Escolar Documentos
Profissional Documentos
Cultura Documentos
The Mechanical Ventilator
Enviado por
John AlcantaraDescrição original:
Direitos autorais
Formatos disponíveis
Compartilhar este documento
Compartilhar ou incorporar documento
Você considera este documento útil?
Este conteúdo é inapropriado?
Denunciar este documentoDireitos autorais:
Formatos disponíveis
The Mechanical Ventilator
Enviado por
John AlcantaraDireitos autorais:
Formatos disponíveis
Mechanical ventilator is a positive- or negative-pressure breathing device that can maintain ventilation and oxygen delivery for a prolonged
period.
PaO2 50 mm Hg with FiO2 0.60 PaO2 50 mm Hg with pH 7.25 Vital capacity 2 times tidal volume Negative inspiratory force 25 cm H2O Respiratory rate 35/min
Negative-Pressure Ventilators
Iron Lung (Drinker Respirator Tank) Body Wrap (Pneumo-Wrap) Chest Cuirass (Tortoise Shell)
Positive-Pressure Ventilators
Pressure-Cycled Ventilators Time-Cycled Ventilators Volume-Cycled Ventilators Noninvasive Positive-Pressure Ventilation
Negative-pressure ventilators exert a negative pressure on the external chest.
Decreasing the intrathoracic pressure during inspiration allows air to flow into the lung, filling its volume.
It was used extensively during polio epidemics in the past and currently is used by a few polio survivors and patients with other neuromuscular disorders
Portable devices that require a rigid cage or shell to create a negative-pressure chamber around the thorax and abdomen. Because of problems with proper fit and system leaks, these types of ventilators are used only with carefully selected patients.
inflate the lungs by exerting positive pressure on the airway, pushing air in, similar to a bellows mechanism, forcing the alveoli to expand during inspiration. These ventilators are widely used in the hospital setting and are increasingly used in the home for patients with primary lung disease.
delivers a flow of air (inspiration) until it reaches a preset pressure, and then cycles off, and expiration occurs passively.
terminate or control inspiration after a preset time. The volume of air the patient receives is regulated by the length of inspiration and the flow rate of the air.
Most commonly used The volume of air delivered with each inspiration is preset. Once this preset volume is delivered to the patient, the ventilator cycles off and exhalation occurs passively.
A method of positive-pressure ventilation that can be given via face masks that cover the nose and mouth, nasal masks, or other oral or nasal devices
refers
to how breaths are delivered to the patient. The most commonly used modes are:
Assistcontrol Intermittent Mandatory Ventilation Synchronized Intermittent Mandatory Ventilation Pressure Support Ventilation Airway Pressure Release Ventilation
provides
full ventilatory support by delivering a preset tidal volume and respiratory rate.
provides a combination of mechanically assisted breaths and spontaneous breaths.
delivers a preset tidal volume and number of breaths per minute. Between ventilator-delivered breaths, the patient can breathe spontaneously with no assistance from the ventilator on those extra breaths.
applies a pressure plateau to the airway throughout the patienttriggered inspiration to decrease resistance within the tracheal tube and ventilator tubing. Pressure support is reduced gradually as the patients strength increases.
a time triggered, pressure-limited, timecycled mode of mechanical ventilation that allows unrestricted, spontaneous breathing throughout the ventilatory cycle. The inflation period is long, and breaths may be initiated spontaneously as well as by the ventilator.
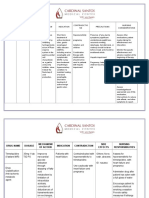
Type of ventilator (eg, volume-cycled, pressurecycled, negative-pressure)
Controlling mode (eg, controlled ventilation, assistcontrol ventilation, synchronized intermittent mandatory ventilation)
Tidal volume and rate settings (tidal volume is usually set at 6 to 12 mL/kg [ideal body weight]; rate is usually set at 12 to 16 breaths/min)
FiO2 setting Inspiratory pressure reached and pressure limit (normal is 15 to 20 cm H2O; this increases if there is increased airway resistance or decreased compliance) Sensitivity (a 2-cm H2O inspiratory force should trigger the ventilator) Inspiratory-to-expiratory ratio (usually 1:3 [1 second of inspiration to 3 seconds of expiration] or 1:2)
Minute volume (tidal volume respiratory rate, usually 6 to 8 L/min) Sigh settings (usually set at 1.5 times the tidal volume and ranging from 1 to 3 per hour), if applicable Water in the tubing, disconnection or kinking of the tubing
Humidification
(humidifier filled with water) and temperature (turned on and functioning properly) and pressure support level, if applicable (PEEP is usually set at 5 to 15 cm H2O)
Alarms
PEEP
If the ventilator system malfunctions and the problem cannot be identified and corrected immediately, the nurse must ventilate the patient with a manual resuscitation bag until the problem is resolved.
