Escolar Documentos
Profissional Documentos
Cultura Documentos
SKIN Notes 2012
Enviado por
anisuafuraDescrição original:
Direitos autorais
Formatos disponíveis
Compartilhar este documento
Compartilhar ou incorporar documento
Você considera este documento útil?
Este conteúdo é inapropriado?
Denunciar este documentoDireitos autorais:
Formatos disponíveis
SKIN Notes 2012
Enviado por
anisuafuraDireitos autorais:
Formatos disponíveis
PATHOLOGY OF THE INTEGUMENTARY SYSTEM
Paul Hanna Systemic Pathology II (VPM 222)
(http://people.upei.ca/hanna)
Winter 2012
Reference texts: Pathologic Basis of Veterinary Disease, Zachary, McGavin (ed): 5th edition (2012), Chapter 17 Pathology of Domestic Animals, Maxie (ed), 5th edition (2007), vol 1, Chapter 5
Source: Textbook of Veterinary Histology, Lea & Febiger, 1976
1. Skin (cutis) Epidermis Layers - corneal, ( granular), spinous, basal. Cells - keratinocytes, melanocytes, Langerhans' cells, Merkel cells. Adnexa - hair, glands (sebaceous, apocrine, eccrine - - circumanal, tail, anal), claws and hooves. Dermis Fibers (collagen, reticulin, elastin), ground substance (glycosaminoglycans, proteoglycans), cells (fibroblasts, mast cells, histiocytes, smooth muscle), vessels (blood, lymph), nerves. 2. Hypodermis (subcutis) Lipocytes (panniculus adiposus, digital cushion), fibers (collagen, elastin), vessels, nerves. GENERAL FUNCTIONS Enclosing barrier (moisture in), protection (physical, chemical, microbiological), sensory (touch, temperature, pressure, pain, itch), temperature & blood pressure regulation (hair coat, sweat glands, blood vessels), storage (water, electrolytes, vitamins / vitamin D production, fat, CHO, proteins, etc), adnexa production (hair, claws / hooves, horn, etc), pigmentation (coloration and UV protection), immunoregulation / antimicrobial action. RESPONSE OF SKIN TO INJURY Because the skin is the largest organ of the body and is in direct contact with both the external and internal environments, it is susceptible to a wide range of insults. The skin has a limited range of responses, thus histopathology of punch biopsies and other ancillary tests are often required to determine the etiology.
Dermatopathology
2 -----------------------------------------------------------------------------------------------------------------------------------
Winter 2012
GROSS MORPHOLOGY OF SKIN LESIONS PRIMARY LESIONS - are the direct result of the underlying disease process; most important diagnostically a) Macule -a circumscribed, area of discoloration (eg pigmentation, hemorrhage) up to 1 cm in diameter. b) Patch - a macule over 1 cm in size. c) Papule - a small (< 1 cm diameter) solid elevation of the skin. d) Plaque - a larger, flat-topped elevation formed by the extension or coalescing of papules. e) Nodule - a circumscribed, solid elevation >1 cm in diameter that usually extends into the deeper layers. f) Tumor - a large mass (neoplasia implied) that may involve any structure of the skin or subcutis. g) Cyst - an epithelial lined cavity in the dermis or subcutis containing fluid or semisolid material. h) Vesicle - a well circumscribed, < 1 cm diameter, elevation of the epidermis, filled with clear fluid. i) Bulla - a vesicle (blister) > 1 cm diameter. j) Pustule - a small, circumscribed, pus filled elevation of the epidermis. k) Abscess - a well demarcated fluctuant lesion resulting from dermal or subcutaneous accumulation of pus. l) Wheal - a sharply circumscribed, raised lesion due to dermal edema; will blanch with pressure. SKIN LESIONS THAT MAY BE PRIMARY OR SECONDARY a) Scale - an accumulation of loose fragments (flakes / dandruff) of cornified skin; can be primary (eg primary seborrhea) or secondary (eg chronic inflammation). b) Crust - accumulation of dried material (eg exudate, blood /serum, scale, medication) on skin surface; can be primary (eg primary seborrhea) or secondary (eg self-trauma, pyoderma, etc). c) Comedo - a hair follicle lumen plugged with cornified cells and sebaceous material; can be primary (eg Schnauzer comedone syndrome) or secondary (eg demodecosis). d) Abnormalities of hair Alopecia - partial to complete loss of hair (baldness); can be primary (eg endocrine disease, follicular dysplasia) or secondary (eg with self-trauma or inflammation). Hypotrichosis / atrichia - less hair than normal or absence of hair (ie failure to develop). Effluvium / defluxion - excessive shedding or falling out of the hair. Hypertrichosis (hirsutism) - excessive growth of hair. e) Abnormal Pigmentation or Coloration Red (erythema) - inflammation / vasodilation Black - hypermelanosis (melanoderma) / melanotrichia White - hypomelanosis (leukoderma) / leukotrichia / albinism Red-purple-brown-black - purpura (macular hemorrhage < 1cm = petechiae, > 1cm = ecchymoses) Yellow - icterus Blue - cyanosis SECONDARY LESIONS - evolve from primary lesions, via self-trauma, altered keratinization, etc. a) Epidermal collarette - a circular rim of keratin flakes following loss of the roofof a vesicle or pustule. b) Erosion - a shallow epidermal defect that doesn't penetrate the basal laminar zone; heals without scarring. c) Ulcer - a break in the epidermis with exposure of the underlying dermis; usually heals with a scar. d) Excoriation - erosions or ulcers caused by scratching, biting or rubbing, usually due to pruritus. e) Scar - an area of fibrous tissue that has replaced the damaged dermis and/or subcutis. f) Fissure - a linear cleavage of usually thickened, inelastic skin. g) Lichenification - a thickening and hardening of the skin with exaggeration of the superficial markings. h) Callus - a thickened, rough, alopecic, lichenified plaque that develops on the skin.
Dermatopathology
3 -----------------------------------------------------------------------------------------------------------------------------------
Winter 2012
DISTRIBUTION OF SKIN LESIONS Regional location and symmetry or asymmetry of skin lesions are important diagnostic aids. AGE, BREED AND SEX PREDISPOSITIONS OF SKIN DISEASES Many dermatologic disorders have predispositions: AGE (eg demodecosis, juvenile cellulitis), BREED (eg primary seborrhea of Cocker spaniels, skin fold pyoderma of Shar peis) SEX (eg estrogen-responsive or testosterone-responsive dermatoses).
