Escolar Documentos
Profissional Documentos
Cultura Documentos
Organophosphate
Enviado por
hendra_darmawan_4Título original
Direitos autorais
Formatos disponíveis
Compartilhar este documento
Compartilhar ou incorporar documento
Você considera este documento útil?
Este conteúdo é inapropriado?
Denunciar este documentoDireitos autorais:
Formatos disponíveis
Organophosphate
Enviado por
hendra_darmawan_4Direitos autorais:
Formatos disponíveis
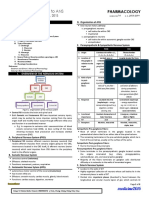
Organophosphates
and carbamates are potent cholinesterase inhibitors capable of causing severe cholinergic toxicity following cutaneous exposure, inhalation, or ingestion.
Wide:
3,000,000
World
per yr people are exposed. up to 300,000 fatalities.
15
to 18 % of all poisoning in Aleppo. Chemical weapons (nerve gases) are organophosphate agents.
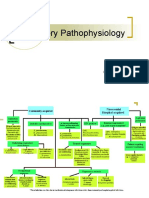
Organophosphorous
acetylcholinesterase overabundance of acetylcholine in the synapse By time the compound undergoes a conformational change (aging) renders the enzyme irreversibly resistant to reactivation.
Carbamate
compounds bind to
compounds unlike organophosphates, are transient cholinesterase inhibitors.
Generally
oral or respiratory exposures result in signs or symptoms within three hours.
symptoms of toxicity from dermal absorption may be delayed up to 12 hours.
while
Generally manifests in minutes to hours
Evidence of cholinergic excess
SLUDGE =
Salivation, Lacrimation, Urination, Defecation, Gastric Emptying.
Bradycardia, Bronchorrhea, Bronchospasm.
BBB
Respiratory insufficiency can result from muscle weakness, decreased central drive, increased secretions, and bronchospasm and it is the lead cause of death. Cardiac arrhythmias, including heart block and QTc prolongation may be due to hypoxemia.
ACH: acetylcholine; Epi: epinephrine; NE: norepinephrine; NMJ: neuromuscular junction.
In children
Seizures are more common (22%-25%). Lethargy and coma (54%-96%). Flaccid muscle weakness,
miosis, excessive salivation are common presenting signs.
10
to 40 % of organophosphorous agent poisoned patients.
24-96 hours after exposure respiratory, and proximal muscle weakness are prominent features.
Occurs Bulbar,
Generally
resolves completely in 1-3 weeks.
Organophosphate
Induced Delayed Neuropathy (OPIDN). specific organophosphorous agents. Usually occurs several weeks after exposure. Primarily motor involvement (symmetrical
Sensory
motor polyneuropathy) flaccid weakness of lower extremities, ascends to involve upper extremities.
disturbances are usually mild. May resolve spontaneously, but can result in permanent neurologic dysfunction.
88% of parents initially deny any exposure history.
petroleum
If
or garlic-like odor.
doubt exists a trial of Atropine (0.01 to 0.02 mg/kg) may be employed. The absence of signs or symptoms of anticholinergic effects following atropine challenge strongly supports the diagnosis
RBC acetylcholinesterase activity:
provides a measure of the degree of toxicity. determine the effectiveness of antidote therapy.
plasma (or pseudo-) cholinesterase activity:
more easily performed. not correlate well with the severity of poisoning. a depression of 25% or more is strong evidence of excessive organophosphate absorption.
o not delay the treatment until
laboratory confirmation is obtained.
Deliver 100 % oxygen via facemask Strongly consider intubation:
patients who appear mildly poisoned may rapidly
Consider volume resuscitation with normal saline or ringer to treat Bradycardia and hypotension. Use activated charcoal within one hour of an ingestion.
develop respiratory failure.
In cases of dermal exposure aggressive decontamination with complete removal of the patient's clothes and vigorous irrigation of the affected areas should be performed.
Competes
with acetylcholine at muscarinic receptors.
Initial
dose 0.05 mg/kg IV bolous. Doubled every 3 to 5 min until bronchial secretions and wheezing stop (SaO2). Repeat every 10 to 30 min until all absorbed organophosphate metabolized (few hours to several days; usually 2 to 12 hours).
