Escolar Documentos
Profissional Documentos
Cultura Documentos
CPR
Enviado por
Margeline PepinoDescrição original:
Título original
Direitos autorais
Formatos disponíveis
Compartilhar este documento
Compartilhar ou incorporar documento
Você considera este documento útil?
Este conteúdo é inapropriado?
Denunciar este documentoDireitos autorais:
Formatos disponíveis
CPR
Enviado por
Margeline PepinoDireitos autorais:
Formatos disponíveis
Cardiopulmonary Resuscitation
349
Procedure 17: Cardiopulmonary Resuscitation
Introduction
Cardiopulmonary arrest (CPA) occurs when a patients heart and lungs stop functioning. In children, CPA usually begins as a primary respiratory arrest. This is in contrast to adults, in whom CPA or sudden death is almost always Contraindication a primary cardiac event that occurs with onset Newly born, infant, or child with effective perfusion (palpable central or of ventricular fibrillation and an abrupt change peripheral pulse) in the hearts electrical activity. Because cessation of effective breathing is the precipitating Equipment factor in pediatric CPA, airway management Mouth-to-mask device and ventilation are to children in CPA what Bag-mask device, infant or child defibrillation is to adults. Cardiopulmonary Airway adjuncts Appropriate mask sizes resuscitation (CPR) refers to basic airway management, artificial ventilation, and chest compressions to provide oxygen and circulation to core organs: the heart, brain, and lungs. In children, CPR has been shown to improve survival from drowning, and it may also benefit patients in CPA from other causes.
Indications Newly born, neonate, infant, or child of any age who is apneic and pulseless Newly born with a heart rate less than 60 beats/min and not improving after standard newborn care Neonate, infants and children with a heart rate less than 60 beats/min and poor perfusion.
Rationale
CPR encompasses the basic procedures for sustaining critical oxygenation, ventilation, and perfusion recommended by the American Heart Association. The pediatric techniques are slightly modified from the adult techniques to reflect the known differences in CPA between age groups. Furthermore, there are specific differences between infants and children, including num-
ber of rescuers, placement of hands and fingers, rates of ventilation, and rates and depth of chest compressions.
Preparation
1. Position a child on a hard surface. Position a neonate or infant on a hard surface or on the forearm of the rescuer with the hand supporting the head.
17-1 Assess Responsiveness
Assess responsiveness. If unresponsive, assess breathing.
350
Cardiopulmonary Resuscitation
17-2 Assess Breathing
Open airway using either the headtilt/chin-lift maneuver (medical patient) or modified jaw thrust maneuver (trauma patient) to achieve a neutral position. If spinal injury is possible, have a second rescuer maintain manual spinal stabilization. Remove any obvious obstructions, such as loose teeth or vomitus.
Look, listen, and feel for signs of breathing.
Manipulation of the head to keep the airway in a neutral position is essential for effective ventilation. A towel roll under the shoulders of the infant or small child may help maintain neutral head position.
Compression Rates
These are the timing rates for single rescuers, not the actual number of compressions delivered each minute because of pauses for ventilations and reassessments. Newly born: At least 120 events/min Neonate and infant: 100 compressions/min Child 18 years: 100 compressions/min Child over 8 years: 100 compressions/min
Possible Complications
Coronary vessel injury Diaphragm injury Hemopericardium Hemothorax Interference with ventilation Liver injury Myocardial injury Pneumothorax Rib fractures Spleen injury Sternal fracture
Cardiopulmonary Resuscitation
351
17-3 Ventilation Rate
If not breathing, begin mouth-to-mask ventilation, or perform bag-mask ventilation with 100% oxygen. Give two initial breaths at a rate of 1 second per breath. If breaths now expand the chest, assess pulse. Take no more than 10 seconds. Slowly repeat squeeze-release-release to time bag-mask ventilation rate.
If first breath does not expand the chest, reposition the head and attempt again. If breaths are still ineffective, suction the mouth with a bulb syringe or flexible suction catheter (newly born) or a large-bore rigid suction catheter (neonates, infants, and children) and attempt breaths again.