VOCABULARY OF DERMATOHISTOPATHOLOGY (for information only) EPIDERMAL CHANGES a) Hyperkeratosis - increased thickness of stratum corneum; ortho- (anuclear) or para-keratotic (nucleated). b) Epidermal hyperplasia (acanthosis) - increased thickness of the noncornified epidermis. c) Epidermal atrophy - decreased thickness of the noncornified epidermis. d) Intracellular edema - cell damage leading to hydropic (vacuolar) or ballooning degeneration. e) Intercellular edema (spongiosis) - accumulation of edema fluid in the intercellular spaces. f) Acantholysis - loss of cohesion between epidermal cells leading to clefts, vesicles / bullae or pustules. g) Exocytosis - migration of inflammatory cells through the intercellular spaces of the epidermis. h) Pustule (microabscess) - microscopic or macroscopic cavities filled with inflammatory cells. i) Crust - surface accumulations of varying combinations of keratin, serum, cell debris, bacteria, etc. j) Necrosis / apoptosis - microscopic forms of keratinocyte death. k) Dyskeratosis - premature or abnormal keratinization in the viable layers of the epidermis. l) Hyper- & hypopigmentation - excessive or decreased amounts of melanin within the epidermis. DERMAL CHANGES a) Dermal edema - see widened spaces between dermal collagen, perivascular edema or lymphatic dilation. b) Collagen changes - including hyalinization, degeneration, mineralization, etc. c) Fibroplasia / fibrosis / sclerosis - formation and maturation of fibrous tissue, leading to scarring. d) Pigmentary incontinence - melanin granules free within the dermis or within dermal macrophages. e) Follicular changes - include atrophy, dilation, keratosis, dysplasia, inflammation, etc. f) Glandular changes - include inflammation, atrophy, hyperplasia, cystic change, etc. g) Vascular changes - include fibrinoid degeneration, vasculitis, thromboembolism, etc. SUBCUTANEOUS FAT (PANNICULUS ADIPOSUS) CHANGES A variety of reactions (inflammation, necrosis, fibrosis, etc) can occur from the direct extension of similar changes in the overlying dermis or can occur in isolation from changes in the overlying skin.
HISTOPATHOLOGIC PATTERN-ANALYSIS Dermatitis is not a particularly useful term from a diagnostic or therapeutic point of view, since the skin becomes inflamed in response to a myriad of causes. A method of pattern-analysis (at low magnification) of skin lesions has proved useful in relating inflammatory patterns to various types of skin diseases. With the addition of details observed at higher magnification, a specific diagnosis can often be made.
Dermatopathology
4 -----------------------------------------------------------------------------------------------------------------------------------
Winter 2012
1) PERIVASCULAR (INTERSTITIAL) DERMATITIS C the predominant inflammatory reaction is centered on the superficial and/or deep dermal vessels. Perivascular (interstitial) dermatitis (ie no significant epidermal changes) C esp. hypersensitivities and urticaria. Spongiotic perivascular (interstitial) dermatitis (ie with epidermal spongiosis) C esp. hypersensitivities, contact dermatitis, ectoparasitism, viral, dermatophytosis, Malasseziasis, etc. Hyperplastic perivascular (interstitial) dermatitis (ie with epidermal hyperplasia and hyperkeratosis) C common chronic dermatitis reaction of many causes which is mostly non-diagnostic. C seen especially in chronic hypersensitivities, altered keratinization, lick dermatitis, etc. 2) INTERFACE DERMATITIS C obscuring of the dermoepidermal junction by hydropic degeneration / apoptosis &/or a lichenoid infiltrate. C seen with a variety of immune-mediated and/or autoimmune skin diseases, drug reactions, viral infections (eg BVD, MCF, Rinderpest). 3) VASCULITIS (neutrophilic, lymphocytic, eosinophilic or mixed) C seen with a variety of infections (eg septicemias, RMSF, Equine viral arteritis), immune-mediated diseases (eg drug reactions) and others. 4) NODULAR AND DIFFUSE DERMATITIS C can be granulomatous, pyogranulomatous, neutrophilic, eosinophilic, or mixed. C especially due to traumatic implantation of foreign material (eg hair, plant material) or a wide variety of bacteria, fungi or protozoa. C for identification of specific agents use polarization, special stains and microbial culture. 5) INTRAEPIDERMAL OR SUBEPIDERMAL VESICULAR AND PUSTULAR DERMATITIS C vesicles are fragile and transient (esp in dogs & cats) C vesicles often evolve rapidly into pustules. C intraepidermal vesicles/pustules can result from: acantholysis (eg. neutrophilic proteolytic enzymes in bacterial infection, pemphigus autoantibodies) coalescing ballooning degeneration in viral dermatitis (eg pox viruses, vesicular viruses) intense intracellular and/or intercellular edema of the epidermis (with any severe dermatitis) C subepidermal vesicles can result from: dermoepidermal separation (eg bullous pemphigoid) severe subepidermal edema and/or cellular infiltration (eg urticaria, cellulitis) 6) PERIFOLLICULITIS / FOLLICULITIS / FURUNCULOSIS C especially due to bacteria (esp. Staphylococcus),fungi (esp. ringworm) or parasites (esp. demodex). C sebaceous adenitis, hidradenitis and bulbitis are other occasional types of adnexal inflammation. 7) PANNICULITIS C is often an extension an overlying nodular or diffuse dermatitis with similar inflammatory cell types. C other specific causes include nutritional steatitis, injection reactions and idiopathic. 8) ATROPHIC DERMATOSIS C usually due to endocrine disorders and less frequently nutritional or developmental dermatoses. C see varying combinations of orthokeratotic hyperkeratosis, epidermal melanosis, sebaceous gland atrophy, and follicular changes indicative of hair cycle arrest and/or atrophy (eg telogen predominance without hair shafts, dilation & keratin plugging of follicles, follicular atrophy).