Keep
a maintenance dose of atropine for 2-3 days after disappearing of manifestation. and mydriasis are not appropriate markers for therapeutic improvement, as they may indicate continued hypoxia, hypovolemia, or sympathetic stimulation.
Tachycardia
Fever,
muscle fibrillation, and delirium are the main signs of atropine toxicity that indicate that atropine administration should be discontinued, at least temporarily.
Cholinesterase reactivating agent that are effective in treating both muscarinic and nicotinic symptoms.
Use
within 48 hours after poisoning.
Use
Use
with concurrent(bersama) of atropine.
only for moderate to severe Organophosphate poisoning and not carbamate. if neuromuscular dysfunction is present.
Use
25-50
mg/kg IV in 100 ml NS over 30 min.
Repeated Or
after 1 to 2 hours, then every 10 to 12 hour interval if needed
infusion at 10-20 mg/kg/hour.
Continuous Monitor
Blood pressure during administration
Prophylactic
Diazepam
diazepam has been shown to decrease neurocognitive dysfunction after poisoning.
0.1-0.2 mg/kg IV, repeat as necessary if seizures occur.
phenytoin
has no effect on organophosphate agent-induced seizures.
hydrocarbon bases; thus, the clinician should consider hydrocarbon pneumonitis and not to do gastric lavage.
Organophosphates are usually dissolved in
Você também pode gostar
- Community Acquired Pneumonia, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsNo EverandCommunity Acquired Pneumonia, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsAinda não há avaliações
- Problem-based Approach to Gastroenterology and HepatologyNo EverandProblem-based Approach to Gastroenterology and HepatologyJohn N. PlevrisAinda não há avaliações
- Erythrosquamous Diseases / Papulosquamous DiseasesDocumento38 páginasErythrosquamous Diseases / Papulosquamous DiseasesadystiAinda não há avaliações
- Pneumonia AlgorithmDocumento3 páginasPneumonia AlgorithmBien ChuAinda não há avaliações
- LA Myxoma Case PresentationDocumento34 páginasLA Myxoma Case PresentationWiwik Puji LestariAinda não há avaliações
- Pulmonary Embolism Guide: Causes, Symptoms & DiagnosisDocumento60 páginasPulmonary Embolism Guide: Causes, Symptoms & DiagnosisRafika RaraAinda não há avaliações
- Cough: PHR Sangita ShakyaDocumento21 páginasCough: PHR Sangita ShakyaCurex QAAinda não há avaliações
- PnemoniaDocumento4 páginasPnemoniadhavalAinda não há avaliações
- Anal FistulaDocumento26 páginasAnal FistulaBeverly PagcaliwaganAinda não há avaliações
- InhalDocumento33 páginasInhallupeAinda não há avaliações
- Hydrocarbon PoisoningDocumento10 páginasHydrocarbon PoisoningVarshith GandlaAinda não há avaliações
- Pneumoconiosis PDFDocumento10 páginasPneumoconiosis PDFAnonymous lF3962RA1cAinda não há avaliações
- Thermal BurnsDocumento50 páginasThermal BurnsPooya WindyAinda não há avaliações
- Dr. Sana Bashir DPT, MS-CPPTDocumento46 páginasDr. Sana Bashir DPT, MS-CPPTbkdfiesefll100% (1)
- Cardiac TamponadeDocumento6 páginasCardiac TamponadeVicky XieAinda não há avaliações
- Acute Dyspnea First RevisionDocumento56 páginasAcute Dyspnea First RevisionAradhanaRamchandaniAinda não há avaliações
- Lecture Secondary TuberculosisDocumento78 páginasLecture Secondary TuberculosisslyfoxkittyAinda não há avaliações
- Cor PulmonaleDocumento8 páginasCor PulmonaleAymen OmerAinda não há avaliações
