onset
Rapicl onset
presentation)
Etiology
Aneurysm (berry)
Itisk(s)
Ilypertension Bleeding Diathesis
Associated with polycystic
kidney disease aud aortic coarctation
fuleriosclerosis [Iypeftensiorr Diabetes Mellitus
I-Ieart (Valvular) Disease
furatomic Locatiott
Middle cerebralartery (comnon)
History
Severe Cephalgia
Severe Cephalgia
Stiff neck May be lristory of altered
level ofconsciousness
tlsually no Cephalgia Often history of TtAs
Usually no Cephalgia
Physical Exanr
Focal Neurological Signs
Nonfocal exam Nuchal rigidity
Focal Neurological Signs
Focal Neurological Signs
hrteural Carotid Bruit(s)
www.thepalife.com
Arteny'Site of Involvernent
lnternal Carotid Artery
Character-istic Feature(s) of CYA
Ipsilateml Monocular Blindness (Anaurosis Fugax) Contmlateral Herniparesis Contralateral l{emianesthesia/Hemianalgesia
Contralateral Lower Extremity paresis; aneslhesia,./analgesia Minirnal Contralateral Upper Extremity No Face Clnnges Contralateral Upper Extrcmities paresis; anesthesia/analgesia Contralateral Lower Face droop (Tongue cleviates to sicle opposite of lesion; no fasiculal.ions) Minimal/No Lower Extrernify Changes Aphasia (if dorninant hemisphere is involved) Contralateral l{omonymous Hemianopsia (rvith macu|ar sparing) Ipsilateral Cranial Nerve III Palsy Memory deficits (if hippocarnpus is involved)
Auterior Cerebral Artery
Middle Cerebral Artery
Posterior Cerebral Artery
Vertebrobasilar Artely
Diplopia (PPRF or CN ltr, fV, VD Watch for CN dysftrnction Ataxia / Vertigo (cerebellar signs) Bilateral Motor/Sensory Changes
Purc Motor (basilar pons or internal capsule) conlralateral to lesion Pure Sensory (thalalnus) contralateral to lesion Clurnsy I-Iand-Dysaltlu ia
Lacunar CVA
www.thepalife.com
Traumatic Brain Iniuries
FACTS & F/GURES
A. lncidence
a. - 2 million Americans with Head Trauma annually b, - 500,000 are admitted to the hospital c, - 100,000 deaths per year (- 60 % occur before arrivalto the ED) d, Aicohol consumpiion is involved in - 25 - 50 % of cases B. Classificaiions (arrival to ED) a. Mild Head lniury EYE Ooeninq 4
3 2
1
GLASGOW COIvIA SCALE
.ay
n
erra$1^*J ^. .. h{'-1 -( ' d9. n v-.<v"' b, Moderate Head lniurv ecs=9-13 d'n*>Z
oof' \
-ze%die
c. Severe head lniury
GCS=14-15
80 % of rniuries
Spontaneous To soeech To Pain No response
VERBAL Response
5
Alert & Oriented
Disoriented Nonsensical soeakino Moans/Unintelliqible sounds No response
-1o%oflnjuries
4
3
2
1
-40%die
- 10 % of lnjuries
GCS=Eorless
MOTOR Response
6
4
5
I
1
Follows commands Localizes pain Withdrawals from oain Decorticate posturinq Decerebrate posturinq No response
,R
C. Tvpes of Brain lniurv FO RCE(-1 00 ms)
Primary Injury
NeuralTissue ^/ lniuru
Contusion Laceration Difiuse Axonal lnjury
\.|
Cerebral
V ascul ar
I
niury
lntraparenchymal Hemorrhage Epidural Hematoma Subdural Hematoma Subarachnoid Hemorrhage
Secondary lnjury
Hypotension Hypoxemia Hypovolemia lncreased lntracranial Pressure
www.thepalife.com
SPECIFIC DIAGNOSTIC ENTITIES
cLosED "
{-Eng-aryAl
me''"5 r'rdrrrS Epidurai Hematota * SKr\ Rnr\.nc, I
i
rec Lesions
#hcrL,'.a'h
-l
,/ - 1 % of all traumatic brain injuries (- 12 % die) ./ - 80 - 90 % associated wiih a skull fracture (often tears a meningeal artery) \/ Only - 20 % have classic: lnjury - LOC - Lucid lnterval - Deterioration
Up to 60 % have no loss of consciousness Underlying brain injury is generally not severe 60 % occur in patients < 20 yo < 10 % occur in patients > 50 yo
'/ ./ r'
'v\.{a.