Dermatopathology
Winter 2012
-----------------------------------------------------------------------------------------------------------------------------------
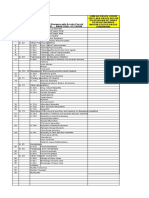
Superficial perivascular dermatitis
Spongiotic perivascular dermatitis
Hyperplastic perivascular dermatitis
Interface dermatitis with hydropic degeneration and lichenoid infiltrate
Vasculitis
Nodular dermatitis
Diffuse dermatitis
Intraepidermal vesicular and pustular dermatitis
Subepidermal vesicular and pustular dermatitis
Perifolliculitis
Folliculitis
Furunculosis
Panniculitis
Atrophic dermatosis
Dermatopathology
Winter 2012
-----------------------------------------------------------------------------------------------------------------------------------
CONGENITAL AND HEREDITARY SKIN DISEASE
C note the difference between the terms congenital (present at birth; can be hereditary or acquired), hereditary (genetic) and acquired (environmental, eg viral, toxic, etc). 1. Congenital Hypotrichosis C reported in all domestic species (variety of heritable syndromes in many breeds). C absence of hair follicles or abnormal follicular development (follicular dysplasia). Cattle: C hereditary - several modes of inheritance in different breeds. C acquired - causes include: intrauterine BVD infection, iodine deficiency and goitre, adenohypophyseal hypoplasia in Guernsey and Jerseys and maternal ingestion of Veratrum album. C R/O telogen or anagen defluxion (effluvium) - mass precipitation of hairs caused by a variety of stresses including febrile illness, parturition, surgical shock, etc Dogs and Cats: - several hereditary forms of hypotrichosis. 2. Some Other Congenital / Hereditary Skin Diseases (for information only) Hereditary Collagen Dysplasia in most species Ichthyosis in many species Pattern Baldness of dogs Pityriasis Rosea [Porcine Juvenile Pustular and Psoriasiform Dermatitis] Dermatomyositis of Collies and Shelties (complex pathogenesis; interface dermatitis clefting)
ENVIRONMENTAL INDUCED SKIN DISEASE
I. ACTINIC (SUN) INJURY Epidemiology C the amount of light reaching skin is determined by: Environmental Factors < atmosphere / latitude / altitude / shelter Host Factors < quantity of hair / pigmentation / stratum corneum / genetics Etiopathogenesis C visible light range is ~ 400-700 nm; longwave UV is ~ 320-400 nm (UV-A); damaging portion is by middlewave UV ~ 290-320 nm (UV-B) which represents ~ 1% of the light reaching the skin. C ozone strongly absorbs shortwave UV < 290 nm (UV-C) which is very damaging. C UV-B light energy is absorbed by some molecules in the skin ! electron transfer with the generation of free radicals ! damage to nucleic acids, proteins & lipid membranes ! cell injury / death. C also causes mutagenesis (tumorigenesis) pyrimidine dimer formation has been shown to occur in mutation hot spots on P53 gene (tumor suppressor gene) in basal epidermal cells. cells with mutated P53 have an impaired ability to: i) delay replication until any DNA damage is repaired, and ii) undergo apoptosis when DNA is damaged beyond repair. UV can also be a tumor promoter, in that health cells which are damaged by UV light and undergo apoptosis, can be preferentially replaced by cells with mutated P53 (which are resilient to UV induced apoptosis).
Dermatopathology
Winter 2012
----------------------------------------------------------------------------------------------------------------------------------1. Primary Phototoxicity ("sunburn" or "solar dermatitis") C due to: direct endothelial damage damage to keratinocytes with release of inflammatory mediators. C typically see initial redness (sunburn erythema), followed by pain, edema, blistering, etc
2. Photosensitization C when photodynamic substances in skin are activated by UV-A (normally not harmful) or visible light. C the absorbed energy creates oxygen free radicals which damage the skin. Type I - exogenous origin of photodynamic agents, esp. certain plant toxins and drugs Type II - aberrant endogenous pigment synthesis, ie porphyrias Type III - (hepatogenous type) failure to remove phylloerythrin (from chlorophyll) which is photoreactive Type IV - unknown etiology / pathogenesis
II. CHEMICAL INJURY Local application - agent must penetrate hair & stratum corneum; enhanced by moisture &/or skin damage. Systemic absorption - ingestion of toxins with systemic effects on the skin and usually other organs. 1. Primary Contact Irritant Dermatitis C skin contact by substances expected to cause irritation, ie caustic chemicals (eg acids, alkalies), concentrated drugs (eg insecticides), soaps/detergents, body excretions (eg anal sac, urine), etc. 2. Some Other Chemically Induced Skin Diseases (for information only) Gangrenous Ergotism and Fescue Toxicosis Inorganic poisons, eg thallium, selenium, mercury, arsenic, etc
III. PHYSICAL INJURY 1. Acral Lick Dermatitis C focal self-trauma, typically found on the dorsal surface of the distal region of a limb. Epidemiology C dogs, esp. large breeds. Etiopathogenesis C psychogenic (emotional/psychologic) C usually results from: boredom - alone during day. anxiety - new home, pet, baby, etc. / loss of companion, etc. / any other stress. 2. Some Other Physically Induced Skin Diseases (for information only) Abrasion, Laceration, Ulceration and Foreign Bodies Extremes in Temperature - cold vs thermal injury (eg flame, scald, electrical, lightning, etc) Callus / Hygroma Feline psychogenic dermatitis (one cause of feline symmetric alopecia) Radiation
Dermatopathology
Winter 2012
-----------------------------------------------------------------------------------------------------------------------------------
INFECTIOUS SKIN DISEASE
I. VIRAL SKIN DISEASES Local Infection C intact skin is resistant to viral penetration; local infection (eg pox or papilloma viruses) requires abrasion or arthropod bite. Systemic Infection (with skin involvement) C epitheliotropic: eg MCF, vesicular viruses. C pantropic: eg distemper, hog cholera. C other: eg pruritus caused by pseudorabies or scrapie. Diagnosis C history & clinical signs / lesions. C skin biopsy - mostly vesicular to pustular dermatitis, viral inclusion bodies. C serology. C virus isolation or identification (eg PCR, EM) A SMALL SELECTION OF VIRAL DERMATITIDES CANINE Papilloma virus - (see Neoplasia) Canine distemper virus - dogs (also wolf/coyote, ferret/mink, raccoon, others) CATTLE Bovine mammallitis virus (bovine herpes 2) Pseudocowpox (Parapoxvirus) - cosmopolitan, common Papilloma virus - (see Neoplasia) SHEEP and GOATS Contagious viral pustular dermatitis [= Contagious ecthyma = "Orf"] (Parapoxvirus) Epidemiology C common viral infection in young sheep & goats; world wide distribution. C occasionally affects humans, cattle, dogs, others. Etiopathogenesis C starts at commissures of mouth (initiated by abrasions from pasture or forage) and spreads to lips and oral cavity; eyelids, feet, viscera. C typical pox phases (ie hydropic / ballooning degeneration of keratinocytes with cytoplasmic inclusion bodies ! vesiculation ! intraepidermal pustules ! crust); but Orf is much more proliferative (hyperplastic) than most other poxvirus infections. SWINE Swinepox (Suispox): common, cosmopolitan, usually mild HORSES Papilloma virus (see Neoplasia)
Dermatopathology
Winter 2012
----------------------------------------------------------------------------------------------------------------------------------II. BACTERIAL SKIN DISEASES (PYODERMA) Etiopathogenesis C healthy skin is resistant to infection by pathogenic bacteria because of: lack of moisture. continuous desquamation of stratum corneum. ecologic pressure of normal flora (antibiotics, lipases). C factors assisting bacterial colonization / proliferation include: moisture and dirt lead to dilution of lipid barrier and abrasion of cornified layer. altered cornification (eg seborrhea, endocrine skin diseases) physical damage (friction, parasites, self-trauma, etc.). C once infection is established the result then depends on pathogenicity of the agent and the defense mechanisms of the host.
