Escolar Documentos
Profissional Documentos
Cultura Documentos
The Complete Periodontal Examination
Enviado por
Piyusha SharmaDescrição original:
Direitos autorais
Formatos disponíveis
Compartilhar este documento
Compartilhar ou incorporar documento
Você considera este documento útil?
Este conteúdo é inapropriado?
Denunciar este documentoDireitos autorais:
Formatos disponíveis
The Complete Periodontal Examination
Enviado por
Piyusha SharmaDireitos autorais:
Formatos disponíveis
GARY C.
ARMITAGE
A thorough periodontal examination is a critically important data-collection activity that is necessary to arrive at a diagnosis and develop a treatment plan.
The purpose of this chapter is to itemize and describe the basic components of a complete periodontal examination and briefly review their importance in the overall care of the patient.
Prior to conducting the hands-on examination, the information-gathering process begins with taking medical and dental histories from the patient. A valuable aspect of this history-taking discussion is that it begins to develop the doctor-patient relationship.
The discussion helps in clarify important variables that may affect the periodontal health of the patient. A key component of the history-taking session is determination of the patients chief complaint. Prior to the examination it is important to know why the patient is seeking a periodontal evaluation.
With advance knowledge of the chief complaint, the examiner can, during the course of the examination, specifically look for possible expectations or causes of patients concerns and problems.
Prior to conducting a periodontal examination it is customary to routinely inspect the extraoral tissues of the head & neck. Examination of all non- periodontal tissues in the mouth should be performed. Performance of a periodontal examination is a multi-task activity. The examiner looks for any signs of periodontal disease or other abnormalities.
In general, an overall inspection is made during which changes in color, shape & texture of the gingival tissues are assessed. An appraisal of potential etiologic & predisposing factors is continuously being made during the examination process.
Detailed measurements of probing depths and clinical attachment loss are taken & recorded. Finally, the teeth are inspected for occlusal relationships and restorative needs.
One of the very first things to note during a periodontal examination is the presence or absence of disease. The four most common signs of gingival inflammation that are routinely observed during a periodontal examination are:
1. 2. 3. 4.
Redness Swelling Bleeding on probing Purulent exudate Gingival redness & swelling usually are seen together and occur first at the gingival margin
Without treatment the inflammation can eventually involve the interproximal area and in some cases extend into portions of attached gingiva.
Sometimes the redness associated with gingival inflammation can be subtle. Healthy gingiva is firm and resilient, whereas edematous tissue is often enlarged and puffy. Recognition of the presence or absence of gingival edema helps the clinician determine if the tissues are healthy or diseased.
It also serves another important purposeanticipating the response to treatment. It should also be remembered that not all areas of gingival redness and swelling are due to periodontal disease, endodontic infections sometimes drain through the orifice of a periodontal pocket thereby mimicking a periodontal abscess.
Bleeding on probing is an objective sign of gingival inflammation; it is either absent or present. Inflamed tissues bleed when gently probed because of minute ulcerations in the pocket epithelium and fragility of the underlying vasculature.
At the initial examination the percentage of sites that exhibit bleeding on probing prior to treatment is a clinically useful piece of information since it provides a full-mouth pre-treatment assessment of the extent of gingival inflammation.
Purulent exudate can occasionally be found at sites with gingivitis, it is often detected at sites with chronic periodontitis. Its presence signifies that the site is inflamed and infected. Highly purulent periodontal abscesses are associated with rapid and extensive destruction of bone and surrounding tissues.
During examination, notations should be made of any deviation from normal periodontal anatomy such asalterations in contour, aberrant frenal attachment and minimal amounts or lack of keratinized gingiva.
Altered gingival contours can be the result of a wide range of factors. They become clinically important if they create esthetic problems, make plaque control difficult or interfere with function. e.g. Drug induced ginival enlargement or sometimes the enlargement is due to unusual anatomic variations.
Mandibular tori can become so large that they interfere with chewing or impede access for plaque procedures. In some patients with long standing chronic periodontitis, gingiva becomes firm and enlarged referred to as fibrotic and will not disappear after scaling and root planing.
During examination, notations should be made about narrow bands or the complete absence of keratinised gingiva. Main clinical importance of an adequate zone of keratinised gingiva is that it is often necessary for the patient to comfortably perform oral hygiene procedures
The gingiva overlying teeth with narrow zones of keratinised gingiva is often thin and is prone to toothbrush induced damage followed by recession. Aberrant frenal attachments are anatomic features in which they become problem when they interfere with oral hygiene or other self care procedures.
During the course of a periodontal examination the clinician should begin to develop an idea of what etiologic and predisposing factors are present. As the examination is being performed the clinician should develop an impression of what modifiable factors might be responsible for, or increase the risk for periodontal infections?
Where are the heaviest deposits of plaque and calculus? Are there local factors that can be might increase the risk for periodontal infections? Tooth related factors such as- close roots, palatal-gingival grooves, furcation anatomy, cervical enamel projections, overhangs on dental restorations and other local contributing factors should be noticed and recorded.