If pulse is present ( 60 beats/min), but the victim is still not breathing, continue ventilations. Give one every 2 seconds in newly born and rescue breaths at a rate of 12 to 20 breaths per minute (every 3 to 5 seconds) until spontaneous breathing resumes.
Use the E-C clamp technique to achieve a good mask seal and watch for adequate chest rise to ensure effective ventilation.
Continuously assess effectiveness of CPR by ensuring chest rise and feeling for a palpable pulse every 2 minutes.
352
Cardiopulmonary Resuscitation
17-4 Compression Rate
Check central pulse. Newly born: umbilical cord stump or listen to precordium. Neonate and infant: brachial pulse or femoral pulse. Child: carotid pulse. If pulse is absent or if heart rate is less than 60 beats/min, with shock or poor peripheral perfusion, begin chest compressions. Newly born: 3 compressions: 1 ventilation. Neonate, infant, and child: one rescuer 30 compressions: 2 ventilations, two rescuers 15 compressions: 2 ventilations. Use proper compression technique, compression-ventilation ratio, depth of compression, and compression-release ratio (Tables P17-1 and P17-2).
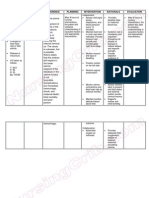
Table P17-1
Age
Newly born (<1 day) Neonate (128 days) and infant (112 months) Child 18 years Child over 8 years One or two rescuers
Compression and Ventilation Rates per Minute*
Rate of Compressions (min)
120 100 100 100
Rescue Breaths per Minute without Compressions (mouth to mouth or mask)
30 1220 1220 1012
Rescue Breaths per Minute with Compressions with Advanced Airway
30 810 810 810
*The rate of compressions and the actual number of compressions delivered per minute are different. The rate of compressions refers to the timing of compressions when they are being performed, and the rate does not account for pauses for breathing. Delivered compressions are the actual number of compressions delivered per minute after accounting for breathing. The ratios are calculated from the timing rates, not the delivered rates.
Table P17-2
Age
Newly born (< 1 day) Neonate (128 days) One rescuer Two rescuers Infant (112 months) One rescuer Two rescuers Child 18 years One rescuer Two rescuers Child over 8 years One or two rescuers
Parameters for BLS Resuscitation for Health Care Providers
Compressions (min)
120
Compression to Ventilation Ratio
3:1
1 /3
Depth (in)
depth of chest
Hand Placement for Compression
2 fingers at lower 1/3 of sternum, 1 finger below nipple line, or 2 thumbs at midsternum with hands encircling chest 2 or 3 fingers at lower 1/3 of sternum, 1 finger below nipple line 2 thumbs at midsternum with hands encircling chest 2 fingers at midsternum, 1 finger below nipple line 2 thumbs at lower 1/2 of sternum with hands encircling chest
100 30:2 15:2 100 30:2 15:2 100 30:2 15:2 100 30:2
1 /3
to 1/2 depth of chest
1 /3
to 1/2 depth of chest
1 /3 to 12 depth of chest /
Heel of 1 or 2 hands at lower 1/2 of sternum (do not push on xiphoid process) Heel of one hand, other hand on top, at lower 1/2 of sternum between nipples
1.52.0 inches
Cardiopulmonary Resuscitation
353
17-5 Finger or Hand Placement
Newly born: Use the two thumb encircling chest method for the newborn. The two finger method is acceptable, but should be used when the two thumb method is not easily accomplished. Compression depth should be one third of chest depth. Two thumb technique: encircle the chest and use thumbs just below the intermammary line with the fingers supporting the spine. Two finger technique: Use two fingers on the lower 1/3 of the sternum just below the intermammary line, with the other hand supporting the spine. Lay rescuers and lone health care providers use two finger technique. Two health care providers use two thumbs encircling hands technique. Child (1 to 8 years old): Use the heel of one hand on the sternum above the xiphoid process. Compression depth should be one third to one half the depth of the chest. Child (> 8 years): Use the heel of both hands on the sternum above the xiphoid process.
