Escolar Documentos
Profissional Documentos
Cultura Documentos
923
Enviado por
Main AnDescrição original:
Direitos autorais
Formatos disponíveis
Compartilhar este documento
Compartilhar ou incorporar documento
Você considera este documento útil?
Este conteúdo é inapropriado?
Denunciar este documentoDireitos autorais:
Formatos disponíveis
923
Enviado por
Main AnDireitos autorais:
Formatos disponíveis
Poster # 923
Tuberculosis (TB) in a cohort of Latin American infants and children Data from the NISDI Pediatric Protocol
J A Menezes1, L Freimanis-Hance2, Suzanne Essama-Bibi2, T Abreu3, F Ferreira4, N Pavia Ruz5, B Grinsztejn6, L Serchuck7, R Hazra7, and C Worrell7 for the NISDI Pediatric Study Group 2008 Hospital dos Servidores do Estado, Rio de Janeiro, Brazil1, Westat, Rockville, MD2, Instituto de Puericultura e Pediatria Martagao Gesteira, Rio de Janeiro, Brazil3, Universidade Federal de Minas Gerais, Belo Horizonte, Brazil4, Hospital Infantil de Mexico Federico Gomez, Mexico City, Mexico5, Hospital Geral Nova de Iguacu Setor de DST/AIDS, Rio de Janeiro, Brazil6, and Eunice Kennedy Shriver National Institute of Child Health and Human Development7
ABSTRACT
Background: Tuberculosis (TB) is a major opportunistic infection of HIVinfected persons in Latin America. Accurate measures of the burden of childhood TB are lacking partly because diagnosis of TB in children is difficult. Studies of TB in HIV infected children are clearly needed. Methods: A retrospective study of TB diagnoses was done within the NICHD International Site Development Initiative (NISDI) pediatric protocol, which is a prospective cohort study enrolling HIV-infected (HIV+) and HIV-exposed uninfected (HIV-) children at multiple clinical sites in Latin America. This paper describes the occurrence and clinical manifestations of TB in the cohort of HIV+ children, and the diagnostic methods used. Results: From 2002-2006, 1404 infants, children and adolescents (742 HIV+, 620 HIV-, 42 indeterminate) were enrolled at 15 sites (11 in Brazil, 2 in Mexico, 2 in Argentina). While only 1 case of TB was identified in the HIVgroup, 58 of the HIV+ children had had at least one episode of TB; the majority (53/58) were diagnosed before enrollment. Most of the children were either diagnosed with HIV prior to TB (median 11.4 months) or diagnosed with both conditions within a month of each other (50% and 28% respectively). The diagnosis of TB preceded that of HIV for 22% of children (median 9.4 months; range 4.5-33 months). At diagnosis 15 cases were <1 year old, 24 were 1-4 years, 16 were 5-14 years and 3 were >14 years. The most common clinical presentation was miliary disease (48%). Pulmonary and extra-pulmonary disease were seen in 36% and 16% respectively. The most commonly reported symptoms were fever (60%) and weight loss (33%). Bacteriological evidence alone or in combination with other methods was used in 43% of diagnoses, while clinical and/or radiological evidence were used in 47%. 31% reported contact with a case of TB, usually at home, and 74% had received BCG. 21 had a tuberculin skin test performed and 8 tested positive. TB episodes occurred within 6 months of initiation of antiretroviral therapy in 9 cases, suggesting immune reconstitution. Conclusions: The proportion of affected children with close contact to a known TB case emphasizes the need for adequate contact tracing of adult TB cases. Diagnosis of TB may have indicated HIV infection in as many as half of the cases. Screening for HIV or TB should be performed in children upon diagnosis of either condition. Research on optimizing preventive strategies in TB-exposed, HIV+ children is needed.
Name: Jacqueline Menezes Mailing Address: Hospital dos Servidores do Estado, R. Sacadura Cabral 178 Anexo IV, 4 andar, 20221-903 RIO DE JANEIRO, Brazil Tel: 55(21) 2230018 Fax: 55(21) 22637135 Email: jacqueline@diphse.com.br
OBJECTIVES
To evaluate the occurrence of TB in a cohort of HIV infected infants, children and adolescents from Latin American countries. To describe cases of TB with respect to: Clinical presentation. The temporal association of TB diagnosis with HIV diagnosis. Diagnostic methods. Epidemiological data: 19 out of 58 subjects (33%) reported contact with a known case of TB. In 14/19 (74%) contact occurred at home. In 18/19 (95%) frequency of contact was daily. BCG immunization:
RESULTS
The most frequent signs and symptoms were fever, reported in 60%, and weight loss, reported in 33%. More than half (53%) were hospitalized for the TB episode.