- Cysticercosis Diagnosis and TreatmentDocumento18 páginasCysticercosis Diagnosis and TreatmentPhan Cảnh TrìnhAinda não há avaliações
- PancreatitisDocumento59 páginasPancreatitisAarif RanaAinda não há avaliações
- Infective EndocarditisDocumento68 páginasInfective EndocarditisDr. Rajesh PadhiAinda não há avaliações
- Viral Warts (Verrucae) : College of Medicine Name: Qasim Hussain AL-Haleimi AC:207002113Documento18 páginasViral Warts (Verrucae) : College of Medicine Name: Qasim Hussain AL-Haleimi AC:207002113Qasim HaleimiAinda não há avaliações
- Primary Pulmonary TuberculosisDocumento4 páginasPrimary Pulmonary TuberculosisdocdorkmeAinda não há avaliações
- Pathology of The Lung: Djumadi AchmadDocumento26 páginasPathology of The Lung: Djumadi AchmadVivi DeviyanaAinda não há avaliações
- Opportunistic Infections in HIVDocumento50 páginasOpportunistic Infections in HIVamandaAinda não há avaliações
- Complications of HIV/AIDSDocumento60 páginasComplications of HIV/AIDSgladz25Ainda não há avaliações
- Carcinoma Rectum - Janak - NEWDocumento74 páginasCarcinoma Rectum - Janak - NEWTowhidulIslamAinda não há avaliações
- Asthma and CopdDocumento44 páginasAsthma and CopdBeer Dilacshe100% (1)
- Venous Thromboembolism (VTE) - McMaster Pathophysiology ReviewDocumento9 páginasVenous Thromboembolism (VTE) - McMaster Pathophysiology ReviewFadiyah UlfahAinda não há avaliações
- Trigeminal Neuralgia: Defination: According To Iasp (International Association For The Study of Pain)Documento11 páginasTrigeminal Neuralgia: Defination: According To Iasp (International Association For The Study of Pain)saketaggarwalAinda não há avaliações
- A Case Report of Classical Hodgkin's Lymphoma Presented With Anemia of Chronic Disease As Microcytic Hypochromic TypeDocumento3 páginasA Case Report of Classical Hodgkin's Lymphoma Presented With Anemia of Chronic Disease As Microcytic Hypochromic TypeIOSRjournalAinda não há avaliações
- Group Case Study - Pulmonary TBDocumento8 páginasGroup Case Study - Pulmonary TBCj NiñalAinda não há avaliações
- Invasive Pulmonary Aspergi Llosis: Seminars in Respiratory and Critical Care MedicineDocumento24 páginasInvasive Pulmonary Aspergi Llosis: Seminars in Respiratory and Critical Care MedicineChengShiun ShiueAinda não há avaliações
- Acute Rheumatic Heart DiseaseDocumento25 páginasAcute Rheumatic Heart DiseaseArun GeorgeAinda não há avaliações
- Management of ACS Complicated With Acute Heart Failure DR BudianaDocumento27 páginasManagement of ACS Complicated With Acute Heart Failure DR BudianaLuh Leni AriniAinda não há avaliações
- Cardiovascular System: by DR - Nuha Abdel GhaffarDocumento41 páginasCardiovascular System: by DR - Nuha Abdel GhaffarMohammed Alaa EldeanAinda não há avaliações
- Pneumonia and Lung AbscessDocumento50 páginasPneumonia and Lung AbscessMarc Imhotep Cray, M.D.Ainda não há avaliações
- Pathology of the Digestive SystemDocumento28 páginasPathology of the Digestive SystemDianNursyifaRahmahAinda não há avaliações
- On Study Of: Dr.A.K.RastogiDocumento73 páginasOn Study Of: Dr.A.K.RastogiMudit MisraAinda não há avaliações
- SyphilisDocumento89 páginasSyphilisAnuZ13thAinda não há avaliações
- TB TreatmentDocumento58 páginasTB TreatmentNdayisaba CorneilleAinda não há avaliações
- Pneumonia Guide: Causes, Symptoms, Diagnosis and TreatmentDocumento6 páginasPneumonia Guide: Causes, Symptoms, Diagnosis and TreatmentRem AlfelorAinda não há avaliações