Coughing
or plugged airway tube
Patient
Suction airway for secretions, empty condensation fluid from circuit
bucking ventilator
Decreasing
Adjust sensitivity
lung compliance
Manually ventilate patient
Increase in compliance
None
Leak in ventilator or tubing; cuff on tube/ humidifier not tight
Check entire ventilator circuit for patency Correct leak
Você também pode gostar
- A Simple Guide to Hypovolemia, Diagnosis, Treatment and Related ConditionsNo EverandA Simple Guide to Hypovolemia, Diagnosis, Treatment and Related ConditionsAinda não há avaliações
- Ventilator, Weaning, SuctioningDocumento81 páginasVentilator, Weaning, SuctioningwaqarAinda não há avaliações
- Managing Chest DrainageDocumento63 páginasManaging Chest DrainagecarlalynneAinda não há avaliações
- Extubation CriteriaDocumento17 páginasExtubation CriteriaOliver TabagAinda não há avaliações
- ARDSDocumento27 páginasARDSChloie Marie RosalejosAinda não há avaliações
- Terminology Causes of Cardiac Arrest C.P.R. For The Adult, Child & Baby Stroke & Stroke ManagementDocumento28 páginasTerminology Causes of Cardiac Arrest C.P.R. For The Adult, Child & Baby Stroke & Stroke Managementbusiness911Ainda não há avaliações
- Managing Mechanical VentilationDocumento7 páginasManaging Mechanical VentilationArden QuiambaoAinda não há avaliações
- OxygenationDocumento50 páginasOxygenationLulu MushiAinda não há avaliações
- Suctioning Artificial Airways - AdultsDocumento27 páginasSuctioning Artificial Airways - AdultssdaAinda não há avaliações
- Basics of Mechanical Ventilation For Residents: DR Ghaleb Almekhlafi MD, SFCCM PSMMCDocumento43 páginasBasics of Mechanical Ventilation For Residents: DR Ghaleb Almekhlafi MD, SFCCM PSMMCGHALEB A. Almekhlafi100% (1)
- NebulisationDocumento26 páginasNebulisationSilpa Jose TAinda não há avaliações
- Basic VentilationDocumento64 páginasBasic VentilationGBJ VisionAinda não há avaliações
- Airway Skills 2 - Bag Valve MaskDocumento4 páginasAirway Skills 2 - Bag Valve MaskRinna MauLiddaAinda não há avaliações
- Mechanical Ventilation and Intracranial PressureDocumento30 páginasMechanical Ventilation and Intracranial PressureFlavius AnghelAinda não há avaliações
- Mechanical Ventilation TherapyDocumento17 páginasMechanical Ventilation TherapyFaizal FlAinda não há avaliações
- Abcde ApproachDocumento3 páginasAbcde ApproachMaria Isabel Medina MesaAinda não há avaliações
- Respiratory Therapist, NICU/ICUDocumento5 páginasRespiratory Therapist, NICU/ICUapi-77517256Ainda não há avaliações
- Nursing DiagnosisDocumento4 páginasNursing DiagnosisKrizzia CarlosAinda não há avaliações
- Aerosoltherapy Nebu 120503115712 Phpapp01Documento65 páginasAerosoltherapy Nebu 120503115712 Phpapp01Aan Ika SugathotAinda não há avaliações
- 07.03.53 Mechanical VentilationDocumento5 páginas07.03.53 Mechanical VentilationSuganya BalachandranAinda não há avaliações
- Nursing Management of Mechanically Ventilated PatientsDocumento179 páginasNursing Management of Mechanically Ventilated PatientsSourabh AlawaAinda não há avaliações
- Cardiac TestsDocumento17 páginasCardiac TestsGiorgiana pAinda não há avaliações
- 161111163114Documento31 páginas161111163114lejizixAinda não há avaliações
- Tracheostomy Care - An Evidence-Based Guide - American Nurse TodayDocumento4 páginasTracheostomy Care - An Evidence-Based Guide - American Nurse TodayZulaikah Nur IstiqomahAinda não há avaliações
- Acute Respiratory Distress SyndromeDocumento70 páginasAcute Respiratory Distress SyndromeAndrea Del Villar100% (1)
- AlbuminDocumento14 páginasAlbuminMaria Chona Penillos HularAinda não há avaliações
- JD Respiratory TherapistDocumento3 páginasJD Respiratory TherapistLawrence MacaraegAinda não há avaliações