'/ '/ rrtsvln'r' -i*).,n *W"Y a' \
qJ-
Subdural Hematorna - 35 % of severe traumatic brain injuries Most occur in patients > 60 yo * Atrophic brains (elderly and alcoholics) are at greatest risk
l6$ff:l''}jr" l'F [6scAriem.,t
il
. t . ^. i,",*.r
'v
yd
vn,,X
-
'- J
i '/
mechanisms Underlying brain injury is generally more severe * Simple (no associated parenchymal injury - - 20 % die) * Complicated (associated brain injury - - 50 % die)
Hffiliil3.tffii$;,ti:1?H,ltiJlla...r.,"tion
Subarachnoid Bleed (Hemorrhage)
(:f1s(,^f/
b. lntra-axial Lesions - Cerebral Coniusions & Lacerations * Concussions
4t
Cn^
it:ru'cr{t,t\
cYc [c'-
- Diffuse Axonal lnjuries (Axonal Shearing)
lncreased lntracranial Pressure
- Herniation Syndromes
. Cushing Response (hyperiension; bradycardia; irregular respirations)
OPEN a. Penetrating lnjuries
www.thepalife.com
t,'
.-
f ro.'lrrt
INITIAL EVALUATION & TREATMENT
A, Salvage brain tissue not already irreversibly injured B. ldeniifyicorrect eniiiies that may cause secondary injury
tqtut ' t
/-'"'''
'
LFr"rl'+tt
lnjury
lmmobilize cervical spine (GCS < 6 = 14 % have C1 or C2 fracture)
GCS<9
lntubate (ETT) Hyperventilate lVs Monitors Resuscitate Sedation/Paralysis Secondary Survey (Life Threats....,)
GCS>9
lVs Monitors Frequent Serial Examinations (NEURO) Secondary Survey Monitor for ETTiHyperventilaiion need
,/ /
CT Scan
,/
4--""'
Neurosureeon
E lev ated Inttucranial Pressure Hyperventiiation Mannitol
Pentobarbiotai
----a
Operative Lesion
Epidural Hematoma Subdural hematoma lntracranial Hemorrhage with shift Depressed Skull Fracture
Non-Operative Lesion
Non-Depressed Skull Fracture Contusion Subarachnoid Hemorrhage
Causes
A. Causes
Motor Vehicle Accidents (MVA) - 45 o/o (cause - 60 % of deaths) Falls - 15 % (cause - 12 0/o of deaths) Assaulis - 14 o/o (Firearms - 14 o/o of deaths - approximately 75 o/o occur at the scene) OccupationalAccidents 10 % RecreationalAccidents 10 %
B.
Prevention
c. Firearm Legislation
a. Safety (Seat) Belts and Air Bags b. Helmets
www.thepalife.com
Considerations at Presentation:
a. Low-risk lniuries
- Not likely to deteriorate - Normal neurologic examination * Asymptomatic; Subjective complaints: Headache, Dizzy... .,. - Minor injury: * Scalp wound Hematoma, Abrasion, Laceration....
*"* Approximately 0,3
3 % will deteriorate
b. Moderate -risk lniuries
- Difficult group to ass.ign a prognosis - Neurologic Signs & Symptoms of unclear significance " Brief LOC; Vomiting; Post-traumatic amnesia.....
* Progressive headache; Child age < 2 yo..