- Agranulocytosis FinalDocumento17 páginasAgranulocytosis FinalsanthiyasandyAinda não há avaliações
- Acute Limb IschemicDocumento32 páginasAcute Limb IschemicAnanda YulianAinda não há avaliações
- Acute Pneumonia: Richard T. Ellison III and Gerald R. DonowitzDocumento30 páginasAcute Pneumonia: Richard T. Ellison III and Gerald R. DonowitzNilay ChatterjeeAinda não há avaliações
- Gastric CancerDocumento7 páginasGastric CancerMicah PingawanAinda não há avaliações
- Dr. B. Srinivasa Rao MD Department of Internal Medicine Rajiv Gandhi Institute of Medical Sciences SrikakulamDocumento58 páginasDr. B. Srinivasa Rao MD Department of Internal Medicine Rajiv Gandhi Institute of Medical Sciences SrikakulamPradeep Kumar KaremAinda não há avaliações
- Anal Canal: Fissure in Ano HaemorrhoidsDocumento37 páginasAnal Canal: Fissure in Ano Haemorrhoidsyash shrivastavaAinda não há avaliações
- LEUKOPENIA CAUSES AND TYPESDocumento3 páginasLEUKOPENIA CAUSES AND TYPESN Nur AriniAinda não há avaliações
- Pathophysiology of Malaria: How Parasite Infection Affects the BodyDocumento20 páginasPathophysiology of Malaria: How Parasite Infection Affects the Bodymelia100% (1)
- Causes, Symptoms & Types of Cerebral InfarctionDocumento2 páginasCauses, Symptoms & Types of Cerebral InfarctionMarie Aurora Gielbert MarianoAinda não há avaliações
- Respiratory Pathophysiology: B. Pimentel, M.D. University of Makati College of NursingDocumento12 páginasRespiratory Pathophysiology: B. Pimentel, M.D. University of Makati College of NursingDoc JacqueAinda não há avaliações
- HepatomegalyDocumento2 páginasHepatomegalyFuyumi RiaAinda não há avaliações
- Acute Respiratory Distress SyndromeDocumento3 páginasAcute Respiratory Distress SyndromedindayantAinda não há avaliações
- Phyllodes Tumors of The Breast FINALDocumento25 páginasPhyllodes Tumors of The Breast FINALchinnnababuAinda não há avaliações
- National Program of Cancer Registries Education and Training SeriesDocumento93 páginasNational Program of Cancer Registries Education and Training SeriesNADEEMAinda não há avaliações
- What Is Gas Gangrene? Causes, Symptoms, Treatment & PreventionDocumento6 páginasWhat Is Gas Gangrene? Causes, Symptoms, Treatment & PreventionIwan AchmadiAinda não há avaliações
- Esophagus, TearDocumento36 páginasEsophagus, Tearapi-19641337Ainda não há avaliações
- NEPHROTIC SYNDROME - HamidDocumento20 páginasNEPHROTIC SYNDROME - HamidAbdul Hamid OmarAinda não há avaliações
- Case Presentation: by Michael ArmstrongDocumento21 páginasCase Presentation: by Michael ArmstrongWirawan Amirul BahriAinda não há avaliações
- Med TermsDocumento139 páginasMed TermsCassandra PattonAinda não há avaliações
- Complementary & Alternative Medicine Source Book 2010Documento655 páginasComplementary & Alternative Medicine Source Book 2010Angel Celestial100% (4)
- VitaminsDocumento2 páginasVitaminshendra_darmawan_4Ainda não há avaliações
- GB Station 7Documento3 páginasGB Station 7hendra_darmawan_4Ainda não há avaliações
- Common Cold EducationDocumento2 páginasCommon Cold Educationhendra_darmawan_4Ainda não há avaliações
- Poisoned of Corrosive AgentDocumento30 páginasPoisoned of Corrosive AgentSandy WijayaAinda não há avaliações
- Type2 Diabetes HandoutDocumento1 páginaType2 Diabetes Handouthendra_darmawan_4Ainda não há avaliações