17-6 Compressions
The depth of chest compressions should be approximately one third to one half the depth of the chest. Compressions should be deep enough to produce a palpable brachial, femoral, or carotid pulse. Push hard and fast and release completely to allow chest to fully rise. Use the two-rescuer technique when possible. Reassessment: Check pulse after approximately every 5 compressionventilation cycles.
A common problem in the transition from one-rescuer to two-rescuer child CPR is the lack of coordination between ventilations and compressions.
354
AED and Defibrillation
Procedure 18: AED and Defibrillation
Introduction
Synchronized cardioversion for tachydysrhythmias has long been part of adult emergency care and is one of the most effective treatments for sudden cardiac arrest from ventricular dysrhythmias. However, ventricular dysrhythmias are rare in children, especially in infants, and Contraindication pediatric supraventricular tachycardia (SVT) is Conscious patient with good perfusion usually treatable with medical therapy. For these reasons, pediatric synchronized carEquipment dioversion is not often indicated. However, Automatic external defibrillator when a child develops ventricular fibrillation or Standard defibrillator pulseless ventricular tachycardia, defibrillation Newer models feature lower power outputs to deliver lower energy countershocks (unsynchronized cardioversion) may be lifesaving. Also, synchronized cardioversion may resuscitate a child in shock with SVT. Use the synchronized mode when there is SVT or ventricular tachycardia with a pulse, and the asynchronized (defibrillation) mode for ventricular fibrillation or ventricular tachycardia without a pulse.
Indications Ventricular fibrillation Pulseless ventricular tachycardia SVT with shock and no vascular access rapidly available (synchronized) Ventricular tachycardia with shock and unresponsiveness with pulse and no vascular access rapidly available Atrial fibrillation or atrial flutter with shock
Rationale
When a childs heart deteriorates into ventricular tachycardia or fibrillation, there is usually a severe systemic insult such as profound hypoxia, ischemia, electrocution, or myocarditis. Death may result if treatment is delayed. SVT, in contrast, is usually a more stable cardiac rhythm. When the child is pulseless and has ventricular fibrillation or ventricular tachycardia, perform defibrillation as quickly as possible with the appropriate technique. If a child has SVT or ventricular tachycardia and shock, use synchronized cardioversion. Do not attempt to perform synchronized cardioversion on a child with SVT who is well perfused.
Do not deliver synchronized cardioversion to a conscious child with SVT or ventricular tachycardia unless the child is in shock and has no IV or IO access rapidly available for medical treatment.
Preparation
1. Open airway and ventilate with bag-mask device with 100% oxygen while assembling equipment for cardioversion or defibrillation. 2. If child is pulseless, begin closed-chest compressions, until automatic external defibrillator (AED) or conventional defibrillator is available.
For a child with ventricular fibrillation or pulseless ventricular tachycardia, use the asynchronized (defibrillation) mode.
AED and Defibrillation
355
18-1 Conventional Defibrillator Use
Apply the paddles directly to the skin. Place one paddle on the anterior chest wall on the right side of the sternum inferior to the clavicle and the other paddle on the left midclavicular line at the level of the xiphoid process. As another option, use the anterior-posterior position. Begin recording rhythm. Deliver the electrical countershock with firm pressure. per EMS protocol. Treat bradycardia or other dysrhythmias.
Assess the patient for evidence of reperfusion and check the monitor for the rhythm. Clear the nearby area to avoid shocking someone. Announce, I am going to shock on three. One, I am clear. Two, you are clear. Three, everybody is clear.
If the first electrical shock is unsuccessful, deliver additional electrical countershocks as per EMS protocol. Give specific dysrhythmia treatment with epinephrine or other drugs, as
The preferred paddle location in children is controversial and no study in humans has compared the two techniques. Anterior chest wall placement has the advantage of a supine child and easier airway management. Anterior-posterior placement may allow larger paddles and more effective delivery of the charge.