- lnjury (?):
" Arduous Assessment to make (Work-up ???) *** Approximately 40 % will have an abnormal CT scan
** Approximately I
% will need a neurosurgical procedure
*n Approximately 10 % will deteriorate
c. Hiqh-risk lniuries
- Criteria-defined neurosurgical emergencies
- Neurolog ic Assessment dem onstrates si gnificant findings * Depressed LOC (not explained by drugs, EIOH...) * Focal Neurologic signs
" Decreasing LOC
* Skull Penetration or Depressed Fracture
- lnjury: Suspect Primdry or Secondary Brain lnjury
*** Approximately 25 % will need a neurosurgical procedure
References
Manual of Neurology; McGraw-Hill 2002 (0-07-137351-9) Handbook of Neurosurgery; Thieme New York; 2001 (0-865Z7-909-0) Emergency Medicine Reporls December 3, 2001: Head Trauma: Emergency Management and lmaging December 17,20Q1: Head Trauma: Severe, Moderate and Minor Head Trauma May 11, Traumatic Brain lnjury: State-of-the-Art Proiocols
1998:
Você também pode gostar
- Panre and Pance Review Cardiovascular IIDocumento26 páginasPanre and Pance Review Cardiovascular IIThe Physician Assistant Life100% (1)
- PANRE and PANCE Review NeurologyDocumento15 páginasPANRE and PANCE Review NeurologyThe Physician Assistant Life60% (5)
- PANRE and PANCE Review PsychologyDocumento35 páginasPANRE and PANCE Review PsychologyThe Physician Assistant LifeAinda não há avaliações
- Clinicial Thinking and Test Taking PANRE and PANCEDocumento12 páginasClinicial Thinking and Test Taking PANRE and PANCEThe Physician Assistant Life100% (2)
- EENT PANCE and PANRE Content Blueprint Patient PresentationsDocumento8 páginasEENT PANCE and PANRE Content Blueprint Patient PresentationsThe Physician Assistant LifeAinda não há avaliações
- PANRE and PANCE Review Infectios DiseaseDocumento32 páginasPANRE and PANCE Review Infectios DiseaseThe Physician Assistant Life100% (1)
- PANRE and PANCE Review Antimicrobial PharmacologyDocumento27 páginasPANRE and PANCE Review Antimicrobial PharmacologyThe Physician Assistant Life100% (2)
- PANCE Antimicrobial Review BlueprintDocumento40 páginasPANCE Antimicrobial Review BlueprintFlora LawrenceAinda não há avaliações
- Pneumonia and ID PANCE ReviewDocumento107 páginasPneumonia and ID PANCE ReviewFlora Lawrence100% (1)
- Chapter 1 CardiologyDocumento48 páginasChapter 1 CardiologyAnh100% (2)
- Pance Review Q&ADocumento40 páginasPance Review Q&ABetsy Issac Pidugu100% (2)
- PANCE Prep Pearls Valvular DiseaseDocumento4 páginasPANCE Prep Pearls Valvular Diseasekat100% (2)
- Packrat 3-21-14 AnswerDocumento40 páginasPackrat 3-21-14 AnswerChristina Ly100% (1)
- PANRE and PANCE Review Cardiovascular IDocumento21 páginasPANRE and PANCE Review Cardiovascular IThe Physician Assistant LifeAinda não há avaliações
- Rutger's PANRE and PANCE Practice Questions 1 of 2Documento35 páginasRutger's PANRE and PANCE Practice Questions 1 of 2nubianlocks100% (3)
- PA - Coursepack DAY 1Documento352 páginasPA - Coursepack DAY 1Elly NuñezAinda não há avaliações
- PANCE/PANRE Cardiovascular and Pulmonary Word AssociationsDocumento27 páginasPANCE/PANRE Cardiovascular and Pulmonary Word Associationst2091100% (1)
- PA Practice 13Documento34 páginasPA Practice 13sweetiex3100% (1)
- PANCE Prep Pearls Cardio Questions PDFDocumento9 páginasPANCE Prep Pearls Cardio Questions PDFkat100% (3)
- Rosh ReviewDocumento125 páginasRosh ReviewPrince Du100% (2)
- RoshDocumento55 páginasRoshHuy Hoang100% (2)
- Internal Medicine EOR-PrintDocumento276 páginasInternal Medicine EOR-PrintDanielle GroupfiveAinda não há avaliações
- Sample Questions and CritiquesDocumento14 páginasSample Questions and CritiquesaayceeAinda não há avaliações
- PANCE Pearls Master 2013Documento19 páginasPANCE Pearls Master 2013Haley Shields100% (7)
- Cardiovascular PANCE Review GuideDocumento11 páginasCardiovascular PANCE Review GuidePhysician Assistant Review100% (1)