PRIMARY PYODERMA SKIN BACTERIA PATTERN ANTIBIOTICS otherwise healthy (esp young) one species characteristic successful
SECONDARY PYODERMA not healthy (eg parasites, etc) > one species not characteristic not successful
SUPERFICIAL PYODERMA INVOLVES REPAIR DURATION LYMPH NODE SYSTEMIC GROSS HISTOLOGY epidermis no scarring short no no pustules (epidermal collarettes), crusts pustules to perivascular / interstitial dermatitis with neutrophils
DEEP PYODERMA follicles / dermis / subcutis scarring chronic yes pustule, nodule, abscess, sinus folliculitis / furunculosis &/or nodular to diffuse dermatitis / panniculitis, suppurative to granulomatous, bacterial agent
Diagnosis C history & clinical signs / lesions. C bacterial culture C skin biopsy
Dermatopathology
Winter 2012
----------------------------------------------------------------------------------------------------------------------------------A SMALL SELECTION OF BACTERIAL DERMATITIDES CANINE Pyotraumatic dermatitis (hot spots or acute moist dermatitis) C intense pruritus (esp. fleas) ! self-trauma ! secondary bacterial infection. Puppy pyoderma (Impetigo) C pustular dermatitis primarily due to Staphylococcus, occasionally Streptococcus. Skin fold pyoderma (Intertrigo) C eg's include facial, lip, vulvar, tail-fold and body-fold dermatitis. FELINE Subcutaneous Abscesses C esp. bite wounds in cats (P. multocida, Streptococcus, Bacteroides spp, etc). RUMINANTS Papillomatous Digital Dermatitis (hairy heel warts) C erosive to papillomatous, intensely painful lesions in skin bordering the interdigital space. C large numbers of spirochetes (apparent new species of Treponema) are present within the lesions. Dermatophilosis (D. congolensis) in many species C esp. ruminants and horses; also reported in dogs and cats. HORSES Staphylococcal Folliculitis / Furunculosis C esp in saddle & tack areas; esp in summer. C also one cause of pastern dermatitis (a dermatitis typically affecting the caudal aspect of the pasterns). PORCINE Exudative Epidermitis (Greasy Pig Disease) Epidemiology C suckling to early weaners; acute, rapidly spreading, often fatal. Etiopathogenesis C infection with Staphylococcus hyicus C predisposing factors include: immature protective mechanisms skin abrasion poor nutrition, concurrent infections
10
Septicemia Salmonella - lesions are the result of endotoxemia (ie venous thrombosis / infarction of extremities). "Diamond Skin Disease" (usually Swine Erysipelas, rarely Actinobacillus suis) - lesions are the result of localized vasculitis and thrombosis.
Dermatopathology
Winter 2012
-----------------------------------------------------------------------------------------------------------------------------------
11
III. MYCOTIC SKIN DISEASES Diagnosis C history & clinical signs / lesions. C fungal identification (UV light, direct exam, smears) and/or culture. C skin biopsy. 1. Cutaneous (Superficial) Mycoses - restricted to keratinized tissues, ie hair, stratum corneum, nails. Dermatophytosis (Ringworm) Epidemiology C common in all domestics ( esp. cats and cattle); zoonotic. C worldwide distribution esp. hot, humid environments. Etiopathogenesis C due infection with keratinophilic fungi, primarily in the genera of Microsporum or Trichophyton. C young animals are more susceptible and severe disease occurs in immunocompromised animals. C predisposing factors: overcrowding, high humidity, poor sanitation and nutrition. C contagious; transmission direct or by fomites (esp. stabled animals). C attacks keratinized layers with enzymes (keratinase, collagenase, and elastase). C the inflammatory reaction is to these proteases as they diffuse into the dermis. Dermatomycosis C a fungal infection of the cornified layer of skin, hair or claws caused by a nondermatophyte. C Malasseziasis (Malassezia pachydermatis) and Candidiasis (Candida spp). 2. Subcutaneous Mycoses C traumatic implantation of a wide variety of saprophytic fungi. C some lesions caused by specific agents and others caused by a group of related agents; egs Eumycotic mycetoma (non-pigmented or pigmented fungi), Phaeohyphomycosis (pigmented fungi), Pythiosis (Florida horse leeches), Zygomycosis (Mucormycosis and others), Sporotrichosis, etc. 3. Systemic Mycoses C primarily by inhalation of saprophytes, skin involvement, eg Blastomycosis, Cryptococcosis, etc C usually due to compromised resistance to infection.