Preparation
Conventional Defibrillator Use
1. Select the proper paddle size. Use the 8-cm adult paddles if these will fit on the chest wall; otherwise, use the 4.5-cm pediatric paddles (Table P18-1). 2. Prep paddles or skin electrodes with electrode jelly, paste, or saline-soaked gauze pads, or use self-adhesive defibrillator pads. Do not let jelly or paste from one site touch the other and form an electrical bridge between sites, which could result in ineffective defibrillation or skin burns. 3. Establish appropriate electrical charge (Table P18-2). 4. Select synchronized or asynchronized mode. 5. Properly charge pack and stop chest compressions.
Table P18-1
Paddle Size
8-cm adult paddles (Use in children over 12 months of age or weighing more than 10 kg) On anterior chest wall, OR Anterior-posterior 4.5-cm pediatric paddles (Use in infants up to 12 months of age or weighing less than 10 kg) on the anterior chest wall
Failure to firmly apply paddles to the chest wall will decrease effective delivery of charge.
356
AED and Defibrillation
18-2 One Rescuer with an AED
For children under 8 years of age use a child-pad cable system if available. There are inadequate data to recommend AED use for the child less than 1 year of age. Verify unresponsiveness. Check for signs of circulation. If there are no signs of circulation, attach the AED and proceed with the AED treatment algorithm. The AED operator should take the following actions. ATTACH the AED. Select the correct pads for victims size and age (adult vs. child). Peel the backing from the pads. Attach the adhesive pads to the victim as shown on the pads. (If only adult pads are available, and they overlap when placed on the chest, use an anterior [chest] and posterior [back] placement.) Attach the electrode cable to the AED (if not preconnected).
Open the airway, and check for breathing. POWER ON the AED and follow voice prompts. Some devices will turn on when the AED lid or carrying case is opened.
Allow the AED to ANALYZE the victims rhythm (clear victim during analysis). Deliver a SHOCK if needed (clear victim before shock).
If the victim is not breathing effectively, give two ventilations.
Reasonable variations in this sequence are acceptable.
Table P18-2
Dysrhythmia
Ventricular fibrillation Ventricular tachycardia without a pulse
Appropriate Electrical Charge for Countershock
Mode
Defibrillation (asynchronized)
Possible Complications
Ineffective delivery of countershock because of failure to charge, improper positioning on the chest, incorrect paddle size, or improper conduction medium Burns on the chest wall Failure to clear before voltage discharge, leading to electrical shock of a team member or bystander Tachydysrhythmia Bradycardia Myocardial damage or necrosis Cardiogenic shock Embolic phenomena
Charge
2 J/kg, then 4 J/kg, then 4 J/kg, as needed. Then 4 J/kg after CPR and each dose of medication. 0.51.0 J/kg. Repeat as needed.
Ventricular tachycardia with pulse SVT Atrial fibrillation and atrial flutter with shock
Synchronized
AED and Defibrillation
357
18-3 Two Rescuer AED Sequence of Action
Adapted from Circulation 2005: 112: IV 3546. Verify unresponsiveness. If victim is unresponsive, have partner call 9-1-1. Get AED. Check for signs of circulation: if no signs of circulation are present, perform these steps. Perform chest compressions and prepare to attach the AED. If there is any doubt that the signs of circulation are present, the first rescuer initiates chest compressions while the second rescuer prepares to use the AED. Remove clothing covering the victims chest to provide chest compressions and apply the AED electrode pads. ATTACH the AED to the victim. Select correct pads for the victims size and age. Peel the backing from the pads. Ask the rescuer performing CPR to stop chest compressions. Attach the adhesive pads to the victim as shown on the pads. (If only adult pads are available, and they overlap when placed on the chest, use an anterior [chest] and posterior [back] placement.) Attach the AED connecting cables to the AED (if not preconnected). ANALYZE rhythm. Clear the victim before and during analysis. Check that no one is touching the victim. Press the ANALYZE button to start rhythm analysis (some brands of AEDs do not require this step).Shock Indicated message. Resume CPR until AED is charged and ready to deliver shock. Clear the victim once more before pushing the SHOCK button (Im clear, youre clear, everybodys clear). Check that no one is touching the victim. Press the SHOCK button (victim may display muscle contractions). No Shock Indicated message. Check for signs of circulation (including a pulse). If signs of circulation are present, check breathing. If breathing is inadequate, assist breathing. If breathing is adequate, place the victim in the recovery position, with the AED attached.