Figure 4. Immune suppression and clinical presentation of TB in HIV-infected children. Clinical presentation in 22 cases for which CD4 results were available near the time of TB diagnosis.
RESULTS
Timing of TB diagnosis with respect to HIV diagnosis and initiation of ART: 50% were diagnosed with HIV first (median 11.4 mos; range 1.2-85.2 mos before TB diagnosis). 28% received both diagnoses within the same month. 22% were diagnosed with TB first (median 9.6 mos; range 4.5-33 mos before HIV diagnosis). 9 TB episodes (16%) occured within 6 months of initiating
4 Number of cases 3 2 1 0 2 1 0 CD4 <15% 0 CD4 15 - <25% 2 4 4 4 Miliary Pulm. Lymph.
METHODS
Study Population A retrospective study of TB diagnoses was done within the NISDI pediatric protocol, a prospective cohort study enrolling HIV-infected and HIV-exposed uninfected children at multiple clinical sites in Latin America. Subjects enrolled from 2002-2006 who had medical records available to sites from the time of TB episodes were included.
43/58 (74%) children received at least one dose of BCG (2 had received 2 doses). Age at BCG was < 1 month in 49% and < 6 months in 90%. Tuberculin Skin Testing (TST): PPD was performed in 21 (40%) of cases; 13 (62%) were negative. Use of Isoniazid preventive therapy (IPT) within the cohort: Only 9 subjects received IPT: 7 HIV+ and 2 HIV-; none of the children who received IPT developed TB disease.
5 5
ART, possibly indicating immune reconstitution syndrome.
CONCLUSIONS
One third of children with TB reported close contact with a known case of TB. None received IPT. Childhood TB reflects recent transmission and
25
24
CD4 >25%
points to inadequate contact tracing within health systems. Diagnosis of TB may have indicated HIV infection in 22% of subjects,
Number of patients
Definitions In presumed TB the diagnosis is suspected based on clinical, radiologic, and/or non-specific laboratory findings, as well as response to empiric treatment; specific tests for M.Tb were negative or not done. In proven TB, the criteria for a presumed case have been met and M.Tb has been detected by a specific test for the organism.
Level of immunosupression
20
15
15
16
<12mo 1-4yr
revealing possible missed opportunities for early diagnosis and treatment Table 1. Diagnostic Methods (all cases).
Bacteriologic alone Radiological alone Clinical alone 1 3 8 16 7
of HIV infection. Diagnosis of HIV could have prompted screening and prophylaxis for TB and might have avoided the development of active TB in some patients. Screening for HIV or TB should be performed in children upon diagnosis of either condition. Research on optimizing preventive strategies in TB-exposed, HIV positive children and improving diagnostic methods are needed.
10
5-14yr >14yr
3 <12mo 1-4yr 5-14yr >14yr
BACKGROUND
Infection and disease due to Mycobacterium tuberculosis (M.Tb) are highly prevalent in the developing world; TB is a major opportunistic infection in HIV-infected people. Infants and children under 5 years of age are at particular risk for infection, disease and death. Data about TB in HIV-infected children are scarce, partly because the diagnosis of TB is difficult in children and even more challenging in HIV-infected patients [1,2,3]. Compared to other countries in the region, TB incidence in Brazil (40.8/100,000) is comparable to that in Argentina (39/100,000), and higher than that in Mexico (21/100,000) [4,5]. Peru, Bolivia, Ecuador, Guyana and Haiti all have TB incidences > 100/100,000 [4,5]. Other studies describing cohorts of HIV infected children with TB have also been retrospective and/or hospital-based (2, 7-9).
Number of Cases
RESULTS
1404 infants, children and adolescents (742 HIV-infected, 620 HIV exposed, uninfected, 42 indeterminate) were enrolled at 15 sites (11 in Brazil, 2 in Mexico, 2 in Argentina) as March 2006. 1 case of TB was identified in the HIV- group (not discussed further). 58 in the HIV-infected (HIV+) group had an episode of TB. 91% of HIV+ TB cases (53/58) were diagnosed before enrollment.
30 25 20 15 10 5 0 Brazil Mexico 15 8 2 3 1 Proven Presumed 29
Clinical and radiological Clinical and Bacteriologic
Figure 2. Distribution of cases by age at TB diagnosis, according to the age ranges used by WHO.