- End of Rotation Exam Sample-Exam PDFDocumento27 páginasEnd of Rotation Exam Sample-Exam PDFDanielle GroupfiveAinda não há avaliações
- PANCE Table Review: Study Stack for PANCE Exam QuestionsDocumento34 páginasPANCE Table Review: Study Stack for PANCE Exam Questionsjrubin83669Ainda não há avaliações
- Packrat Form 9Documento102 páginasPackrat Form 9PhysAssistant75% (4)
- Surgery PackratDocumento46 páginasSurgery PackratRicardo Nelson100% (4)
- Packrat 15Documento86 páginasPackrat 15enh0219100% (8)
- Questions: Questions All Things Pa-C - Free Practice QuizDocumento12 páginasQuestions: Questions All Things Pa-C - Free Practice QuizJaellah MatawaAinda não há avaliações
- Cardiology Study Guide HandoutDocumento86 páginasCardiology Study Guide Handoutalinida89100% (1)
- PANCE Prep Pearls GI Questions PDFDocumento10 páginasPANCE Prep Pearls GI Questions PDFkat100% (1)
- Packrat 14 PDFDocumento86 páginasPackrat 14 PDFkat100% (1)
- Obgyn SGDocumento40 páginasObgyn SGNatalieAinda não há avaliações
- Packrat Cardio QuestionsDocumento63 páginasPackrat Cardio Questionscrystalshe100% (1)
- PACKRAT Cardio Questions PDFDocumento63 páginasPACKRAT Cardio Questions PDFkat100% (1)
- PANCE - Endo Review 2020Documento56 páginasPANCE - Endo Review 2020Siam100% (1)
- Packrat 14 - 2009Documento86 páginasPackrat 14 - 2009EmersonMoreno80% (5)
- Rutger's PANRE and PANCE Practice Questions 2 of 2Documento38 páginasRutger's PANRE and PANCE Practice Questions 2 of 2nubianlocks100% (3)
- Word AssociationDocumento27 páginasWord AssociationMilan Kolovrat100% (1)
- 750 Flashcard Questions PAPrep Copy 2 2Documento54 páginas750 Flashcard Questions PAPrep Copy 2 2Mary Anne Lerma- PetersonAinda não há avaliações
- Peds EORDocumento17 páginasPeds EORRachel BarrosAinda não há avaliações
- Pakrat 10Documento67 páginasPakrat 10towexpertAinda não há avaliações
- Packrat 15 - 2010Documento86 páginasPackrat 15 - 2010EmersonMoreno80% (5)
- Rosh EbookDocumento825 páginasRosh EbookLeila Nabavi100% (2)
- High Impact OutlineDocumento13 páginasHigh Impact OutlineHannah JosephAinda não há avaliações
- Packrat 12Documento80 páginasPackrat 12vkamdar87100% (4)
- Pance Prep Pearls AntibioticsDocumento14 páginasPance Prep Pearls Antibioticskat100% (4)
- Master the Physician Assistant National Recertifying Exam (PANRE)No EverandMaster the Physician Assistant National Recertifying Exam (PANRE)Ainda não há avaliações
- Physician Assistant PANCE & PANRE: a QuickStudy Laminated Reference GuideNo EverandPhysician Assistant PANCE & PANRE: a QuickStudy Laminated Reference GuideAinda não há avaliações
- NATIONAL CERTIFYING EXAMINATION FOR PHYSICIAN'S ASSISTANT (PA/NCE): Passbooks Study GuideNo EverandNATIONAL CERTIFYING EXAMINATION FOR PHYSICIAN'S ASSISTANT (PA/NCE): Passbooks Study GuideAinda não há avaliações
- The 10-Minute Physical Exam: recognizing medical syndromesNo EverandThe 10-Minute Physical Exam: recognizing medical syndromesAinda não há avaliações
- Physician's Assistant: Passbooks Study GuideNo EverandPhysician's Assistant: Passbooks Study GuideAinda não há avaliações
- Step 3 Board-Ready USMLE Junkies 2nd Edition: The Must-Have USMLE Step 3 Review CompanionNo EverandStep 3 Board-Ready USMLE Junkies 2nd Edition: The Must-Have USMLE Step 3 Review CompanionAinda não há avaliações
- EENT PANCE and PANRE Content Blueprint Patient PresentationsDocumento8 páginasEENT PANCE and PANRE Content Blueprint Patient PresentationsThe Physician Assistant LifeAinda não há avaliações
- Episode 25 - The Audio PANCE and PANRE Physician Assistant Board Review PodcastDocumento4 páginasEpisode 25 - The Audio PANCE and PANRE Physician Assistant Board Review PodcastThe Physician Assistant LifeAinda não há avaliações
- The Audio PANCE and PANRE Episode 23 - The Physician Assistant LifeDocumento5 páginasThe Audio PANCE and PANRE Episode 23 - The Physician Assistant LifeThe Physician Assistant LifeAinda não há avaliações