Open airway: head-tilt/chin-lift (or jaw thrust if trauma is suspected).
Check for effective breathing: provide breathing if needed. Check for breathing (look, listen, and feel). If not breathing, give two slow breaths. A mouthto-mask device should be available in the AED carrying case.
Attempt defibrillation with the AED if no signs of circulation are present. Place the AED near the rescuer who will be operating it. The AED is usually placed on the side of the victim opposite the rescuer who is performing CPR. The rescuer begins performing CPR while the rescuer who was performing CPR prepares to operate the AED. (It is acceptable to reverse these roles.)
The AED operator takes the following actions. POWER ON the AED first (some devices will turn on automatically when the AED lid or carrying case is opened).
If no signs of circulation are present, resume CPR for 5 cycles, then recheck for signs of circulation. If there are still no signs of circulation, analyze rhythm, repeat the analyze rhythm step, then follow the shock indicated or no shock indicated steps as appropriate.
Você também pode gostar
- First Aid Essentials for Life Saving (39Documento64 páginasFirst Aid Essentials for Life Saving (39KBDAinda não há avaliações
- Adult BLSDocumento22 páginasAdult BLSnessaoliveiraAinda não há avaliações
- Basic Life SupportDocumento5 páginasBasic Life SupportbuenoevelynAinda não há avaliações
- CPR - Cardiopulmonary ResuscitationDocumento31 páginasCPR - Cardiopulmonary ResuscitationPanji HerlambangAinda não há avaliações
- IGNOU MBA MS-11 Solved AssignmentDocumento5 páginasIGNOU MBA MS-11 Solved AssignmenttobinsAinda não há avaliações
- RSI For Nurses ICUDocumento107 páginasRSI For Nurses ICUAshraf HusseinAinda não há avaliações
- BASIC LIFE SUPPORT: ESSENTIAL CONCEPTS AND PROCEDURESDocumento8 páginasBASIC LIFE SUPPORT: ESSENTIAL CONCEPTS AND PROCEDURESHynne Jhea EchavezAinda não há avaliações
- Acls AnpDocumento20 páginasAcls AnpNirupama KsAinda não há avaliações
- FINAL CA-1 Tutorial Textbook 2017Documento74 páginasFINAL CA-1 Tutorial Textbook 2017Farjad IkramAinda não há avaliações
- Anesthesia TechnologyDocumento56 páginasAnesthesia TechnologyDeepali SinghAinda não há avaliações
- Spinal Anesthesia: Ji Mandal Ji Solonio Ji Tumanan Ji TuveraDocumento32 páginasSpinal Anesthesia: Ji Mandal Ji Solonio Ji Tumanan Ji TuveraGehlatin TumananAinda não há avaliações
- Seminar ON Cardiopulmonary Resuscitation: Submitted To Submitted byDocumento18 páginasSeminar ON Cardiopulmonary Resuscitation: Submitted To Submitted bymerin sunilAinda não há avaliações
- Severe Dengue in ICUDocumento35 páginasSevere Dengue in ICUanaeshklAinda não há avaliações
- Aldrete Discharge Scoring - Appropriate For Post Anesthesia PhaseDocumento28 páginasAldrete Discharge Scoring - Appropriate For Post Anesthesia PhaseHeather PorterAinda não há avaliações
- Role of Anesthesia Nurse in Operation TheatreDocumento37 páginasRole of Anesthesia Nurse in Operation TheatreZainul SaifiAinda não há avaliações
- Ava Checklist BookletDocumento16 páginasAva Checklist BookletCatarina Rafaela100% (1)
- Algorithm For Perioperative Management of Anticoagulation1Documento8 páginasAlgorithm For Perioperative Management of Anticoagulation1andi namirah100% (1)