It is also important to keep in mind what is known about potential risk factors for chronic periodontitis such as- cigarette smoking, poor compliance, aging, psychological stress and genetic susceptibility.
Assessments of periodontal damage are a mandatory component of a complete periodontal examination. Measurements taken with caliberated periodontal probes are the main way in which damage to periodontium is assessed. Measurements include- probing depths, clinical attachment loss and gingival recession.
Probing depth and clinical attachment loss measurements are routinely recorded at six sites around each tooth An attempt is made to probe every portion of the gingival crevice or pocket around each tooth. In addition to above assessments, radiographs are a necessary adjunct to a thorough periodontal examination.
Probing depth measurements are important because they give a good approximation of periodontal pockets Knowledge of depth, extent and location of pockets gives the clinician a good idea where therapy is indicated. Probing depth reduction is often one of the main goal of many forms of periodontal therapy.
Clinical attachment loss is the distance from the CEJ to the base of probable crevice. If CEJ is missing because it has been destroyed by dental caries or has been removed by placement of a dental restoration, another fixed reference point can be used to measure attachment loss.
Such landmarks include the apical margin of a restoration or the incisal edge of a tooth. When attachment loss are taken from a fixed landmark other than the CEJ they are called relative attachment loss measurements. These are the best way to assess the presence or absence of additional periodontal damage.
Prior to placing patients in the maintenance phase of therapy, clinical attachment loss readings should be taken since these measurements serve as a baseline from which future determinations of additional attachment loss are judged.
Gingival recession is the distance from the CEJ to the gingival margin. Recession is often of major concern to patients since it is a readily visible manifestation of periodontal damage and can cause esthetic problems when occur around anterior teeth.
Damage from periodontal disease often involves the furcation areas of multirooted teeth. The severity of furcation involvement is an important factor in developing a treatment plan for affected sites. Therefore, during a complete periodontal examination the location and severity of furcation involvements should be recorded.
The final assessment of periodontal damage that should be recorded during a complete periodontal examination is abnormal tooth mobility. Although this symptom may have several causes other than periodontal infections, loss of alveolar bone from periodontitis is a major cause of alveolar tooth mobility.
Although the primary focus of a periodontal examination is the periodontium, the teeth also need to be carefully inspected for dental caries, restorative problems and occlusal discrepancies. Tooth related problems have considerable importance in the overall periodontal treatment plan.
Most acceptable charting systems are simple, easy to fill out and read, and contain all of the relevant information collected during the periodontal examination. The periodontal chart requires the help of a dental assistant who serves as a recorder of the examination findings.
The chart shown has places for assessments of probing depths, the presence or absence of plaque, clinical attachment loss, the presence or absence of bleeding on probing and the distance from the CEJ to gingival margin. Assessments of periodontal damage measurements at six sites around each tooth are usually recorded.
Some examiners prefer to record, as the very first step, the presence or absence of plaque on each tooth and surface. The second step is to measure the probing depth, CEJ to GM distance, and the presence to absence of BOP
These three pieces of information are collected virtually at the same time. There is usually no problem in understanding how to measure gingival recession i.e. the CEJ to GM distance when the gingival margin is apical to CEJ.
In addition, there is usually not a problem in understanding that the clinical attachment loss can be obtained by adding the probing depth to the amount of gingival recession. The problem occurs when the gingival margin is coronal to CEJ. In this case, the gingival margin is in full view of examiner
To determine the CEJ to GM measurement the examiner must feel for CEJ with the tip of probe and estimate how far coronally the GM is from CEJ. If GM is at CEJ, then the recording will be 0. If GM is coronal to CEJ recording will be negative.
After completion of active periodontal therapy, prior to placing the patient on a maintenance therapy, the examination should be repeated. The information to be collected is same as that obtained during the initial examination.
A key purpose of this post-treatment evaluation examination is to determine if the administered therapy was successful in arresting the patients disease. The examination also provides baseline data to which all clinical data collected at subsequent examinations can be compared.