- Respiratory Care ModalitiesDocumento63 páginasRespiratory Care ModalitiesErica Clerigo LandichoAinda não há avaliações
- Cardiopulmonary ResuscitationDocumento10 páginasCardiopulmonary ResuscitationZacchariah Zeref CaraigAinda não há avaliações
- Pneumonia: DefinitionDocumento5 páginasPneumonia: DefinitionhemaanandhyAinda não há avaliações
- Pulmonary ContusionDocumento83 páginasPulmonary ContusionLouise Anne Agnazata GayoAinda não há avaliações
- Asthma Action PlanDocumento2 páginasAsthma Action PlanCharles S. Williams RRT, AE-CAinda não há avaliações
- Cardiac ArrestDocumento50 páginasCardiac ArrestAnju Radhika100% (1)
- AARC Clinical Practice Guideline: Incentive SpirometryDocumento10 páginasAARC Clinical Practice Guideline: Incentive SpirometrytruptimptAinda não há avaliações
- Tension Pneumothorax: Modifiable FactorsDocumento3 páginasTension Pneumothorax: Modifiable FactorsJustin MaverickAinda não há avaliações
- On Emergency DrugsDocumento25 páginasOn Emergency DrugsBikram Chhetry100% (1)
- Administration of Inotropes Evidence Based Nursing PolicyDocumento8 páginasAdministration of Inotropes Evidence Based Nursing PolicyRonald ThakorAinda não há avaliações
- 10 AsthmaDocumento39 páginas10 AsthmaAkash MishraAinda não há avaliações
- Ajnr 7 4 2 PDFDocumento8 páginasAjnr 7 4 2 PDFniaAinda não há avaliações
- Severe Asthma ChildrenDocumento4 páginasSevere Asthma ChildreneddcitoAinda não há avaliações
- Noninvasive VentilationDocumento6 páginasNoninvasive VentilationEma MagfirahAinda não há avaliações
- Concept MapDocumento1 páginaConcept Mapapi-246466200Ainda não há avaliações
- Ethical Principles: Example: Surgery, or Any ProcedureDocumento3 páginasEthical Principles: Example: Surgery, or Any ProcedureKevin Miguel Rivera100% (1)
- Respiratory DiseasesDocumento11 páginasRespiratory DiseasesMichael Angelo SeñaAinda não há avaliações
- Cardio-Pulmonary Resuscitation (CPR)Documento18 páginasCardio-Pulmonary Resuscitation (CPR)Savita HanamsagarAinda não há avaliações
- Acute Respiratory FailureDocumento19 páginasAcute Respiratory Failurek uche100% (1)
- Cardio-Pulmonary Resuscitation: Dr. Sebastian ValceaDocumento16 páginasCardio-Pulmonary Resuscitation: Dr. Sebastian ValceaAna MariaAinda não há avaliações
- CopdDocumento14 páginasCopdMohd Farid Bin RosliAinda não há avaliações
- Epidural Anesthesia (OB)Documento3 páginasEpidural Anesthesia (OB)zooAinda não há avaliações
- Feeding JejunostomyDocumento4 páginasFeeding JejunostomyAbuAinda não há avaliações
- Vent Workshop NP Boot CampDocumento47 páginasVent Workshop NP Boot CampChing WeiAinda não há avaliações
- Updated: Dec 07, 2016 Author: Justina Gamache, MD Chief Editor: Guy W Soo Hoo, MD, MPHDocumento42 páginasUpdated: Dec 07, 2016 Author: Justina Gamache, MD Chief Editor: Guy W Soo Hoo, MD, MPHgita suci arianiAinda não há avaliações
- Pulmonary Function Testing1Documento51 páginasPulmonary Function Testing1kusaarAinda não há avaliações
- Respi MVDocumento25 páginasRespi MVtimie_reyesAinda não há avaliações
- Bronchial AsthmaDocumento71 páginasBronchial AsthmaHero MondaresAinda não há avaliações
- VSim SARAH LIN For Nursing - Health Assessment POST QUIZDocumento5 páginasVSim SARAH LIN For Nursing - Health Assessment POST QUIZWen RodsaAinda não há avaliações
- Pleural Fluid AnalysisDocumento15 páginasPleural Fluid AnalysisNatalie Sarah MoonAinda não há avaliações
- Respiratory Assessment (IPPA) : Check Tactile FremitusDocumento5 páginasRespiratory Assessment (IPPA) : Check Tactile FremitusMabesAinda não há avaliações
- English in Urgent Care Medicine – Anglictina V Urgentní Medicíne: Textbook – UcebniceNo EverandEnglish in Urgent Care Medicine – Anglictina V Urgentní Medicíne: Textbook – UcebniceAinda não há avaliações