IV. ALGAL SKIN DISEASE Protothecosis - due to saprophytic achloric algae of the genus Prototheca.
Dermatopathology
Winter 2012
----------------------------------------------------------------------------------------------------------------------------------V. PARASITIC SKIN DISEASES C ectoparasitism (live on body surface) vs. endoparasitism (live within the body). C note, infestation (cutaneous habitation by ectoparasites) vs infection (invasion and multiplication of microorganisms in tissues, causing cell damage and inflammation). C parasites cause disease directly by: inflammation (pruritus / self-trauma, hypersensitivity reaction) blood sucking toxin injection (eg. tick paralysis) < results in: annoyance, reduced production and unthrifty / blemished hides. C parasites cause disease indirectly by: being important vectors of infectious agents causing systemic diseases; eg WNV, RMSF, Lyme borreliosis, Leishmaniasis, dirofilariasis. predisposing to pyoderma, myiasis or local viral infections. Diagnosis C history & clinical signs (esp. pruritus) / lesions C parasite identification (eg. scrapings) C skin biopsy 1. MITES Demodectic Mange Epidemiology C mainly dogs (breed/familial predispositions), occasionally other species. Etiopathogenesis C Demodex spp. are part of the normal microfauna. C see disease in dogs with genetic predisposition and selective or partial states of immunodeficiency. Localized form < young dogs, 3-10 months, usually self-limiting. Generalized form < in young dogs following localized form. C when seen in older dogs, usually have serious internal disease and/or immunosuppression. C on histology see massive proliferation of mites, folliculitis / furunculosis, secondary pyoderma. Sarcoptic Mange (Scabies) Epidemiology C most frequent in pigs > dogs > ruminants, horses; little breed or age predisposition. Etiopathogenesis C highly contagious, host varieties (eg. S. scabiei var. suis). C people readily parasitized by animal adapted species (but don't usually complete life cycle). C male and females mites mate near surface then females burrow deeper and lay eggs. C lesions due to: mechanical damage from burrowing in epidermis. irritation from mite saliva and excreta. severe self-trauma due to hypersensitivity to mite products. Notoedric Mange (Notoedres cati) - primarily cats ("Feline Scabies") and rabbits. Otodectic Mange (Otodectes cyanotis) - ear mite of carnivores. Psoroptic Mange (Psoroptes sp) - many species, esp. ears of goats and rabbits. Chorioptic Mange (Chorioptes spp) - ruminants and horses. Cheyletiellosis (Cheyletiella spp) - primarily cats, dogs, and rabbits. Psorergatic Mange (Psorergates ovis) - of sheep. Trombiculidiasis - "chiggers"- larvae of trombiculid mites. Many others
12
Dermatopathology
Winter 2012
----------------------------------------------------------------------------------------------------------------------------------2. TICKS Hard (Ixodid) ticks C Ixodes spp. (vector of Lyme disease), Rhipicephalus spp, Dermacentor spp Soft (Argasid) ticks 3. FLEAS C the single most important cause of skin disease in small animals. C in dogs and cats Ctenocephalides felis most common, also C. canis. C manifestations of flea infestation include: asymptomatic carriers flea-bite dermatitis (papular / crusting dermatitis, pruritus / self-trauma) flea allergy dermatitis (see Immune-mediated skin disease) 4. LICE (PEDICULOSIS) Sucking lice (eg Linognathus spp., Hematopinus spp.) feed on blood and tissue fluids. Biting lice (eg Damalini spp., Trichodectes spp.) feed on exfoliated epithelium and debris. 5. FLIES Fly bite dermatitis - due to biting flies. Vectors of infectious disease - by biting and non-biting flies. Myiasis - invasion of animal tissues by fly larvae (maggots); eg's Warbles (Hypoderma) - primarily cattle; occasionally horses Cuterebriasis - esp. cats, dogs and small wild mammals. Screwworm myiasis 6. HELMINTH DISEASE Cutaneous larval migration C adults live in non-cutaneous sites while larval stages migrate through skin. Cutaneous Habronemiasis - Habronemia & Draschia spp. in horses - in "normal" life cycle, larvae deposited near mouth and are swallowed and complete life cycle in the stomach wall. - when larvae deposited on moist skin (esp. eyelid or prepuce) by house or stable fly; results in ulcerative dermatitis (r/o squamous cell carcinoma, ulcerated sarcoid, others). Others: Hookworm dermatitis in dogs and ruminants, Pelodera dermatitis in dogs, ruminants, horses, Strongyloidiasis ruminants and horses, Parelaphostrongylosis of goats, etc Filarial Dermatitis C adults or microfilaria spend some time in the skin. C egs: Onchocerciasis - esp. O. cervicalis in horses, Stephanofilariasis of ruminants, Dirofilarial (heartworm) dermatitis in dogs, etc. 7. PROTOZOAL DISEASES C Sarcocystosis in cattle C Leishmaniasis in humans, dogs, rodents and others C Besnoitiosis in wild ungulates, cattle and horses
13
Dermatopathology
Winter 2012
-----------------------------------------------------------------------------------------------------------------------------------
14
IMMUNE-MEDIATED SKIN DISEASE
I. HYPERSENSITIVITY REACTIONS Definition C a reaction that develops in response to normally harmless foreign compounds. C recall hypersensitivity (HS) reactions types I, II, III & IV. C most cutaneous HS's are mediated by types I and/or IV HS reactions. C pruritus is a feature common to most HS's. Diagnosis C history and clinical signs (esp. pruritus) / lesions. C skin biopsy (often non-specific; compatible with many HS's and/or other etiologies). C intradermal skin testing, elimination of offending antigens and/or clinical response to therapy. 