- The Audio PANCE and PANRE Episode 13Documento4 páginasThe Audio PANCE and PANRE Episode 13The Physician Assistant LifeAinda não há avaliações
- The Audio PANCE and PANRE Episode 9Documento4 páginasThe Audio PANCE and PANRE Episode 9The Physician Assistant Life100% (1)
- The Audio PANCE and PANRE Episode 15Documento4 páginasThe Audio PANCE and PANRE Episode 15The Physician Assistant Life100% (1)
- Episode 19 - The Audio PANCE and PANRE Board Review Podcast - The Physician Assistant LifeDocumento5 páginasEpisode 19 - The Audio PANCE and PANRE Board Review Podcast - The Physician Assistant LifeThe Physician Assistant LifeAinda não há avaliações
- The Audio PANCE and PANRE Episode 17Documento4 páginasThe Audio PANCE and PANRE Episode 17The Physician Assistant LifeAinda não há avaliações
- The Audio PANCE and PANRE Episode 7Documento4 páginasThe Audio PANCE and PANRE Episode 7The Physician Assistant LifeAinda não há avaliações
- The Audio PANCE and PANRE Episode 11Documento4 páginasThe Audio PANCE and PANRE Episode 11The Physician Assistant Life100% (1)
- Statin Trial SummaryDocumento1 páginaStatin Trial SummaryThe Physician Assistant LifeAinda não há avaliações
- Physician Assistant Application Letter of Recommendation Sample 1Documento1 páginaPhysician Assistant Application Letter of Recommendation Sample 1The Physician Assistant Life100% (1)
- The Turkey Book - An Introductory Manual For The WardsDocumento147 páginasThe Turkey Book - An Introductory Manual For The WardsThe Physician Assistant LifeAinda não há avaliações
- PANRE and PANCE Review Antimicrobial PharmacologyDocumento27 páginasPANRE and PANCE Review Antimicrobial PharmacologyThe Physician Assistant Life100% (2)
- Physician Assistants in Primary Care Trends and CharacteristicsDocumento5 páginasPhysician Assistants in Primary Care Trends and CharacteristicsThe Physician Assistant LifeAinda não há avaliações
- Physician Assistant Applicant Letter of Recommendation Sample 2Documento1 páginaPhysician Assistant Applicant Letter of Recommendation Sample 2The Physician Assistant Life100% (3)
- PANRE and PANCE Review Cardiovascular IDocumento21 páginasPANRE and PANCE Review Cardiovascular IThe Physician Assistant LifeAinda não há avaliações
- Management of Lacerations in The Emergency DepartmentDocumento27 páginasManagement of Lacerations in The Emergency DepartmentThe Physician Assistant LifeAinda não há avaliações
- Physician Assistant Cover Letter SampleDocumento1 páginaPhysician Assistant Cover Letter SampleThe Physician Assistant LifeAinda não há avaliações
- The Truth About Salt and Your Health Why Potassium May Be The AntidoteDocumento8 páginasThe Truth About Salt and Your Health Why Potassium May Be The AntidoteThe Physician Assistant LifeAinda não há avaliações
- PANRE and PANCE Review Infectios DiseaseDocumento32 páginasPANRE and PANCE Review Infectios DiseaseThe Physician Assistant Life100% (1)
- When A Parent Has Cancer How To Talk To Your KidsDocumento47 páginasWhen A Parent Has Cancer How To Talk To Your KidsThe Physician Assistant Life100% (1)
- Physician Assistant Certification and Recertification Exam Review - PANRE - PANCEDocumento14 páginasPhysician Assistant Certification and Recertification Exam Review - PANRE - PANCEThe Physician Assistant Life100% (3)
- Hobby 01: COD. 9942062.01 REV. 00Documento9 páginasHobby 01: COD. 9942062.01 REV. 00Alexander SharamiginAinda não há avaliações
- MACRO XII Subhash Dey All Chapters PPTs (Teaching Made Easier)Documento2.231 páginasMACRO XII Subhash Dey All Chapters PPTs (Teaching Made Easier)Vatsal HarkarAinda não há avaliações
- Kaustubh Laturkar Fuel Cell ReportDocumento3 páginasKaustubh Laturkar Fuel Cell Reportkos19188Ainda não há avaliações
- NNDC Planning Applications 4oct - 11 OctDocumento4 páginasNNDC Planning Applications 4oct - 11 OctRichard SmithAinda não há avaliações