- Nursing Diagnosis For DKADocumento6 páginasNursing Diagnosis For DKARhanne Bolante88% (24)
- Jherwin Latest ResumeDocumento2 páginasJherwin Latest ResumeJohn AlcantaraAinda não há avaliações
- NovomixDocumento5 páginasNovomixJohn AlcantaraAinda não há avaliações
- OmepronDocumento3 páginasOmepronJohn AlcantaraAinda não há avaliações
- NovomixDocumento5 páginasNovomixJohn AlcantaraAinda não há avaliações
- Ugib NCPDocumento5 páginasUgib NCPMarlo ParaynoAinda não há avaliações
- Anatomy and PhysiologyDocumento13 páginasAnatomy and PhysiologyernestoAinda não há avaliações
- Drug Therapy Targets For Diabetic Nephropathy: An Overview: Review ArticleDocumento9 páginasDrug Therapy Targets For Diabetic Nephropathy: An Overview: Review ArticleJohn AlcantaraAinda não há avaliações
- BREAST CANCER ReportDocumento9 páginasBREAST CANCER ReportJohn AlcantaraAinda não há avaliações
- Apn2 Case Study DkaDocumento25 páginasApn2 Case Study DkaJohn AlcantaraAinda não há avaliações
- Activity Intolerance Related To Decreased Cardiac Output, Due To EndocarditisDocumento4 páginasActivity Intolerance Related To Decreased Cardiac Output, Due To EndocarditisJohn AlcantaraAinda não há avaliações
- Pathophysiology: Diet Sedentary Lifestyle Familial History of Hypertension Age - Common in 40 and AboveDocumento4 páginasPathophysiology: Diet Sedentary Lifestyle Familial History of Hypertension Age - Common in 40 and AboveJohn AlcantaraAinda não há avaliações
- Diabetic Ketoacidosis Case StudyDocumento6 páginasDiabetic Ketoacidosis Case StudyJohn AlcantaraAinda não há avaliações
- Diabetic Ketoacidosis Case StudyDocumento6 páginasDiabetic Ketoacidosis Case StudyJohn AlcantaraAinda não há avaliações
- Drug Therapy Targets For Diabetic Nephropathy: An Overview: Review ArticleDocumento9 páginasDrug Therapy Targets For Diabetic Nephropathy: An Overview: Review ArticleJohn AlcantaraAinda não há avaliações
- PneumoniaDocumento18 páginasPneumoniaJohn AlcantaraAinda não há avaliações
- PneumoniaDocumento18 páginasPneumoniaJohn AlcantaraAinda não há avaliações
- Breast CancerDocumento18 páginasBreast CancerJohn AlcantaraAinda não há avaliações
- Ecg LectureDocumento95 páginasEcg LectureJohn AlcantaraAinda não há avaliações
- Ovarian CancerDocumento27 páginasOvarian CancerJohn Alcantara100% (1)
- PneumothoraxDocumento13 páginasPneumothoraxJohn AlcantaraAinda não há avaliações
- Pulmonary Embolism (BALANDAN)Documento26 páginasPulmonary Embolism (BALANDAN)John AlcantaraAinda não há avaliações
- PulmonaryDocumento3 páginasPulmonaryJohn AlcantaraAinda não há avaliações
- Breast Cancer Case StudyDocumento48 páginasBreast Cancer Case Studyjansestacio93% (54)
- NCP Risk For Fluid Volume DeficitDocumento2 páginasNCP Risk For Fluid Volume DeficitJeanineReyes44% (9)
- Presented By: Jan Patrick C. DiezDocumento25 páginasPresented By: Jan Patrick C. DiezJohn AlcantaraAinda não há avaliações
- Cervical Cancer Powerpoint New EditDocumento24 páginasCervical Cancer Powerpoint New EditJohn AlcantaraAinda não há avaliações
- LactuloseDocumento2 páginasLactuloseGrace Iloreta RN82% (11)
- Breastcancer Edited 100201202904 Phpapp01Documento59 páginasBreastcancer Edited 100201202904 Phpapp01John AlcantaraAinda não há avaliações
- Biology Synopsis Bridge Course (8.5.18 To19.5.18)Documento37 páginasBiology Synopsis Bridge Course (8.5.18 To19.5.18)Anil Kumar AAinda não há avaliações
- CCCF - 2012 - EN Prevention and Reduction PDFDocumento178 páginasCCCF - 2012 - EN Prevention and Reduction PDFdorinutza280Ainda não há avaliações
- Patient'S Case Performa FileDocumento13 páginasPatient'S Case Performa Filevipul tandonAinda não há avaliações