1. ATOPIC DERMATITIS Epidemiology C atopy is common and familial in dogs, with many breeds predisposed; also in cats and horses. Etiopathogenesis C associated with a variety of predominately percutaneously absorbed allergens (eg house dust mites). C complex type I HS (also abnormal cell-mediated immune function) to normally innocuous antigens. C possible dysfunction of T cells leading to overproduction of specific IgE. C results in mast cell degranulation (eg histamine, leukotrienes) 6 pruritus 6 self-trauma. Gross C primary lesions not seen; secondary lesions are due to self-trauma: erythema, excoriation and alopecia; with time develop hyperpigmentation and lichenification. C starts on face, feet, ventral abdomen, perineum; with chronicity can become generalized. Histology C early: superficial perivascular dermatitis, often just edema. (non-specific!) C later: hyperplastic perivascular / interstitial dermatitis, 2o pyoderma / Malasseziasis (non-specific!) Differential Diagnosis C especially other allergies (flea, food, etc.) and ectoparasitism (scabies, fleas, etc.). 2. FLEA ALLERGY DERMATITIS Epidemiology C most common hypersensitivity of cats and dogs; often seasonal (summer / fall) in cold winter areas. Etiopathogenesis C mediated by combination of types I & IV HS reactions to antigens in flea saliva. C once sensitized, few fleas are needed to initiate severe reaction. C intense pruritus 6 self-trauma / secondary infections. Gross C primary lesion is an erythematous papule or wheal, however self-trauma quickly leads to alopecia and crusts; with chronicity see hyperpigmentation and lichenification. C in dogs, lesions usually on lumbosacral regions, caudomedial thighs and caudoventral abdomen; can become generalized in severely affected individuals. C in cats, lesions usually occur on head and neck (main cause of "Miliary Dermatitis" of cats). Histology C perivascular / interstitial dermatitis with predominance of eosinophils & mast cells early and mononuclear inflammatory cells later. C may see spongiotic perivascular dermatitis with eosinophils; +/- eosinophilic microabscesses (flea nibbles)
Dermatopathology
Winter 2012
----------------------------------------------------------------------------------------------------------------------------------3. SOME OTHER HYPERSENSITIVITY REACTIONS (for information only) Urticaria (hives or wheals) / Angioedema (edematous swellings) Allergic Contact Dermatitis [Contact HS] Food Hypersensitivity (Allergy) Equine Insect (Culicoides) Hypersensitivity Etc
15
II. AUTOIMMUNE REACTIONS C diseases that develop when autoantibodies or T cells react against self rather than foreign antigens. Epidemiology C autoimmune diseases are rare in domestic animals. C have a hereditary predisposition. C dogs > horses, cats > others. Etiopathogenesis Pemphigus C autoantibodies bind to keratinocyte desmosomal Ag's (eg desmoglein 1 or 3) loss of cohesion & inflammatory mediators acantholysis & neutrophilic infiltration intraepidermal pustules. Bullous pemphigoid C autoantibodies against specific Ags in the basal lamina activation of complement & inflammatory mediators subepidermal vesicles / pustules. Discoid (cutaneous) lupus erythematosus C postulated that UV light alters keratinocyte Ags autoimmune response interface dermatitis. Diagnosis C history and clinical signs / lesions. C skin biopsy; esp. vesicular / pustular and interface dermatitis. C immunohistochemistry.
III. SOME OTHER IMMUNE-MEDIATED DISORDERS (for information only) Immune-mediated Vasculitis (type 3 HS reaction following infections, drugs) Erythema Multiforme (most commonly associated with drugs and infections) Toxic Epidermal Necrolysis (most commonly associated with drugs and infections) Vogt-Koyanagi-Harada-like syndrome [cutaneous depigmentation and uveitis in dogs] Plasma Cell Pododermatitis of cats Cutaneous Amyloidosis Etc
Dermatopathology
Winter 2012
-----------------------------------------------------------------------------------------------------------------------------------
16
ENDOCRINE SKIN DISEASE
C hormones act on skin & other organs by modifying existing physiological processes. Gross Bilateral symmetrical alopecia (nonpruritic) Hyperpigmentation Secondary seborrhea and/or pyoderma Histology (atrophic dermatosis pattern) Hyperkeratosis Epidermal melanosis Follicular changes - keratosis, atrophy, catagen or telogen (hairless) predominance Sebaceous gland atrophy Diagnosis History and clinical signs / lesions. Skin biopsies - usually atrophic dermatosis, lesions specific to a particular endocrine dermatosis. Demonstration of hormone deficiency or excess and/or response to specific therapy.
1. HYPOTHYROIDISM C the most common endocrinopathy causing skin disease of dogs ( classical clinical signs). C [T3 / T4] affects basal metabolic rate ie protein synthesis and mitotic activity. Gross C typical endocrine changes; thickened skin due to cutaneous mucinosis (tragic expression!). Histology C typical atrophic dermatosis pattern. C often hyperplasia of epidermis and infundibular (superficial) region of follicle, increased dermal mucin. 2. HYPERADRENOCORTICISM C second most common endocrinopathy of dogs. C increase in endogenous or exogenous (iatrogenic) glucocorticoids. Gross C typical endocrine changes. C skin often thin with decreased elasticity and poor wound healing. C calcinosis cutis (dystrophic mineralization of dermal collagen), comedones. Histology C typical atrophic dermatosis pattern. C often epidermal / dermal atrophy, marked follicular keratosis (comedones), dystrophic mineralization. 3. SOME OTHER ENDOCRINE SKIN DISEASE (for information only) Gonadal Hormone Imbalances - eg female hyperestrogenism, sertoli cell tumor-associated skin disease. Alopecia X (growth hormone / castration-responsive dermatosis) Equine pars intermedia pituitary adenoma Etc.
Dermatopathology
Winter 2012
-----------------------------------------------------------------------------------------------------------------------------------
17
NUTRITIONAL SKIN DISEASE (for information only)
1. Zinc deficiency / Zinc-responsive dermatosis C in swine, dogs, ruminants; see marked parakeratotic hyperkeratosis. 2. Copper deficiency (molybdenum toxicity) C primarily ruminants; depigmentation (many other systems can be affected). 3. Nutritional panniculitis / steatitis C in cats, mink, foals and pigs; associated with high dietary levels of unsaturated fatty acid and/or vitamin E / selenium deficiency 4. Vitamin E / Selenium Responsive Dermatosis C in goats; scaling and alopecia of the coat along the back (marked hyperkeratosis).