- Lecture 9 BurnsDocumento4 páginasLecture 9 BurnsRose Ann RaquizaAinda não há avaliações
- Orientation To AnesthesiaDocumento28 páginasOrientation To AnesthesiaDebi SumarliAinda não há avaliações
- Cardiopulmonary ResuscitationDocumento29 páginasCardiopulmonary ResuscitationSarahAinda não há avaliações
- Basic Life SupportDocumento22 páginasBasic Life SupportDhiren PranamiAinda não há avaliações
- Perioperative Fluid TherapyDocumento36 páginasPerioperative Fluid TherapyUmhy GumianaAinda não há avaliações
- BLS: Essential Steps for Cardiac EmergenciesDocumento10 páginasBLS: Essential Steps for Cardiac EmergenciesharpreetAinda não há avaliações
- CPRDocumento4 páginasCPRjeetAinda não há avaliações
- Surgical Cricothyrotomy (Assist)Documento5 páginasSurgical Cricothyrotomy (Assist)ydtrgnAinda não há avaliações
- Disaster MGMTDocumento72 páginasDisaster MGMTVarinder PalAinda não há avaliações
- Ic-01-039 Infection Control in Adult Intensive Care UnitDocumento7 páginasIc-01-039 Infection Control in Adult Intensive Care UnitDerick RanaAinda não há avaliações
- Addis Ababa University Faculty of Medicine Difficult Airway ManagementDocumento54 páginasAddis Ababa University Faculty of Medicine Difficult Airway ManagementagatakassaAinda não há avaliações
- PG Guide BooksDocumento4 páginasPG Guide BooksKingKamalAinda não há avaliações
- Basic Life SupportDocumento22 páginasBasic Life SupportTotoLesterAinda não há avaliações
- How To Prepare For The EDAIC 2019Documento17 páginasHow To Prepare For The EDAIC 2019sand52525Ainda não há avaliações
- DPN Icu PDFDocumento1 páginaDPN Icu PDFharoonAinda não há avaliações
- Anes AirwayDocumento24 páginasAnes AirwayyanaAinda não há avaliações
- ECG MonitoringDocumento28 páginasECG MonitoringGlaiza Mae Olivar-ArguillesAinda não há avaliações
- UCL Aneasthesia Year 4 Workbookv15Documento83 páginasUCL Aneasthesia Year 4 Workbookv15Jay KayAinda não há avaliações
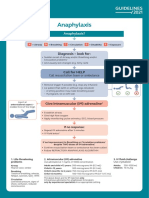
- Anaphylaxis Algorithm 2021Documento1 páginaAnaphylaxis Algorithm 2021Shawn Gaurav JhaAinda não há avaliações
- Hospital Emergency Response ChecklistDocumento26 páginasHospital Emergency Response ChecklistlupibudiAinda não há avaliações
- Paediatric Life SupportDocumento88 páginasPaediatric Life SupportmaharaniAinda não há avaliações
- Sop Icu H & FW 12725 28.04.2018Documento20 páginasSop Icu H & FW 12725 28.04.2018shah007zaadAinda não há avaliações
- Ventilator Systems ExplainedDocumento26 páginasVentilator Systems ExplainedAnh TrầnAinda não há avaliações
- Handbook For Iccp Item WritersDocumento14 páginasHandbook For Iccp Item WriterssanthoshvjAinda não há avaliações
- ICU Severity ScoresDocumento49 páginasICU Severity ScoresRizki Puji AgustinAinda não há avaliações
- Modes of Cardiac Pacing, Nomenclature and SelectionDocumento32 páginasModes of Cardiac Pacing, Nomenclature and SelectionMohammad AlmuhaiminAinda não há avaliações
- Anaphylaxis With Angioedema: Section I: Scenario DemographicsDocumento7 páginasAnaphylaxis With Angioedema: Section I: Scenario DemographicsharasthaAinda não há avaliações