- Methotrexate MTX: Antineoplastic Agents Antibetabolites Drug Mechanism Clinical Use ToxicityDocumento2 páginasMethotrexate MTX: Antineoplastic Agents Antibetabolites Drug Mechanism Clinical Use Toxicityhendra_darmawan_4Ainda não há avaliações
- VitaminsDocumento2 páginasVitaminshendra_darmawan_4Ainda não há avaliações
- Penanganan Terkini Infeksi Virus Sitomegalo (CMV) + EditDocumento72 páginasPenanganan Terkini Infeksi Virus Sitomegalo (CMV) + Edithendra_darmawan_4Ainda não há avaliações
- Problem Solving and Patient Management in Family PracticeDocumento21 páginasProblem Solving and Patient Management in Family Practicehendra_darmawan_4Ainda não há avaliações
- Drug Mechanism Use Side/Adverse Effects Nursing ImplicationsDocumento3 páginasDrug Mechanism Use Side/Adverse Effects Nursing Implicationshendra_darmawan_4Ainda não há avaliações
- Faal KBK GinjalDocumento37 páginasFaal KBK Ginjalhendra_darmawan_4Ainda não há avaliações
- Peripheral Nerve-Blok NeuromuscularDocumento42 páginasPeripheral Nerve-Blok Neuromuscularhendra_darmawan_4Ainda não há avaliações
- Hipertensi SMT Vi KBKDocumento64 páginasHipertensi SMT Vi KBKhendra_darmawan_4Ainda não há avaliações
- Urine Case 2010-2Documento9 páginasUrine Case 2010-2hendra_darmawan_4Ainda não há avaliações
- Uti 2010Documento25 páginasUti 2010hendra_darmawan_4Ainda não há avaliações
- Evaluating HealthCare Service (Rev)Documento29 páginasEvaluating HealthCare Service (Rev)hendra_darmawan_4Ainda não há avaliações
- Sub Arachnoid BlockDocumento32 páginasSub Arachnoid Blockhendra_darmawan_4Ainda não há avaliações
- Nonvolatile Anesthetic AgentsDocumento14 páginasNonvolatile Anesthetic Agentshendra_darmawan_4Ainda não há avaliações
- Lecture Presentation - Fluid, Electrolyte and Acid Base BalanceDocumento16 páginasLecture Presentation - Fluid, Electrolyte and Acid Base Balancehendra_darmawan_4100% (2)
- Kul Perdana Anasthesiology DR - HariBDocumento23 páginasKul Perdana Anasthesiology DR - HariBhendra_darmawan_4Ainda não há avaliações
- Fluids 2000Documento45 páginasFluids 2000hendra_darmawan_4Ainda não há avaliações
- Xfluid and Electrolytes 1Documento52 páginasXfluid and Electrolytes 1api-3816499Ainda não há avaliações
- Arterial Blood Gas AnalysisDocumento28 páginasArterial Blood Gas Analysishendra_darmawan_4Ainda não há avaliações
- Non EthanolDocumento39 páginasNon Ethanolhendra_darmawan_4Ainda não há avaliações
- Xfluid and Electrolytes 1Documento52 páginasXfluid and Electrolytes 1api-3816499Ainda não há avaliações
- Fluid & Electrolyte TherapyDocumento33 páginasFluid & Electrolyte Therapyhendra_darmawan_4Ainda não há avaliações
- Ika-kelompok-Acute Fever in ChildrenDocumento40 páginasIka-kelompok-Acute Fever in Childrenhendra_darmawan_4Ainda não há avaliações
- Kuliah Hiv2007Documento41 páginasKuliah Hiv2007hendra_darmawan_4Ainda não há avaliações
- To Study The Dose Response Curve (DRC) of Acetylcholine Using Frog Rectus Abdominis MuscleDocumento15 páginasTo Study The Dose Response Curve (DRC) of Acetylcholine Using Frog Rectus Abdominis MuscleVidhiAinda não há avaliações
- MecamylanimeDocumento15 páginasMecamylanimeNoor HaiderAinda não há avaliações
- Pumhs Pharma McqsDocumento3 páginasPumhs Pharma McqsAzra BalochAinda não há avaliações
- EnvironmentDocumento9 páginasEnvironmentrimantasjankusAinda não há avaliações
- Autonomic Nervous System - PPT 1Documento98 páginasAutonomic Nervous System - PPT 1PROF DR SHAHMURAD100% (9)