MISCELLANEOUS SKIN DISEASES
1. Disorders of Cornification C cornification includes all the processes that form the stratum corneum (eg keratinization, formation of lipid rich intercellular domain, etc) Seborrhea C broad classification for many clinical syndromes with scaling, crusting, +/- greasiness (1o vs 2o). C basic feature is defect in cornification ( abnormal sebum production). C involves 3 main abnormalities: altered keratinization scaling & crusting. altered surface lipids increased free fatty acids and decreased diester waxes. altered bacterial & yeast flora also increased numbers / unit area. Primary Seborrhea C primarily seen in dogs; heritable, breed specific disorders of cornification. C clinical subtypes (which may be intermixed): seborrhea sicca (dry) - esp. German Shepherds, dachshunds, Doberman's seborrhea oleosa (waxy/oily) - esp. Cocker Spaniels, Springer Spaniels and Chinese Shar Pei seborrheic dermatitis - likely due to secondary pyoderma &/or Malassezia infections. Secondary Seborrhea C occurs with a multitude of unrelated disease processes; eg endocrine, dermatophytosis, ectoparasites, etc. 2. SOME OTHER MISCELLANEOUS SKIN DISEASES (for information only) C there are a large number of species and/or breed specific dermatoses of usually poorly defined etiology, eg Eosinophilic Dermatitides Feline Eosinophilic Granuloma Complex Feline Eosinophilic Ulcer (feline indolent rodent, feline rodent ulcer) Feline Eosinophilic Plaque Feline Eosinophilic Granuloma (feline linear granuloma, feline collagenolytic granuloma) Equine Nodular Collagenolytic Granuloma (eosinophilic granuloma with collagen degeneration)
Dermatopathology
Winter 2012
-----------------------------------------------------------------------------------------------------------------------------------
18
NEOPLASTIC SKIN DISEASES
C the skin is the most common site of neoplasia in most domestic species. Etiopathogenesis (see general pathology) C damage to the genome by radiation, viruses, chemicals, etc. C influenced by genetics, hormones, etc. Diagnosis C distinct gross morphology and location often relate to identification and prognosis. C definitive diagnosis by cytology / histology of biopsies ie. fine needle, punch, excisional, etc. C specific categorization occasionally requires cell markers (immunohistochemistry) or electron microscopy. Classification C Ectodermal: tumors of the epidermis and adnexa. C Melanocytic: tumors of melanocytic origin. C Mesodermal: tumors of mesenchymal or round cell origin.
ECTODERMAL NEOPLASMS 1. Epidermal Origin Squamous Cell Carcinoma (SCC) C relatively common neoplasm; on poorly pigmented areas of cats, Hereford cattle, horses. C sunlight (UV-light) exposure is probably the most important carcinogenic stimulus for these tumors. Gross C firm, poorly demarcated mass, ulceration or proliferative/papillary. C often located on head (eye / ear); especially unpigmented areas. Biologic Behaviour C locally invasive with tissue destruction. C low metastatic potential of most skin SCC (possible exception is canine nailbed SCC). Papilloma - most domestic species, mostly viral, species specific papilloma viruses (occ. non-viral). Basal cell tumors 2. Adnexal Origin Hair follicle tumors - eg trichoepithelioma, pilomatrixoma, etc. Sebaceous gland tumors - nodular hyperplasia to adenomas to carcinomas. Perianal gland tumors - nodular hyperplasia to adenomas to carcinomas. Sweat gland (apocrine and eccrine) tumours - nodular hyperplasia to adenomas to carcinomas.
Dermatopathology
Winter 2012
----------------------------------------------------------------------------------------------------------------------------------MELANOCYTIC NEOPLASMS 1. Melanoma (Melanocytoma) C common in dogs, gray horses, some swine. C melanocytoma refers to the beign form; melanoma or malignant melanoma refers to malignancy. Gross C dark brown-black, macules, papules, nodules tumors; usually single in the dog, multiple in horse. Biologic Behaviour Dogs < eyelid or skin, if < 2 cm mostly benign. < digits or skin, if > 2 cm (or any size in oral cavity) mostly malignant. < also use general histologic criteria of malignancy. Gray-White Horses < common at 6 yrs., 80% in aged population (> 15 yrs). < especially on perineum (in some cases tumors can enlarge to several kilos) . < occasionally see local invasion and metastasis to viscera.
19
MESODERMAL NEOPLASMS 1. Mesenchymal Neoplasms Cutaneous soft-tissue sarcomas (spindle cell tumor/sarcoma) C grouping of some spindle cell tumor types esp schwannomas, hemangiopericytomas, etc. (ie many forms histologically interchangeable, require immunohistochemistry or EM to accurately classify). C common in dogs; less in cats and horses. Gross C firm to gelatinous, gray-white nodular mass; single or multinodular, any site especially limbs. Biologic Behaviour C most are locally invasive with frequent local recurrence after removal (usually due to incomplete excision). C metastatic potential correlates to degree of histologic anaplasia (low grade vs high grade). Vaccine-site sarcomas of cats - highly invasive mesenchymal tumor occurring at sites of vaccination. Equine and feline sarcoids - fibropapillomas resulting from infection with bovine papillomavirus. Fat cell neoplasms - lipoma / liposarcoma. Fibroblastic tumors - fibroma / fibrosarcoma. Myxomatous tumors - myxoma / myxosarcoma. Tumors of blood vessel origin - hemangioma (-sarcoma), lymphangioma (-sarcoma). Tumors of neural origin - eg benign peripheral nerve sheath tumor (schwannoma). Smooth muscle tumors - leiomyoma / leiomyosarcoma.
Dermatopathology
Winter 2012
-----------------------------------------------------------------------------------------------------------------------------------
20
2. Round Cell Neoplasms Mast Cell Tumors C common in dogs (mean age 8 yrs.) and to a lesser extent in cats. Gross C single or multiple, edematous nodular masses. C often hairless and ulcerated in late stages. Biologic Behaviour C most frequent potentially malignant skin tumor of the dog. C in dogs, behaviour correlates with histologic criteria of malignancy (histologic grading system) Histiocytic Neoplasms -some examples: Canine cutaneous histiocytoma - common benign tumor (Langerhans cells) of usually young dogs. Cutaneous & systemic reactive histiocytosis - dysregulated proliferation of dermal dendritic cells. Histocytic sarcoma (malignant histiocytosis) - neoplastic proliferation of dermal dendritic cells. Lymphocytic Neoplasms Epitheliotropic lymphoma - eg mycosis fungoides and others. Nonepitheliotropic lymphoma - dermal location. Cutaneous plasmacytoma - extramedullary, ie only rarely associated with multiple myeloma. Cutaneous lymphocytosis (pseudolymphoma) - focal dermal lymphoid hyperplasia in response to Ag. Others: transmissible venereal tumor, cutaneous neuroendocrine (Merkel cell) tumor, etc.