- Clay ShonkwilerDocumento9 páginasClay ShonkwilerJeoff Libo-onAinda não há avaliações
- SI44M 60H 80H-DeN1730-V12web DownloadedDocumento4 páginasSI44M 60H 80H-DeN1730-V12web DownloadedtauraimukumbaAinda não há avaliações
- 2009 ESC Guidelines On EndocarditisDocumento45 páginas2009 ESC Guidelines On EndocarditisDaondy Friarsa SoehartoAinda não há avaliações
- Vertical Jaw Relation Recording MethodsDocumento17 páginasVertical Jaw Relation Recording MethodsHarish VsAinda não há avaliações
- Coley A4Documento49 páginasColey A4mfiarkeeaAinda não há avaliações
- Nutrition Effects of VitaminsDocumento21 páginasNutrition Effects of Vitaminsblessed cccAinda não há avaliações
- Abbey Pain Scale assessment toolDocumento2 páginasAbbey Pain Scale assessment toolMuhammad RezgiaAinda não há avaliações
- JMJ Marist Brothers Notre Dame of Marbel University Integrated Basic Education Department City of Koronadal, South CotabatoDocumento13 páginasJMJ Marist Brothers Notre Dame of Marbel University Integrated Basic Education Department City of Koronadal, South CotabatoNestor Gerotape DiosanaAinda não há avaliações
- Mathematics: Minimum Level Learning MaterialDocumento60 páginasMathematics: Minimum Level Learning MaterialTusar SardarAinda não há avaliações
- 20 N 60 C 3Documento13 páginas20 N 60 C 3rashidmirzaAinda não há avaliações
- ###Questions Model PDFDocumento2 páginas###Questions Model PDFDave DMAinda não há avaliações
- Tracking sports training efficiency with surface EMGDocumento8 páginasTracking sports training efficiency with surface EMGsdjuknicAinda não há avaliações
- BBO 2011 ROUND 2 QUESTIONSDocumento16 páginasBBO 2011 ROUND 2 QUESTIONSMalvina YuanAinda não há avaliações
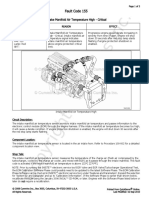
- Fault Code 155: Intake Manifold Air Temperature High - CriticalDocumento3 páginasFault Code 155: Intake Manifold Air Temperature High - Criticalhamilton miranda100% (1)
- History of Cancer ChemotherapyDocumento9 páginasHistory of Cancer ChemotherapyJoydeep MajumdarAinda não há avaliações
- Dell Precision Workstations: The #1 Workstations in The WorldDocumento7 páginasDell Precision Workstations: The #1 Workstations in The WorldDiego RodriguezAinda não há avaliações
- L4004N - 0920 - Nilfisk - Robotic-brochure-Liberty SC60Documento12 páginasL4004N - 0920 - Nilfisk - Robotic-brochure-Liberty SC60Lucianderson Marques FerreiraAinda não há avaliações
- NQ-NQM Panelboards and Qonq Load Centers Information Manual 80043-712-06 Rev.02 06-2015 2 PiezasDocumento144 páginasNQ-NQM Panelboards and Qonq Load Centers Information Manual 80043-712-06 Rev.02 06-2015 2 PiezasNadia EspinozaAinda não há avaliações
- Monsterology Activity KitDocumento2 páginasMonsterology Activity KitCandlewick PressAinda não há avaliações
- ASME B31.4-2016 Pipeline Transportation Systems For Liquids and SlurriesDocumento1 páginaASME B31.4-2016 Pipeline Transportation Systems For Liquids and SlurriesJose Rodrigo Salguero DuranAinda não há avaliações
- Mathematics 5 Q1 W10Documento31 páginasMathematics 5 Q1 W10Aices Jasmin Melgar BongaoAinda não há avaliações
- I Wanna Be Yours Arctic Monkeys Love SongDocumento3 páginasI Wanna Be Yours Arctic Monkeys Love SongAndréia E NiltonAinda não há avaliações
- Artikel Ilmiah FikriDocumento6 páginasArtikel Ilmiah FikriViola Mei DamayantiAinda não há avaliações
- 03.can-Bus and Sae-Bus j1939 - CatDocumento29 páginas03.can-Bus and Sae-Bus j1939 - CatEdison Pfoccori BarrionuevoAinda não há avaliações
- CIVL-365 Tutorial 8 SolutionDocumento3 páginasCIVL-365 Tutorial 8 SolutionIvsAinda não há avaliações
- Global Warming Is The Term Used To Describe A Gradual Increase in The Average Temperature of The EarthDocumento6 páginasGlobal Warming Is The Term Used To Describe A Gradual Increase in The Average Temperature of The EarthSaswataBhattacharyaAinda não há avaliações