Você também pode gostar
- The Making of A Global World 1Documento6 páginasThe Making of A Global World 1SujitnkbpsAinda não há avaliações
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeNo EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeNota: 4 de 5 estrelas4/5 (5794)
- Water Recycling PurposesDocumento14 páginasWater Recycling PurposesSiti Shahirah Binti SuhailiAinda não há avaliações
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceNo EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceNota: 4 de 5 estrelas4/5 (895)
- Aptdc Tirupati Tour PDFDocumento1 páginaAptdc Tirupati Tour PDFAfrid Afrid ShaikAinda não há avaliações
- The Yellow House: A Memoir (2019 National Book Award Winner)No EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Nota: 4 de 5 estrelas4/5 (98)
- A View About The Determinants of Change in Share Prices A Case From Karachi Stock Exchange (Banking)Documento17 páginasA View About The Determinants of Change in Share Prices A Case From Karachi Stock Exchange (Banking)(FPTU HCM) Phạm Anh Thiện TùngAinda não há avaliações
- Change Control Procedure: Yogendra GhanwatkarDocumento19 páginasChange Control Procedure: Yogendra GhanwatkaryogendraAinda não há avaliações
- The Little Book of Hygge: Danish Secrets to Happy LivingNo EverandThe Little Book of Hygge: Danish Secrets to Happy LivingNota: 3.5 de 5 estrelas3.5/5 (400)
- EU Regulation On The Approval of L-Category VehiclesDocumento15 páginasEU Regulation On The Approval of L-Category Vehicles3r0sAinda não há avaliações
- The Emperor of All Maladies: A Biography of CancerNo EverandThe Emperor of All Maladies: A Biography of CancerNota: 4.5 de 5 estrelas4.5/5 (271)
- Coconut Oil Refiners Association, Inc. vs. TorresDocumento38 páginasCoconut Oil Refiners Association, Inc. vs. TorresPia SottoAinda não há avaliações
- Never Split the Difference: Negotiating As If Your Life Depended On ItNo EverandNever Split the Difference: Negotiating As If Your Life Depended On ItNota: 4.5 de 5 estrelas4.5/5 (838)
- DSE at A GlanceDocumento27 páginasDSE at A GlanceMahbubul HaqueAinda não há avaliações
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyNo EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyNota: 3.5 de 5 estrelas3.5/5 (2259)
- Benetton (A) CaseDocumento15 páginasBenetton (A) CaseRaminder NagpalAinda não há avaliações
- Legal Agreement LetterDocumento1 páginaLegal Agreement LetterJun RiveraAinda não há avaliações
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureNo EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureNota: 4.5 de 5 estrelas4.5/5 (474)
- Project On SurveyorsDocumento40 páginasProject On SurveyorsamitAinda não há avaliações
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryNo EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryNota: 3.5 de 5 estrelas3.5/5 (231)
- Business Plan SampleDocumento14 páginasBusiness Plan SampleGwyneth MuegaAinda não há avaliações
- Team of Rivals: The Political Genius of Abraham LincolnNo EverandTeam of Rivals: The Political Genius of Abraham LincolnNota: 4.5 de 5 estrelas4.5/5 (234)
- P1 Ii2005Documento3 páginasP1 Ii2005Boris YanguezAinda não há avaliações
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaNo EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaNota: 4.5 de 5 estrelas4.5/5 (266)
- International Financial Management 8th Edition Eun Test BankDocumento38 páginasInternational Financial Management 8th Edition Eun Test BankPatrickLawsontwygq100% (15)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersNo EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersNota: 4.5 de 5 estrelas4.5/5 (345)
- Project ReportDocumento110 páginasProject ReportAlaji Bah CireAinda não há avaliações
- RBS Internship ReportDocumento61 páginasRBS Internship ReportWaqas javed100% (3)
- The Unwinding: An Inner History of the New AmericaNo EverandThe Unwinding: An Inner History of the New AmericaNota: 4 de 5 estrelas4/5 (45)
- Patent Trolling in IndiaDocumento3 páginasPatent Trolling in IndiaM VridhiAinda não há avaliações
- Procedure For Making Location DecisionsDocumento7 páginasProcedure For Making Location DecisionsFitz JaminitAinda não há avaliações
- The Possibility of Making An Umbrella and Raincoat in A Plastic WrapperDocumento15 páginasThe Possibility of Making An Umbrella and Raincoat in A Plastic WrapperMadelline B. TamayoAinda não há avaliações
- Thai LawDocumento18 páginasThai LawsohaibleghariAinda não há avaliações
- Activity 1 - GlobalizationDocumento4 páginasActivity 1 - GlobalizationIris leavesAinda não há avaliações
- Dhiratara Pradipta Narendra (1506790210)Documento4 páginasDhiratara Pradipta Narendra (1506790210)Pradipta NarendraAinda não há avaliações
- Use CaseDocumento4 páginasUse CasemeriiAinda não há avaliações
- Daily ChecklistDocumento1 páginaDaily ChecklistPatel AspAinda não há avaliações
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreNo EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreNota: 4 de 5 estrelas4/5 (1090)
- Report of The Committee On Regulatory Regime For Trees Grown On Private Land Nov 2012Documento42 páginasReport of The Committee On Regulatory Regime For Trees Grown On Private Land Nov 2012Ravi Shankar KolluruAinda não há avaliações
- Metropolitan Transport Corporation Guindy Estate JJ Nagar WestDocumento5 páginasMetropolitan Transport Corporation Guindy Estate JJ Nagar WestbiindduuAinda não há avaliações
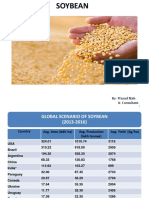
- Soybean Scenario - LaturDocumento18 páginasSoybean Scenario - LaturPrasad NaleAinda não há avaliações
- SWCH 01Documento12 páginasSWCH 01mahakali23Ainda não há avaliações
- Environment Case Alcoa 2016Documento4 páginasEnvironment Case Alcoa 2016Victor TorresAinda não há avaliações
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)No EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Nota: 4.5 de 5 estrelas4.5/5 (121)
- Oil Opportunities in SudanDocumento16 páginasOil Opportunities in SudanEssam Eldin Metwally AhmedAinda não há avaliações