Você também pode gostar
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeNo EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeNota: 4 de 5 estrelas4/5 (5795)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreNo EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreNota: 4 de 5 estrelas4/5 (1090)
- Never Split the Difference: Negotiating As If Your Life Depended On ItNo EverandNever Split the Difference: Negotiating As If Your Life Depended On ItNota: 4.5 de 5 estrelas4.5/5 (838)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceNo EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceNota: 4 de 5 estrelas4/5 (895)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersNo EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersNota: 4.5 de 5 estrelas4.5/5 (345)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureNo EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureNota: 4.5 de 5 estrelas4.5/5 (474)
- The Emperor of All Maladies: A Biography of CancerNo EverandThe Emperor of All Maladies: A Biography of CancerNota: 4.5 de 5 estrelas4.5/5 (271)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)No EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Nota: 4.5 de 5 estrelas4.5/5 (121)
- The Little Book of Hygge: Danish Secrets to Happy LivingNo EverandThe Little Book of Hygge: Danish Secrets to Happy LivingNota: 3.5 de 5 estrelas3.5/5 (400)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyNo EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyNota: 3.5 de 5 estrelas3.5/5 (2259)
- The Yellow House: A Memoir (2019 National Book Award Winner)No EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Nota: 4 de 5 estrelas4/5 (98)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaNo EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaNota: 4.5 de 5 estrelas4.5/5 (266)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryNo EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryNota: 3.5 de 5 estrelas3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnNo EverandTeam of Rivals: The Political Genius of Abraham LincolnNota: 4.5 de 5 estrelas4.5/5 (234)
- Gordon's 11 Functional Health Patterns AssessmentDocumento2 páginasGordon's 11 Functional Health Patterns Assessmentmtuckrn84% (37)
- The Unwinding: An Inner History of the New AmericaNo EverandThe Unwinding: An Inner History of the New AmericaNota: 4 de 5 estrelas4/5 (45)
- Antibiotic Decision Making in IcuDocumento11 páginasAntibiotic Decision Making in IcumalvindersahiAinda não há avaliações
- 1 Labor and Delivery ProcessDocumento13 páginas1 Labor and Delivery ProcessBardiaga JmayAinda não há avaliações
- First AID For The USMLE Public HealthDocumento20 páginasFirst AID For The USMLE Public HealthLilit M-yanAinda não há avaliações
- Nodular Goiter Concept MapDocumento5 páginasNodular Goiter Concept MapAllene PaderangaAinda não há avaliações
- Universal PrecutionsDocumento30 páginasUniversal PrecutionsShirmi BamunusingheAinda não há avaliações
- Toxicity of ToadsDocumento29 páginasToxicity of ToadsAdarshBijapurAinda não há avaliações
- Icd-10 Oktober 2021Documento9 páginasIcd-10 Oktober 2021Nia KurniawatiAinda não há avaliações
- Diabetes and The Nutrition and Diets For Its PreveDocumento16 páginasDiabetes and The Nutrition and Diets For Its PreveRam MAinda não há avaliações
- Test Bank For Clinical Immunology and Serology A Laboratory Perspective 3rd Edition StevensDocumento11 páginasTest Bank For Clinical Immunology and Serology A Laboratory Perspective 3rd Edition StevensWilbur Penny100% (35)
- Lesson 4-Uniform Hospital Discharge Data SetDocumento14 páginasLesson 4-Uniform Hospital Discharge Data SetSwamyAinda não há avaliações
- Henoch Schonlein Purpura GuidelineDocumento12 páginasHenoch Schonlein Purpura GuidelinewenyinriantoAinda não há avaliações
- DERMA SPMC LeprosyDocumento9 páginasDERMA SPMC LeprosyNicole Alexandra KhoAinda não há avaliações
- AsepsisDocumento20 páginasAsepsisErSandeepVermaAinda não há avaliações
- Introduction To Stem CellsDocumento32 páginasIntroduction To Stem CellsAtif Amin Baig100% (2)
- What Is A PsychiatristDocumento2 páginasWhat Is A Psychiatristmercy robinsonAinda não há avaliações
- Evaluation and Management of Pediatric Community-Acquired PneumoniaDocumento46 páginasEvaluation and Management of Pediatric Community-Acquired PneumoniaJan Marvin Lichauco MendozaAinda não há avaliações
- Lassa Fever: What You Need To Know AboutDocumento2 páginasLassa Fever: What You Need To Know AboutMoses AyoadeAinda não há avaliações
- Module 5 - Formative Assessment 10 - NCM 112 CARE OF CLIENTS WITH PROBLEMS IN OXYGFENATION FLUDocumento9 páginasModule 5 - Formative Assessment 10 - NCM 112 CARE OF CLIENTS WITH PROBLEMS IN OXYGFENATION FLUDharylle CariñoAinda não há avaliações
- Double Stimulations During The Follicular and Luteal Phases of Poor Responders in IVF/ICSI Programmes (Shanghai Protocol)Documento8 páginasDouble Stimulations During The Follicular and Luteal Phases of Poor Responders in IVF/ICSI Programmes (Shanghai Protocol)Nirmal KumawatAinda não há avaliações
- Dementia and Effort Test PerformanceDocumento21 páginasDementia and Effort Test PerformanceIcaroAinda não há avaliações
- Introduction To The Immune System: Department of Biotechnology Ramaiah University of Applied Sciences BangaloreDocumento86 páginasIntroduction To The Immune System: Department of Biotechnology Ramaiah University of Applied Sciences Bangaloreprathyoosha baskaran100% (1)
- 0 - Hospital Design 2020 PDFDocumento3 páginas0 - Hospital Design 2020 PDFPriya DharshiniAinda não há avaliações
- Pediatric Nursing GastroDocumento3 páginasPediatric Nursing GastronieacatleyaAinda não há avaliações
- Pharmacokinetics & Pharmacodynamics PDFDocumento31 páginasPharmacokinetics & Pharmacodynamics PDFhuong LAinda não há avaliações
- Negative Inspiratory Pressure As A Predictor of Weaning Mechanical VentilationDocumento3 páginasNegative Inspiratory Pressure As A Predictor of Weaning Mechanical VentilationamonlisaAinda não há avaliações
- Table 1 Classification and Staging Systems For AKIDocumento1 páginaTable 1 Classification and Staging Systems For AKIAnityo NugrohoAinda não há avaliações
- HSV1 HSV2 R-Gene & VZV R-GeneDocumento2 páginasHSV1 HSV2 R-Gene & VZV R-GeneSachinAinda não há avaliações
- NCPDocumento7 páginasNCPJo Chiko FlorendoAinda não há avaliações
- Clinical Genetics: General Aspects and Laboratory DiagnosticsDocumento14 páginasClinical Genetics: General Aspects and Laboratory DiagnosticsKinga-Borbála GagyiAinda não há avaliações