- Abcde ApproachDocumento3 páginasAbcde ApproachMaria Isabel Medina MesaAinda não há avaliações
- 2020 BLS Science Summary TableDocumento1 página2020 BLS Science Summary TableChristine ElbanbuenaAinda não há avaliações
- Acute Lung Injury and Ards: Andreas Crede Emergency Medicine RegistrarDocumento47 páginasAcute Lung Injury and Ards: Andreas Crede Emergency Medicine RegistrarYohanes FirmansyahAinda não há avaliações
- Intubation ProcedureDocumento5 páginasIntubation ProcedurePurwadi SujalmoAinda não há avaliações
- Basic Life SupportDocumento2 páginasBasic Life SupportMeg GutierrezAinda não há avaliações
- Cardiopulmonary ResuscitationDocumento8 páginasCardiopulmonary ResuscitationEditor IJTSRDAinda não há avaliações
- Recruitment Maneuvers and PEEP TitrationDocumento17 páginasRecruitment Maneuvers and PEEP TitrationDiego Cruces OrdoñezAinda não há avaliações
- Dr. Aris - Introduction of Anesthesiology DR - Aris, SpAnDocumento60 páginasDr. Aris - Introduction of Anesthesiology DR - Aris, SpAnErlita FebriyantiAinda não há avaliações
- Cant Intubate Cant VentilateDocumento6 páginasCant Intubate Cant Ventilatedannyromero2712Ainda não há avaliações
- Life Threatening Rhythm: Presenter: Muhammad Najmuddin Bin Hussain 2. Wan Muhammad Nasirudin Bin Wan YusoffDocumento17 páginasLife Threatening Rhythm: Presenter: Muhammad Najmuddin Bin Hussain 2. Wan Muhammad Nasirudin Bin Wan YusoffWan NasirudinAinda não há avaliações
- ELSO Guidelines General All ECLS Version1.1 PDFDocumento24 páginasELSO Guidelines General All ECLS Version1.1 PDFBranka KurtovicAinda não há avaliações
- Chest PT in Icu 1996@609.full PDFDocumento17 páginasChest PT in Icu 1996@609.full PDFDyah SafitriAinda não há avaliações
- Basic Life Support (BLS) and Advanced Cardiac Life Support (ACLS)Documento7 páginasBasic Life Support (BLS) and Advanced Cardiac Life Support (ACLS)Rizki YuliantoAinda não há avaliações
- ICU Scoring Systems A Complete Guide - 2020 EditionNo EverandICU Scoring Systems A Complete Guide - 2020 EditionAinda não há avaliações
- Nursing Care Plan Placenta PreviaDocumento2 páginasNursing Care Plan Placenta Previaderic98% (42)
- 45 MargeDocumento1 página45 MargeMargeline PepinoAinda não há avaliações
- Mefenamic AcidDocumento4 páginasMefenamic AcidprincijinAinda não há avaliações
- JNC 7 (Klasifikasi Hipertensi) PDFDocumento2 páginasJNC 7 (Klasifikasi Hipertensi) PDFAbdur RahmanAinda não há avaliações
- AbortionDocumento16 páginasAbortionMargeline PepinoAinda não há avaliações
- Pediatric Emergency Assessment Recognition and StabilizationDocumento182 páginasPediatric Emergency Assessment Recognition and StabilizationFernando Arancibia100% (2)
- CPR/AED For The Professional RescuerDocumento35 páginasCPR/AED For The Professional RescuerLany dwiAinda não há avaliações
- Lifepak 20e: Defibrillator/MonitorDocumento12 páginasLifepak 20e: Defibrillator/MonitorGabriel MudlongAinda não há avaliações
- 15 Item ACLS Drill Answers and RationaleDocumento6 páginas15 Item ACLS Drill Answers and RationaleAijem RyanAinda não há avaliações
- BLS TestDocumento76 páginasBLS Testshishashane73% (11)