Bacteriologic and Radiologic 1 All three categories No test reported 16 6
REFERENCES
1. 2. 3. 4. 5. 6. 7. 8. 9. Chintu C, et al. Int J Tuberc Lung Dis 2005; 9:477-484 Cohen JM, et al. HIV Medicine 2008; 9:277-284 Corrigan DL, et al. Breathe 2007; 3(4): 351-63 Brasil, (2007) Ministrio da Sade, Programa Nacional de Controle da Tuberculose, Secretaria de Vigilncia em Sade. WHO (2008) Global tuberculosis control www.who.int/tb/publications/global report/2008 accessed 01/02/2009 Rekha B, et al. Pediatr Resp Rev 2007; 8: 99-106 Geoghagen M, et al. CDC West Indian Med J 2004;53:339-345 Viani RM, et al. Int J Tuberc Lung Dis 2008; 12: 411-416 Ramrez-Cardich, et al. Int J Infect Dis 2006; 10:278-281
16 Number of cases 14 12 10 8 6 4 2 0 9
15
Table 2. Chest x-ray results at diagnosis
11 Miliary Pulmon. Lymph. 3 2 1 1 1 >14
Localized infiltrate Hilar/paratracheal adenopathy Miliary infiltrate Multilobar infiltrate Pleural effusion Cavitation
14/35 (40%) 12 /35 (34%) 10/ /35 (29%) 07 /35 (20%) 04 /35 (11%) 03 /35 (9%)
4 2 <12 mo
ACKNOWLEDGMENTS
Funded by:
Argentina
1-4 yr
5-14 yr
Figure 3. Clinical presentation by age at TB diagnosis. Figure 1. Distribution of cases of TB in HIV+ children according to country of origin and whether proven or presumed.
(Eunice Kennedy Shriver National Institute of Child Health and Human Development, Bethesda, Maryland). Supported by NICHD Contract # HHSN267200800001C (NICHD Control # N01-DK-8-0001). We want to thank the Study Participants, Clinical Sites, the NISDI Executive Committee, and Westat.
Você também pode gostar
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryNo EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryNota: 3.5 de 5 estrelas3.5/5 (231)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)No EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Nota: 4.5 de 5 estrelas4.5/5 (119)
- Never Split the Difference: Negotiating As If Your Life Depended On ItNo EverandNever Split the Difference: Negotiating As If Your Life Depended On ItNota: 4.5 de 5 estrelas4.5/5 (838)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaNo EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaNota: 4.5 de 5 estrelas4.5/5 (265)
- The Little Book of Hygge: Danish Secrets to Happy LivingNo EverandThe Little Book of Hygge: Danish Secrets to Happy LivingNota: 3.5 de 5 estrelas3.5/5 (399)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyNo EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyNota: 3.5 de 5 estrelas3.5/5 (2219)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeNo EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeNota: 4 de 5 estrelas4/5 (5794)
- Team of Rivals: The Political Genius of Abraham LincolnNo EverandTeam of Rivals: The Political Genius of Abraham LincolnNota: 4.5 de 5 estrelas4.5/5 (234)
- The Emperor of All Maladies: A Biography of CancerNo EverandThe Emperor of All Maladies: A Biography of CancerNota: 4.5 de 5 estrelas4.5/5 (271)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreNo EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreNota: 4 de 5 estrelas4/5 (1090)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersNo EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersNota: 4.5 de 5 estrelas4.5/5 (344)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceNo EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceNota: 4 de 5 estrelas4/5 (890)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureNo EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureNota: 4.5 de 5 estrelas4.5/5 (474)
- The Unwinding: An Inner History of the New AmericaNo EverandThe Unwinding: An Inner History of the New AmericaNota: 4 de 5 estrelas4/5 (45)
- The Yellow House: A Memoir (2019 National Book Award Winner)No EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Nota: 4 de 5 estrelas4/5 (98)
- Useful Vocabs For OET Writing & Speaking PDFDocumento2 páginasUseful Vocabs For OET Writing & Speaking PDFLiju K Oommen100% (3)
- Module 3 - Nursing Assessment in Family Nursing PracticeDocumento7 páginasModule 3 - Nursing Assessment in Family Nursing PracticeRogedith DelaRosaAinda não há avaliações
- Planning For A Health Career: Unit 4Documento34 páginasPlanning For A Health Career: Unit 4Lanie Tamacio BadayAinda não há avaliações