- Questions PharmaDocumento176 páginasQuestions Pharmaminakshi boss100% (3)
- Long-Term Effects of Repeated Botulinum Toxin Injection in Cosmetic Therapeutics - Crook, 2022Documento8 páginasLong-Term Effects of Repeated Botulinum Toxin Injection in Cosmetic Therapeutics - Crook, 2022Rafael Autran Cavalcante AraújoAinda não há avaliações
- Antiparasitc PharmacologyDocumento153 páginasAntiparasitc PharmacologyMohanad Al-BayatiAinda não há avaliações
- Review of Pharmacology (PGMEE) Paperback - 2018 (PDFDrive)Documento660 páginasReview of Pharmacology (PGMEE) Paperback - 2018 (PDFDrive)xwendnla russiaAinda não há avaliações
- Pharmacology QuestionsDocumento33 páginasPharmacology QuestionsPurnimaAinda não há avaliações
- Pharmacology 2.2 Introduction To ANS - Dr. ReyesDocumento8 páginasPharmacology 2.2 Introduction To ANS - Dr. ReyesAesthetics MinAinda não há avaliações
- IARI PHD Entrance Question Paper 2011 - EntomologyDocumento13 páginasIARI PHD Entrance Question Paper 2011 - EntomologyAbhay Kumar100% (1)
- Muscles NotesDocumento13 páginasMuscles NotesGabrielle ThompsonAinda não há avaliações
- 2010 A Level h2 Biology Dunman HighDocumento46 páginas2010 A Level h2 Biology Dunman HighStephyAinda não há avaliações
- Autonomic Nervous System Anatomy and PhysiologyDocumento50 páginasAutonomic Nervous System Anatomy and PhysiologyMAHARANIAinda não há avaliações
- ANS Physiology and PharmacologyDocumento79 páginasANS Physiology and PharmacologyMarc Imhotep Cray, M.D.100% (1)
- Parasympathomimetic DrugsDocumento15 páginasParasympathomimetic DrugsRohit PrajapatiAinda não há avaliações
- GABA 500: Gamma-Aminobutyric AcidDocumento2 páginasGABA 500: Gamma-Aminobutyric AcidHary YrehamAinda não há avaliações
- Anatomy MusclesDocumento76 páginasAnatomy MusclesMathios TigerosAinda não há avaliações
- Tutorial 2Documento4 páginasTutorial 2Lina KhanAinda não há avaliações
- Potent Ethanomedicinal Plant Semecarpus Anacardium Linn A ReviewDocumento7 páginasPotent Ethanomedicinal Plant Semecarpus Anacardium Linn A ReviewBASKAR RAJAinda não há avaliações
- Cns Drugs Summary Review Notes FinalDocumento12 páginasCns Drugs Summary Review Notes Finalمريم حجيAinda não há avaliações
- Systemic Response To Injury and Metabolic SupportDocumento118 páginasSystemic Response To Injury and Metabolic SupportNicole DeverasAinda não há avaliações
- 1.1 Synthesis and Metabolism of AcetylcholineDocumento1 página1.1 Synthesis and Metabolism of AcetylcholineDRxNaveen Maurya012Ainda não há avaliações
- Dr. Niranjan Murthy H L Asst. Prof. of Physiology SSMC, TumkurDocumento39 páginasDr. Niranjan Murthy H L Asst. Prof. of Physiology SSMC, Tumkurnirilib100% (1)
- 4 2-PharmacologyDocumento33 páginas4 2-PharmacologyAmiel GarciaAinda não há avaliações
- Active Ingredient Conct. (%W/W) Trade Name Formulation Usage Class Moa Group Moa CodeDocumento63 páginasActive Ingredient Conct. (%W/W) Trade Name Formulation Usage Class Moa Group Moa CodeMitsuton Lanspira100% (1)
- Neurons Nerve Fibers and Peripheral NervesDocumento20 páginasNeurons Nerve Fibers and Peripheral NervesCJ GoAinda não há avaliações
- NEUROMUSCULAR TRANSMISSION: ANATOMY AND PHYSIOLOGYDocumento45 páginasNEUROMUSCULAR TRANSMISSION: ANATOMY AND PHYSIOLOGYparuAinda não há avaliações
- Chapter 12 Organophosphate PoisoningDocumento13 páginasChapter 12 Organophosphate Poisoningarief muhammadAinda não há avaliações