- P/N:Eng-Beneheart D3-210285X8P-20180411: ©2018 Shenzhen Mindray Bio-Medical Electronics Co.,Ltd. All Rights ReservedDocumento4 páginasP/N:Eng-Beneheart D3-210285X8P-20180411: ©2018 Shenzhen Mindray Bio-Medical Electronics Co.,Ltd. All Rights ReservedrachmonaaAinda não há avaliações
- Resuscitation Guide Lines 2005: Aries PerdanaDocumento36 páginasResuscitation Guide Lines 2005: Aries PerdanaLa Ode RinaldiAinda não há avaliações
- Medical Emergencies in The Dental Surgery20.11.08Documento21 páginasMedical Emergencies in The Dental Surgery20.11.08Yusuf KozniewskiAinda não há avaliações
- Desfibrilador DEA LifepointDocumento22 páginasDesfibrilador DEA LifepointabeklAinda não há avaliações
- BHF Community Report 2015 PDFDocumento14 páginasBHF Community Report 2015 PDFKen KnickerbockerAinda não há avaliações
- Resume of Yelly2danniDocumento1 páginaResume of Yelly2danniapi-31704300Ainda não há avaliações
- SCHILLER - Fred Easy - ManualDocumento94 páginasSCHILLER - Fred Easy - ManualMatíasAinda não há avaliações
- Survival Techniques PrelimDocumento26 páginasSurvival Techniques PrelimIsaackurt AdaAinda não há avaliações
- CCC CPR AED Community Training GenericDocumento18 páginasCCC CPR AED Community Training GenericDev Dutt Dey100% (1)
- BLS CPR and AED Skills EvaluationDocumento1 páginaBLS CPR and AED Skills EvaluationACHS IVAinda não há avaliações
- Soal Kasus HipertensiDocumento3 páginasSoal Kasus HipertensiAlya NamiraAinda não há avaliações
- HESI ReviewerDocumento10 páginasHESI ReviewerAnonymous XhAUv9lp8100% (2)
- 15-1010 BLS ProviderManual S PDFDocumento99 páginas15-1010 BLS ProviderManual S PDFAlma Aulia100% (7)
- Camden Squadron - Dec 2009Documento12 páginasCamden Squadron - Dec 2009CAP Unit NewslettersAinda não há avaliações
- AmericanRedCross RespondingToEmergencies InstructorsManual 031612Documento351 páginasAmericanRedCross RespondingToEmergencies InstructorsManual 031612jacobrts80% (5)
- Basic First Aid For Cardiac Arrest: ShockDocumento6 páginasBasic First Aid For Cardiac Arrest: ShockJinky Verano CortezAinda não há avaliações
- r215 NremtDocumento1 páginar215 Nremtapi-538596708Ainda não há avaliações
- Pediatric Medical DevicesDocumento25 páginasPediatric Medical DevicesDuck Mann-ConsulAinda não há avaliações
- BeneHeart C and S Series Ops Manual (English)Documento78 páginasBeneHeart C and S Series Ops Manual (English)Bong Kek ChiewAinda não há avaliações
- Rec Center News Sun City West May 2008Documento24 páginasRec Center News Sun City West May 2008Del Webb Sun Cities MuseumAinda não há avaliações
- Jfe-700 (E) 7zpna2082 (Ed.4) Installation 210706Documento202 páginasJfe-700 (E) 7zpna2082 (Ed.4) Installation 210706Papa StasAinda não há avaliações
- Maintain First Aid KitsDocumento3 páginasMaintain First Aid KitsMarshal OctavianusAinda não há avaliações
- Palatine IL Ex-Mayor Rita Mullins Claims Save-A-Life Foundation Trained Chicago Police (2001)Documento2 páginasPalatine IL Ex-Mayor Rita Mullins Claims Save-A-Life Foundation Trained Chicago Police (2001)Gordon T. PrattAinda não há avaliações
- Emergency Medical ServicesDocumento9 páginasEmergency Medical ServicesSAinda não há avaliações
- IVE BLS Provider Manual Ebook, International EnglishDocumento179 páginasIVE BLS Provider Manual Ebook, International EnglishDayanna Narciso80% (5)