- Running Head: Evidence-Based Practice: Pressure Ulcer RiskDocumento5 páginasRunning Head: Evidence-Based Practice: Pressure Ulcer RiskElise HowardAinda não há avaliações
- Lesson Plan For COT First QuarterDocumento4 páginasLesson Plan For COT First QuarterJunnel Maravilla100% (1)
- Sanford Chris CVDocumento9 páginasSanford Chris CVChris SanfordAinda não há avaliações
- Medicine Lec.9 - Viral Infection IIDocumento42 páginasMedicine Lec.9 - Viral Infection II7fefdfbea1Ainda não há avaliações
- M. Sc. Nursing Programme Analysis: Post-Graduate Education-Msc NursingDocumento11 páginasM. Sc. Nursing Programme Analysis: Post-Graduate Education-Msc NursingMallika JoonAinda não há avaliações
- Steps in Viral Pathogenesis-Lecture ThreeDocumento3 páginasSteps in Viral Pathogenesis-Lecture ThreeIM CTAinda não há avaliações
- The Psychiatric Review of Symptoms - A Screening Tool For Family Physicians - American Family PhysicianDocumento7 páginasThe Psychiatric Review of Symptoms - A Screening Tool For Family Physicians - American Family PhysicianTimothy TurscakAinda não há avaliações
- Bells Palsy Handbook Facial Nerve Palsy or Bells Palsy Facial Paralysis Causes, Symptoms, Treatment, Face Exercises ... (Alan MC Donald DR Alexa Smith) (Z-Library)Documento94 páginasBells Palsy Handbook Facial Nerve Palsy or Bells Palsy Facial Paralysis Causes, Symptoms, Treatment, Face Exercises ... (Alan MC Donald DR Alexa Smith) (Z-Library)mayakhoAinda não há avaliações
- An Impression Technique For Patients With Fixed Orthodontic AppliancesDocumento2 páginasAn Impression Technique For Patients With Fixed Orthodontic Appliancesmoji_puiAinda não há avaliações
- Case Study: Epidemiology LaboratoryDocumento5 páginasCase Study: Epidemiology LaboratoryDonna IlarAinda não há avaliações
- Better Strategies For Covid VaccinationsDocumento8 páginasBetter Strategies For Covid VaccinationsMiguel Angel Vilar HerreroAinda não há avaliações
- Knowledge, Attitude and Practice of Cancer Screening Among Health Care Professionals in A Central Hospital in NepalDocumento8 páginasKnowledge, Attitude and Practice of Cancer Screening Among Health Care Professionals in A Central Hospital in NepalBruce LennyAinda não há avaliações
- Chapter 1 Lesson 1Documento8 páginasChapter 1 Lesson 1Aizel ManiagoAinda não há avaliações
- Robsons Ten Group Classification of Cesarean Section at A Tertiary Center in NepalDocumento6 páginasRobsons Ten Group Classification of Cesarean Section at A Tertiary Center in NepalgehanathAinda não há avaliações
- Manangan, Eugene B. - FDAR Boggy UterusDocumento2 páginasManangan, Eugene B. - FDAR Boggy UterusGin MananganAinda não há avaliações
- Observational Studies Lecture - ReviewDocumento3 páginasObservational Studies Lecture - ReviewKelsey AndersonAinda não há avaliações
- Caries TimelineDocumento11 páginasCaries TimelineManuelRomeroFAinda não há avaliações
- Guidelines For Toxicity/safety Profile Evaluation of Ayurved & Siddha, Plant DrugsDocumento5 páginasGuidelines For Toxicity/safety Profile Evaluation of Ayurved & Siddha, Plant DrugsPRAKASH DESHPANDEAinda não há avaliações
- Fellowship Accreditation in Pediatric Otolaryngology: A Review of The IssuesDocumento5 páginasFellowship Accreditation in Pediatric Otolaryngology: A Review of The IssuesDeepBhattacharyyaAinda não há avaliações
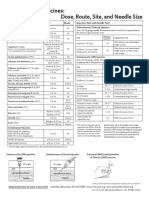
- Injection Site and Needle Size Vaccine Dose RouteDocumento1 páginaInjection Site and Needle Size Vaccine Dose RouteDr Ambana GowdaAinda não há avaliações
- BG Group Standard Health Management BG-ST-HR-SER-004 (HSSE Management System Framework Section 9.1.3)Documento18 páginasBG Group Standard Health Management BG-ST-HR-SER-004 (HSSE Management System Framework Section 9.1.3)Sunday Augustine ChibuzoAinda não há avaliações
- Breast LumpDocumento4 páginasBreast LumpYoussef Refaat RaoofAinda não há avaliações
- Medical MycologyDocumento10 páginasMedical MycologyNive KojAinda não há avaliações
- Konsulta ItrDocumento1 páginaKonsulta ItrBarangay DanaoAinda não há avaliações
- Eform For Players Cluster MeetDocumento8 páginasEform For Players Cluster Meetseph bronAinda não há avaliações
- Pedia Tickler Update 2017Documento2 páginasPedia Tickler Update 2017Tani BokAinda não há avaliações
- What Is Brain CancerDocumento3 páginasWhat Is Brain Canceryash vardhanAinda não há avaliações