- Filipino Scientists: GE 07 Science, Technology and SocietyDocumento4 páginasFilipino Scientists: GE 07 Science, Technology and SocietyEvangeline EnocAinda não há avaliações
- Basic First Aid TrainingDocumento32 páginasBasic First Aid Trainingtukaram patilAinda não há avaliações
- Big Data Final ReportDocumento34 páginasBig Data Final Reportclinfox100% (2)
- Mendelian & Modern Genetics: General Biology 2Documento51 páginasMendelian & Modern Genetics: General Biology 2sannsannAinda não há avaliações
- Hendry County Complaint, SoFlo AG, LLC.Documento16 páginasHendry County Complaint, SoFlo AG, LLC.News-PressAinda não há avaliações
- The Importance of Empathy ArticleDocumento3 páginasThe Importance of Empathy ArticleslvAinda não há avaliações
- Vijayalakshmi MenopauseDocumento7 páginasVijayalakshmi MenopauseakankshaAinda não há avaliações
- Psych Drugs Cheat SheetDocumento4 páginasPsych Drugs Cheat SheetSunel100% (35)
- Infection Control Committee 6 Icc. Meeting DATE: MAY 22, 2020 TIME: 11:50 AM - 3:40 PM Venue: Board Room, Administrative Office 10Th FloorDocumento7 páginasInfection Control Committee 6 Icc. Meeting DATE: MAY 22, 2020 TIME: 11:50 AM - 3:40 PM Venue: Board Room, Administrative Office 10Th FloorCris GalendezAinda não há avaliações
- Eucalyptus Oil PDFDocumento2 páginasEucalyptus Oil PDFJenniferAinda não há avaliações
- Cases and Doctrines On Legal MedicineDocumento44 páginasCases and Doctrines On Legal MedicineEliza MontemayorAinda não há avaliações
- Cell LineageDocumento7 páginasCell LineageAmar Kant JhaAinda não há avaliações
- Figo Misoprostol IufdDocumento0 páginaFigo Misoprostol IufdAntoni KurniawanAinda não há avaliações
- Monograph On Lung Cancer July14Documento48 páginasMonograph On Lung Cancer July14PatAinda não há avaliações
- Neurodegenerative DiseasesDocumento2 páginasNeurodegenerative DiseasesBerniceTanAinda não há avaliações
- Genetic Recombination in Bacteria Horizon of The BDocumento9 páginasGenetic Recombination in Bacteria Horizon of The BAngelo HernandezAinda não há avaliações
- Natal PlanetsDocumento290 páginasNatal PlanetsAnonymous PErKNy9100% (1)
- A Novel Method For Detection of The Transition Between Atrial Fibrillation and Sinus RhythmDocumento7 páginasA Novel Method For Detection of The Transition Between Atrial Fibrillation and Sinus RhythmcfunnyxAinda não há avaliações
- Clinico-Pathological Study On Haemophilia: An Analysis of 50 CasesDocumento4 páginasClinico-Pathological Study On Haemophilia: An Analysis of 50 CasesSajjad Hossain ShuvoAinda não há avaliações
- VPP No InvasivaDocumento12 páginasVPP No InvasivaItzel AgustínAinda não há avaliações
- The Effects of Virus Variants On COVID-19 Vaccines: Inglés Nivel II Examen FinalDocumento4 páginasThe Effects of Virus Variants On COVID-19 Vaccines: Inglés Nivel II Examen FinalDIEGOAinda não há avaliações
- Anger: Realized By: Supervised byDocumento15 páginasAnger: Realized By: Supervised byChahinaz Frid-ZahraouiAinda não há avaliações
- (Ebook PDF) Equine Ophthalmology 3Rd Edition by Brian C. GilgerDocumento41 páginas(Ebook PDF) Equine Ophthalmology 3Rd Edition by Brian C. Gilgerjessica.rohrbach136100% (47)
- MannitolDocumento10 páginasMannitolFenzy Septiana AnggrainiAinda não há avaliações
- Diagnostic Value of Gastric Shake Test For Hyaline Membrane Disease in Preterm InfantDocumento6 páginasDiagnostic Value of Gastric Shake Test For Hyaline Membrane Disease in Preterm InfantNovia KurniantiAinda não há avaliações
- SMH Annual Report 2016Documento12 páginasSMH Annual Report 2016Chelsey BoyleAinda não há avaliações
- Chi Cards 1Documento43 páginasChi Cards 1SwordAceAinda não há avaliações